Highlights
-
•
Young adult COVID-19 patient presented with acute abdomen.
-
•
Evaluation of patient revealed splenomegaly, splenic rupture and hemoperitoneum.
-
•
Patient recover with conservative management.
Keywords: COVID-19, Splenic infarction, Spontaneous hemoperitoneum, Acute abdomen
Abstract
Introduction
Coronavirus disease (COVID-19) is a global a pandemic caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Patients commonly present with respiratory tract symptoms and fever. However two third are asymptomatic and unusual presentation is evolving. This has cause management dilemma among physicians.
Presentation of case
A 35 year young otherwise healthy male presented to emergency department of this institute with fever of 103 °F, abdominal pain, and pancytopenia with progressive fall in hemoglobin level was tested positive for COVID-19. Contrast enhance computed tomography of the patient revealed hemoperitoneum with splenic infarct. He was admitted in intensive care unit and managed with supportive treatment.
Discussion
Respiratory and gastrointestinal symptoms with hematological abnormalities like lymphopenia, thrombocytopenia are common presentation of COVID-19. Although coagulopathy and vasculitis has been a well-documented entity in patients with COIVD-19, visceral infarction leading to spontaneous hemoperitoeum was unusual and rare clinical presentation.
Conclusion
A high degree of clinical suspicion and thorough evaluation helps in the diagnosis of COVID-19 and related complications. The management of cases with unusual presentation requires judicious and careful approach.
1. Introduction
Severe acute respiratory syndrome Coronavirus-2 (SARS-CoV-2) infection has emerged as Corona virus disease-2019 (COVID-19) pandemic [1]. Most of the infected patients remain asymptomatic or experience mild to moderate respiratory illness and recover without special treatment [2,3]. With the rise in COVID-19 confirmed cases, patient are getting admitted in hospital with atypical presentation. Atypical modes of presentation can cause not only in delayed diagnosis but is also a potential threat to infection prevention and control [4].
Spontaneous hemoperitoneum is a life threatening condition that usually occurs in patients with known coagulation disorder or under anticoagulants [5]. Vasculitis, a defined entity in COVID-19 patients has been associated with multiple visceral infarct but concomitant massive hemoperitoneum has been scarcely described. This rare but life threatening form of acute abdomen depicts another spectrum of this global pandemic. We report here a rare case presentation of spontaneous hemoperitoneum and splenic infarct in COVID-19 according to SCARE guideline [6].
2. Case report
32years old serving soldier with no known co-morbidities presented in emergency department (ED) of our institute with fever for 6 days. The fever was associated with chills and rigors. He did not complained of cough, shortness of breath, myalgia, diarrhea and vomiting. He had no history of travel out of duty station in last two months and no history of contact with COVID-19 confirmed cases. He denied history of trauma and drug intake. He was non-smoker, non-alcoholic, and had no known personal or family history of bleeding and coagulation disorders. He was evaluated in ED by attending consultant physician and surgeon on duty. He was admitted in COVID-19 isolation ward and subjected to thorough clinical, laboratory and imaging studies. The maximum temperature recorded was 103 °F, blood pressure was 110/70 mmHg, and oxygen saturation in room air was 92%. His blood parameters showed leucopenia and thrombocytopenia with near normal blood hemoglobin level (Table 1). Rest of the blood biochemistry, liver enzymes, coagulation profile (prothrombin time, D-dimer) was within normal limit. Chest X-ray did not show any abnormality. His nasopharyngeal swab specimen was tested positive for SARS-COv-2. He was under symptomatic treatment for fever. The urine and blood sample send for culture showed no growth of organism. On the third day of admission his cell counts tend to normalize but there was progressive fall in blood hemoglobin level from 14.1 gm/dl to 7.3 gm/dl.
Table 1.
Hematological parameter of the patient.
| Parameters | 08/08/020 | 09/08/020 | 10/08/020 | 11/08/020 |
|---|---|---|---|---|
| Hemoglobin (gm %) | 14.1 | 13.5 | 9.4 | 7.3 |
| Platelets (per cu mm) | 50000 | 55000 | 100000 | 150000 |
| TLC (per cu mm) | 2900 | 4800 | 5000 | 5400 |
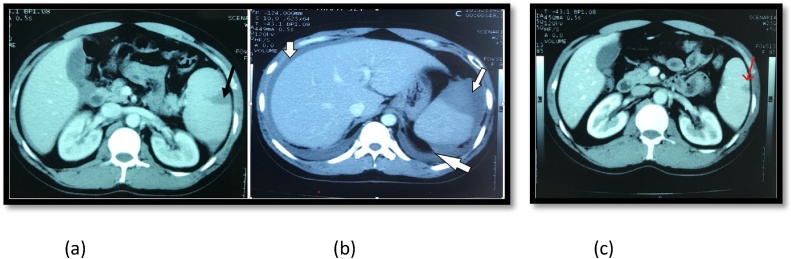
On the same day patient complained of moderate to severe periumbilical pain without features of peritonitis. Abdominal ultrasound showed intraperitoneal collection in perisplenic space. Contrast computed tomography study (CECT-abdomen pelvis) images revealed contrast extravasation from breached capsule in upper pole of spleen during porto-venous phase, which is suggestive of infarct laceration of splenic. Cranio-caudally the spleen measure 14 cm and splenic index is 1048. There was moderate intraperitoneal collection localized in perisplenic space, perihepatic space and pelvic cavity (Fig. 1a & b). Patient developed generalized maculopapular rash without itching (Fig. 2). He was transferred to COVID-19 intensive care unit (ICU) with monitoring of vitals, urine output and serial hemoglobin and was transfused with three unit of packed RBC. Besides, he was given symptomatic and supportive care. Our patient remain clinically stable during ICU admission and the hemoperitoneum resolved spontaneously on 7th day of admission (Fig. 1c).
Fig. 1.
CT findings of the patient shwoning.
a) Spleenic infarct laceration b) hemoperitoneum c) resolved infarction rupture.
Fig. 2.

Dermatological menifestation of the patient.
3. Discussion
Fever, cough, and myalgia are three most common symptoms of COVID-19 [7]. 30–40% of COVID-19 patient are asymptomatic [8]. Thromboembolic phenomenon is common event in this disease. However, spontaneous hemoperitoneum is a rarely reported. Lymphocytic endothelitis within lungs, kidney, heart, intestine and liver has been reported in COVID-19 cases. In these patients vasculitis could be result of viral infiltration of endothelium or result of immune reaction that leads to leucocytoclastic vasculitis. The pathological appearance shows lymphocytic infiltration within the vessels, hyperplasia of small vessels with thickening and stenosis [[9], [10], [11]].
COVID-19 disease is also associated with thrombocytopenia and coagulopathy and in severe form develops disseminated intravascular coagulation (DIC). Studies have shown that severe lymphopenia and elevation of D-dimer is associated with high mortality and represents inappropriate activation of coagulation leading to DIC [12,13]. COVID-19 has non-specific dermatological manifestation like maculopapular, urticarial, and vesicular eruptions and transient livedo reticularis [14]. Thromboembolic complications including acute stroke and pulmonary embolism has been reported in young patient [15,16]. Visceral infarction has been previously described in COVID-19 patients with previous cardiac events and involved spleen, kidney and small bowel [17]. The COVID-19 patient treated with anticoagulants were at high risk of bleeding complications. Radiological embolization was choice of intervention in such events [18]. Hemoperitoneum with substantial drop in hemoglobin due to spontaneous intraperitoneal hemorrhage could be the newer presentation of same disease spectrum.
4. Conclusion
Abdominal pain in COVID-19 patient requires further evaluation to rule out visceral infarct. Prothrombotic condition in COVID-19 has important implication in its clinical presentation, and management including judicious use of thrombolytic therapy. Vasculitis and small vessel thrombosis resulting in infarct laceration and hemoperitoneum could be self-limiting events.
Declaration of Competing Interest
None.
Funding
None.
Ethical approval
Not applicable/exempt from ethical review committee of Nepalese Army Institute of Health Sciences for case reports.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
All authors have contributed equally for data collections, writing and editing.
Registration of research studies
N/A.
Guarantor
Bikash Bikram Thapa MBBS, MS, MSPH.
Saurab Karki MBBS, MS.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Contributor Information
Saurab Karki, Email: saurab.karki@naihs.edu.np.
Sushil Bahadur Rawal, Email: sushil.rawal@naihs.edu.np.
Srijan Malla, Email: srijan.malla@naihs.edu.np.
Jyoti Rayamajhi, Email: jyoti.rayamajhi@naihs.edu.np.
Bikash Bikram Thapa, Email: bikashbikram.thapa@naihs.edu.np.
References
- 1.Weiss P., Murdoch D.R. Clinical course and mortality risk of severe COVID-19. Lancet. 2020;395(10229):1014–1015. doi: 10.1016/S0140-6736(20)30633-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Adhikari S.P., Meng S., Wu Y.J., Mao Y.P., Ye R.X., Wang Q.Z., Sun C., Sylvia S., Rozelle S., Raat H., Zhou H. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: a scoping review. Infect. Dis. Poverty. 2020;9(1):29. doi: 10.1186/s40249-020-00646-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Zhang L., Fan G., Xu J., Gu X., Cheng Z., Yu T., Xia J., Wei Y., Wu W., Xie X., Yin W., Li H., Liu M., Xiao Y., Gao H., Guo L., Xie J., Wang G., Jiang R., Gao Z., Jin Q., Wang J., Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guarneri C., Rullo E.V., Pavone P., Berretta M., Ceccarelli M., Natale A., Nunnari G. Silent COVID-19: what your skin can reveal. Lancet Infect. Dis. 2020 doi: 10.1016/S1473-3099(20)30402-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Freeman B.B., Critchlow J.F., Cohen S., Edlow J.A. Spontaneous intraperitoneal hemorrhage as the initial presentation of a gastrointestinal stromal tumor: a case report. Int. J. Emerg. Med. 2010;3(1):53–56. doi: 10.1007/s12245-009-0141-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Agha R.A., Borrelli M.R., Farwana R., Koshy K., Fowler A.J., Orgill D.P. The SCARE 2018 statement: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2018;60:132–136. doi: 10.1016/j.ijsu.2018.10.028. [DOI] [PubMed] [Google Scholar]
- 7.Stokes E.K., Zambrano L.D., Anderson K.N., Marder E.P., Raz K.M., El Burai Felix S., Tie Y., Fullerton K.E. Coronavirus disease 2019 case surveillance - United States, January 22-May 30, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020;69(24):759–765. doi: 10.15585/mmwr.mm6924e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Oran D.P., Topol E.J. Prevalence of asymptomatic SARS-CoV-2 infection: a narrative review. Ann. Intern. Med. 2020;173(5):362–367. doi: 10.7326/M20-3012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Roncati L., Ligabue G., Fabbiani L., Malagoli C., Gallo G., Lusenti B., Nasillo V., Manenti A., Maiorana A. Type 3 hypersensitivity in COVID-19 vasculitis. Clin. Immunol. 2020;217:108487. doi: 10.1016/j.clim.2020.108487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Becker R.C. COVID-19-associated vasculitis and vasculopathy. J. Thromb. Thrombolysis. 2020 doi: 10.1007/s11239-020-02230-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bradley B.T., Maioli H., Johnston R., Chaudhry I., Fink S.L., Xu H., Najafian B., Deutsch G., Lacy J.M., Williams T., Yarid N., Marshall D.A. Histopathology and ultrastructural findings of fatal COVID-19 infections in Washington State: a case series. Lancet. 2020;396(10247):320–332. doi: 10.1016/S0140-6736(20)31305-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lippi G., Plebani M., Henry B.M. Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: a meta-analysis. Clin. Chim. Acta. 2020;506:145–148. doi: 10.1016/j.cca.2020.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tang N., Li D., Wang X., Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J. Thromb. Haemost. 2020;18(4):844–847. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Galvan Casas C., Catala A., Carretero Hernandez G., Rodriguez-Jimenez P., Fernandez-Nieto D., Rodriguez-Villa Lario A., Navarro Fernandez I., Ruiz-Villaverde R., Falkenhain-Lopez D., Llamas Velasco M., Garcia-Gavin J., Baniandres O., Gonzalez-Cruz C., Morillas-Lahuerta V., Cubiro X., Figueras Nart I., Selda-Enriquez G., Romani J., Fusta-Novell X., Melian-Olivera A., Roncero Riesco M., Burgos-Blasco P., Sola Ortigosa J., Feito Rodriguez M., Garcia-Doval I. Classification of the cutaneous manifestations of COVID-19: a rapid prospective nationwide consensus study in Spain with 375 cases. Br. J. Dermatol. 2020;183(1):71–77. doi: 10.1111/bjd.19163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Danzi G.B., Loffi M., Galeazzi G., Gherbesi E. Acute pulmonary embolism and COVID-19 pneumonia: a random association? Eur. Heart J. 2020;41(19):1858. doi: 10.1093/eurheartj/ehaa254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Oxley T.J., Mocco J., Majidi S., Kellner C.P., Shoirah H., Singh I.P., De Leacy R.A., Shigematsu T., Ladner T.R., Yaeger K.A., Skliut M., Weinberger J., Dangayach N.S., Bederson J.B., Tuhrim S., Fifi J.T. Large-vessel stroke as a presenting feature of Covid-19 in the young. N. Engl. J. Med. 2020;382(20):e60. doi: 10.1056/NEJMc2009787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Besutti G., Bonacini R., Iotti V., Marini G., Riva N., Dolci G., Maiorana M., Spaggiari L., Monelli F., Ligabue G., Guaraldi G., Rossi P.G., Pattacini P., Massari M. Abdominal visceral infarction in 3 patients with COVID-19. Emerg. Infect. Dis. 2020;26(8):1926–1928. doi: 10.3201/eid2608.201161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Conti C.B., Henchi S., Coppeta G.P., Testa S., Grassia R. Bleeding in COVID-19 severe pneumonia: the other side of abnormal coagulation pattern? Eur. J. Intern. Med. 2020;77:147–149. doi: 10.1016/j.ejim.2020.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]