Abstract
Background
Health care workers, especially frontline nurses, faced great challenges during the coronavirus disease 2019 (COVID-19) outbreak.
Aims
To assess the magnitude of the psychological status and associated risk factors among nurses in the pandemic center in Wuhan, China.
Methods
In this study, we enrolled nurses from Renmin Hospital of Wuhan University. The questionnaire was designed to obtain basic information of the participants, and included four psychological assessment scales. We issued the questionnaires at two different points of time. We conducted the first survey on January 29 to February 2 (outbreak period) with 709 eligible responses, and the second survey on February 26 to February 28 (stable period) with 621 eligible responses. The nurses from Wuchang Fangcang shelter hospital were also enrolled in the second survey.
Results
During the pandemic, over one-third of nurses suffered from depression, anxiety, and insomnia. In the outbreak period, the nurses showed significantly higher risks for depression, anxiety, and posttraumatic stress disorder (PTSD) symptoms than those in the stable period (P < 0.01). Notably, the nurses from the Fangcang shelter hospitals were more likely to present psychological problems than those from other frontline or non-frontline (all P < 0.001) units, especially for insomnia (38.3% with severe insomnia). The nurses from the frontline, with worse physical condition and uncertain concerns about this pandemic as compared to the others, were more likely to bear psychological problems. Thus, online psychological information and sufficient protection conditions were effective interventions to help mitigate psychological distress. The nurses from Fangcang shelter hospitals suffered a significantly higher risk of psychological problems than those from other units.
Conclusion
The psychological status of nurses needs more attention during the COVID-19 pandemic, especially for those who fought in the frontline during the peak of the outbreak.
Keywords: Nurse, COVID-19, Psychological problem, Fangcang shelter hospitals
1. Introduction
In December 2019, a novel coronavirus, identified as coronavirus disease 2019 (COVID-19) by the World Health Organization (WHO) (Huang et al., 2020; Novel Coronavirus Pneumonia Emergency Response Epidemiology Team, 2020; Zhu et al., 2020) emerged in Wuhan, Hubei Province, China. This disease spread quickly and became a global pandemic (Jernigan et al., 2020). The Chinese government organized personnel, medical resources, and all other related materials actively and effectively to fight this epidemic. Almost all nurses nationwide either joined in or were ready to fight against this pandemic in Wuhan, China.
At the beginning of the pandemic, all of the health care workers were confronted with great challenges, such as limited knowledge about the clinical presentations and effective drugs, the rapidly increasing number of infected patients, limited medical resources, and inadequate protective supplies, among others (Peeri et al., 2020). Thus, the Fangcang shelter hospitals were constructed to address the increasing number of COVID-19 patients by converting exhibition centers and stadiums into health-care facilities (Chen et al., 2020). Under these stressful situations, many health care workers inevitably suffered great stress, especially for the nurses on the frontline. Several studies showed that the health care workers endured significant high psychological distress in the outbreak of SARS or MERS (Maunder, 2004; Nickell et al., 2004; Oh et al., 2017; Park et al., 2018), especially the nurses.(Maunder, 2004). However, most of these studies only evaluated the prevalence of psychiatric morbidity in a cross-sectional manner, and did not investigate the changes of psychological state in a longitudinal manner.
In this study, we evaluated the psychological status of nurses and the risk factors in different periods of the COVID-19 pandemic, by using the Generalized Anxiety Disorder Questionnaire (GAD-7), Patient Health Questionnaire (PHQ-9), Insomnia Severity Index (ISI), and Impact of Events Scale-Revised (IES-R). Moreover, we evaluated the psychological status of nurses from Fangcang shelter hospitals, which were among the first medical institutions worldwide that were created to fight the epidemic.
2. Participants and methods
2.1. Participants and study design
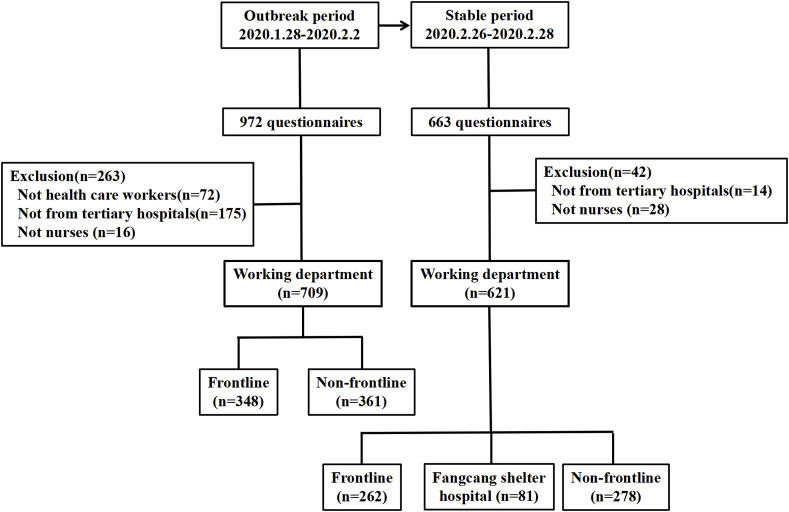
In this study, we enrolled all the nurses from Renmin Hospital of Wuhan University. All the participants completed the questionnaire and submitted their informed consent anonymously online because of the pandemic. The questionnaire was designed to obtain the basic information of the participants, and included four psychological assessment scales using WeChat, which is the most popular social media software in China. We issued the questionnaires at different points during the COVID-19 outbreak in the same WeChat groups. We conducted the first survey (outbreak period) from January 29 to February 2, which was the peak of the spread of COVID-19. We issued the second survey (stable period) from February 26 to February 28, during the stable stage of the pandemic, which was after its comprehensive prevention and control. We excluded the participants who completed their questionnaire with a duration of less than 300 s or more than 1 h. Finally, we selected a total of 1330 questionnaires for analysis, including 709 questionnaires for qualified participants in the outbreak period (excluding 72 non-health care workers, 172 not from tertiary hospital, and 16 non-nurses from 972 questionnaires) and 621 questionnaires in the stable period (excluding 14 not from tertiary hospitals and 28 not nurses from 663 questionnaires). The data drawn from both the outbreak and stable periods are from the same WeChat groups; however, we could not match the questionnaires to the individuals because the questionnaires were completed anonymously online. We classified all nurses from the emergency department, fever clinics, medical unit for COVID-19 patients, and Fangcang shelter hospitals as frontline nurses, while the others were classified as non-frontline nurses. Fangcang shelter hospitals were put into use in batches from February 5. Moreover, some health care workers from Renmin Hospital of Wuhan University were deployed to the Wuchang Fangcang shelter hospital. These nurses (n = 81), who worked in the Wuchang Fangcang hospital during the stable period, were analyzed separately. The flowchart of the nurses’ recruitment was shown in Fig. 1 . The investigation was carried out in accordance with the latest version of the Declaration of Helsinki. This study protocol was approved by the Institutional Ethics Committee of Renmin Hospital of Wuhan University. Informed consent of the participants was obtained after the nature of the procedures had been fully explained.
Fig. 1.
Flowchart of the recruitment of nurses.
2.2. Evaluation of psychological status
We used four questionnaire scales to evaluate the psychological status of nurses during the pandemic, which are the Patient Healthy Questionnaire (PHQ-9), Generalized Anxiety Disorder (GAD-7), Insomnia Severity Index (ISI), and Impact of Events Scale-Revised (IES-R). The validity and reliability of depression by the PHQ-9 scale (Cameron et al., 2008; Löwe et al., 2004) and generalized anxiety by the GAD-7 scale (Spitzer et al., 2006; Swinson, 2006) were previously demonstrated. The PHQ-9 is a single factor structure with 9 items rated from 0 (“almost never”) to 3 (“almost always”). The GAD-7 Scale consisted of 7 items; each item was scored from 0 to 3. Based on the score of the scales, the severity of anxiety or depression for participants were divided into normal (0–4), mild (5–9), moderate (10–14), and severe (>15). The ISI (Morin et al., 2011) is a seven-item instrument for insomnia assessment that uses a 5-point Likert scale (0 = not at all, 4 = extremely). The insomnia status was divided into no sleep difficulties (0–7), mild (8–14), moderate (15–21), and severe (22–28) insomnia. The IES-R scale (Creamer et al., 2003) assessed posttraumatic stress disorder (PTSD) symptoms based on DSM-IV criteria. Each item is rated using a five-point Likert scale ranging from 0 (not at all) to 4 (very much), for a total score ranging from 0 to 88. The participants scoring more than 34 points suggests possible PTSD.
2.3. Statistical analysis
All statistical analyses were carried out using the IBM SPSS Statistics (Version 16) and R software (version 3.5.1). We used one-way ANOVA and Chi-square test to compare the differences of related factors among the psychological status of nurses based on the PHQ-9, GAD-7, ISI and IES-R. We used univariable and multivariable logistic regressions to estimate the potential factors affecting the mental health of nurses. A corresponding 95% confidence interval (CI) was calculated, and the statistical significance level was set at P < 0.05.
3. Results
3.1. Basic characteristics of nurses
We enrolled a total of 1330 questionnaires for qualified participants, which included 709 (53.3%) from the outbreak period and 621 (46.7%) from the stable period (Table 1 ). In the second survey, we included 81 (13.0%) questionnaires from the Wuchang Fangcang shelter hospital. Most of the nurses were female (96.9%) and less than 40 years old (85%). The rates of marriage and living alone in the outbreak period were significantly lower than those in the stable period (P = 0.024 and P < 0.0001, respectively). The proportion of nurses that faced suspected cases (i.e., cohabitants with cough and fatigue, etc.) during the outbreak period were significantly higher than that in the stable period (P < 0.0001). The protective measures, which included protection training and conditions and confidence, as well as the physical condition and uncertainty of fighting against the pandemic, significantly improved in the stable period compared to the outbreak period (P < 0.0001). Lastly, there was a higher proportion of nurses benefiting from some online psychological consultation in the stable period (76.7%).
-
2.
Psychological status of nurses in different periods of pandemic
Table 1.
The Characteristic of Nurses from the tertiary hospital in Wuhan.
| Peak period |
Stable period |
P value |
||||
|---|---|---|---|---|---|---|
| No. |
% |
No. |
% |
|||
| 709 | 621 | |||||
| Gender | Male | 25 | 3.5 | 16 | 2.6 | 0.201 |
| Female | 684 | 96.5 | 605 | 97.4 | ||
| Age/year | 18–25 | 182 | 25.7 | 122 | 19.6 | 0.071 |
| 26–30 | 240 | 33.9 | 220 | 35.4 | ||
| 30–40 | 191 | 26.9 | 186 | 30.0 | ||
| >40 | 96 | 13.5 | 93 | 15.0 | ||
| Marital status | Unmarried | 323 | 45.6 | 237 | 38.2 | 0.024 |
| Married | 376 | 53.0 | 373 | 60.1 | ||
| Others | 10 | 1.4 | 11 | 1.8 | ||
| Professional title | None | 97 | 13.7 | 79 | 12.7 | 0.954 |
| Primary | 413 | 58.3 | 362 | 58.3 | ||
| Junior | 190 | 26.8 | 172 | 27.7 | ||
| Senior | 9 | 1.3 | 8 | 1.3 | ||
| Live alone | Yes | 207 | 29.2 | 244 | 39.3 | <0.001 |
| No | 502 | 70.8 | 377 | 60.7 | ||
| Cohabitants with suspicious symptoms | Yes | 129 | 18.2 | 27 | 4.3 | <0.001 |
| No | 580 | 81.8 | 594 | 95.7 | ||
| Adequate protection training | Yes | 484 | 68.3 | 587 | 94.5 | <0.001 |
| No | 225 | 31.7 | 34 | 5.5 | ||
| Sufficient protection conditions | Yes | 581 | 81.9 | 607 | 97.7 | <0.001 |
| No | 128 | 18.1 | 14 | 2.3 | ||
| Sufficient protection confidence | Yes | 518 | 73.1 | 595 | 95.8 | <0.001 |
| No | 191 | 26.9 | 26 | 4.2 | ||
| Value of online psychological information | Yes | 483 | 68.1 | 476 | 76.7 | <0.001 |
| No | 226 | 31.9 | 145 | 23.3 | ||
| Change of physical condition | Similar | 493 | 69.5 | 475 | 76.5 | 0.004 |
| Worse | 216 | 30.5 | 146 | 23.5 | ||
| Uncertainty of fighting against the epidemic | Yes | 411 | 58.0 | 201 | 32.4 | <0.001 |
| No | 298 | 42.0 | 420 | 67.6 | ||
| Working department* | Frontline | 348 | 49.1 | 262 | 42.2 | – |
| Non-frontline unit | 361 | 50.9 | 278 | 44.8 | ||
| Fangcang shelter hospital | – | – | 81 | 13.0 | ||
*The nurses from the emergency department, fever clinics, medical unit for COVID-19 patients, or Fangcang shelter hospital, were identified as frontline nurses, while the others were classified as non-frontline nurses. Fangcang shelter hospitals were constructed and first used after February 5, which were not investigated in the outbreak period.
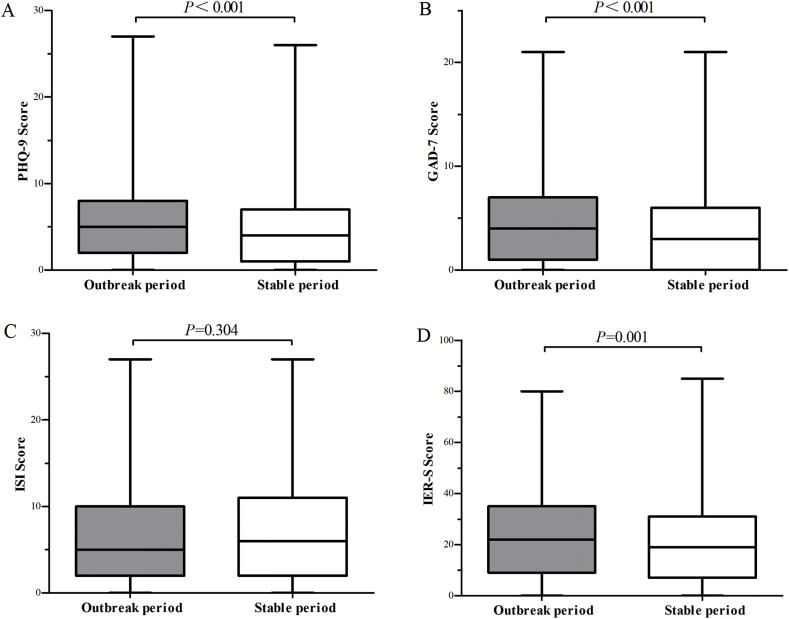
The psychological scores of the nurses in the four scales were shown in Fig. 2 . The nurses in the outbreak period had significantly higher risks for depression, anxiety, and PTSD symptoms than those in the stable period (5.59 ± 5.041 versus 4.67 ± 4.274, P < 0.001, 4.74 ± 4.651 versus 3.61 ± 3.996, P < 0.001, and 23.41 ± 16.607 versus 20.45 ± 15.292, P = 0.001, respectively), but not for the insomnia (6.57 ± 5.636 versus 6.90 ± 6.007, P = 0.304).
Fig. 2.
Scores on the psychological status of nurses in different periods of the pandemic. The differences of scores of psychological status from four questionnaire scales, which included the Patient Healthy Questionnaire (PHQ-9) (Fig. 2A), Generalized Anxiety Disorder (GAD-7) (Fig. 2B), Insomnia Severity Index (ISI) (Fig. 2C), and Impact of Events Scale-Revised (IES-R) (Fig. 2D).
During the pandemic, over one-third of nurses had symptomatic depression, anxiety, and insomnia (Table 2 ), while over one-fifth of nurses presented PTSD symptoms. During the outbreak period, the nurses on the frontline showed significantly higher proportions of the symptoms of depression, anxiety, insomnia, and PTSD (all P < 0.001). During the stable period, these proportions on the psychological problems in nurses decreased significantly. However, the differences from the frontline unit (including those in the Fangcang shelter hospitals) were still significantly higher than those from the non-frontline (all P < 0.05). Further analysis showed that the nurses from Fangcang shelter hospitals in the stable period were more likely to present psychological problems than those from other frontline or non-frontline units (all P < 0.001), especially for insomnia (38.3% with severe insomnia). In contrast, there were no differences in the rates of depression, anxiety, insomnia, and PTSD symptoms between the nurses from the different frontline (not including the nurses from Fangcang shelter hospitals) and non-frontline (all P > 0.05) units in the stable period.
-
3.
Analysis of the influence factors of psychological status
Table 2.
Psychological status of nurses in different periods of the pandemic.
| Questionnaires | Total |
Frontline |
Non-frontline |
Fangcang shelter hospitals |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | No | % | P value | ||
| Outbreak period | ||||||||||
| PHQ-9 | Normal | 335 | 47.2 | 138 | 39.7 | 197 | 54.6 | – | – | <0.001 |
| Mild | 265 | 37.4 | 134 | 38.5 | 131 | 36.3 | – | – | ||
| Moderate-severe | 109 | 15.4 | 76 | 21.8 | 33 | 9.1 | – | – | ||
| GAD-7 | Normal | 376 | 53.0 | 155 | 44.5 | 221 | 61.2 | – | – | <0.001 |
| Mild | 249 | 35.1 | 136 | 39.1 | 113 | 31.3 | – | – | ||
| Moderate-severe | 84 | 11.8 | 57 | 16.4 | 27 | 7.5 | – | – | ||
| ISI | Normal | 436 | 61.5 | 186 | 53.4 | 250 | 69.3 | – | – | <0.001 |
| Mild | 207 | 29.2 | 111 | 31.9 | 96 | 26.6 | – | – | ||
| Moderate-severe | 66 | 9.3 | 51 | 14.7 | 15 | 4.2 | – | – | ||
| IER-S | Normal | 525 | 74.0 | 232 | 66.7 | 293 | 81.2 | – | – | <0.001 |
| Abnormal | 184 | 26.0 | 116 | 33.3 | 68 | 18.8 | – | – | ||
| Stable period | ||||||||||
| PHQ-9 | Normal | 333 | 53.6 | 143 | 54.6 | 161 | 57.9 | 29 | 35.8 | <0.001 |
| Mild | 219 | 35.3 | 95 | 36.3 | 92 | 33.1 | 32 | 39.5 | ||
| Moderate-severe | 69 | 11.1 | 24 | 9.2 | 25 | 9.0 | 20 | 24.7 | ||
| GAD-7 | Normal | 381 | 61.4 | 161 | 61.5 | 180 | 64.7 | 40 | 49.4 | <0.001 |
| Mild | 201 | 32.4 | 89 | 34.0 | 85 | 30.6 | 27 | 33.3 | ||
| Moderate-severe | 39 | 6.3 | 12 | 4.6 | 13 | 4.7 | 14 | 17.3 | ||
| ISI | Normal | 373 | 60.1 | 168 | 64.1 | 181 | 65.1 | 24 | 29.6 | <0.001 |
| Mild | 176 | 28.3 | 78 | 29.8 | 72 | 25.9 | 26 | 32.1 | ||
| Moderate-severe | 72 | 11.6 | 16 | 6.1 | 25 | 9.0 | 31 | 38.3 | ||
| IER-S | Normal | 501 | 80.7 | 212 | 80.9 | 231 | 83.1 | 58 | 71.6 | 0.07 |
| Abnormal | 120 | 19.3 | 50 | 19.1 | 47 | 16.9 | 23 | 28.4 | ||
Abbreviations: PHQ-9, the Patient Healthy Questionnaire; GAD-7, Generalized Anxiety Disorder; ISI, Insomnia Severity Index; IES-R, Impact of Events Scale-Revised.
We used the logistic regression model to investigate the independent impact factors for psychological status of nurses using univariable and multivariable models. We evaluated a total of 13 related factors for the analysis, which included gender, age, marital status, professional title, living alone, cohabitants with suspicious symptoms, adequate protection training, sufficient protection conditions and confidence, value of online psychological information, change of physical condition, uncertainty of fighting against the pandemic, and working department. Among the 13 influencing factors, the independent impact factors for depression, anxiety, insomnia, and PTSD symptoms are the nurses from different working departments, change of physical condition, and uncertainty of fighting against the pandemic (Table 3 ). Additionally, the value of online psychological information was also an independent impact factor for the anxiety, insomnia, and PTSD symptoms, as well as the sufficient protection conditions for PTSD symptoms. The results of our multivariable logistic regression analysis showed that the nurses from the frontline of Fangcang shelter hospitals suffered significantly higher risks of depression, anxiety, insomnia, and PTSD symptoms than those from other frontline.
Table 3.
Independent factors for psychological status of nurses in multivariate analysis using the multivariable logistic regression analysis.
| Questionnaires | Factors | P value | OR (95.0% CI) |
|---|---|---|---|
| PHQ-9 | |||
| Working department | 0.001 | ||
| Non-frontline vs frontline | 0.018 | 0.749 (0.589–0.952) | |
| Fangcang shelter hospitals vs frontline | 0.016 | 1.943 (1.134–3.332) | |
| Physical condition change worse; Yes vs No | <0.001 | 1.671 (1.284–2.175) | |
| Uncertainty of fighting against the epidemic; Yes vs No | <0.001 | 0.502 (0.396–0.635) | |
| GAD-7 | |||
| Working department | 0.001 | ||
| Non-frontline vs frontline | 0.003 | 0.687 (0.536–0.879) | |
| Fangcang shelter hospitals vs frontline | 0.089 | 1.585 (0.932–2.695) | |
| Physical condition change worse; Yes vs No | <0.001 | 1.792 (1.376–2.333) | |
| Uncertainty of fighting against the epidemic; Yes vs No | <0.001 | 0.420 (0.330–0.535) | |
| Value of online psychological information; Yes vs No | 0.035 | 1.325 (1.020–1.721) | |
| ISI | |||
| Working department | <0.001 | ||
| Non-frontline vs frontline | 0.052 | 0.783 (0.611–1.002) | |
| Fangcang shelter hospitals vs frontline | <0.001 | 3.520 (2.008–6.169) | |
| Physical condition change worse; Yes vs No | 0.006 | 1.445 (1.110–1.880) | |
| Uncertainty of fighting against the epidemic; Yes vs No | <0.001 | 0.522 (0.409–0.668) | |
| Value of online psychological information; Yes vs No | 0.002 | 1.507 (1.162–1.955) | |
| IER-S | |||
| Working department | 0.015 | ||
| Non-frontline vs frontline | 0.014 | 0.690 (0.514–0.927) | |
| Fangcang shelter hospitals vs frontline | 0.282 | 1.392 (0.762–2.541) | |
| Physical condition change worse; Yes vs No | 0.003 | 1.567 (1.166–2.107) | |
| Uncertainty of fighting against the epidemic; Yes vs No | <0.001 | 0.371 (0.277–0.497) | |
| Value of online psychological information; Yes vs No | 0.004 | 1.556 (1.155–2.097) | |
| Sufficient protection conditions; Yes vs No | 0.002 | 1.813 (1.243–2.644) | |
Abbreviations: PHQ-9, the Patient Healthy Questionnaire; GAD-7, Generalized Anxiety Disorder; ISI, Insomnia Severity Index; IES-R, Impact of Events Scale-Revised.
4. Discussion
During the COVID-19 pandemic, everyone was exposed to great psychological stress, especially the health care workers. In this study, we focused on the effects of COVID-19 on the psychological distress of nurses in the epicenter, which is Wuhan, China. To our knowledge, this is the first report to investigate the dynamic changes of the psychological status of nurses during the COVID-19 pandemic. Our results showed that over one-third of the frontline nurses suffered symptomatic depression, anxiety, and insomnia, while over one-fifth presented with the symptoms of PTSD during the outbreak period; while these psychological problems declined to similar levels between the frontline and non-frontline nurses during the stable period with the improvements in the series of securities, such as living conditions, protection training, conditions and confidence, and online psychological consultation, among others. However, we should pay more attention to the nurses from the Fangcang shelter hospitals, since they continue to experience high levels of symptomatic distress during the stable period.
In our study, there were significant differences in marital status between two time points of the survey with more younger nurses (18–25 years old) in the outbreak period. More elder nurses were sent to fight the pandemic in the stable period because of normal off-work rotation. The proportion of married nurses in the stable period was higher than these in the outbreak. The married nurses were more likely to select solitary living to decrease the likelihood of infecting their families. Additionally, in the stable period, with the improvement of the above mentioned series of securities, more free apartments or hotels were offered for health care workers by the Chinese government and the private public welfare fund. These changes might bring better impacts on the psychological status of nurses, which was confirmed in our subsequent analysis.
The nurses in the outbreak period were more likely to display higher proportions of psychological distress, especially for the nurses from the frontline. This psychological distress had been demonstrated in several reports during the SARS 2003 outbreak (Maunder, 2004; Nickell et al., 2004). Recently, a survey study with a small sample size from a tertiary infectious disease hospital in China also showed higher incidence of anxiety and stress disorders among the health care workers under the COVID-19 pandemic (Huang et al., 2020). In the stable period, the proportion of nurses with psychological problems decreased significantly, while the psychological stress of nurses from the frontline were similar to the nurses from the non-frontline. The improvement in psychological states were also previously confirmed during the 2003 SARS pandemic (Su et al., 2007). Su et al. (2007) showed that the occurrence of psychiatric symptoms was linked to direct exposure to SARS patient care, previous mood disorder history, younger age, and perceived negative feelings. Having a positive coping attitude and strong social and family support might be protective factors against acute stress.
During the pandemic, we also investigated the independent impact factors for the psychological status of nurses using the logistic regression model. Among all the 13 related factors, the nurses from the frontline, with worse physical condition and uncertain concerns about this pandemic, were more likely to bear psychological problems based on the univariable and multivariable analysis. As the main powers that fight against COVID-19, most of the nurses are less than 40 years old, with limited experiences regarding the infectious pandemic and inadequate professional training from infectious or severe units; thus, inevitably leading to psychological problems. The online psychological information and sufficient protection conditions were helpful for acute stress. In China, Chen et al. (2020) developed a detailed psychological intervention plan to maintain mental health for health care workers in February 2020. Moreover, Kisely et al. (2020) reviewed the occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on health care workers. Their results showed the effective interventions for mitigating psychological distress for health care workers in an emerging disease outbreak, such as sufficient protective supplies, appropriate work shifts and regular breaks, identification of and responses to psychological problems, and psychological interventions, among others. In our hospital, we have been conducting a series of effective measures to alleviate the psychological pressure on nurses, especially for frontline nurses. First, our hospital guaranteed not only food and daily living supplies but also a place for rest. Second, we arranged trainings in disease knowledge and protective measures to protect them from infection. Third, the hospital developed detailed rules and standard protective measures and protocols. Additionally, each ward had a WeChat group on psychological counseling with psychological counselors. Health care workers could access the schedule of online balint groups, distance mindfulness cognitive behavioral therapy, and music helpful for improving sleep, among others. The telephone numbers of the psychological counselors were constantly broadcasted in the WeChat group. The psychological counselors regularly visited the rest area to listen to the difficulties or stories encountered by the staff at work, and provided them support accordingly. In our survey, over three-fifths of the nurses considered the online psychological consultation as effective. In the multivariable logistic regression analysis, the online psychological consultation was the independent factor for anxiety, insomnia, and PTSD symptoms.
In February 2020, the Fangcang shelter hospitals (Chen et al., 2020), which are large-scale temporary hospitals, were established to battle the COVID-19 outbreak for the first time in China. They have three key characteristics, which are rapid construction, massive scale, and low cost, making them particularly well-suited to address public health emergencies. The Fangcang shelter hospitals have been very successful so far in effectively blocking the spread of COVID-19 among the population. However, there were also plenty of difficulties and challenges in terms of the administration of Fangcang shelter hospitals, such as low health worker-to-patient ratio and heavy duties, caring for and sheltering a large number of patients, limited medical resources and activity spaces, completely new circumstance for the health care workers, and coordination of multiple medical teams from other local hospitals or other hospitals outside of Hubei provinces, among others. These situations aggravated work intensities and difficulties and increased the risk of psychological problems of nurses. Thus, we should pay more attention to the nurses working in Fangcang shelter hospitals who have higher psychosocial morbidity.
There are several limitations in our study. First, due to the pandemic, there was a possible bias in the enrollment of participants since we used online investigation. Second, the online investigation we conducted by WeChat may not be the best method for data collection, but it is indeed a safe and efficient way during this pandemic. Third, the differences of psychological status among doctors and other health care workers should be further evaluated. Fourth, the nurses were mainly from a single tertiary hospital, and the sample size of nurses from the Wuchang Fangcang shelter hospital was relatively small. Additionally, the influences of the pandemic on the psychological status of health care workers in the future need to be further investigated, especially for the nurses from Fangcang shelter hospitals.
5. Conclusions
In summary, our study indicates that more attention should be paid to the psychological status of nurses during the COVID-19 pandemic, especially for the nurses from the frontline. During this pandemic, it is necessary to take effective measures and interventions to minimize the psychological pressure of nurses, especially in the outbreak period. We recommend that nurses should have regular health assessments, psychological intervention, or necessary medications during the pandemic, which would have subsequent relevant impacts on the future, especially for the nurses working in Fangcang shelter hospitals.
Funding
This research was supported by the grants from the Fundamental Research Funds for the Central Universities (2042019kf0229), Medical Science Advancement Program of Wuhan University (TFLC2018001), and the National Key R&D Program of China (2018YFC1314600).
CRediT authorship contribution statement
Zhongxiang Cai: Conceptualization, Methodology, Validation, Formal analysis, Resources, Data curation, Supervision. Qin Cui: Validation, Formal analysis, Writing - original draft, Visualization. Zhongchun Liu: Methodology, Project administration, Funding acquisition. Juanjuan Li: Formal analysis, Investigation. Xuan Gong: Investigation, Resources, Project administration. Jingfang Liu: Investigation, Resources, Project administration. Zhiying Wan: Investigation, Resources. Xiaoping Yuan: Investigation, Resources. Xiaofen Li: Investigation, Resources. Chuang Chen: Conceptualization, Writing - review & editing, Visualization, Supervision, Funding acquisition. Gaohua Wang: Conceptualization, Writing - review & editing, Visualization, Supervision, Funding acquisition.
Declaration of competing interest
The author declared no conflict of interest.
Acknowledgements
The authors would like to thank the help of the health care workers for the distribution and assessment of the questionnaires.
References
- Cameron I.M., Crawford J.R., Lawton K., Reid I.C. Psychometric comparison of PHQ-9 and HADS for measuring depression severity in primary care. Br. J. Gen. Pract. 2008;58(546):32–36. doi: 10.3399/bjgp08X263794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Q., Liang M., Li Y., Guo J., Fei D., Wang L., He L., Sheng C., Cai Y., Li X., Wang J., Zhang Z. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7(4):E15–E16. doi: 10.1016/S2215-0366(20)30078-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen S., Zhang Z., Yang J., Wang J., Zhai X., Bärnighausen T., Wang C. Fangcang shelter hospitals: a novel concept for responding to public health emergencies. Lancet. 2020;395(10232):1305–1314. doi: 10.1016/S0140-6736(20)30744-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creamer M., Bell R., Failla S. Psychometric properties of the impact of event scale-revised. Behav. Res. Ther. 2003;41(12):1489–1496. doi: 10.1016/j.brat.2003.07.010. [DOI] [PubMed] [Google Scholar]
- Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Zhang L., Fan G., Xu J., Gu X., Cheng Z., Yu T., Xia J., Wei Y., Wu W., Xie X., Yin W., Li H., Liu M., Xiao Y., Gao H., Guo L., Xie J., Wang G., Jiang R., Gao Z., Jin Q., Wang J., Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang J.Z., Han M.F., Luo T.D., Ren A.K., Zhou X.P. Mental health survey of 230 medical staff in a tertiary infectious disease hospital for COVID-19. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi. 2020;38 doi: 10.3760/cma.j.cn121094-20200219-00063. (0), E001. [DOI] [PubMed] [Google Scholar]
- Jernigan D.B., CollectiveName : CDC Covid-19 Response Team Update: public health response to the coronavirus disease 2019 outbreak-United States, february 24, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020;69(8):216–219. doi: 10.15585/mmwr.mm6908e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kisely S., Warren N., McMahon L., Dalais C., Henry I., Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ. 2020;369:m1642. doi: 10.1136/bmj.m1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Löwe B., Kroenke K., Herzog W., Gräfe K. Measuring depression outcome with a brief self-report instrument: sensitivity to change of the Patient Health Questionnaire (PHQ-9) J. Affect. Disord. 2004;81(1):61–66. doi: 10.1016/S0165-0327(03)00198-8. [DOI] [PubMed] [Google Scholar]
- Maunder R. The experience of the 2003 SARS outbreak as a traumatic stress among frontline healthcare workers in Toronto: lessons learned. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2004;359(1447):1117–1125. doi: 10.1098/rstb.2004.1483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morin C.M., Belleville G., Bélanger L., Ivers H. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep (Basel) 2011;34(5):601–608. doi: 10.1093/sleep/34.5.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nickell L.A., Crighton E.J., Tracy C.S., Al-Enazy H., Bolaji Y., Hanjrah S., Hussain A., Makhlouf S., Upshur R.E. Psychosocial effects of SARS on hospital staff: survey of a large tertiary care institution. CMAJ (Can. Med. Assoc. J.) 2004;170(5):793–798. doi: 10.1503/cmaj.1031077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Novel Coronavirus Pneumonia Emergency Response Epidemiology Team The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Zhonghua Liuxingbingxue Zazhi. 2020;41(2):145–151. [Google Scholar]
- Oh N., Hong N., Ryu D.H., Bae S.G., Kam S., Kim K.Y. Exploring nursing intention, stress, and professionalism in response to infectious disease emergencies: the experience of local public hospital nurses during the 2015 MERS outbreak in South Korea. Asian Nurs. Res. 2017;11(3):230–236. doi: 10.1016/j.anr.2017.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park J.S., Lee E.H., Park N.R., Choi Y.H. Mental health of nurses working at a government-designated hospital during a MERS-CoV outbreak: a cross-sectional study. Arch. Psychiatr. Nurs. 2018;32(1):2–6. doi: 10.1016/j.apnu.2017.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peeri N.C., Shrestha N., Rahman M.S., Zaki R., Tan Z., Bibi S., Baghbanzadeh M., Aghamohammadi N., Zhang W., Haque U. The SARS, MERS and novel coronavirus (COVID-19) epidemics, the newest and biggest global health threats: what lessons have we learned? Int. J. Epidemiol. 2020:1–10. doi: 10.1093/ije/dyaa033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Su T.P., Lien T.C., Yang C.Y., Su Y.L., Wang J.H., Tsai S.L., Yin J.C. Prevalence of psychiatric morbidity and psychological adaptation of the nurses in a structured SARS caring unit during outbreak: a prospective and periodic assessment study in Taiwan. J. Psychiatr. Res. 2007;41(1–2):119–130. doi: 10.1016/j.jpsychires.2005.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swinson R.P. The GAD-7 scale was accurate for diagnosing generalised anxiety disorder. Evid. Base Med. 2006;11(6):184. doi: 10.1136/ebm.11.6.184. [DOI] [PubMed] [Google Scholar]
- Zhu N., Zhang D., Wang W., Li X., Yang B., Song J., Zhao X., Huang B., Shi W., Lu R., Niu P., Zhan F., Ma X., Wang D., Xu W., Wu G., Gao G.F., Tan W., CollectiveName: China Novel Coronavirus Investigating and Research Team A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 2020;382(8):727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]