Abstract
The rapid rise of cases of coronavirus disease 2019 (COVID-19) has led to the implementation of public health measures on an unprecedented scale. These measures have significantly affected the training environment and the mental health of health care providers and learners. Design thinking offers creative and innovative solutions to emergent complex problems, including those related to training and patient care that have arisen as a result of the COVID-19 pandemic. Design thinking can accelerate the development and implementation of solution prototypes through a process of inspiration, ideation, and implementation. Digital technology can be leveraged as part of this process to provide care and education in new or enhanced ways. Online knowledge hubs, videoconference-based interactive sessions, virtual simulations, and technology-enhanced coaching for health care providers are potential solutions to address identified issues. Limitations of this model include inherent bias toward utilitarian instead of egalitarian principles and the subsequent threat to diversity, equity, and inclusion in solutions. Although medical educators have embraced digital transformation during the COVID-19 pandemic, there is a need to ensure that these changes are sustained.
The rapid rise of cases of coronavirus disease 2019 (COVID-19) has led to the implementation of public health measures on an unprecedented scale to “flatten the curve” and reduce mortality.1 These measures (e.g., home quarantine, social isolation, physical distancing, curfews, closures of schools and universities) have significantly affected the training environment and the mental health of learners across the continuum of education. As the demand for some health services increases exponentially and the morbidity of patients with COVID-19 rises, the pandemic is also causing unprecedented psychological distress in health care providers (HCPs) and health professions students, including burnout2,3 and moral injury, the latter of which is exacerbated by shortages in specific health services (e.g., access to ventilators) in the face of growing needs.4 Now, the lives of frontline HCPs are characterized not only by loss and stress but also by volatility, uncertainty, complexity, and ambiguity. Moreover, stress can lead to learner disengagement and interrupt the consolidation of memory, which can be detrimental to learning.
In parallel, the nature and setting of clinical work have changed for many HCPs and learners. They must adapt to physical distancing and social isolation by rapidly integrating the virtual delivery of health services. Similar to adaptations made during the 2003 severe acute respiratory syndrome (SARS) pandemic, the changes made during COVID-19 are leading HCPs to rethink medical education delivery and its focus.5 As noted by Torous and colleagues,6 the COVID-19 pandemic is an opportunity to accelerate the use of digital technology to provide access to quality care for people with complex health needs. The unpredictable scale and timing of the COVID-19 pandemic, paired with evolving digital innovation in medicine, have created a propitious environment for improving both education and patient care.
Medical educators require new models for generating solutions to address the complex training and care needs that have emerged as a result of COVID-19. Design thinking offers creative and innovative solutions to complex problems,7 including those related to volatility, uncertainty, complexity, and ambiguity.8 Design thinking principles have been applied in medical education to create educational strategies and programs.5,7,9,10 With this approach, solutions can be developed or implemented both to sustain existing education and training resources and to enhance existing methods and content to meet the new needs presented by COVID-19. Finally, design thinking can support innovation in response to new competencies and needs that have arisen during the current public health crisis.
In this article, we discuss the role of rapid design thinking during the COVID-19 pandemic to generate innovative solutions to address unique medical education challenges. Using this lens, we share insights into the role digital solutions can play to address these challenges. Finally, we identify potential limitations of rapid design thinking in today’s care and education environments.
Using Rapid Design Thinking to Generate Innovations During COVID-19
Design thinking is a process that involves observation, collaboration, fast learning, the visualization of ideas, rapid prototyping, feedback gathering, and redesign.11 The stepwise strategies used in design thinking are: (1) empathize: use a needs assessment process to identify the problem and opportunities by observing, engaging, and empathizing with users; (2) define: frame the problem in a user-centered manner; (3) ideate: identify a broad range of ideas and potential solutions; (4) prototype: use an iterative process of testing scaled down versions of solutions with users; and (5) test: implement and refine the chosen solution with user feedback.12 This last step includes the consideration of such issues as compatibility in a dynamically changing context over time.7
Similar to plan–do–study–act cycles, design thinking is an iterative process with cycles of improvement.13 It is perfectly suited to a rapidly changing environment because it gives users the ability to innovate and it acts as a vehicle for organizational change.14 Design thinking can accelerate the development of prototypes and their implementation in the current COVID-19 environment, where there is rapidly evolving information and quick and wide dissemination is necessary. Apart from accelerated solutions, the goal of design thinking is to develop human-centered solutions and to enhance the user experience; both are critical to improving the uptake of innovations.5
Design thinking has distinct features compared with other common innovation frameworks, such as agile project management.15 Design thinking involves deep content analysis, opportunity mapping, and problem framing as well as problem solving. In comparison, agile project management is more implementation focused and generally smaller in scale. Design thinking is an ideal framework for identifying and implementing solutions to COVID-19 challenges that are highly complex, larger in scope, and involving multiple stakeholders.
Given that there are numerous rapid design thinking models, we chose to focus on 3 essential stages and their relevance in medical education during the COVID-19 pandemic (see Figure 1 and below).5 The first stage (define) draws inspiration from the problem or opportunity at hand. The second stage (ideate) is ideation, during which innovative educational ideas are generated. Finally, the third stage (test) deals with implementation (i.e., putting innovations into practice).5
Figure 1.
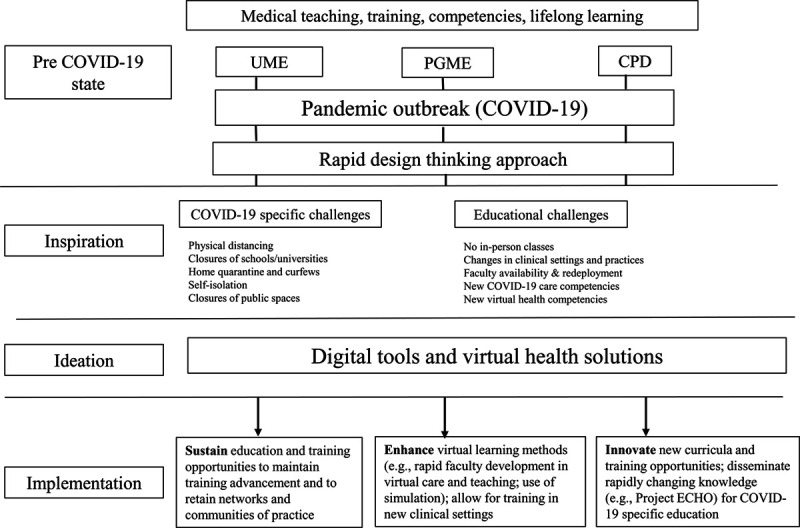
Rapid design thinking approach to overcoming COVID-19 challenges in medical education. Abbreviations: UME, undergraduate medical education; PGME, postgraduate medical education; CPD, continuing professional development.
One core component of rapid design thinking is accelerated prototyping, which can be particularly helpful during times of large-scale disruption. Accelerated prototyping involves implementing, testing, and refining user-driven solutions in an iterative manner.16 This approach is well suited to the rapidly changing COVID-19 environment and the impact of the pandemic on health professions training and education delivery.
In the following sections, we explore how these 3 stages of rapid design thinking may be used to address the challenges of COVID-19 in medical education.
Inspiration stage
COVID-19 presents a unique tripartite set of challenges for medical education and training. First, information is abundant and in a constant state of flux.17 Due to the evolving nature of the pandemic, new information is being generated within a short period of time.18 This information needs to be curated and presented to a diverse range of learners and HCPs to share with patients, their caregivers, and the general public. The process of learning new skills and updating medical knowledge to provide safe and effective care highlights the need for both lifelong learning and narrowing the gap from research to practice.
Second, physical distancing has disrupted training programs, creating uncertainty for learners. COVID-19 mitigation interventions also have interrupted in-person education events, large classroom sessions, and traditional clinical teaching methods. In addition, virtual means of delivering clinical care, such as telemedicine, are increasing the need for proficiency in the use of digital tools. Given social distancing requirements, additional efforts are needed to maintain team connection and integrate services in a constantly changing environment.
Third, COVID-19 has affected HCPs’ ability to teach, mentor, and sustain engagement in academic activities. The possibility of redeployment to meet pandemic care needs has caused anxiety in HCPs, limited their availability for teaching, and negatively affected the learner experience. Emerging reports from teaching hospitals affected by COVID-19 suggest that HCPs, especially those directly involved in assessing and managing COVID-19 patients, are at a high risk of developing psychological distress and other mental health symptoms.19–21 For example, anxiety, depression, insomnia,20,22 and burnout3 have been reported in these individuals. In addition, quarantining and social isolation have been associated with negative psychological consequences, such as post-traumatic stress symptoms, confusion, and anger.23,24 HCPs also can experience stress-related responses, fear of contagion, and concern for their family’s health.25,26
Although, understandably, the current focus is on controlling and acutely managing the COVID-19 pandemic, supporting HCPs and community members to build resilience and coping strategies is imperative. Online interactive tools, COVID-19 awareness resources, and training using simulations can help HCPs working with COVID-19 learn new medical skills that improve their well-being.
Ideation stage
The pandemic has presented many opportunities to use new digital tools to deliver clinical care, access credible COVID-19 resources and training, and support HCPs’ and learners’ well-being. Design thinking can help HCPs develop a mechanism for rapidly gathering ideas related to these activities. Planning teams with representation from key stakeholder groups should function as “education command centers” that initiate idea generation. Virtual focus groups, team meetings, and online discussion forums also can inform this ideation phase.
Digital solutions have already emerged to bridge the care gaps created by social isolation and travel restrictions during COVID-19. Torous and colleagues6 observed an increase in video care visits, and they emphasize the need to train HCPs and patients so they can participate fully in this type of virtual care. Building capacity in telemedicine, and virtual care more broadly, requires a range of education interventions to ensure competency, including online education modules; videoconference-based sessions; and longitudinal, technology-enhanced coaching for HCPs.27
Both HCPs and learners require curated (i.e., reliable) online sources to access updated information and tools to manage both the physical and mental health consequences of COVID-19. Online “knowledge hubs” could distill information for learners and guide them to “just-in-time” resources, while balancing cognitive load. Learners need to develop critical appraisal skills to effectively assess the credibility of the gray literature, online resources, and social media related to COVID-19. For instance, the donning and doffing of personal protective equipment (PPE) is a key procedure related to COVID-19 care; HCPs need to develop virtual simulations delivered via videoconferencing to allow learners to practice these procedures safely (i.e., without the risks of exposure to the virus) without wasting limited PPE supplies.28
Computer-based simulations can help HCPs and learners practice challenging scenarios in a nonthreatening (“low stake”) environment, for example, making complex decisions about the allocation of resources. HCPs also need to provide training in end-of-life care, as they and learners will be managing patients who may not have access to life-sustaining equipment like ventilators.29 They urgently need enhanced communication skills to have these difficult discussions with patients and families.
HCPs and learners are already adapting to new ways of working during COVID-19. Similar to innovations in clinical practice, they must learn to attend to their self-care in innovative ways. An integrated pathway, consisting of self-assessment tools and access to mental health resources (ranging from resilience building exercises to formal psychotherapies), is needed to support the psychological well-being of HCPs and learners. Early during the pandemic in China, HCPs with mild distress were interested in online resources, while those with more severe symptoms sought help from mental health professionals.30 An online platform is ideal to integrate these resources, provide easy access, and create virtual communities of practice and support.
List 1
Steps to Consider When Implementing an Educational Innovation During the COVID-19 Pandemic
-
•
Reflect on the organizational mission.
It is important to reflect on why the organization does the work it does and to align educational innovations with the vision, core values, and organizational strategy.
-
•
Quantify organizational strengths and resources.
The degree of success of an innovation depends on the extent to which existing skill sets and resources are harnessed.
-
•
Determine community needs without making assumptions. Ask.
Stakeholder engagement (including faculty, learners, and patients) and the co-creation of innovation products are crucial to alignment with purpose and add value.
-
•
Avoid reinventing the wheel. Ensure a strategy is not developed that addresses a need that has already been met by someone else.
A design thinking approach to developing and implementing educational innovations should be efficient, impact driven, and build on existing solutions, especially given the rapidly changing landscape of the COVID-19 pandemic.
-
•
Prioritize deliverables.
Priority setting should be driven by goals, value to stakeholders, and the resource capacity of the organization.
-
•
Decide which parts of existing educational activities to sacrifice, which to maintain, which to enhance, and which to create.
Organizing, eliminating waste, pruning, and prioritizing innovations are important steps in implementation. Decision-making tools can be used.
-
•
Be deliberate about the trade-offs between speed, scope, and cost. Decide which is the priority.
Decisive leadership is necessary to strike a balance by encouraging coproduction, collaboration, and scalability.
Implementation stage
During a crisis like the COVID-19 pandemic, the implementation stage in rapid design thinking is contingent on accelerated prototyping with iterative feedback during testing.16 The engagement of HCPs and learners during this stage is crucial for prototyping driven by end users. Continuous conversations with these and other stakeholders help to contextualize their needs, elicit preferences, and identify “on-the-fly” education strategies that can be integrated into local settings. Due to physical distancing, soliciting timely feedback during each prototyping cycle can be facilitated by digital technology. List 1 summarizes several factors to consider when implementing an educational innovation during COVID-19.
Sustaining innovations in medical education during a pandemic that could last for months has unique implementation needs. Sustainability efforts should involve existing networks, communities of practice, and various methods for curriculum delivery (e.g., existing online education platforms). Innovations also can leverage existing curricula and competency frameworks (e.g., the Accreditation Council for Graduate Medical Education core competencies,31 CanMEDS roles32) to quickly build new training opportunities.
In the following sections, we consider the unique factors associated with the rapid implementation of virtual care, knowledge hubs and online training, and self-care and mental health support for HCPs and learners.
Rapid implementation of virtual care.
If properly executed, the scope of the digital revolution ushered in by COVID-19 could transform the educational ecosystem.33 The rapid explosion of virtual care has created new opportunities for training in telemedicine. In addition, residents and students displaced from traditional care environments may now undergo clinical training in new virtual care rotations and placements.
However, fear of novel digital technology, limited telemedicine capacity, lack of end users’ involvement, lack of awareness of digital tools, and lack of trust in these tools have been shown to impede the implementation of such resources.34,35 Therefore, the rapid scaling of virtual care offerings during COVID-19 should follow a compassionate virtual care model,36 address medico-legal privacy issues, and meet documentation requirements. Going beyond virtual learning sessions, workplace-based training supported by virtual coaching for learners is needed to continue rapid prototyping within clinical settings.
Rapid implementation of knowledge hubs and online training.
The creation of online knowledge hubs can help HCPs and learners access the most up-to-date information when they need it. In turn, HCPs and learners can provide real-time feedback on their knowledge needs and modify the content to ensure it remains useful and up to date. For example, crowd sourcing can be used to identify new resources and solicit feedback. These processes will facilitate iterative user-driven solutions, a key aspect of rapid design thinking.16 Establishing clear processes, stable online platforms, and streamlined workflows supported by an information curation and development team is necessary for rapid review, revision, and dissemination of constantly changing information and educational resources to support HCPs and learners. At the same time, newer platforms, mechanisms, and experiences must be established. For example, other key virtual learning opportunities, such as those offered by social media, webinars, and podcasts, can be leveraged.
As the growing number of patients with COVID-19 threatens to overwhelm health care systems, rapid upskilling and redeployment of HCPs and learners are needed. Implementation strategies should quickly identify gaps based on a review of discipline-specific core competencies, online assessments of knowledge, and virtual simulations to assess procedural skills. Simulation is a critical component to skills-based training, specifically when dealing with high-risk or rare situations related to COVID-19. Virtual simulations can build on existing experiences from surgical residency programs, which can be adapted to address training needs during the pandemic.37
Rapid implementation of self-care and mental health support for HCPs and learners.
There is extensive literature on self-care and mental health support for HCPs and learners.38 However, the rapid upscaling of programs to support the unique needs of providers during COVID-19 requires adaptation and implementation for this context. This process can start with an environmental scan of existing virtual communities of practice. These networks can provide the necessary infrastructure and bring together HCPs and learners for training and the navigation of online self-help resources. For example, Project Extension for Community Healthcare Outcomes has demonstrated capacity to virtually connect HCPs around the world. This model could be used to support HCPs and learners in addressing their mental health needs during COVID-19.39–42
For direct mental health support, emerging evidence indicates that online self-help interventions using artificial intelligence improve the user experience.19 In China, online psychological counseling (using WeChat) has been offered 24 hours a day, free of cost, during the COVID-19 pandemic.43 Counseling by telephone, online psychological support tools, and app-based counseling have also been used and can be expanded to other settings.19
Iterative data collection from HCPs and learners as they access these educational and support resources is a critical component of the implementation stage, as the content should be congruent with phase-specific needs during the pandemic.
Limitations of a Rapid Design Thinking Model
General limitations
The deployment of solutions to address the educational challenges of COVID-19 comes with significant risks. First, virtual design thinking solutions may not remedy the risks related to social isolation between learners and their peers and teachers. Second, there is a lack of data on the efficiency and efficacy of these new learning modalities and approaches; therefore, interventions should be firmly anchored in learning theories and examine educational outcomes. Third, many organizations are reducing their educational budgets, which may constrain their ability to respond with new technological and other solutions to meet rapidly changing needs post pandemic. In addition, design thinkers will need to mitigate the financial stress anticipated for organizations during and after COVID-19. Fourth, design thinking innovations could potentially accelerate the need for emerging health professions, such as medical virtualists,44 HCPs with expertise in artificial intelligence,45 and the use of predictive analytics. Therefore, competency in these areas may be needed sooner than anticipated.
Bias and threats to equity, diversity, and inclusion
Another potential limitation of rapid design thinking is inherent in its very methodology. In times of rapid change and scarce resources, utilitarian principles are usually favored as a way to maximize the overall health and well-being of a society.46 Less popular are the egalitarian principles that purport that all individuals are equal and that inequalities between groups should be addressed.29 If rapid design thinking is used to inspire, ideate, and implement innovative educational strategies, then a concomitant effort is needed to ensure these processes address inequity.
All individuals, whether they believe themselves to be prejudiced or not, hold mental schemas that classify people into categories based on gender, race, ethnicity, age, sexual orientation, and religion, to name a few; this categorization often leads to bias and stereotyping.47 Although the design thinking process was conceived to include feedback from multiple stakeholders, it must include strategies to identify inherent biases. Strategies can be implemented at each stage of the process to address equity, diversity, and inclusion. For example, designers can challenge their assumptions and become aware of their biases by taking the implicit bias test.48 Creating opportunities for the design team to become aware of their implicit biases forces them to shift how they identify problems and understand proposed solutions.
Testing proposed innovations during each of the 3 design thinking stages against the common goals and values of the team to ensure alignment with diverse perspectives should not be a symbolic effort. Including screening questions can prompt designers to ensure they are addressing inequity. For example, access to care is key to addressing inequity, and research shows that access to broadband Internet and smartphones depends on the racial, ethnic, and socioeconomic status of individuals.49 Designers would need to respond to these issues during the rapid design thinking process.
Increasing the diversity of the design team alone will not reduce bias and discrimination.50 The process itself must include ways to address the issues of power and privilege within a team. For example, if the organizational leadership decides that a utilitarian approach is needed during a pandemic to maximize communal well-being, then all decisions, regardless of the diversity of the team, will be affected by this ideology. However, research shows that ideological influences can be challenged when groups share common goals and values.51
Conclusion
Like in all aspects of society, the COVID-19 pandemic has triggered considerable change in medical education. Rapid design thinking can be used to develop and implement solutions to overcome COVID-19-related barriers in medical education. It can help educators transform the COVID-19 crisis into an opportunity for positive and sustained change. We must ensure that the digital transformation gained during the COVID-19 pandemic continues, instead of reverting back to the pre-COVID status quo.
Footnotes
Funding/Support: None reported.
Other disclosures: None reported.
Ethical approval: Reported as not applicable.
References
- 1.Rose S. Medical student education in the time of COVID-19 [published online ahead of print March 31, 2020]. JAMA. doi:10.1001/jama.2020.5227. [DOI] [PubMed] [Google Scholar]
- 2.Fessell D, Cherniss C. Coronavirus disease 2019 (COVID-19) and beyond: Micropractices for burnout prevention and emotional wellness. J Am Coll Radiol. 2020;17:746–748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dewey C, Hingle S, Goelz E, Linzer M. Supporting clinicians during the COVID-19 pandemic. Ann Intern Med. 2020;172:752–753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Williamson V, Murphy D, Greenberg N. COVID-19 and experiences of moral injury in front-line key workers. Occup Med (Lond). 2020;70:317–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McLaughlin JE, Wolcott MD, Hubbard D, Umstead K, Rider TR. A qualitative review of the design thinking framework in health professions education. BMC Med Educ. 2019;19:98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Torous J, Jan Myrick K, Rauseo-Ricupero N, Firth J. Digital mental health and COVID-19: Using technology today to accelerate the curve on access and quality tomorrow. JMIR Ment Health. 2020;7:e18848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Badwan B, Bothara R, Latijnhouwers M, Smithies A, Sandars J. The importance of design thinking in medical education. Med Teach. 2018;40:425–426. [DOI] [PubMed] [Google Scholar]
- 8.Krawchuk F. Elkington R, van der Steege M, Glick-Smoth JL, Breen JM. Design thinking: How to thrive in a VUCA world. Exceptional Leadership by Design: How Design in Great Organizations Produces Great Leadership. 2018Somerville, MA: Emerald Publishing Limited; [Google Scholar]
- 9.Gottlieb M, Wagner E, Wagner A, Chan T. Applying design thinking principles to curricular development in medical education. AEM Educ Train. 2017;1:21–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ku B, Shah A, Rosen P. Making design thinking a part of medical education. N Eng J Med Catalyst. Published June 30, 2016. [Google Scholar]
- 11.Lockwood T. Design Thinking: Integrating Innovation, Customer Experience and Brand Value. 2010New York, NY: Allworth Press; [Google Scholar]
- 12.Deitte LA, Omary RA. The power of design thinking in medical education. Acad Radiol. 2019;26:1417–1420. [DOI] [PubMed] [Google Scholar]
- 13.Altman M, Huang TTK, Breland JY. Design thinking in health care. Prev Chronic Dis. 2018;15:E117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dunne D. Implementing design thinking in organizations: An exploratory study. J Organization Design. 2018;7:16. [Google Scholar]
- 15.Kitzmiller R, Hunt E, Sproat SB. Adopting best practices: “Agility” moves from software development to healthcare project management. Comput Inform Nurs. 2006;24:75–82. [DOI] [PubMed] [Google Scholar]
- 16.Roberts JP, Fisher TR, Trowbridge MJ, Bent C. A design thinking framework for healthcare management and innovation. Healthc (Amst). 2016;4:11–14. [DOI] [PubMed] [Google Scholar]
- 17.Hernandez-Garcia I, Gimenez-Julvez T. Assessment of health information about COVID-19 prevention on the internet: Infodemiological study. JMIR Public Health Surveill. 2020;6:e18717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chiolero A. Covid-19: A digital epidemic. BMJ. 2020;368:m764. [DOI] [PubMed] [Google Scholar]
- 19.Chen Q, Liang M, Li Y, et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7:e15–e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3:e203976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ho CS, Chee CY, Ho RC. Mental health strategies to combat the psychological impact of COVID-19 beyond paranoia and panic. Ann Acad Med Singap. 2020;49:155–160. [PubMed] [Google Scholar]
- 22.Kang L, Li Y, Hu S, et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry. 2020;7:e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet. 2020;395:912–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Xiang YT, Yang Y, Li W, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7:228–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maunder RG, Lancee WJ, Balderson KE, et al. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg Infect Dis. 2006;12:1924–1932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Maunder RG, Leszcz M, Savage D, et al. Applying the lessons of SARS to pandemic influenza: An evidence-based approach to mitigating the stress experienced by healthcare workers. Can J Public Health. 2008;99:486–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hilty D, Chan S, Torous J, Luo J, Boland R. A framework for competencies for the use of mobile technologies in psychiatry and medicine: Scoping review. JMIR Mhealth Uhealth. 2020;8:e12229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ogden PE, Cobbs LS, Howell MR, Sibbitt SJ, DiPette DJ. Clinical simulation: Importance to the internal medicine educational mission. Am J Med. 2007;120:820–824. [DOI] [PubMed] [Google Scholar]
- 29.Emanuel EJ, Persad G, Upshur R, et al. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med. 2020;382:2049–2055. [DOI] [PubMed] [Google Scholar]
- 30.Kang L, Ma S, Chen M, et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: A cross-sectional study. Brain Behav Immun. 2020;87:11–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Swing SR. The ACGME outcome project: Retrospective and prospective. Med Teach. 2007;29:648–654. [DOI] [PubMed] [Google Scholar]
- 32.Frank JR, Danoff D. The CanMEDS initiative: Implementing an outcomes-based framework of physician competencies. Med Teach. 2007;29:642–647. [DOI] [PubMed] [Google Scholar]
- 33.Keesara S, Jonas A, Schulman K. Covid-19 and health care’s digital revolution. N Engl J Med. 2020;382:e82. [DOI] [PubMed] [Google Scholar]
- 34.Poncette AS, Spies C, Mosch L, et al. Clinical requirements of future patient monitoring in the intensive care unit: Qualitative study. JMIR Med Inform. 2019;7:e13064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hong YR, Lawrence J, Williams D, Jr, Mainous III A. Population-level interest and telehealth capacity of US hospitals in response to COVID-19: Cross-sectional analysis of Google search and national hospital survey data. JMIR Public Health Surveill. 2020;6:e18961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kemp J, Zhang T, Inglis F, et al. Delivery of compassionate mental health care in a digital technology-driven age: Scoping review. J Med Internet Res. 2020;22:e16263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chick RC, Clifton GT, Peace KM, et al. Using technology to maintain the education of residents during the COVID-19 pandemic. J Surg Educ. 2020;77:729–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ruiz-Fernandez MD, Ortiz-Amo R, Ortega-Galan AM, Ibanez-Masero O, Rodriguez-Salvador MDM, Ramos-Pichardo JD. Mindfulness therapies on health professionals. Int J Ment Health Nurs. 2020;29:127–140. [DOI] [PubMed] [Google Scholar]
- 39.Serhal E, Arena A, Sockalingam S, Mohri L, Crawford A. Adapting the consolidated framework for implementation research to create organizational readiness and implementation tools for Project ECHO. J Contin Educ Health Prof. 2018;38:145–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sockalingam S, Arena A, Serhal E, Mohri L, Alloo J, Crawford A. Building provincial mental health capacity in primary care: An evaluation of a Project ECHO mental health program. Acad Psychiatry. 2018;42:451–457. [DOI] [PubMed] [Google Scholar]
- 41.Zhou C, Crawford A, Serhal E, Kurdyak P, Sockalingam S. The impact of Project ECHO on participant and patient outcomes: A systematic review. Acad Med. 2016;91:1439–1461. [DOI] [PubMed] [Google Scholar]
- 42.Sockalingam S, Clarkin C, Serhal E, Pereira C, Crawford A. Responding to health care professionals’ mental health needs during COVID-19 through the rapid implementation of Project ECHO [published online ahead of print July 9, 2020]. J Cont Educ Health Prof. doi:10.1097/CEH.0000000000000311. [DOI] [PubMed] [Google Scholar]
- 43.Li W, Yang Y, Liu ZH, et al. Progression of mental health services during the COVID-19 outbreak in China. Int J Biol Sci. 2020;16:1732–1738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sharma R, Nachum S, Davidson KW, Nochomovitz M. It’s not just FaceTime: Core competencies for the medical virtualist. Int J Emerg Med. 2019;12:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Johnston SC. Anticipating and training the physician of the future: The importance of caring in an age of artificial intelligence. Acad Med. 2018;93:1105–1106. [DOI] [PubMed] [Google Scholar]
- 46.Culyer AJ. Equity—Some theory and its policy implications. J Med Ethics. 2001;27:275–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Massey DS. Racial formation in theory and practice: The case of Mexicans in the United States. Race Soc Probl. 2009;1:12–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Greenwald AG, McGhee DE, Schwartz JL. Measuring individual differences in implicit cognition: The implicit association test. J Pers Soc Psychol. 1998;74:1464–1480. [DOI] [PubMed] [Google Scholar]
- 49.Anderson M. Mobile technology and home broadband 2019. Pew Research Center. https://www.pewresearch.org/internet/2019/06/13/mobile-technology-and-home-broadband-2019. Published June 13, 2019. Accessed August 13, 2020. [Google Scholar]
- 50.Davidson MN. The End of Diversity as We Know It: Why Diversity Efforts Fail and How Leveraging Difference Can Succeed. 2011San Francisco, CA: Berrett-Koehler Publishers; [Google Scholar]
- 51.Ely RJ, Thomas DA. Cultural diversity at work: The effects of diversity perspectives on work group processes and outcomes. Adm Sci Q. 2001;46:229–273. [Google Scholar]


