Abstract
COVID-19 is the infectious disease caused by a recently discovered SARS-CoV-2. Following an initial outbreak in December 2019 in Wuhan, China, the virus has spread globally culminating in the WHO declaring a pandemic on 11 March 2020. We present the case of a patient with an initial presentation of COVID-19 pneumonitis requiring mechanical ventilation for nearly 2 weeks and total admission time of 3 weeks. She was given prophylactic dose anticoagulation according to hospital protocol during this time. Following a week at home, she was readmitted with acute massive pulmonary embolism with severe respiratory and cardiac failure, representing the first such case in the literature.
Keywords: pulmonary embolism, adult intensive care
Background
Our understanding of COVID-19 continues to evolve as the disease remains a global public health emergency. A plethora of research has been conducted to investigate the disease process and the optimal treatment modalities but there still remain many unknowns. Infection with SARS-CoV-2 is often asymptomatic but leads to deregulated immune responses with multiorgan failure and critical illness in a minority of patients.1
This case examines aspects of COVID-19 emphasising the increased thrombogenicity seen during infection and the potential need for extended anticoagulation following recovery particularly in those patients with severe illness and pre-existing risk factors.
Case presentation
A 52-year-old woman with a background of obesity and undiagnosed type 2 diabetes mellitus was admitted to intensive care with breathlessness preceded by a week-long viral prodrome. Admission chest radiography revealed diffuse bilateral infiltrates (figure 1) associated with severe type 1 respiratory failure (PaO2/FiO2 ratio 75 mm Hg prior to mechanical ventilation). After a 24-hour trial of continuous positive airway pressure, she deteriorated with tiredness, increased work of breathing and fluctuating conscious level. A confirmatory nasopharyngeal swab detected SARS-CoV-2 RNA.
Figure 1.
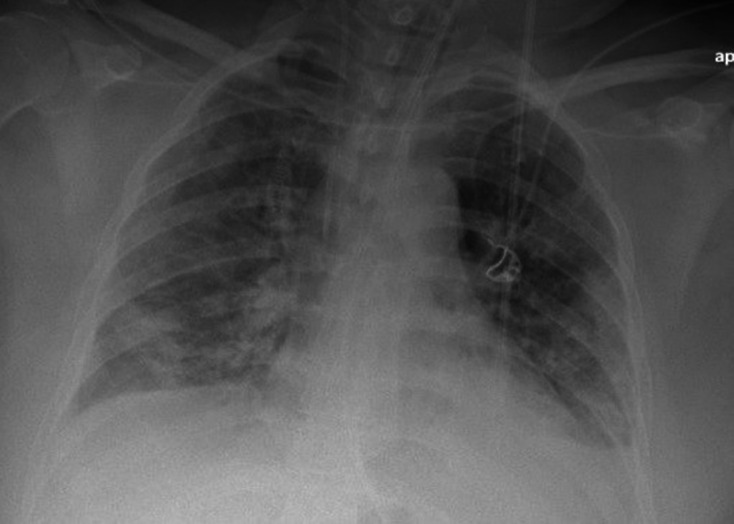
Diffuse bilateral infiltrates on first admission chest radiography.
Following endotracheal intubation and mechanical ventilation, she underwent intensive care treatment for 2 weeks including airway pressure release ventilation, multiple sessions of prone positioning, antimicrobial therapy for secondary bacterial infection and continuous renal replacement therapy for 5 days. She gradually improved and after 11 days was successfully liberated from respiratory support without requirement of reintubation or tracheostomy. Her condition continued to improve with rigorous physiotherapy and after step-down to the ward, she was successfully discharged home after a total 3-week inpatient stay.
During her hospitalisation she received consistent doses of prophylactic low molecular weight heparin (LMWH) adjusted to her weight (101 kg, body mass index (BMI) 42) according to standard hospital protocol for venous thromboembolism (VTE) prophylaxis. Initially 60 mg of Enoxaparin was administered subcutaneously once daily, increased to 40 mg two times per day after 4 days to reflect updated local anticoagulation protocols for those seriously affected by the disease. She was stepped down to ward from the intensive care unit and later at the time of discharge to home she was given insulin and antihypertensive medication to take away. LMWH was discontinued in keeping with standard hospital protocol predating any specific COVID-19 guidance.
One week later at 22:00 hours, she was brought to the emergency department by ambulance with severe breathlessness. She reported 2 days of right-sided chest pain with progressive dyspnoea culminating in syncope prior to presentation to the emergency department.
On arrival the patient was conscious but unable to complete sentences. Initial examination demonstrated a diaphoretic and agitated patient with unremarkable chest auscultation. The respiratory rate was 40/min and oxygen saturations were 85% on 15 L via a non-rebreathe device with a partial pressure arterial oxygen of 7.5 kPa. Her systolic blood pressure was 80 mm Hg with a heart rate of 130 beats/minute and cold peripheries. Although alert she was confused and unable to give a clear history. She was apyrexial with unremarkable abdominal and lower limb examinations.
Investigations
Electrocardiography demonstrated a sinus tachycardia and right heart strain suggested by subtle S-waves in Lead I associated with Q-waves and subtle T-wave inversion in Lead III.
Urgent CT pulmonary angiography (CTPA) was undertaken after initial management revealing bilateral pulmonary emboli with saddle component and right heart strain.
Bedside echocardiography after subsequent admission to intensive care revealed a dilated, impaired right ventricle and a ‘D-shaped’ left ventricle with pronounced left-ward septal deviation, more pronounced during systole indicative of pressure overload.
During the initial presentation D-dimer levels were 1.2 fibrinogen equivalent units (FEU) mcg/mL (normal range in our institution 0.0–0.50 FEU mcg/mL). D-dimer levels at the time of her second admission were 8.1 FEU mcg/mL.
Differential diagnosis
The clinical instability and refractory hypoxia warranted emergency rapid sequence induction and endotracheal intubation with intermittent boluses (10–100 μg) of epinephrine required to support her increasingly labile blood pressure. Despite intubation, hypoxia persisted even after maximal oxygen delivery (FiO2 1.0), recruitment manoeuvres and optimisation of ventilation and patient position. Urgent CT was arranged while thrombolysis was considered.
Other considerations during the initial patient assessment included secondary bacterial infection, atypical pnuemonia, cardiogenic pulmonary oedema and pulmonary embolism (PE). With the overall lack of clarity over the cause of her presentation and the uncertain nature of COVID-19 with its unknown potential for relapse, confirmatory imaging was sought to confirm the diagnosis.
Treatment
With persistent severe hypoxia and hypotension, an urgent decision regarding administration of thrombolysis was required. Intensive care personnel reviewed the images (figures 2 and 3) immediately after performance of the scan. We were able to accurately identify pulmonary emboli (subsequently confirmed on formal reporting an hour later), and this enabled immediate initiation of intravenous thrombolysis with tissue plasminogen activator (10 mg bolus of Alteplase with subsequent 90 mg infusion over 30 min as per our trust protocol) within minutes of completion of CTPA, while still within the scanning room. She was admitted to intensive care to continue ventilation and inotropic support.
Figure 2.
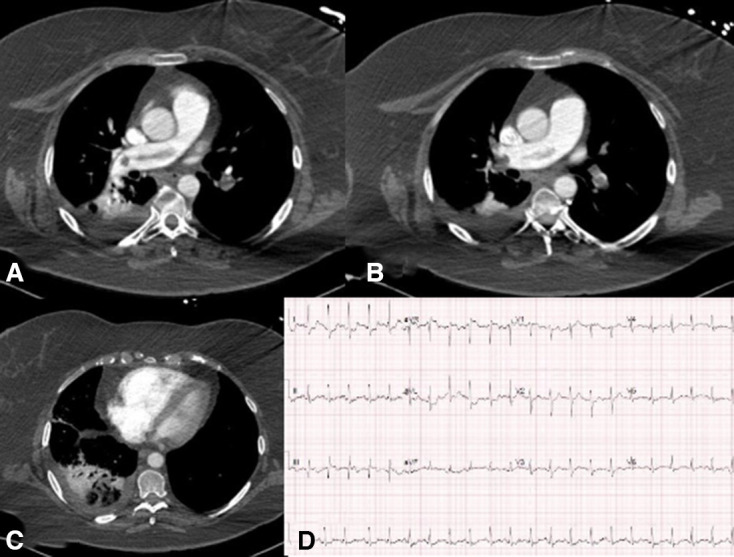
CTPA vascular/soft tissue windows. —(A) saddle embolus component; (B) large volume bilateral pulmonary emboli; (C) right heart enlargement (compared with the left ventricle). (D) ECG demonstrating features of right heart strain with ‘S1 Q3 T3’ pattern. CTPA, CT pulmonary angiography.
Figure 3.
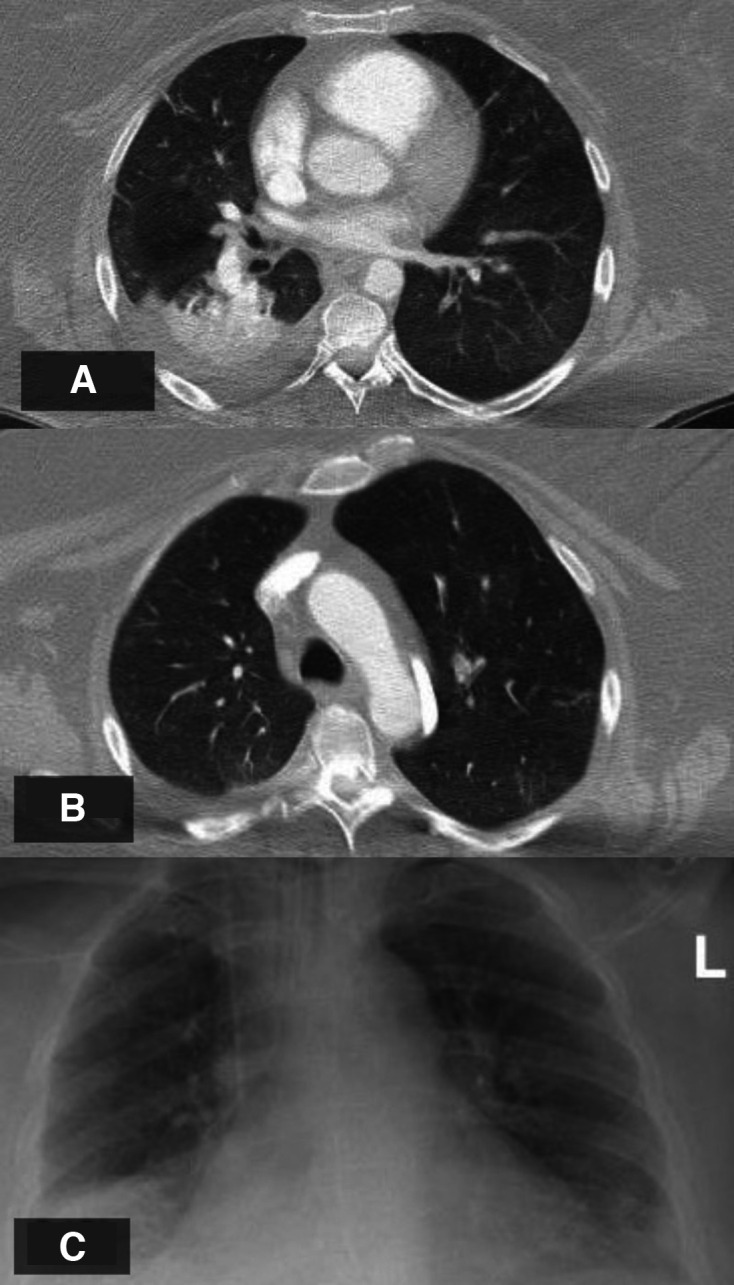
(A) CTPA lung window right basal pleural effusion and posterior ‘wedge’ infarction. Clear lung fields and resolution of ground glass changes following COVID-19 infection (B, C). CTPA, CT pulmonary angiography.
Outcome and follow-up
Overnight she was sedated, ventilated and required an epinephrine infusion (maximum dose 15 μg/min) to maintain an adequate mean arterial blood pressure. She made a rapid recovery. An initial FiO2 of 1.0 was required for 3 hours following endotracheal intubation likely due to significant shunt and deadspace ventilation with the large volume bilateral PE. However following thrombolysis there was a brisk improvement in her clinical condition with no requirement for vasopressors or inotropes at 12 hours post presentation and an FiO2 requirement of 0.5. She was successfully liberated from mechanical ventilation 16 hours later with no immediate neurological sequelae. After step-down to the ward long-term anticoagulation therapy was initiated after multidisciplinary discussion followed by discharge after 5 days.
Discussion
Risk factors for thrombosis are numerous but are generally considered to contribute by three key mechanisms (Virchow’s Triad); endothelial injury, reduced flow/stasis and hypercoagulable state.2 Although there are many unknowns with regard to this novel disease, increasing experience suggests that patients with severe COVID-19 infection have elements of all three.2 Following initial discharge our patient was also noted to have reduced mobility and difficulty exercising with easy fatigability. Allied to her obesity, a risk factor for VTE,3 this illustrates a picture of thromboembolic risk.
Pulmonary emboli has been reported frequently in COVID-19 and are often noted in patients with COVID-19 without other standard risk factors, suggesting that it is an independent risk factor for VTE.4 Data from early French experiences revealed PE prevalence of 23% in patients with severe COVID-19 infection. Requirement for mechanical ventilation was also strongly linked to the presence of PE on imaging.5 There is no current evidence to define the incidence of PE following recovery.
At readmission this patient had little evidence of persistent infection with resolution of the majority of ground glass changes seen in prior imaging or other symptoms such as cough or fever. The duration of the prothrombotic state associated with COVID-19 and therefore the optimal management strategy is unclear.6 This case report aims to review the current literature regarding thromboprophylaxis in patients with COVID-19 and highlights the potential for patient readmission after critical illness.
With regard to the emergent management of PE, guidelines recommend thrombolysis where there is persistent haemodynamic compromise, evidence demonstrating survival benefit and improved long-term outcomes.7 Thrombolysis without cardiovascular compromise is controversial.8 Furthermore refractory hypoxia is not considered a typical indication for thrombolysis which is not without risk; reported rates of intracerebral haemorrhage of 1.7%.7 However case reports and studies do suggest patients with profound respiratory failure may benefit from clot lysis.8 9 It is worthwhile to note that while we administered thrombolysis for hypotension, there was marked improvement in gas exchange to go with stabilised blood pressure.
SARS-CoV-2 is a single-stranded RNA coronavirus.10Common symptoms include fatigue, fever, headache, dyspnoea and myalgia. Although advanced age and comorbidity (eg, hypertension, diabetes mellitus) are risk factors for developing serious illness, young and otherwise healthy patients can become critically unwell.11
Data from populations affected by the COVID-19 demonstrate abnormal activation of the clotting cascade.12 Markers such as D-dimer concentration are associated with deleterious patient trajectory and increased incidence of mortality.9While COVID-19 is typically associated with pneumonia, a multi-system inflammatory disorder and deregulated coagulation are at play leading to poor outcomes in those worst affected.13
Many pathways have been postulated to explain these extreme derangements in clotting. A syndrome of hyperinflammation is seen in those worst affected and it appears that parts of this cascade are responsible for coagulopathy.14It is widely accepted that the general endpoint of the inflammatory process is thrombosis.15 Thus immune system activation and subsequent inflammatory processes are intrinsically linked to clotting.
Common laboratory investigation abnormalities include a lymphopaenia, elevated C-reactive protein, ferritin, interleukin-6 (IL-6, an inflammatory cytokine) and dramatically elevated D-dimers.16 Coagulation tests commonly reveal a prolongation of the prothrombin time and international normalised ratio alongside shortened activated partial thromboplastin times and ratios.16
Studies have implicated elevated expression of IL-6 as a potential cause of endothelial dysfunction leading to thrombosis,17 reinforced further by research implicating IL-6 as a contributor to thrombotic risk in inflammatory conditions such as psoriasis.18 Initial data suggest that patients with complicated COVID-19 infection have nearly three times the concentration of IL-6 compared with those exhibiting less severe disease.19 This highlights the importance of ongoing work examining the efficacy of IL-6 inhibitors as an immunomodulatory therapy.20
Obesity in isolation is a risk factor for VTE. The increased risk for VTE is thought to be in part a result of the background chronic inflammatory state found in obese patients. Hypertrophic adipose tissues lend to the over production of inflammatory cytokines such as TNF-a, interferon-g and IL-6. These cytokines induce an inflammatory state the endpoint of which is an increase in procoagulant factors, increased tissue factor expression and augmented platelet activation.3
Patients with severe COVID-19 infection are at risk of mortality and this risk is compounded by the presence of comorbidity including cardiovascular disease, diabetes mellitus and chronic obstructive pulmonary disease. Obesity is additionally recognised as lending to poor outcomes in COVID-19.21 It appears possible that the obesity-related inflammation exacerbated by COVID-19 mediated effects could lead to excess thrombosis in this group partly explaining the poorer outcomes seen in obese patients.
Thromboprophylaxis can take many forms, however a study by Tang et al demonstrated a clear survival benefit in patients with COVID-19 receiving LMWH as part of their treatment. Severe COVID-19 with either high D-dimers or high likelihood of sepsis-induced coagulopathy were shown to have improved rates of mortality when treated with LMWH at prophylactic doses.22Appropriate use of LMWH may therefore have a central role to play in managing the sick population with COVID-19.
Although classically considered an anticoagulant, heparin does have secondary properties which may have utility in the treatment of COVID-19. Its effects may have a role in disruption of clot production as well as ameliorating the inflammatory effects of thrombin.23 Heparin has been shown to have direct anti-inflammatory properties including the antagonism of cytokines and sequestration of acute phase proteins.24
The International Society for Thrombosis and Haemostasis suggests that prophylactic treatment with LMWH is prudent in all patients with COVID-19, particularly with severe disease or extreme derangements in clotting parameters.25 Regular monitoring of clotting parameters during admission with severe disease was also strongly recommended.
The American College of Cardiology suggests implementing extended courses of thromboprophylaxis in patients with COVID-19 with other risks factors for VTE for example, reduced mobility, pre-existing comorbidity or malignancy. D-dimer levels, greater than two times the upper limit of normal at point of discharge, have also been suggested as a guide for the initiation of prolonged anticoagulation treatment.26
The British Society of Haematology advocates the use of LMWHs in the management of COVID-19.2 Hospital-acquired VTE is defined as any thrombotic event occurring within 90 days of hospital admission even after discharge.2 Compared with other populations, patients with COVID-19 appear to have higher incidences of VTE particularly with deranged clotting markers, critical care admission or reduced mobility.2
Reports from France and the Netherlands revealed a high burden of thrombotic complications (primarily PE) despite routine prophylactic LMWH.27 28 There were strong recommendations towards the use of VTE prophylaxis for all patients requiring intensive care management and a low threshold for more aggressive anticoagulation strategies given the development of thrombotic complications in approximately one third of patients in intensive care despite prophylactic anticoagulation.28
Emerging antithrombotic guidance highlights the potential benefits of extended thromboprophylaxis beyond hospital admission.29 Several risk factors were identified including the presence of a D-dimer level twice the upper limit of normal at the time of potential discharge.29 Suggested regimens described courses of up to 45 days for adequate protection. Other identified risk factors included patients over 60 years old, those with a past history of VTE, active malignancy, reduced mobility, BMIs>30 and recent stay in critical care.29 These recommendations have subsequently been reflected in local guidelines produced shortly after our case.
Learning points.
The case presented illustrates the wide reaching and prolonged sequelae of critical illness following COVID-19 with complications occurring despite recovery from the acute phase of the illness.
Reduced mobility, easy fatigability and weakness in recovered patients are also likely to contribute to morbidity and mortality.
Given the still uncertain nature of COVID-19 and its long-term effects on patients, there will be much to learn in the coming weeks and months regarding subsequent management of patients after the acute phase of the disease.
Further work may better characterise the thrombotic risks and identify appropriate management strategies. The role of thromboprophylaxis for mild cases of COVID-19 in patients with significant risk factors remains unclear. These patients may be advised to self-isolate with resulting reduced levels of physical activity.
It is also uncertain how long the proinflammatory/prothrombotic state associated with COVID-19 persists for after apparent resolution of the disease with regard to physical symptoms for example, oxygen requirement, fever. There are few recommendations for extended thromboprophylaxis but this case supports subsequent early guidance, which suggests it is beneficial in at-risk populations. We would advocate the use of a structured approach on a patient-to-patient basis, balancing thrombotic and bleeding risks.
Footnotes
Twitter: @deepu84in
Contributors: PaV and DSS helped in conception or design of the work. PrV performed data collection. PrV and DSS helped in drafting the article. PaV, PrV and DSS performed critical revision and provided final approval of the version to be published.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020;395:507–13. 10.1016/S0140-6736(20)30211-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hunt B, Retter A, McClintock C. Practical guidance for the prevention of thrombosis and management of coagulopathy and disseminated intravascular coagulation of patients infected with COVID-19. Available: https://b-s-h.org.uk/media/18171/th-and-covid-25-march-2020-final.pdf [Accessed 25 May 2020].
- 3.Blokhin IO, Lentz SR. Mechanisms of thrombosis in obesity. Curr Opin Hematol 2013;20:437–44. 10.1097/MOH.0b013e3283634443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Danzi GB, Loffi M, Galeazzi G, et al. Acute pulmonary embolism and COVID-19 pneumonia: a random association? Eur Heart J 2020;41:1858. 10.1093/eurheartj/ehaa254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grillet F, Behr J, Calame P, et al. Acute pulmonary embolism associated with COVID-19 pneumonia detected with pulmonary CT angiography. Radiology. In Press 2020;296:E186–8. 10.1148/radiol.2020201544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Spyropoulos AC, Levy JH, Ageno W, et al. Scientific and standardization Committee communication: clinical guidance on the diagnosis, prevention, and treatment of venous thromboembolism in hospitalized patients with COVID-19. J Thromb Haemost 2020;18:1859–65. 10.1111/jth.14929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Konstantinides SV, Meyer G, Becattini C, et al. 2019 ESC guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European respiratory Society (ERS). Eur Respir J 2019;54:1901647 10.1183/13993003.01647-2019 [DOI] [PubMed] [Google Scholar]
- 8.D'Cruz R, Morton R, Jakes A, et al. Respiratory failure as an indication for thrombolysis in pulmonary embolism? Eur Respir J 2016;48:PA2469. [Google Scholar]
- 9.Loebinger MR, Bradley JC. Thrombolysis in pulmonary embolism: are we under-using it? QJM 2004;97:361–4. 10.1093/qjmed/hch069 [DOI] [PubMed] [Google Scholar]
- 10.Shereen MA, Khan S, Kazmi A, et al. COVID-19 infection: origin, transmission, and characteristics of human coronaviruses. J Adv Res 2020;24:91–8. 10.1016/j.jare.2020.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fang L, Karakiulakis G, Roth M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir Med 2020;8:e21. 10.1016/S2213-2600(20)30116-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tang N, Li D, Wang X, et al. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost 2020;18:844–7. 10.1111/jth.14768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ruan Q, Yang K, Wang W, et al. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med 2020;46:846–8. 10.1007/s00134-020-05991-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leisman DE, Deutschman CS, Legrand M. Facing COVID-19 in the ICU: vascular dysfunction, thrombosis, and dysregulated inflammation. Intensive Care Med 2020;46:1105–8. 10.1007/s00134-020-06059-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gaertner F, Massberg S. Blood coagulation in immunothrombosis-At the frontline of intravascular immunity. Semin Immunol 2016;28:561–9. 10.1016/j.smim.2016.10.010 [DOI] [PubMed] [Google Scholar]
- 16.Levi M, Thachil J, Iba T, et al. Coagulation abnormalities and thrombosis in patients with COVID-19. Lancet Haematol 2020;7:e438–40. 10.1016/S2352-3026(20)30145-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kerr R, Stirling D, Ludlam CA. Interleukin 6 and haemostasis. Br J Haematol 2001;115:3–12. 10.1046/j.1365-2141.2001.03061.x [DOI] [PubMed] [Google Scholar]
- 18.Wang Y, Golden JB, Fritz Y, et al. Interleukin 6 regulates psoriasiform inflammation-associated thrombosis. JCI Insight 2016;1:e89384. 10.1172/jci.insight.89384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Coomes EA, Haghbayan H. Interleukin-6 in COVID-19: a systematic review and meta-analysis. medRxiv 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Magro G. SARS-CoV-2 and COVID-19: Is interleukin-6 (IL-6) the 'culprit lesion' of ARDS onset? What is there besides Tocilizumab? SGP130Fc. Cytokine X 2020;2:100029. 10.1016/j.cytox.2020.100029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Docherty AB, Harrison EM, Green CA, et al. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study. BMJ 2020;369:m1985. 10.1136/bmj.m1985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tang N, Bai H, Chen X, et al. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost 2020;18:1094–9. 10.1111/jth.14817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thachil J. The versatile heparin in COVID-19. J Thromb Haemost 2020;18:1020–2. 10.1111/jth.14821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Poterucha TJ, Libby P, Goldhaber SZ. More than an anticoagulant: do heparins have direct anti-inflammatory effects? Thromb Haemost 2017;117:437–44. 10.1160/TH16-08-0620 [DOI] [PubMed] [Google Scholar]
- 25.Thachil J, Tang N, Gando S, et al. ISTH interim guidance on recognition and management of coagulopathy in COVID-19. J Thromb Haemost 2020;18:1023–6. 10.1111/jth.14810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bikdeli B, Madhavan MV, Jimenez D, et al. COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up: JACC state-of-the-art review. J Am Coll Cardiol 2020;75:2950–73. 10.1016/j.jacc.2020.04.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Helms J, Tacquard C, Severac F, et al. High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study. Intensive Care Med 2020;46:1089–98. 10.1007/s00134-020-06062-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Klok FA, Kruip MJHA, van der Meer NJM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res 2020;191:145–7. 10.1016/j.thromres.2020.04.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cohoon KP, Mahé G, Tafur AJ, et al. Emergence of institutional antithrombotic protocols for coronavirus 2019. Res Pract Thromb Haemost 2020;4:510–7. 10.1002/rth2.12358 [DOI] [PMC free article] [PubMed] [Google Scholar]


