Abstract
Background
The monocyte/high-density lipoprotein ratio (MHR) has emerged as a promising alternative biomarker in the fields of cardiovascular disease and atrial fibrillation (AF). This retrospective study was aimed to explore the predictive value of the MHR for the late recurrence of AF after radiofrequency ablation.
Methods
From April 2015 to October 2018, patients with paroxysmal AF who had undergone radiofrequency catheter ablation at Subei People’s Hospital of Jiangsu Province were enrolled in our study. All the participants were observed until November 2019 after the procedure. During the postoperative follow up, the patients were categorized into the recurrence group and maintenance of sinus rhythm group based on who had experienced AF recurrence.
Results
One hundred twenty-five patients were diagnosed with paroxysmal AF, with an average age of 61.2 ± 9.3 years. Forty-seven patients had developed late recurrence during a mean follow up of 25.1 ± 12.0 months. The AF recurrence event rates were significantly increased in the highest MHR tertile compared with those in the lowest MHR tertile (22.0% vs. 57.1%; P < 0.05). On multivariate logistic regression analysis, the preablation MHR (OR = 1.34; 95% CI = 1.12 ~ 1.60; P = 0.001) and left atrial diameter (LAD) (OR = 1.21, 95% CI = 1.08 ~ 1.35; P = 0.001) were independent risk factors predicting the recurrence of AF after radiofrequency ablation. Furthermore, receiver operating characteristic (ROC) curve analysis revealed that the area under the curve (AUC) of the MHR was 0.712 (95% CI = 0.618 ~ 0.806; P = 0.000) and that of LAD was 0.739 (95% CI = 0.653 ~ 0.814; P = 0.000). Z-test found no significant difference between the MHR and LAD regarding the AUC (Z = 0.451; P = 0.652).
Conclusion
An elevated preablation MHR was associated with an increased risk of the postoperative recurrence of AF. Additionally, the MHR independently predicted the late recurrence of paroxysmal AF after radiofrequency ablation, with the same predictive value as LAD.
Keywords: Paroxysmal atrial fibrillation, Radiofrequency ablation, Monocyte/HDL ratio, Left atrial diameter, Late recurrence
Background
Atrial fibrillation (AF) is a common tachyarrhythmia, accompanied by disorder of atrial electrical activity and mechanical dysfunction. On account of the gradual aging of the population and unhealthy living habits, the global incidence of AF is expected to escalate over the next few decades. During the attack of AF, part of the blood is stagnated in the atrium, and the slow blood flow easily contributes to thrombus formation in the atrium. Therefore, patients with AF are more likely to have a high incidence of stroke and systemic embolism, seriously affecting the quality of life of patients and resulting in a huge burden to public health [1].
Pulmonary vein electrical isolation achieved by radiofrequency catheter ablation has been the cornerstone of catheter-based therapies for AF, with the greatest efficacy as a promising treatment option in patients with paroxysmal AF [2]. The techniques of catheter ablation for AF have undergone a profound evolution recently. Nonetheless, long-term postoperative atrial arrhythmia-free survival remains unsatisfactory, with a high AF recurrence rate of 25–50% during the postoperative follow up [3]. Therefore, it is of great significance to detect the clinical factors influencing the successful maintenance of the sinus rhythm in patients with AF after ablation.
The monocyte/HDL ratio (MHR), as a new indicator of inflammation and oxidative stress, has been widely explored in the field of cardiovascular disorders, including acute coronary syndrome [4]. Additionally, the MHR was found to be a candidate cardiovascular prognostic marker in chronic kidney disease [5]. Furthermore, the MHR could be used as a predictor of AF recurrence after cryoballoon-based catheter ablation and an elevated preablation MHR was associated with increased recurrence of AF [6]. However, the prognostic value of the MHR in patients with paroxysmal AF after radiofrequency ablation remains controversial. Thus, the study was aimed to investigate the prognostic impact of the MHR on paroxysmal AF after radiofrequency ablation in an observational cohort.
Methods
Study population
In this retrospective study, patients with paroxysmal AF who were admitted for pulmonary vein isolation (PVI) treatment using radiofrequency ablation at the Department of Cardiology of Subei People’s Hospital of Jiangsu Province from April 2015 to October 2018 were enrolled. All the participants had failed antiarrhythmic drugs previously, and no thrombus was found in the left atrium before surgery. Additionally, patients who had met the following criteria were excluded from the present study: rheumatic heart valve disease, left atrial thrombus, LAD> 55 mm, uncontrolled thyroid dysfunction, congenital heart disease, liver and kidney dysfunction, blood system diseases, contraindication to anticoagulation, and malignant tumors with a life expectancy less than 1 year. The preprocedural informed consent was obtained from all the involved participants, and the study was conducted according to the Helsinki Declaration approved by the ethics committee of Northern Jiangsu People’s Hospital.
Catheter ablation procedure and postoperative follow up
The ablation procedure details had been fully described in the study published in Europace [7]. In our study, under the guidance of the three-dimensional mapping system, Ensite3000 Navx (St. Jude Medical) or CARTO system (Biosense Webster, Inc), electrical isolation of the circumferential pulmonary vein lesions was performed by well-experienced professors. Additional ablation lines of the left atrium roof should also be implemented in some patients as necessary. The endpoint of the ablation was the absence or dissociation of potentials between the pulmonary vein and left atrium. Additionally, the electrical block of the pulmonary veins was repeatedly evaluated 30 min after the initial isolation. All the patients took direct oral anticoagulants with warfarin at least 4 weeks before and 3 months after surgery, with a target international normalized ratio of 2.0–3.0. Additionally, all the patients took amiodarone hydrochloride or class IC antiarrhythmic drugs for more than 1 month after ablation. The postoperative follow-up schedules were performed at 3, 6, and 12 months after the surgery and every 6 months thereafter, or whenever they developed discomfort symptoms consistent with recurrent AF. A 48-h Holter electrocardiogram or 12-lead electrocardiogram was recorded at the outpatient follow-up visits. The blanking period was defined as the first 3 months after the AF ablation procedure. Beyond the blank period, AF recurrence referred to the detection of AF/atrial tachycardia attack with a duration >30 s, as assessed by electrocardiographic monitoring.
Data collection
The clinical data of all the patients with AF before ablation were collected and included basic demographic characteristics, disease history, AF duration, the CHA2DS2-VASc score, the HATCH score, the monocyte count and other items within the complete blood count, creatinine and uric acid, Cystatin C, D-Dimer, lipid protein profile, left atrial diameter (LAD), left ventricular ejection fraction (LVEF), and follow-up time. The monocyte/HDL ratio (MHR) was calculated as the monocyte count divided by the HDL. All the blood samples were collected 24 h before the procedure.
Statistical analysis
All the data were analyzed using SPSS software, version 20.0 for Windows (SPSS Inc., Chicago, Illinois, USA). The Kolmogorov–Smirnov criterion was used to assess normality. Continuous variables with a normal distribution were presented as the means ± standard deviation; otherwise, they were described as medians (interquartile range). The categorical variables were summarized as frequencies and percentages. Comparisons of two continuous variables with a normal distribution were carried out by independent samples Student’s t-test, whereas comparisons between two continuous variables were implemented using the Mann–Whitney U test. Categorical variables were compared using chi-squared test or Fisher’s exact test. Univariate and multivariate binary logistic regression analyses using the backward likelihood ratio method were employed to determine the risky predictors of AF recurrence. The correlations were assessed using Spearman’s rank test. Receiver operating characteristic (ROC) curve analysis was used to assess the predictive value of the risk factors to predict AF recurrence. A two-tailed P value < 0.05 was considered statistically significant.
Results
Baseline characteristics and demographical features
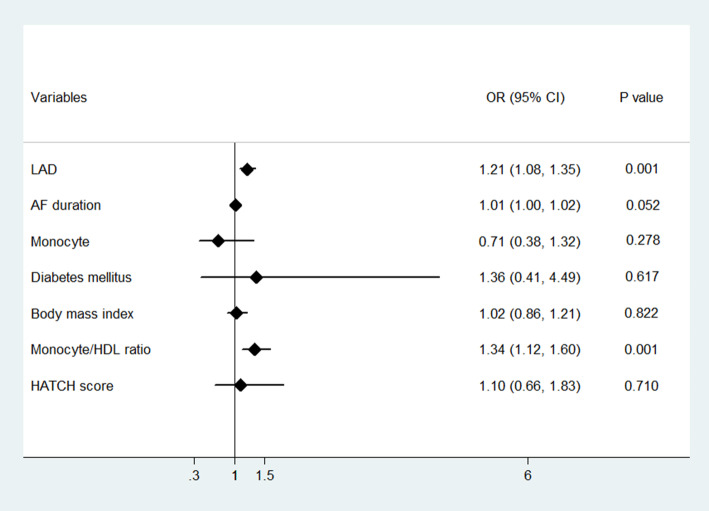
One hundred twenty-five patients with paroxysmal AF were enrolled, including 69 males and 56 females, with an average age of 61.2 ± 9.3 years. Forty-seven patients had developed late recurrence of AF during a mean follow up of 25.1 ± 12.0 months. Depending on the postoperative recurrence of AF, the patients were divided into the recurrence group and maintenance of sinus rhythm group. The baseline demographic characteristics and demographical features, laboratory, and procedural details of both cohorts are summarized in Table 1. The two groups were significantly different in terms of the AF duration, history of diabetes mellitus, body mass index, D-dimer level, monocyte count, HDL cholesterol level, monocyte/HDL ratio, and LAD (P < 0.05). Furthermore, the patients were stratified into 3 groups according to the MHR tertile (T1: < 5.68; T2: 5.68–8.29; T3:≥8.29) and subgroup analysis showed that patients in T3 had a higher rate of AF recurrence than those in T1 (22% vs. 57.1%; P < 0.05; Fig. 1). Additionally, subgroup analyses stratified by LAD tertile (T1: < 33.96 mm; T2: 33.96–38 mm; T3: > 38 mm) revealed that the rate of recurrence was significantly higher in the highest T3 group than that in the T1 and T2 groups (P < 0.05; Fig. 1).
Table 1.
Baseline characteristics and demographical features of the study population
| Variables | sinus rhythm (n = 78) | AF recurrence (n = 47) | P value |
|---|---|---|---|
| Age (years) | 61.5 (13.25) | 63.0 (15.0) | 0.717 |
| Gender (female) | 38 (48.7%) | 18 (38.3%) | 0.256 |
| Body mass index (kg/m2) | 24.7 ± 2.9 | 26.1 ± 3.1 | 0.016* |
| Hypertension | 47 (60.3%) | 34 (72.3%) | 0.171 |
| Diabetes mellitus | 9 (11.5%) | 14 (29.8%) | 0.011* |
| Coronary artery disease | 19 (24.4%) | 9 (19.1%) | 0.499 |
| Stroke | 13 (16.7%) | 8 (17.0%) | 0.959 |
| AF duration (months) | 12.0 (31.25) | 24.0 (48.0) | 0.035* |
| Procedure time (minnutes) | 240 (60.0) | 240 (119.0) | 0.969 |
| CHA2DS2-VASc score | 2.0 (2.0) | 2.0 (2.0) | 0.172 |
| HATCH score | 0.95 ± 0.89 | 1.09 ± 0.93 | 0.418 |
| Hemoglobin (g/L) | 137.9 ± 21.6 | 137.1 ± 16.2 | 0.847 |
| AST (U/L) | 21 (10.25) | 23 (8.0) | 0.578 |
| Serum creatinine (umol/L) | 83.0 ± 18.3 | 86.6 ± 19.1 | 0.301 |
| Uric acid (umol/L) | 309.3 ± 84.5 | 325.2 ± 96.4 | 0.336 |
| WBC (×109/L) | 5.40 (1.91) | 5.69 (2.35) | 0.359 |
| Monocyte (× 109/L) | 0.32 (0.13) | 0.35 (0.15) | 0.007* |
| LDL cholesterol (mmol/L) | 2.42 (1.18) | 2.36 (0.88) | 0.521 |
| HDL cholesterol (mmol/L) | 1.33 (0.54) | 1.09 (0.40) | 0.002* |
| Monocyte/HDL ratio | 6.34 (3.39) | 8.29 (4.99) | 0.000* |
| Cystatin C (mg/L) | 0.8 (0.39) | 0.8 (0.30) | 0.165 |
| D-Dimer (mg/L) | 0.27 (0.21) | 0.27 (0.14) | 0.008* |
| LAD (mm) | 34 (6.0) | 38 (6.0) | 0.000* |
| LVEF (%) | 62 (1.25) | 61 (3.0) | 0.205 |
| Follow-up duration (months) | 22 (20.25) | 19 (12.0) | 0.165 |
*P < 0.05
Fig. 1.
Percentage of the patients developing post-ablation AF recurrence stratified by tertiles of pre-ablation Monocyte/HDL ratio and LAD
Predictors of AF recurrence
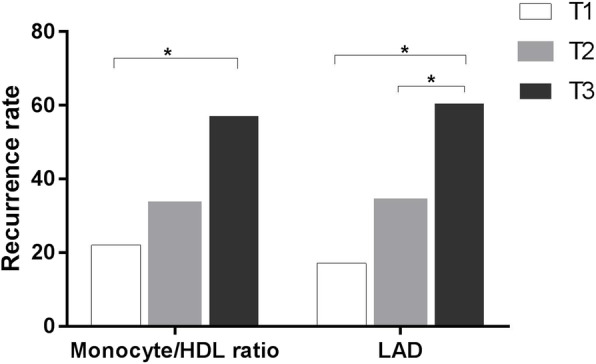
According to univariate binary logistic analysis, AF duration, history of diabetes mellitus, body mass index, monocyte count, the monocyte/HDL ratio, and the LAD were significantly associated with AF recurrence (P < 0.05). However, the CHA2DS2-VASc score, HATCH score, and D-dimer level were identical to those of the sinus rhythm (Table 2). Furthermore, we performed multivariate logistic regression analysis using the backward likelihood ratio method, and the analysis revealed that the LAD (OR = 1.21; 95% CI = 1.08 ~ 1.35; P = 0.001) and preablation MHR (OR = 1.34, 95% CI = 1.12 ~ 1.60, P = 0.001) were independent risk factors predicting the recurrence of AF after radiofrequency ablation. (Fig. 2).
Table 2.
Univariate logistic regression modeling results of the AF recurrence
| Variables | Univariate model | ||
|---|---|---|---|
| OR | 95% CI | P | |
| LAD | 1.250 | 1.125–1.389 | 0.000* |
| AF duration | 1.012 | 1.001–1.023 | 0.026* |
| Monocyte | 1.691 | 1.167–2.451 | 0.005* |
| HDL cholesterol | 0.164 | 0.049–0.543 | 0.003* |
| D-Dimer | 4.560 | 1.0–20.794 | 0.050 |
| Diabetes mellitus | 3.253 | 1.278–8.281 | 0.013* |
| Body mass index | 1.166 | 1.026–1.326 | 0.019* |
| CHA2DS2-VASc score | 1.214 | 0.924–1.597 | 0.164 |
| HATCH score | 1.180 | 0.793–1.755 | 0.415 |
| Monocyte/HDL ratio | 1.377 | 1.176–1.614 | 0.000* |
*P < 0.05
Fig. 2.
Forest plot of multivariate logistic regression modeling results of the AF recurrence after ablation
Predictive value of risk factors
The predictive value of risk factors to predict the recurrence of AF after ablation was evaluated by ROC analysis. The areas under the curve (AUC) of the MHR and LAD were 0.712 (95% CI = 0.618 ~ 0.806; P = 0.000) and 0.739 (95% CI = 0.653 ~ 0.814 P = 0.000), respectively (Fig. 3). Furthermore, Z-test showed no significant difference between the MHR and LAD concerning AUC (Z = 0.451; P = 0.652).
Fig. 3.
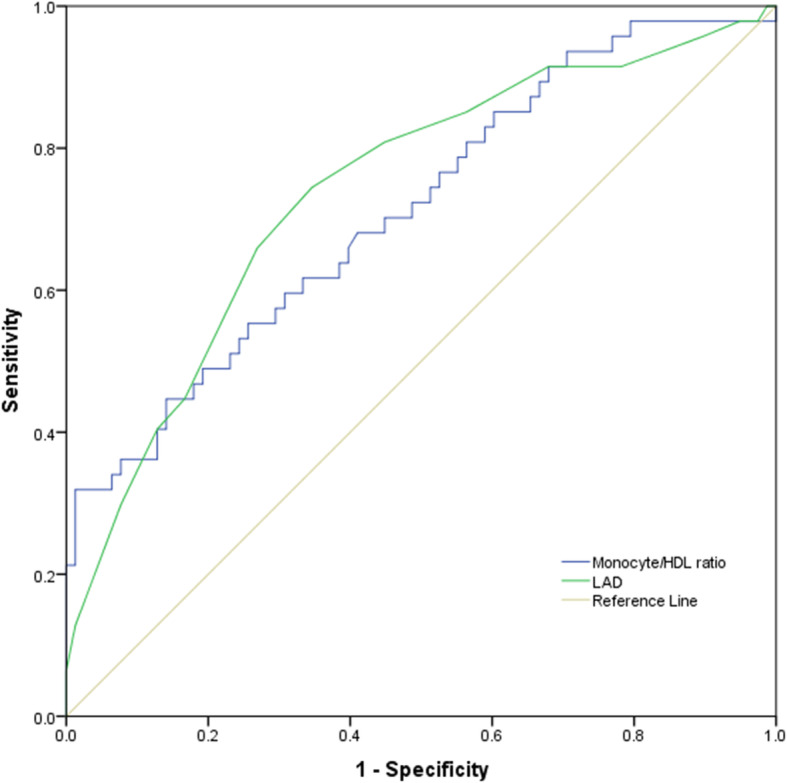
Receiver operating characteristic curve of pre-ablation variables for predicting AF recurrence after ablation
Additionally, correlation analysis revealed a positive correlation of the MHR with the LAD (r = 0.229; P = 0.01; Fig. 4).
Fig. 4.

Correlation of the preablation monocyte/HDL ratio with LAD (r = 0.229, P = 0.01)
Discussion
In our retrospective study, we focused more on the relationship between the preprocedural MHR and development of AF recurrence after radiofrequency ablation. The clinical data of 125 patients of paroxysmal AF treated by circumferential pulmonary vein electrical isolation with an average follow-up time of 25.1 ± 12.0 months was systematically reviewed. We found that the preablation LAD and MHR were risk factors affecting the therapeutic effect of radiofrequency ablation. Additionally, we had demonstrated that the MHR along with LAD is an independent prognostic factor of AF recurrence in patients with paroxysmal AF who had undergone a single catheter ablation procedure.
AF is the most common atrial arrhythmia in clinical practice, which seriously affects the quality of life of patients and may cause some serious complications, such as heart failure and stroke. Presently, radiofrequency catheter ablation is an effective methods to treat AF. The success rate of the radiofrequency ablation of paroxysmal AF is between 70 and 80% in 1 year [8] However, some patients will develop relapse of AF after ablation. Many factors, including the AF duration, LAD, and left ventricular dysfunction, have been reported to be related to the recurrence of AF after radiofrequency ablation. The pathophysiological mechanism of AF has not been clearly revealed yet, and many underlying mechanisms participate in the recurrence and maintenance of AF. In recent years, emerging of evidence has revealed that the cross-linked process of inflammation and oxidative stress may result in atrial fibrosis, which is probably the main constituents of AF pathophysiology [9–11] and may play a role in substrate modification by electrical and structural remodeling of the atrium, consequently increasing the susceptibility of AF [12]. Compared with patients with sinus rhythm, the levels of the markers of inflammation and oxidative stress, such as C-reactive protein and interleukin-6, in patients with AF were significantly increased [13]. Inflammation and oxidative stress promote the occurrence of AF, while inhibition of the inflammatory response could reduce the risk of AF. A meta-analysis of 50 randomized controlled studies [14] revealed that the prophylactic use of corticosteroids to inhibit the inflammatory response significantly reduced the incidence of postoperative AF in 3323 patients who had undergone cardiac surgery.
As a typical inflammatory cell, monocytes mediate the process of inflammation and oxidative stress by binding to adhesion molecules expressed on damaged vascular endothelial cells and inducing the production of various cytokines as well as play an important role in chronic cardiovascular diseases [15]. However, HDL cholesterol could reduce the expression of CD11b and other adhesion molecules on monocytes and damaged endothelial cells, inhibiting the activation and proliferation of monocytes and thus exerting both anti-inflammatory and antioxidant effects [16]. Recently, the combined circulating monocyte count and serum HDL cholesterol in one fraction, termed ‘MHR’, was found to be associated with a poor cardiovascular prognosis and emerged as an independent predictor of major cardiovascular events in patients with chronic kidney disease [5]. As a quantitative index of inflammation and oxidative stress, MHR reflects the degree of inflammation and oxidative stress to a certain extent and was found to not only be a predictor of cardiovascular diseases in patients with chronic obstructive pulmonary disease [17] but also to have a certain value in predicting the occurrence of AF after coronary artery bypass grafting (CABG) [18]. The study included 311 patients who had undergone CABG, and 71 patients developed AF after surgery. The MHR in the group with AF was significantly higher than that of the control group. Additionally, the MHR had also been found as an independent risk factor for AF recurrence after cryoballoon-based catheter ablation. Canpolat et al. [6] enrolled 402 patients who had undergone ablation, and a high MHR before surgery could predict AF recurrence after a mean follow-up time of 20.6 ± 6.0 months. In our present study, the increased MHR along with the LAD before radiofrequency ablation is a strong and independent predictor of AF recurrence during the follow up. In clinical practice, we could evaluate the recurrence risk of AF using the preoperative LAD and MHR to select appropriate patients for the procedure, reduce unnecessary interventions and early identify high-risk patients with recurrence, and provide corresponding strengthening intervention measures, to improve the long-term prognosis of the patients. Additionally, the MHR showed the same value of predicting AF recurrence as the LAD, which has been widely accepted as a risk factor for AF recurrence after ablation [19]. Additionally, the MHR was positively correlated with the LAD.
Limitations
This study is a single-center retrospective study, and the conclusion needs to be further explored by multiple centers. Additionally, the sample size of this study is relatively small, and the postoperative follow-up time is limited. Moreover, the recurrence of asymptomatic AF may be ignored in the follow-up process, contributing to a certain bias in the detection of the postoperative recurrence of AF.
Conclusion
In our study, we observed that the elevated preablation MHR was associated with an increased risk of the postoperative recurrence of AF. Additionally, the MHR independently predicted the late recurrence of paroxysmal AF after radiofrequency ablation, with the same predictive value as the LAD.
Acknowledgements
The authors would like to appreciate the assistance of Dr. Ye Zhu, Dr. Yi Zhang, for their valuable advices on the management of the patients. We thank the editor and the reviewers whose comments/suggestions helped improve and clarify this manuscript.
Abbreviations
- MHR
Monocyte/HDL ratio
- AF
Atrial fibrillation
- LAD
Left atrial diameter
- ROC
Receiver operating characteristic curve
- CI
Confidence interval
- AUC
Area under the curve
- LVEF
Left ventricular ejection fraction
- CABG
Coronary artery bypass grafting
Authors’ contributions
SAC and MMZ: Conceptualization, Investigation, Data curation, Methodology, Formalanalysis, Validation, Writing-original draft, SAC and MMZ contributed equally to this work. MFZ, FL, LS, ZYB, FKC and HXL were involved in gathering the clinical data and editing and revision of the manuscript. XG: Conceptualization, Methodology, Validation, Formal analysis. All the authors were involved in the draft, revision and approval of the final version.
Funding
This work was supported by funds from science and technology department of Jiangsu province, China (No. BL2013022). Funding is mainly used for chronic follow-up and paper publication.
Availability of data and materials
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
Informed consent were obtained from all involved participants and the study was performed in accordance with the Declaration of Helsinki and approved by the institutionalethical board of Northern Jiangsu Province People’s Hospital, Jiangsu Province, China.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
She-an Chen, Email: dlykdxcsa@163.com.
Man-man Zhang, Email: 709266431@qq.com.
Meifang Zheng, Email: 794998553@qq.com.
Fei Liu, Email: liufei19871013@163.com.
Lei Sun, Email: geyinxin@163.com.
Zheng-yu Bao, Email: 15651055520@163.com.
Fu-kun Chen, Email: cfk0722@126.com.
Hong-xiao Li, Email: lhxlmt@126.com.
Xiang Gu, Email: guxiang@yzu.edu.cn.
References
- 1.Pistoia F, Sacco S, Tiseo C, et al. The epidemiology of atrial fibrillation and stroke. Cardiol Clin. 2016;34(2):255–268. doi: 10.1016/j.ccl.2015.12.002. [DOI] [PubMed] [Google Scholar]
- 2.Rottner L, Bellmann B, Lin T, et al. Catheter ablation of atrial fibrillation: state of the art and future perspectives. Cardiol Ther. 2020;9(1):45–58. doi: 10.1007/s40119-019-00158-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Calkins H, Hindricks G, Cappato R, et al. 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation: executive summary. Europace. 2018;20(1):157–208. doi: 10.1093/europace/eux275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Acikgoz SK, Acikgoz E, Sensoy B, et al. Monocyte to high-density lipoprotein cholesterol ratio is predictive of in-hospital and five-year mortality in ST-segment elevation myocardial infarction. Cardiol J. 2016;23(5):505–512. doi: 10.5603/CJ.a2016.0026. [DOI] [PubMed] [Google Scholar]
- 5.Kanbay M, Solak Y, Unal HU, et al. Monocyte count/HDL cholesterol ratio and cardiovascular events in patients with chronic kidney disease. Int Urol Nephrol. 2014;46(8):1619–1625. doi: 10.1007/s11255-014-0730-1. [DOI] [PubMed] [Google Scholar]
- 6.Canpolat U, Aytemir K, Yorgun H, et al. The role of preprocedural monocyte-to-high-density lipoprotein ratio in prediction of atrial fibrillation recurrence after cryoballoon-based catheter ablation. Europace. 2015;17(12):1807–1815. doi: 10.1093/europace/euu291. [DOI] [PubMed] [Google Scholar]
- 7.Efremidis M, Letsas K, Giannopoulos G, et al. Early pulmonary vein reconnection as a predictor of left atrial ablation outcomes for paroxysmal atrial fibrillation. Europace. 2015;17(5):741–746. doi: 10.1093/europace/euu216. [DOI] [PubMed] [Google Scholar]
- 8.Haegeli LM, Calkins H. Catheter ablation of atrial fibrillation: an update. Eur Heart J. 2014;35(36):2454–2459. doi: 10.1093/eurheartj/ehu291. [DOI] [PubMed] [Google Scholar]
- 9.Harada M, Van Wagoner DR, Nattel S. Role of inflammation in atrial fibrillation pathophysiology and management. Circ J. 2015;79(3):495–502. 10.1253/circj.CJ-15-0138. [DOI] [PMC free article] [PubMed]
- 10.Hu YF, Chen YJ, Lin YJ, et al. Inflammation and the pathogenesis of atrial fibrillation. Nat Rev CardiolNat Rev Cardiol. 2015;12(4):230–243. doi: 10.1038/nrcardio.2015.2. [DOI] [PubMed] [Google Scholar]
- 11.Li J, Solus J, Chen Q, et al. Role of inflammation and oxidative stress in atrial fibrillation. Heart Rhythm. 2010;7(4):438–444. doi: 10.1016/j.hrthm.2009.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Frustaci A, Chimenti C, Bellocci F, et al. Histological substrate of atrial biopsies in patients with lone atrial fibrillation. Circulation. 1997;96(4):1180–1184. doi: 10.1161/01.cir.96.4.1180. [DOI] [PubMed] [Google Scholar]
- 13.Psychari SN, Apostolou TS, Sinos L, et al. Relation of elevated C-reactive protein and interleukin-6 levels to left atrial size and duration of episodes in patients with atrial fibrillation. Am J Cardiol. 2005;95(6):764–767. doi: 10.1016/j.amjcard.2004.11.032. [DOI] [PubMed] [Google Scholar]
- 14.Ho KM, Tan JA. Benefits and risks of corticosteroid prophylaxis in adult cardiac surgery: a dose-response meta-analysis. Circulation. 2009;119(14):1853–1866. doi: 10.1161/circulationaha.108.848218. [DOI] [PubMed] [Google Scholar]
- 15.Shahid F, Lip GYH, Shantsila E. Role of monocytes in heart failure and atrial fibrillation. J Am Heart Assoc. 2018;7(3):1. doi: 10.1161/jaha.117.007849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barter PJ, Nicholls S, Rye KA, et al. Antiinflammatory properties of HDL. Circ ResCirc Res. 2004;95(8):764–772. doi: 10.1161/01.res.0000146094.59640.13. [DOI] [PubMed] [Google Scholar]
- 17.Yakar HI, Kanbay A. Could monocyte level/HDL cholesterol ratio predict cardiovascular diseases in patients with COPD? Niger J Clin PractNiger J Clin Pract. 2020;23(4):450–455. doi: 10.4103/njcp.njcp_54_19. [DOI] [PubMed] [Google Scholar]
- 18.Tekkesin AI, Hayiroglu MI, Zehir R, et al. The use of monocyte to HDL ratio to predict postoperative atrial fibrillation after aortocoronary bypass graft surgery. North Clin Istanb. 2017;4(2):145–150. doi: 10.14744/nci.2017.53315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liao YC, Liao JN, Lo LW, et al. Left atrial size and left ventricular end-systolic dimension predict the progression of paroxysmal atrial fibrillation after catheter ablation. J Cardiovasc Electrophysiol. 2017;28(1):23–30. doi: 10.1111/jce.13115. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets analyzed during the current study are available from the corresponding author on reasonable request.