Abstract
Purpose
This scoping review evaluated the currently available data related to abdominal imaging in the SARS-CoV-2 infection.
Method
A systematic review of MEDLINE, EMBASE, SCOPUS, and Web of Science was performed from inception to July 15, 2020 using PRISMA-ScR guidelines. The review included case reports and series discussing radiologic manifestations of SARS-CoV-2 infection in abdominal imaging studies. Studies published from inception to March 31, 2020, were independently screened and reviewed by one author, and another author reviewed studies published after March 31 to July 15, 2020. Study screening and full-text review for publications before March 31, 2020, was performed by one author, and another author for publications after March 31 to July 15, 2020.
Results
Thirty-six studies were included in qualitative synthesis. The prevalence of gastrointestinal symptoms is roughly 18% and includes loss of appetite, nausea, vomiting, diarrhea, and abdominal pain. Sixteen percent of COVID-19 cases may only present with gastrointestinal symptoms. Many patients presenting this way demonstrate evidence of COVID-19 incidentally through abdominal CT imaging at the lung bases. Studies published to date have also reported abdominal imaging findings including small and large bowel wall thickening, fluid-filled colon, pneumatosis intestinalis, pneumoperitoneum, intussusception, and ascites.
Conclusion
Gastrointestinal manifestations and imaging manifestations of SARS-CoV-2 infection are increasingly reported and warrant specific attention during abdominal imaging.
Electronic supplementary material
The online version of this article (10.1007/s00261-020-02739-5) contains supplementary material, which is available to authorized users.
Keywords: 2019-nCoV, SARS-CoV-2, COVID-19, Gastrointestinal, Abdomen, Imaging
Introduction
Nearly 17 million people have been infected with the coronavirus disease (COVID-19) as of July 29, 2020, and more than 660,000 people have died [1]. The most common COVID-19 symptoms include fever (91%), cough (67%), fatigue (51%), and dyspnea (30%) [2]. However, gastrointestinal (GI) symptoms have been increasingly recognized in these patients [3–6] and were likely under-reported in early studies [7]. Some COVID-19 patients have presented only with GI symptoms at initial presentation, or even in the complete absence of respiratory symptoms in some cases [8, 9]. While there is strong evidence that the digestive system can be infected by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [10, 11], there has been less focus on the effects of SARS-CoV-2 on extra-pulmonary systems. Few studies have identified the potential abdominal imaging features of these symptoms [12]. This scoping review aims to discuss the current literature on the imaging features in the abdomen in COVID-19, as well as the relevant clinical manifestations of these image findings.
Methods
This scoping review used the 22-item Preferred Reporting Items for Systematic Review and Meta-Analysis – Scoping Review (PRISMA-ScR) for guidance [13, 14]. A pre-registered protocol was not submitted prior to review.
Literature Search and Selection Criteria
MEDLINE, EMBASE, Scopus, and Web of Science databases were searched for eligible publications from inception to July 15, 2020. Variations of “COVID-19” AND “GASTROINTESTINAL” AND “IMAGING”-related title/abstract/keywords or medical subject heading terms were performed with individual search strategies outlined in Appendix 1–4. No language restrictions were applied and language translation was performed when required. Search results were combined from each database and duplicates were removed using RefWorks. Titles and abstracts were screened for relevance, and full-text review for potentially relevant articles was then performed. To be included in the review, papers needed to address abdominal imaging findings in COVID-19-positive patients. Studies involving animal subjects were excluded. Publications from inception to March 31, 2020, were reviewed by MPW, while articles published between March 31 and July 15, 2020 were reviewed by KL. Given the broad scope of this review, a charting form was not established at the start, but one was developed after full-text review. Publications of unclear relevance were resolved by discussion and consensus between KL and MPW. Reference lists from included studies were screened to identify additional articles of interest. Forward searching of included studies was performed in Google Scholar. Ethics approval was not necessary for this review.
Results
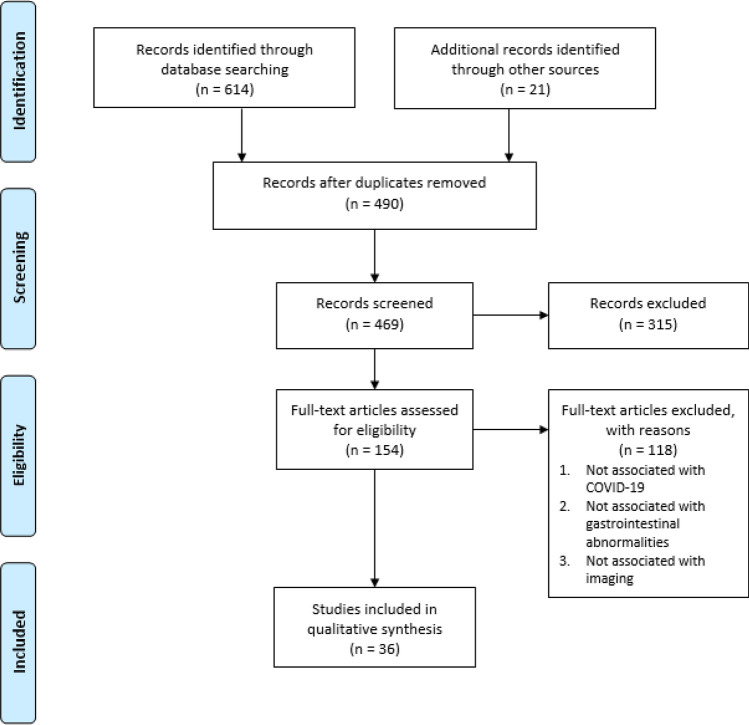
A total of 469 articles were identified from the database search after duplicate removal. After title and abstract screening, 137 articles were identified for full-text review. In addition to studies found from included article reference lists and manual searches, 36 articles were included in qualitative synthesis. The PRISMA flow diagram is shown in Fig. 1.
Fig. 1.
PRISMA flow diagram of the included studies on abdominal imaging findings in patients with SARS-CoV-2 infection. Flow diagram adapted from [14]
Incidental COVID-19 findings based on abdominal computed tomography (CT) indicated by gastrointestinal symptoms
A wide range of GI symptoms have been reported in patients with COVID-19. A multicenter study by Pan et al. found that more than 50% of their 204 patients reported digestive symptoms including lack of appetite, diarrhea, vomiting, and abdominal pain [15]. A recent meta-analysis of 4234 patients found the prevalence of GI symptoms to be 17.6% [16]. Three case reports included hematochezia as a symptom [17–19]. There are also several case reports that describe patients that present with only GI symptoms initially or throughout the course of their entire infection [20–24]. The largest study, a single-center study by Luo et al. found that of 1141 confirmed cases of COVID-19, 16% presented with only GI symptoms [25]. Additionally, many cases of COVID-19 have been found incidentally through abdominal imaging scans indicated by patients presenting mainly or only with GI symptoms [20, 21, 26–29]. Hossain et al found that more than 50% of their 119 patients first demonstrated evidence of COVID-19 incidentally through either an abdominal or cervical spine/neck CT [30]. Some authors now recommend radiologists to carefully review abdominal CT scans for typical COVID-19 findings at the lung bases [31, 32].
Abnormal abdominal imaging findings
Twenty-one studies have now investigated abnormal abdominal imaging findings in patients tested positive for SARS-CoV-2. A summary of findings are shown in Table 1. Ten studies of 23 patients (2 of which are pediatric cases) demonstrate thickening of various regions of the small and large bowel wall [17, 18, 28, 33–39]. Hyperemia and mesenteric thickening have also been observed in tandem with bowel wall thickening. Different mechanisms have been postulated for the cause of thickening in these cases. Such causes include the SARS-CoV-2 infection of bowel epithelia leading to cytokine storm and inflammation, edema, or ischemia indicated by the presence of fibrin clots.
Table 1.
Characteristics and findings of included studies of patients with abnormal abdominal radiologic features
| Studies | N | Age | Gender | Symptoms | Imaging Modality | Abdominal imaging features | Additional information |
|---|---|---|---|---|---|---|---|
| Bhayana et al. | 42 | 18–90 years | NR | Diarrhea, abdominal pain, nausea, vomiting, loss of appetite | CT |
7—colic or rectal thickening 5—small bowel thickening 4—pneumatosis or PV gas 1—perforation |
Suspect thickening is due to ischemia caused by thromboembolic events based on presence of fibrin thrombi |
| Hellinger et al. | 1 | 64 years | NR | Abdominal pain, nausea, vomiting, diarrhea, fever | CT | Thickening of small bowel and hyperemia | Suspect radiologic findings are due to SARS-CoV-2 infection of bowel wall, causing mucosal inflammation |
| Kim et al. | 1 | 42 years | Male | Abdominal, testicular and back pain | CT | Thickening of distal descending and sigmoid colon (colitis) | N/A |
| Sattar et al. | 1 | 38 years | Male | Fever, chills, myalgia, dyspnea, abdominal pain, diarrhea | CT | Thickening of ascending, transverse, descending and sigmoid colon and rectum | Suspect thickening is due to inflammation |
| Sattar et al. | 1 | 74 years | Male | Dry cough, abdominal pain | CT | Thickening of proximal transverse colon | Suspect thickening is due to inflammation |
| Sattar et al. | 1 | 55 years | Male | Fever, cough, nausea, constipation, abdominal pain | CT | Colonic ileus and air in bowel wall | |
| Guo et al. | 1 | 29 years | Male | Fever, diarrhea | CT | Mesenteric thickening with segmental wall swelling of jejunum | Suspect thickening is due to viral infection of intestinal mucosa |
| Tang et al. | 1 | 24 years | Male | Abdominal pain, diarrhea, cough, running nose | CT | Thickening of distal, ascending transverse and descending colon | Thickening identified as edema |
| Carvalho et al. | 1 | 71 years | Female | Abdominal pain, bloody diarrhea, nausea, vomiting, anorexia, distention | CT | Thickening of ascending, transverse, descending, and sigmoid colon | Ruling out other causes of hemorrhagic colitis, authors suggest SARS-CoV-2 GI infection was cause of hemorrhagic colitis |
| Jaijakul et al | 1 | 56 years | Male | Fever, dyspnea, nausea, vomiting, abdominal pain, bloody bowel movements | CT | Thickening of ascending, transverse, and descending colon | Suspect thickening is due to viral infection of gastrointestinal epithelia |
| Calinescu et al. | 2 | 10–13 years | NR | Abdominal pain, fever, vomiting | CT | Ileo-colitis | Suspect thickening is due to cytokine storm inflammation |
| Qiu et al. | 1 | 56 years | Female | Abdominal pain, fever, diarrhea | CT | Right colonic mural thickening | |
| Kielty et al. | 1 | 47 years | Male | Fever, dry cough, vomiting | CT | Pneumatosis of jejunum, proximal ileum, and caecum. Also mural thickening and portal venous gas | |
| Meini et al. | 1 | 44 years | Male | Fever, cough, chest pain | CT | Pneumatosis of caecum and right colon | |
| Di Grezia et al. | 3 | NR | NR | NR | NR | Pneumatosis* | |
| Correa Neto et al | 1 | 80 years | Female | Dry persistent cough, fever, dyspnea | CT | Extensive pneumoperitoneum with free intracavitary fluid | Bowel perforation found later with laparotomy |
| Cai et al. | 1 | 10 months | Female | paroxysmal crying, restlessness, vomiting, currant jelly-like stool | Doppler Ultrasound |
Large amount of abdominal dropsy (edema) Intussusception* |
|
| Martinez-Castano et al. | 1 | 6 months | Male | Vomiting, abdominal cramps, currant jelly stools | Ultrasound | Swirled pattern consisting of alternating hyperechogenicity with hypoechogenicity typical of ileocolic intussusception | |
| Rajalakshmi et al. | 1 | 8 months | Male | Fever, vomiting, bloody stool | Ultrasound | Ileocolic intussusception in subxiphoid region | Suggested cause is mucosal inflammatory changes |
| Moazzam et al. | 1 | 4 months | Male | Abdominal pain, reluctance to feed, drawing up of legs towards abdomen, inconsolable crying, rectal bleeding (currant jelly stool) | Ultrasound | Intussusception of bowel loop in right upper quadrant of abdomen | |
| Lu et al. | 1 | 10 months | NR | NR | NR | Intussusception* | |
| Culver et al. | 1 | 71 years | Male | Acute, severe upper GI bleeding | Ultrasound | 6L ascites | Ascitic fluid tested positive for SARS-CoV-2 RNA |
| Behzad et al. | 1 | 31 years | Male | Abdominal discomfort and absent bowel movement | CT and radiograph |
CT—Nonspecific stranding surrounding mildly distended fluid-filled ascending colon Radiograph—ileus pattern |
CT computed tomography, NR not reported
*Condition mentioned but not reported as radiologic finding
Pneumatosis or portal vein gas has been reported on abdominal CT in 6 patients [33, 40, 41]. An additional 3 patients were reported to have pneumatosis though the diagnostic modality used is not reported [42]. The presence of pneumatosis was reported in various regions of the GI tract, including the jejunum, ileum, caecum, and right colon.
There has been one case report of abdominal CT demonstrating extensive pneumoperitoneum with free intracavitary fluid [43]. Subsequent laparotomy revealed the cause to be perforation of the sigmoid colon accompanied by reduced perfusion of the entire GI tract. The authors suggest this perforation to be the result of septic and thromboembolic phenomena, caused by the viral infection.
A rare ultrasound finding reported in pediatric cases of SARS-CoV-2 infection is ileocolic intussusception. Three separate cases have reported this imaging finding [44–46]. Another two SARS-CoV-2-positive patients have been reported to have intussusception, though it is not known if their condition was identified through imaging modalities [47, 48].
One case report involved a patient with colonic ileus and air in bowel wall on abdominal CT [35]. Behzad et al similarly reported a patient that showed ileus pattern on abdominal radiograph, along with nonspecific stranding surrounding mildly distended fluid-filled ascending colon [49]. Lastly, there has been one case of ascites found on ultrasound in a SARS-CoV-2 patient [50]. Drainage yielded 6L of fluid, and the fluid sample was tested positive for SARS-CoV-2 RNA. The authors suggest that ascites infection may involve infection of ACE2 expressing cells of the esophageal epithelial cells and absorptive enterocytes [3].
Discussion
This scoping review identified 36 primary studies addressing the GI symptoms and radiologic manifestations of SARS-CoV-2 infection of the GI system. On imaging, typical GI findings have included nonspecific small and large bowel wall thickening and liquid stool throughout the bowel. Other more rare presentations such as pneumatosis intestinalis, pneumoperitoneum, and large volume ascites have also been reported. Additionally, the more typically described lung parenchymal findings have also been seen incidentally in the periphery of cross-sectional abdominal imaging. This review highlights features which can cue imaging experts to consider COVID-19 and evaluate for other features which may lead to a COVID-19 diagnosis, particularly in patients with few or no typical COVID-19 symptoms.
This scoping review is subject to some limitations. Given the broad scope of this review and the lack of detailed exclusion criteria, some imaging features may have been potentially missed. Additionally, this review may have missed relevant studies by not utilizing other search databases and exclusion of the gray literature. Furthermore, the lack of early recognition of GI symptoms [7] may limit the available literature in terms of imaging investigations indicated by GI symptoms. Investigating abdominal imaging abnormalities in COVID-19 cases presenting with both respiratory and GI symptoms may be a topic for future investigations.
Conclusion
Gastrointestinal manifestations of COVID-19 have been increasingly recognized. Although rare, imaging features have included bowel wall thickening, fluid-filled colon, pneumatosis, pneumoperitoneum, intussusception, and ascites. Identifying these features on abdominal imaging highlight the need to consider and evaluate for other manifestations of COVID-19 such as lung parenchymal findings. In the appropriate setting, COVID-19 can be raised as a consideration, particularly in patients presenting with atypical symptoms.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Abbreviation
- SARS-Cov-2
Severe acute respiratory syndrome coronavirus 2
- COVID-19
Coronavirus disease 2019
- ACE2
Angiotensin-converting enzyme 2
- GI
Gastrointestinal
Funding
Studentship funding for this scoping review was provided through an Office of the Provost and VP (Academic) Summer Student award from University of Alberta Faculty of Medicine and Dentistry, and through the Radiology Endowment Fund from the University of Alberta Department of Radiology and Diagnostic Imaging.
Compliance with ethical standards
Conflicts of interest
The authors have no relevant conflicts of interest to declare.
Ethics approval
The study is exempt from ethical approval at our institution as all reviewed publications included anonymized data and have acquired appropriate institutional ethical approval where necessary.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Kevin Lui, Email: kslui@ualberta.ca.
Mitchell P. Wilson, Email: mitch.wilson@ualberta.ca
Gavin Low, Email: timgy@yahoo.com.
References
- 1.Johns Hopkins Corona Virus Resource Center (2020) Maps and Trends. https://coronavirus.jhu.edu/map.html
- 2.Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, Ji R, Wang H, Wang Y, Zhou Y. Prevalence of comorbidities in the novel Wuhan coronavirus (COVID-19) infection: a systematic review and meta-analysis. Int J: Infect Dis. 2020;94:91–95. doi: 10.1016/j.ijid.2020.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tian Y, Rong L, Nian W, He Y. Review article: gastrointestinal features in COVID-19 and the possibility of faecal transmission. Alimentary pharmacology & therapeutics. 2020;51:843–851. doi: 10.1111/apt.15731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jin X, Lian J, Hu J, Gao J, Zheng L, Zhang Y, Hao S, Jia H, Cai H, Zhang X, Yu G, Xu K, Wang X, Gu J, Zhang S, Ye C, Jin C, Lu Y, Yu X, Yu X, Huang J, Xu K, Ni Q, Yu C, Zhu B, Li Y, Liu J, Zhao H, Zhang X, Yu L, Guo Y, Su J, Tao J, Lang G, Wu X, Wu W, Qv T, Xiang D, Yi P, Shi D, Chen Y, Ren Y, Qiu Y, Li L, Sheng J, Yang Y. Epidemiological, clinical and virological characteristics of 74 cases of coronavirus-infected disease 2019 (COVID-19) with gastrointestinal symptoms. Gut. 2020;69:1002–1009. doi: 10.1136/gutjnl-2020-320926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wong SH, Lui RN, Sung JJ. Covid-19 and the digestive system. Journal of gastroenterology and hepatology. 2020;35:744–748. doi: 10.1111/jgh.15047. [DOI] [PubMed] [Google Scholar]
- 6.Zhou Z, Zhao N, Shu Y, Han S, Chen B, Shu X. Effect of gastrointestinal symptoms on patients infected with COVID-19. Gastroenterology. 2020;158:2294–2297. doi: 10.1053/j.gastro.2020.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liang W, Feng Z, Rao S, Xiao C, Xue X, Lin Z, Zhang Q, Qi W. Diarrhoea may be underestimated: a missing link in 2019 novel coronavirus. Gut. 2020;69:1141–1143. doi: 10.1136/gutjnl-2020-320832. [DOI] [PubMed] [Google Scholar]
- 8.An P, Chen H, Jiang X, Su J, Xiao Y, Ding Y, Ren H, Ji M, Chen Y, Chen W (2020) Clinical features of 2019 novel coronavirus pneumonia presented gastrointestinal symptoms but without fever onset. Lancet Epub ahead of print
- 9.Collaborative C. Global guidance for surgical care during the COVID-19 pandemic. Br. J. Surg. 2020 doi: 10.1002/bjs.11646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hindson J. COVID-19: faecal–oral transmission? Nature Reviews Gastroenterology & Hepatology. 2020;17:259. doi: 10.1038/s41575-020-0295-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang H, Kang Z, Gong H, Xu D, Wang J, Li Z, Li Z, Cui X, Xiao J, Zhan J, Meng T, Zhou W, Liu J, Xu H. Digestive system is a potential route of COVID-19: an analysis of single-cell coexpression pattern of key proteins in viral entry process. Gut. 2020;69:1010–1018. doi: 10.1136/gutjnl-2020-320953. [DOI] [Google Scholar]
- 12.Wilson MP, Katlariwala P, Low G. Potential implications of novel coronavirus disease (COVID-19) related gastrointestinal symptoms for abdominal imaging. Radiography. 2020;26:274. doi: 10.1016/j.radi.2020.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, Moher D, Peters MDJ, Horsley T, Weeks L, Hempel S, Akl EA, Chang C, McGowan J, Stewart L, Hartling L, Aldcroft A, Wilson MG, Garritty C, Lewin S, Godfrey CM, Macdonald MT, Langlois EV, Soares-Weiser K, Moriarty J, Clifford T, Tunçalp Ö, Straus SE. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Annals of internal medicine. 2018;169:467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 14.Moher D, Liberati A, Tetzlaff J, Altman DG, The PG. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLOS Medicine. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pan L, Mu M, Yang P, Sun Y, Wang R, Yan J, Li P, Hu B, Wang J, Hu C, Jin Y, Niu X, Ping R, Du Y, Li T, Xu G, Hu Q, Tu L. Clinical Characteristics of COVID-19 Patients With Digestive Symptoms in Hubei, China: A Descriptive, Cross-Sectional, Multicenter Study. The American journal of gastroenterology. 2020;115:766–773. doi: 10.14309/ajg.0000000000000620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cheung KS, Hung IFN, Chan PPY, Lung KC, Tso E, Liu R, Ng YY, Chu MY, Chung TWH, Tam AR, Yip CCY, Leung K, Fung AY, Zhang RR, Lin Y, Cheng HM, Zhang AJX, To KKW, Chan K, Yuen K, Leung WK. Gastrointestinal Manifestations of SARS-CoV-2 Infection and Virus Load in Fecal Samples From a Hong Kong Cohort: Systematic Review and Meta-analysis. Gastroenterology. 2020;159:81–95. doi: 10.1053/j.gastro.2020.03.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jaijakul S. Colitis as a Sole Presentation of SARS-CoV-2 Infection: Case Report. SN Comprehensive Clinical Medicine. 2020;2:879–881. doi: 10.1007/s42399-020-00346-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Carvalho A, Alqusairi R, Adams A, Paul M, Kothari N, Peters S, DeBenedet AT. SARS-CoV-2 Gastrointestinal Infection Causing Hemorrhagic Colitis: Implications for Detection and Transmission of COVID-19 Disease. American Journal of Gastroenterology. 2020;115:942–946. doi: 10.14309/ajg.0000000000000667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guotao L, Xingpeng Z, Zhihui D, Huirui W. SARS-CoV-2 infection presenting with hematochezia. Medecine et Maladies Infectieuses. 2020;50:293–296. doi: 10.1016/j.medmal.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pazgan-Simon M, Rorat M, Buczynska I, Zinczuk A, Simon K. Gastrointestinal symptoms as the first, atypical indication of severe acute respiratory syndrome coronavirus 2 infection. Polish Archives Of Internal Medicine. 2020;130:338–339. doi: 10.20452/pamw.15278. [DOI] [PubMed] [Google Scholar]
- 21.Xiao N, Abboud S, McCarthy DM, Parekh N. Incidentally discovered COVID-19 in low-suspicion patients-a threat to front line health care workers. Emergency Radiology. 2020 doi: 10.1007/s10140-020-01792-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yang X, Zhao J, Yan Q, Zhang S, Wang Y, Li Y. A case of COVID-19 patient with the diarrhea as initial symptom and literature review. Clinics and Research in Hepatology and Gastroenterology. 2020 doi: 10.1016/j.clinre.2020.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gahide G, Frandon J, Vendrell JF. COVID-19 patients presenting with afebrile acute abdominal pain. ClinMed. 2020;20:e4–6. doi: 10.7861/clinmed.2020-0150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guan W, Ni Z, Hu Y, Liang W, Ou C, He J, Liu L, Shan H, Lei C, Hui DSC, Du B, Li L, Zeng G, Yuen K, Chen R, Tang C, Wang T, Chen P, Xiang J, Li S, Wang J, Liang Z, Peng Y, Wei L, Liu Y, Hu Y, Peng P, Wang J, Liu J, Chen Z, Li G, Zheng Z, Qiu S, Luo J, Ye C, Zhu S, Zhong N. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Luo S, Zhang X, Xu H. Don’t Overlook Digestive Symptoms in Patients With 2019 Novel Coronavirus Disease (COVID-19) Clinical Gastroenterology and Hepatology. 2020;18:1636–1637. doi: 10.1016/j.cgh.2020.03.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sendi AA, Saggat DF, Alzahrani SJ. Incidental typical COVID-19 appearance on the lung bases, visualized at abdominal CT for a patient that presented with abdominal pain and nausea. Radiol. Case Rep. 2020;15:1238–1241. doi: 10.1016/j.radcr.2020.05.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Siegel A, Chang PJ, Jarou ZJ, Paushter DM, Harmath CB, Arevalo JB, Dachman A. Lung Base Findings of Coronavirus Disease (COVID-19) on Abdominal CT in Patients With Predominant Gastrointestinal Symptoms. American Journal of Roentgenology. 2020 doi: 10.2214/AJR.20.23232. [DOI] [PubMed] [Google Scholar]
- 28.Kim J, Thomsen T, Sell N, Goldsmith AJ. Abdominal and testicular pain: An atypical presentation of COVID-19. American Journal of Emergency Medicine. 2020;38:1542.e1–1542.e3. doi: 10.1016/j.ajem.2020.03.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dane B, Brusca-Augello G, Kim D, Katz DS. Unexpected Findings of Coronavirus Disease (COVID-19) at the Lung Bases on Abdominopelvic CT. American Journal of Roentgenology. 2020 doi: 10.2214/AJR.20.23240. [DOI] [PubMed] [Google Scholar]
- 30.Hossain R, Lazarus MS, Roudenko A, Dako F, Mehta V, Alis J, Zalta B, Lei B, Haramati LB, White CS (2020) CT Scans Obtained for Nonpulmonary Indications: Associated Respiratory Findings of COVID-19. Radiology Epub ahead of print [DOI] [PMC free article] [PubMed]
- 31.Lang M, Som A, Mendoza DP, Flores EJ, Li MD, Shepard JO, Little BP (2020) Detection of Unsuspected Coronavirus Disease 2019 Cases by Computed Tomography and Retrospective Implementation of the Radiological Society of North America/Society of Thoracic Radiology/American College of Radiology Consensus Guidelines. J.Thorac.Imaging Epub ahead of print [DOI] [PubMed]
- 32.Redmond CE, Nicolaou S, Berger FH, Sheikh AM, Patlas MN (2020) Emergency Radiology During the COVID-19 Pandemic: The Canadian Association of Radiologists Recommendations for Practice. Canadian Association of Radiologists Journal Epub ahead of print [DOI] [PubMed]
- 33.Bhayana R, Som A, Li MD, Carey DE, Anderson MA, Blake MA, Catalano O, Gee MS, Hahn PF, Harisinghani M, Kilcoyne A, Lee SI, Mojtahed A, Pandharipande PV, Pierce TT, Rosman DA, Saini S, Samir AE, Simeone JF, Gervais DA, Velmahos G, Misdraji J, Kambadakone A (2020) Abdominal Imaging Findings in COVID-19: Preliminary Observations. Radiology 201908 [DOI] [PMC free article] [PubMed]
- 34.Hellinger JC, Sirous R, Hellinger RL, Krauthamer A. Abdominal presentation of covid-19. Applied Radiology. 2020;49:24–26. [Google Scholar]
- 35.Sattar Y, Connerney M, Rauf H, Saini M, Ullah W, Mamtani S, Syed U, Luddington S, Walfish A. Three Cases of COVID-19 Disease With Colonic Manifestations. American Journal of Gastroenterology. 2020;115:948–950. doi: 10.14309/ajg.0000000000000692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Guo Y, Hu X, Yu F, Chen J, Zheng W, Liu J, Zeng P. Abdomen CT findings in a COVID-19 patient with intestinal symptoms and possibly false negative RT-PCR before initial discharge. Quantitative Imaging in Medicine and Surgery. 2020;10:1158–1161. doi: 10.21037/qims-20-463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tang L, Cheng X, Tian C, Wang R, Zhou H, Wu W, Yan L, Zeng X. Computed tomography (CT) intestinal alterations of Coronavirus Disease 2019 (COVID-19) from the imaging perspective: A case description. Quantitative Imaging in Medicine and Surgery. 2020;10:1145–1149. doi: 10.21037/qims.2020.04.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Calinescu AM, Vidal I, Grazioli S, Lacroix L, Wildhaber BE. Comment on “Beware of Too Aggressive Approach in Children With Acute Abdomen During COVID-19 Outbreak!”. Annals of Surgery. 2020 doi: 10.1097/SLA.0000000000004100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Qiu H, Wander P, Bernstein D, Satapathy SK. Acute on chronic liver failure from novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) Liver International. 2020;40:1590–1593. doi: 10.1111/liv.14506. [DOI] [PubMed] [Google Scholar]
- 40.Meini S, Zini C, Passaleva MT, Frullini A, Fusco F, Carpi R, Piani F (2020) Pneumatosis intestinalis in COVID-19. BMJ Open Gastroenterology 7 [DOI] [PMC free article] [PubMed]
- 41.Kielty J, Duggan WP, O’Dwyer M (2020) Extensive pneumatosis intestinalis and portal venous gas mimicking mesenteric ischaemia in a patient with SARS-CoV-2. Annals of the Royal College of Surgeons of England e1-e3 [DOI] [PMC free article] [PubMed]
- 42.Di Grezia M, Fransvea P, Santullo F, Tirelli F, Fico V, Mirco P, Cozza V, La Greca A, Sganga G. Intra-abdominal hypertension as a trigger of “gut failure” in SARS-CoV-2 infection: Effect of open abdomen (OA) and negative pressure therapy (NPT) on respiratory and gastrointestinal (GI) function. Medical hypotheses. 2020;144:1099542. doi: 10.1016/j.mehy.2020.109954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Corrêa Neto IJF, Viana KF, Silva MBSD, Silva LMD, Oliveira GD, Cecchini ARDS, Rolim AS, Robles L. Perforated acute abdomen in a patient with COVID-19: an atypical manifestation of the disease. Journal of Coloproctology. 2020;40:269–272. doi: 10.1016/j.jcol.2020.05.011. [DOI] [Google Scholar]
- 44.Martinez-Castano I, Calabuig-Barbero E, Gonzalvez-Pinera J, Lopez-Ayala JM. COVID-19 Infection Is a Diagnostic Challenge in Infants With Ileocecal Intussusception. Pediatric emergency care. 2020;36:e368. doi: 10.1097/PEC.0000000000002155. [DOI] [PubMed] [Google Scholar]
- 45.Rajalakshmi L, Satish S, Nandhini G, Ezhilarasi S. UNUSUAL PRESENTATION OF COVID-19 AS INTUSSUSCEPTION. Indian Journal of Practical Pediatrics. 2020;22:236. [Google Scholar]
- 46.Moazzam Z, Salim A, Ashraf A, Jehan F, Arshad M (2020) Intussusception in an infant as a manifestation of COVID-19. Journal of Pediatric Surgery Case Reports 59 [DOI] [PMC free article] [PubMed]
- 47.Lu X, Zhang L, Du H, Zhang J, Li YY, Qu J, Zhang W, Wang Y, Bao S, Li Y, Wu C, Liu H, Liu D, Shao J, Peng X, Yang Y, Liu Z, Xiang Y, Zhang F, Silva RM, Pinkerton KE, Shen K, Xiao H, Xu S, Wong GWK. SARS-CoV-2 Infection in Children. N Engl J Med. 2020;382:1663–1665. doi: 10.1056/NEJMc2005073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cai X, Ma Y, Li S, Chen Y, Rong Z, Li W (2020) Clinical Characteristics of 5 COVID-19 Cases With Non-respiratory Symptoms as the First Manifestation in Children. Frontiers in Pediatrics 8 [DOI] [PMC free article] [PubMed]
- 49.Behzad S, Aghaghazvini L, Radmard AR, Gholamrezanezhad A. Extrapulmonary manifestations of COVID-19: Radiologic and clinical overview. Clinical imaging. 2020;66:35–41. doi: 10.1016/j.clinimag.2020.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Culver A, Arbelot C, Bechis C, Cassir N, Leone M. First description of SARS-CoV-2 in ascites. IDCases. 2020;21:e00836. doi: 10.1016/j.idcr.2020.e00836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wolters Kluwer (2020) COVID-19 TOOLS & RESOURCES FOR CLINICIANS. Expert Search Strategies. http://tools.ovid.com/coronavirus/. Accessed 22 June 2020
- 52.Campbell S (2020) Search Hedge to Retrieve Studies related to COVID-19 from the SCOPUS Database. https://guides.library.ualberta.ca/health-sciences-search-filters/subject-filters. Accessed 22 June 2020
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.