This cross-sectional study evaluates the prevalence and sociodemographic disparities in influenza vaccination among a nationally representative sample of individuals with atherosclerotic cardiovascular disease.
Key Points
Question
What are the prevalence of and sociodemographic differences in influenza vaccination among a nationally representative sample of individuals with atherosclerotic cardiovascular disease?
Findings
In this cross-sectional study of 19 793 US adults with atherosclerotic cardiovascular disease, 32.7% lacked influenza vaccination with statistically significant higher proportions observed among high-risk groups based on younger age, non-Hispanic Black race/ethnicity, low family income, lack of insurance, lower level of education, and lack of usual source of care.
Meaning
Many US adults with established atherosclerotic cardiovascular disease lack influenza vaccination with significant disparities existing based on high-risk sociodemographic characteristics.
Abstract
Importance
Atherosclerotic cardiovascular disease (ASCVD) remains a leading cause of death and disability in the US and worldwide. Influenza vaccination has shown to decrease overall morbidity, mortality, severity of infection, and hospital readmissions among these individuals. However, national estimates of influenza vaccination among individuals with ASCVD in the US are not well studied.
Objective
To evaluate the prevalence of and sociodemographic disparities in influenza vaccination among a nationally representative sample of individuals with ASCVD.
Design, Setting, and Participants
Pooled Medical Expenditure Panel Survey data from 2008 to 2016 were used and included adults 40 years or older with ASCVD. Participants’ ASCVD status was ascertained via self-report and/or International Classification of Diseases, Ninth Revision diagnosis of coronary heart disease, peripheral artery disease, and/or cerebrovascular disease. Analysis began April 2020.
Main Outcomes and Measures
Prevalence and characteristics of adults with ASCVD who lacked influenza vaccination during the past year. Covariates including age, sex, race/ethnicity, family income, insurance status, education level, and usual source of care were assessed.
Results
Of 131 881 adults, 19 793 (15.7%) had ASCVD, corresponding to 22.8 million US adults annually. A total of 7028 adults with ASCVD (32.7%), representing 7.4 million adults, lacked influenza vaccination. The highest odds of lacking vaccination were observed among individuals aged 40 to 64 years (odds ratio [OR], 2.32; 95% CI, 2.06-2.62), without a usual source of care (OR, 2.00; 95% CI, 1.71-2.33), without insurance (OR, 2.05; 95% CI, 1.63-2.58), with a lower education level (OR, 1. 25; 95% CI, 1.12-1.40), with a lower income level (OR, 1.14; 95% CI, 1.01-1.27), and of non-Hispanic Black race/ethnicity (OR, 1.24, 95% CI, 1.10-1.41). A stepwise increase was found in the prevalence and odds of lacking influenza vaccination among individuals with increase in high-risk characteristics. Overall, 1171 individuals (59.7%; 95% CI, 55.8%-63.5%) with 4 or more high-risk characteristics and ASCVD (representing 732 524 US adults annually) reported lack of influenza vaccination (OR, 6.06; 95% CI, 4.88-7.53).
Conclusion and Relevance
Despite current recommendations, a large proportion of US adults with established ASCVD lack influenza vaccination, with several sociodemographic subgroups having greater risk. Focused public health initiatives are needed to increase access to influenza vaccinations for high-risk and underserved populations.
Introduction
Atherosclerotic cardiovascular disease (ASCVD) remains a leading cause of death and disability in the US and worldwide.1 Influenza infection contributes to cardiovascular morbidity and mortality along with an increase in cardiovascular hospitalizations among those with established ASCVD.2,3 Several mechanisms have been proposed to explain cardiovascular outcomes such as acute coronary syndrome, which includes increased risk of plaque rupture, coronary thrombosis during the prothrombotic state of infection, and demand ischemia from increased metabolic needs due to catabolic state of infection.4 Influenza vaccination has been shown to decrease overall morbidity, mortality, severity of infection, and hospital readmissions among individuals with ASCVD.5,6,7 Accordingly, the American Heart Association and the American College of Cardiology provided guidance on the use of vaccination against influenza for secondary prevention among individuals with ASCVD (class I, level B).8 Moreover, the US Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices has recommended influenza vaccination for adults with heart disease for several decades.9 To date, national estimates of vaccination among individuals with ASCVD in the US are not well studied. In this study, among a nationally representative sample of adults with ASCVD, we report estimates of influenza vaccination, characterizing sociodemographic groups, both individually and in combination, that are at greater risk of lacking influenza vaccination.
Methods
Data Source
We included adults 40 years or older with ASCVD using pooled Medical Expenditure Panel Survey (MEPS) data from 2008 to 2016. MEPS is sponsored by the Agency for Healthcare Research and Quality, which provides the most complete national data on health care costs, health care utilization, and health insurance coverage.10 Because MEPS data are deidentified and publicly available, this study was exempt from review by the institutional review board committee.
Study Variables
Participants’ ASCVD status was ascertained from a self-reported and/or International Classification of Diseases, Ninth Revision diagnosis of coronary heart disease, peripheral artery disease, and/or cerebrovascular disease. Influenza vaccination status was self-reported, and individuals were ascertained to have had influenza vaccination if they answered yes to having received the vaccination in the 12 months prior to survey completion. Other covariates included in the study were age (40-65 years and ≥65 years), sex, race/ethnicity (non-Hispanic White, non-Hispanic Black, non-Hispanic Asian, and Hispanic), family income (as a proportion of federal poverty limit; high/middle income [≥200%] and low/poor income [<200%]), insurance status (insured and uninsured), education level (≥some college education and ≤high school), and usual source of care.
Statistical Analysis
We used the person-level sampling weights that were obtained after adjusting for nonresponse, age, sex, and race/ethnicity (based on population estimates from the US Census Bureau) to obtain nationally representative results. We compared the survey-weighted proportions of influenza vaccination across different sociodemographic characteristics using Rao-Scott χ2 analysis. We assessed the association of sociodemographic characteristics with influenza vaccination using multivariable survey-specific logistic regression adjusting for the above-mentioned covariates and reported the adjusted odds ratios (ORs) with 95% CIs. To analyze the cumulative associations between these characteristics and influenza vaccination, we developed a composite model of high-risk characteristics including the following 6 variables: age (ie, 40-64 years), race/ethnicity (ie, non-Hispanic Black), education level (ie, ≤high school), insurance status (ie, uninsured), income level (ie, low- or lowest-income subgroups), and lack of usual source of care. For our analyses, we considered P values less than .05 to be statistically significant a priori and all statistical tests were 2-tailed. All analyses were performed using Stata version 14.0 (StataCorp). Analysis began April 2020.
Results
Of 131 881 adults, 19 793 (15.7%) in our study population had ASCVD, corresponding to 22.8 million US adults annually. Nearly 1 in 3 adults with ASCVD (7028 [32.7%]), representing 7.4 million adults, reported not receiving an influenza vaccination during the past year. A lack of vaccination was significantly higher among adults aged 40 to 64 years (4186 [46.4%]), non-Hispanic Black (1776 [40.8%]) and Hispanic (1360 [39.9%]) individuals, those without a usual source of care (981 [56.6%]), individuals without insurance coverage (891 [64.9%]), those of lower family income level (3590 [35.1%]), and those with a lower level of completed education (4420 [34.4%]), when compared with each subgroup’s relative reference group (Table). Differences in influenza vaccination uptake remained statistically significant after accounting for all sociodemographic covariates and potential confounders. On an adjusted analysis, the highest odds of lacking vaccination were observed among individuals aged 40 to 64 years (OR, 2.32; 95% CI, 2.06-2.62), individuals without a usual source of care (OR, 2.00; 95% CI, 1.71-2.33), uninsured individuals (OR, 2.05; 95% CI, 1.63-2.58), those with a lower level of completed education (OR, 1.25; 95% CI, 1.12-1.40), those with a lower income level (OR, 1.14; 95% CI, 1.01-1.27), and non-Hispanic Black adults (OR, 1.24, 95% CI, 1.10-1.41). There was no significant difference in vaccination by geographic region (Table).
Table. Prevalence and Distribution of Influenza Vaccination by Patient Characteristics Among Individuals With ASCVD.
| Characteristics | Total No. | Not vaccinated | |||
|---|---|---|---|---|---|
| No. | Weighted prevalence, % | Estimated US population | OR (95% CI)a | ||
| Total population | 19 793 | 7028 | 32.7 | 7 437 189 | NA |
| Age category, y | |||||
| ≥65 | 10 996 | 2842 | 23.7 | 3 263 511 | 1 [Reference] |
| 40-64 | 8787 | 4186 | 46.4 | 4 173 678 | 2.32 (2.06-2.62) |
| Sex | |||||
| Female | 9933 | 3534 | 32.1 | 3 412 762 | 1 [Reference] |
| Male | 9860 | 3494 | 33.2 | 4 024 427 | 0.99 (0.90-1.10) |
| Race/ethnicityb | |||||
| Non-Hispanic White | 10 919 | 3452 | 30.5 | 5 273 282 | 1 [Reference] |
| Non-Hispanic Black | 4245 | 1776 | 40.8 | 994 897 | 1.24 (1.10-1.41) |
| Non-Hispanic Asian | 779 | 228 | 30.5 | 167 502 | 0.82 (0.60-1.12) |
| Hispanic | 3331 | 1360 | 39.9 | 773 076 | 1.03 (0.88-1.22) |
| Family income | |||||
| Middle/high | 10 277 | 3438 | 31.2 | 4 387 358 | 1 [Reference] |
| Low | 9516 | 3590 | 35.1 | 3 049 831 | 1.14 (1.01-1.27) |
| Insurance status | |||||
| Insured | 18 421 | 6137 | 31.0 | 6 712 468 | 1 [Reference] |
| Uninsured | 1372 | 891 | 64.9 | 724 721 | 2.05 (1.63-2.58) |
| Education levelb | |||||
| ≥Some college | 7567 | 2537 | 30.5 | 3 093 802 | 1 [Reference] |
| ≤High school | 12 053 | 4420 | 34.4 | 4 297 964 | 1.25 (1.12-1.40) |
| Usual source of careb | |||||
| Yes | 17 847 | 5917 | 30.8 | 904 797 | 1 [Reference] |
| No | 1649 | 981 | 56.6 | 6 485 839 | 2.00 (1.71-2.33) |
| Region | |||||
| Northeast | 3288 | 1060 | 29.6 | 1 235 355 | 1 [Reference] |
| Midwest | 4098 | 1399 | 31.4 | 1 627 660 | 1.07 (0.88-1.29) |
| South | 8379 | 3204 | 34.6 | 3 149 798 | 1.13 (0.97-1.32) |
| West | 4028 | 1365 | 33.1 | 1 424 376 | 1.13 (0.93-1.38) |
Abbreviations: ASCVD, atherosclerotic cardiovascular disease; NA, not applicable; OR, odds ratio.
Model adjusted for age, sex, race/ethnicity, family income, insurance status, education, geographic region, usual source of care, cardiovascular risk factors, and comorbidities.
Counts may not add to total owing to missing values.
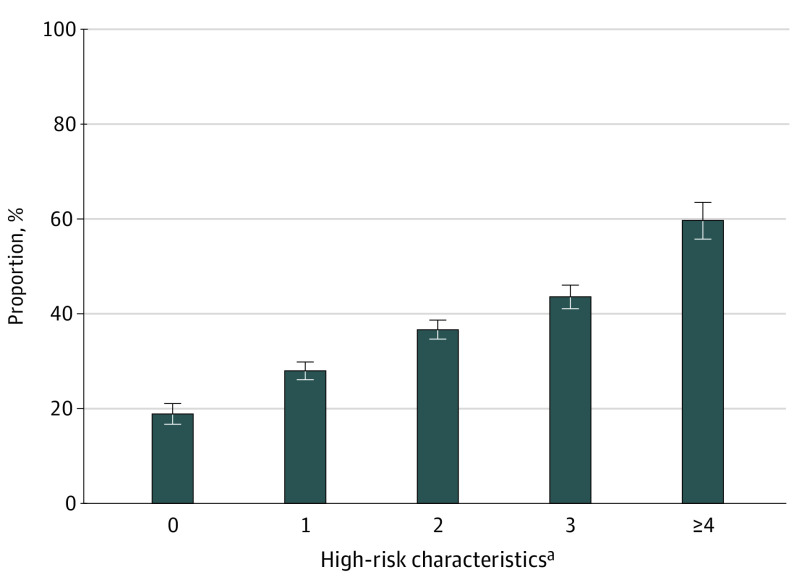
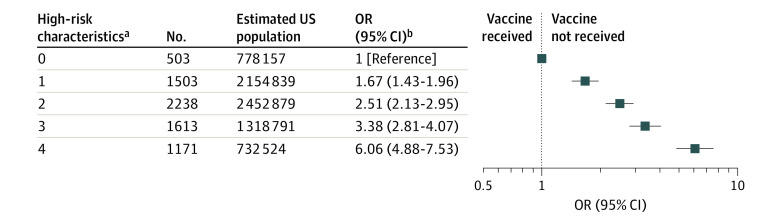
On further analysis of the association of high-risk characteristics with influenza vaccination, when compared with the reference group with no high-risk characteristics (non-Hispanic White individuals aged ≥65 years who had insurance, had a higher education level, had a usual source of care, and belonged to middle-/high-income subgroup), those with 1, 2, 3, and 4 or more high-risk characteristics had a stepwise increase in lack of influenza vaccination (Figure 1). Among adults with 4 or more high-risk characteristics, 1171 (59.7%; 95% CI, 55.8%-63.5%) lacked influenza vaccination, representing 732 524 US adults with ASCVD annually, compared with 503 (18.9%; 95% CI, 16.8%-21.1%) in the reference group. Using multivariable logistic regression, we found that adults with 4 or more high-risk characteristics had nearly 6-fold higher odds (OR, 6.06; 95% CI, 4.88-7.53) of lacking vaccination compared with individuals without any high-risk characteristics (Figure 2). Moreover, adults with 2 high-risk characteristics had nearly 2.5-fold greater odds of lacking vaccination (OR, 2.51; 95% CI, 2.13-2.95), representing approximately 2.4 million US adults with ASCVD annually.
Figure 1. Weighted Proportions and Variations in Lacking Influenza Vaccination Among Adults With Atherosclerotic Cardiovascular Disease Stratified by the Cumulative Number of High-risk Sociodemographic Characteristics.
A stepwise increase in the prevalence of lacking influenza vaccination with increasing high-risk characteristics is noted. Nearly 3 in 5 individuals with 4 or more high-risk characteristics reported lacking influenza vaccination. Error bars indicate 95% CIs.
aHigh-risk characteristics include age 40 to 64 years, non-Hispanic Black race/ethnicity, low/poor family income, uninsured, lack of usual source of care, and high school education level or less.
Figure 2. National Estimates and ORs of Lacking Influenza Vaccination Among Adults With Atherosclerotic Cardiovascular Disease and High-risk Sociodemographic Characteristics.
A stepwise increase in the odds of lacking influenza vaccination with increasing high-risk characteristics was noted. Individuals with 4 or more high-risk characteristics had nearly 6-fold higher odds of lacking influenza vaccination.
aHigh-risk characteristics include age 40 to 64 years, non-Hispanic Black race/ethnicity, low/poor family income, uninsured, lack of usual source of care, and high school education level or less.
bModel adjusted for sex, geographic region, cardiovascular risk factors, and comorbidities. Odds ratios (ORs) and 95% CIs are presented on a log scale.
Discussion
While previous studies have shown significant disparities in influenza vaccination access and uptake,11,12,13 this is the first study to our knowledge that has assessed the prevalence of and sociodemographic disparities in vaccination among a nationally representative sample of adults with ASCVD. In the present cross-sectional study, nearly 1 in 3 adults in the US with established ASCVD, representing approximately 7.4 million adults annually, lacked influenza vaccination. This proportion was significantly higher based on younger age, non-Hispanic Black race/ethnicity, low family income, lack of insurance coverage, lower level of education, and no usual source of care. We found that nearly 3 of 5 adults with 4 or more of these high-risk characteristics lacked vaccination in the last 12 months.
Considering the recent emergence of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2),14 it is imperative to enhance influenza vaccination uptake in higher-risk patients with ASCVD to reduce risk of coinfection and significant adverse outcomes. Recognizing the subgroup of individuals that are at the highest risk of adverse outcomes is germane to design optimal health care policies and/or campaigns specifically tailored for overcoming these care gaps. Interestingly, we noticed a 2-fold higher odds of lacking influenza vaccination among adults aged 40 to 64 years with ASCVD. Patients and clinicians are likely to perceive a lower risk of influenza in a younger population compared with an older population with ASCVD, and this false sense of security could potentially explain the lower vaccination rates among the younger population. With the recent data showing an overall stagnation in the decline of premature heart disease mortality rates among adults younger than 65 years, our findings underscore the importance of patients and clinicians to recognize the risks associated with lacking influenza vaccination among a younger population.15 Additionally, these data illuminate groups that are at higher risk for not receiving influenza vaccination and may also inform future efforts for more targeted public health approaches for future coronavirus disease 2019 (COVID-19) vaccination outreach among high-risk populations such as those with established ASCVD.
Limitations
These results should be interpreted considering the following limitations. First, the cross-sectional nature of MEPS data limits the ability to assess causal relationships between sociodemographic characteristics and influenza vaccination within the past year. The possibility of a bilateral relationship in which individuals’ socioeconomic and environmental circumstances may inhibit access to health care services such as vaccination and that resulting poor health can influence future financial status cannot be discounted. Second, it is worth noting that the presence or absence of influenza vaccination has highly confounded the observational analyses associating influenza vaccination with lower incidence of cardiovascular events. Therefore, well-powered randomized clinical trials, such as the upcoming INVESTED trial (NCT02787044), are critical to evaluate the protective effect of influenza vaccination on cardiovascular events.
Conclusions
In conclusion, nationally, nearly one-third of adults with ASCVD lacked influenza vaccination with disproportionately higher rates observed among vulnerable sociodemographic groups. These results underscore the importance of focused public health interventions and awareness efforts aimed at increasing access to and use of influenza vaccinations among these higher-risk subgroups with underlying cardiovascular conditions.
References
- 1.Benjamin EJ, Blaha MJ, Chiuve SE, et al. ; American Heart Association Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics-2017 update: a report from the American Heart Association. Circulation. 2017;135(10):e146-e603. doi: 10.1161/CIR.0000000000000485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nguyen JL, Yang W, Ito K, Matte TD, Shaman J, Kinney PL. Seasonal influenza infections and cardiovascular disease mortality. JAMA Cardiol. 2016;1(3):274-281. doi: 10.1001/jamacardio.2016.0433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thompson WW, Shay DK, Weintraub E, et al. Influenza-associated hospitalizations in the United States. JAMA. 2004;292(11):1333-1340. doi: 10.1001/jama.292.11.1333 [DOI] [PubMed] [Google Scholar]
- 4.MacIntyre CR, Mahimbo A, Moa AM, Barnes M. Influenza vaccine as a coronary intervention for prevention of myocardial infarction. Heart. 2016;102(24):1953-1956. doi: 10.1136/heartjnl-2016-309983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Siscovick DS, Raghunathan TE, Lin D, et al. Influenza vaccination and the risk of primary cardiac arrest. Am J Epidemiol. 2000;152(7):674-677. doi: 10.1093/aje/152.7.674 [DOI] [PubMed] [Google Scholar]
- 6.Lavallée P, Perchaud V, Gautier-Bertrand M, Grabli D, Amarenco P. Association between influenza vaccination and reduced risk of brain infarction. Stroke. 2002;33(2):513-518. doi: 10.1161/hs0202.102328 [DOI] [PubMed] [Google Scholar]
- 7.Naghavi M, Barlas Z, Siadaty S, Naguib S, Madjid M, Casscells W. Association of influenza vaccination and reduced risk of recurrent myocardial infarction. Circulation. 2000;102(25):3039-3045. doi: 10.1161/01.CIR.102.25.3039 [DOI] [PubMed] [Google Scholar]
- 8.Davis MM, Taubert K, Benin AL, et al. ; American Heart Association; American College of Cardiology . Influenza vaccination as secondary prevention for cardiovascular disease: a science advisory from the American Heart Association/American College of Cardiology. Circulation. 2006;114(14):1549-1553. doi: 10.1161/CIRCULATIONAHA.106.178242 [DOI] [PubMed] [Google Scholar]
- 9.Grohskopf LA, Alyanak E, Broder KR, Walter EB, Fry AM, Jernigan DB. Prevention and control of seasonal influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices: United States, 2019-20 influenza season. MMWR Recomm Rep. 2019;68(3):1-21. doi: 10.15585/mmwr.rr6803a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Remschmidt C, Wichmann O, Harder T. Influenza vaccination in patients with end-stage renal disease: systematic review and assessment of quality of evidence related to vaccine efficacy, effectiveness, and safety. BMC Med. 2014;12:244. doi: 10.1186/s12916-014-0244-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Logan JL. Disparities in influenza immunization among US adults. J Natl Med Assoc. 2009;101(2):161-166. doi: 10.1016/S0027-9684(15)30830-0 [DOI] [PubMed] [Google Scholar]
- 12.Fiscella K, Dressler R, Meldrum S, Holt K. Impact of influenza vaccination disparities on elderly mortality in the United States. Prev Med. 2007;45(1):83-87. doi: 10.1016/j.ypmed.2007.03.007 [DOI] [PubMed] [Google Scholar]
- 13.Bleser WK, Miranda PY, Jean-Jacques M. Racial/ethnic disparities in influenza vaccination of chronically ill US adults: the mediating role of perceived discrimination in health care. Med Care. 2016;54(6):570-577. doi: 10.1097/MLR.0000000000000544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Madjid M, Safavi-Naeini P, Solomon SD, Vardeny O. Potential effects of coronaviruses on the cardiovascular system: a review. JAMA Cardiol. Published March 27, 2020. doi: 10.1001/jamacardio.2020.1286 [DOI] [PubMed] [Google Scholar]
- 15.Ritchey MD, Wall HK, George MG, Wright JS. US trends in premature heart disease mortality over the past 50 years: where do we go from here? Trends Cardiovasc Med. 2019;S1050-1738(19)30134-30133. doi: 10.1016/j.tcm.2019.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]