Abstract
Sclerosing extramedullary hematopoietic tumor (SEMHT) is a rare disease that was originally named fibrous hematopoietic tumor or myelosclerosis. The process typically occurs in patients with a history of chronic myeloproliferative disorders and may afflict the skin, lung, breast, gastrointestinal tract, breast, kidney, lymph node, and thyroid gland. In this article, we report the case of a 37-year-old female with more than 5 years history of acute B-cell lymphoblastic leukemia who presented with right upper quadrant pain and tenderness. Computed tomography scan showed multiple new ring-enhancing low-density lesions within the right and left hepatic lobes. A computed tomography–guided liver core biopsy was performed on one of the new liver lesions and showed extramedullary hematopoiesis with atypical megakaryocytes and sinusoidal capillarization with associated fibroblastic proliferation. Numerous atypical megakaryocytes were scattered in the background of haphazard collagen deposition. No significant blasts or a leukemic process were identified. Bone marrow aspiration and biopsy showed extensive reticulin fibrosis (MF-3), trilineage dysplasia, increased blasts (10% to 19%), and hypercellularity (close to 100%), which was consistent with MDS-EB-2. Cytogenetics was reported as follows: 44~46,XX,-3,add(3)(p13),-5,-6,-7,17,del(17)(p12),+1~5mar[cp9]/46,XX. Molecular analysis was negative for both JAK2 V617F and CALR exon 9 activating mutations. In summary, we contributed a new case of SEMHT diagnosis in a synchronous presentation with poor clinical evolution associated chromosome 7 deletion and intact JAK2 and CALR exon 9. Care should be taken when diagnosing intraabdominal and retroperitoneal soft tissue masses with the history of hematological disorders.
Keywords: sclerosing extramedullary hematopoietic tumor, chronic myeloproliferative disorders
Introduction
Sclerosing extramedullary hematopoietic tumor (SEMHT) is a rare tumor-like condition that was previously referred to as fibrous hematopoietic tumor or myelosclerosis.1,2 The lesion presents in patients with a history of chronic myeloproliferative disorders, including chronic myelogenous leukemia, polycythemia vera, and essential thrombocythemia and may involve a variety of different organs including lung, breast, skin, gastrointestinal tract, breast, kidney, lymph node, and thyroid gland. These lesions can be morphologically concerning for a number of entities including sarcomas and lymphomas. The presence of hematopoietic elements including megakaryocytes (which can show atypia), fibroblastic proliferation, and fibrosis along with immunohistochemical stains (factor VIII, CD15, CD30, and S100) are helpful in distinguishing SEMHT from other malignancy.
Case Report
This patient is a 37-year-old female who presented with right upper quadrant pain and tenderness for 3 to 4 days with referred pain in the right shoulder on deep breathing. Review of her history showed 2 right lobe liver masses that were initially identified by computed tomography (CT) scan about 5 years prior that were most suggestive of hemangiomas and were stable in the following CT scans. The current CT scan showed multiple new ring-enhancing low-density lesions within the right and left hepatic lobes. The dimension of the right hepatic lesion is up to 2.1 cm. The patient had a history of treated Philadelphia chromosome negative acute B-cell lymphoblastic leukemia initially diagnosed 6 years prior to the current presentation with subsequent myelodysplastic syndrome with excess blast, subtype 2 (MDS-EB-2) diagnosed 6 months ago. Bone marrow aspiration and biopsy 3 days before this visit showed extensive reticulin fibrosis (MF-3), trilineage dysplasia, increased blasts (10% to 19%), and cellularity (close to 100%), which was consistent with MDS-EB-2. Cytogenetics: 44~46,XX,-3,add(3)(p13),-5,-6,-7,17,del(17)(p12),+1~5mar[cp9]/46,XX. JAK2 V617F activating mutation and CALR exon 9 insertions/deletions were not detected.
Complete blood cell counts were reported as follows: white blood cell 0.5, hemoglobin 7.4 g/dL, hematocrit 20.0%, mean corpuscular volume 86.1 fL, red cell distribution width 12.4%, and platelets 4000. The differential was reported as follows: granulocytes 12%, lymphocytes 85.5%, and monocytes 4%.
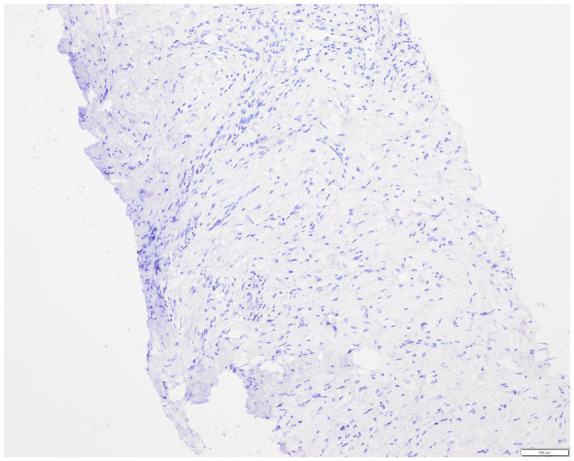
A CT-guided liver core biopsy was performed on one of the liver lesions and showed megakaryocytes and sinusoidal capillarization adjacent to an area of fibroblastic proliferation (Figure 1). The megakaryocytes were atypical and were identified along with intermingled areas of fibroblastic proliferation and fibrosclerosis (Figure 2). A few atypical megakaryocytes were also identified within the dilated sinusoids. Prominent cholestasis was observed outside the fibrous area. Immunohistochemical staining was performed. Pax-5 and myeloperoxidase staining was negative. Keratin was positive only in hepatocytes (Figure 3) and Myosin staining highlighted smooth muscle and a few scattered cells (Figure 4). CD31 and CD34 stained vessels and scattered cells. CD61 stained megakaryocytes (Figure 5). CD163 stained numerous histiocytes. No significant blast or leukemic process was identified. Based on these findings the diagnosis of SEMHT was considered.
Figure 1.

Extramedullary hematopoiesis with megakaryocytes and sinusoidal capillarization adjacent to an area of fibroblastic proliferation (hematoxylin-eosin, 40×).
Figure 2.

Numerous atypical megakaryocytes along with fibroblastic proliferation and fibrosis/sclerosis (hematoxylin-eosin, 200×).
Figure 3.

Cytokeratin, immunohistochemical stain (100×).
Figure 4.
Myosin, immunohistochemical stain (100×).
Figure 5.

CD61, immunohistochemical stain (100×).
Discussion
While the majority of SEMHT cases present in patients with a history of chronic myeloproliferative disorder, we present a case report of a patient with >5 years history of B-ALL, 0.5 years of MDS-EB-2, and recent history of liver lesions with accompanying liver biopsy. The cytogenetic complexity and the presence of -7/del (7q) places the patient into the poor prognostic category for MDS and raises the possibility of chemotherapy-associated MDS. Recent bone marrow pathology showed extensive reticulin fibrosis, which can lead to extramedullary hematopoiesis (EMH). SEMHT is reported to be more commonly seen in idiopathic MF and is usually located in the abdomen, retroperitoneum, and mesentery.3 It can rarely present in the liver, where an additional diagnostic challenge of distinguishing it from the more commonly seen benign EMH. EMH is typically more cellular and less fibrotic compared with SEMHT. Atypical megakaryocytes present in SEMHT are the diagnostic hallmark to differentiate between the 2 entities and are not identified in EMH. SEMHT usually develops after the diagnosis of chronic myeloproliferative disorders whereas EMH can be observed in other diseases including sickle cell anemia, thalassemia, hemoglobinopathies, and hereditary spherocytosis.4 SEMHT may be misdiagnosed not only as EMH but also other neoplasms including Hodgkin’s disease (where the atypical cells can be mistaken for Reed Sternberg cells), carcinoma, or sarcoma.
In summary, we contribute a new case of SEMHT presenting synchronously with therapy-associated MDS with a poor clinical prognosis, associated chromosome 7 deletion, and intact JAK2 and CALR exon 9. A critical evaluation with attention to history of hematological disorders, immunohistochemistry, and morphology can help in the accurate identification of this rare entity, which is usually associated with chronic myeloproliferative lesions with worse outcome and may therefore be of prognostic significance.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work is supported by the Department of Pathology, Baylor & Scott White Health, Temple, Texas.
Ethics Approval: Our institution does not require ethical approval for reporting individual cases or case series.
Informed Consent: Informed consent for patient information to be published in this article was not obtained because we have lost contact with this patient.
References
- 1. Beckman E, Oehrle J. Fibrous hematopoietic tumors arising in agnogenic myeloid metaplasia. Hum Pathol. 1982;13:804-810. [DOI] [PubMed] [Google Scholar]
- 2. Remstein ED, Kurtin PJ, Nascimento AG. Sclerosing extramedullary hematopoietic tumor in chronic myeloproliferative disorders. Am J Surg Pathol. 2000;24:51-55. [DOI] [PubMed] [Google Scholar]
- 3. Kwon Y, Yu E, Huh J, Lee SK, Ro JY. Sclerosing extramedullary hematopoietic tumor involving lesser omentum and ligamentumteres in liver explant. Ann Diagn Pathol. 2004;8: 227-232. [DOI] [PubMed] [Google Scholar]
- 4. Karaarslan S, Nese N, Oncel G, et al. Sclerosing extramedullary hematopoietic tumor mimicking intra-abdominal sarcoma. J Pathol Transl Med. 2015;49:335-338. [DOI] [PMC free article] [PubMed] [Google Scholar]


