Abstract
PURPOSE:
Lung cancer remains the leading cause of cancer death in the United States, with outcomes likely worsened by the presence of poorer outcomes among vulnerable populations such as the homeless. We hypothesized that homeless patients experience delays in biopsy, decreased appointment adherence, and increased overall mortality rates.
METHODS:
We conducted a retrospective electronic medical record–based review of all patients with non–small-cell lung cancer (NSCLC; N = 133) between September 2012 and September 2018 at an academic county hospital in Seattle, Washington.
RESULTS:
Of the 133 patients treated for NSCLC, 22 (17%) were homeless at the time of their treatment. Among homeless patients with localized lung cancer, the mean time from radiographic finding to biopsy was 248 days, compared with 116 days among housed patients (P = .37). Homeless patients with advanced disease missed a mean of 26% of appointments in the year after diagnosis, compared with 16% among housed patients (P = .03). Homeless patients with advanced NSCLC had a median survival of 0.58 years, versus 1.30 years in housed patients (P = .48).
CONCLUSION:
To our knowledge, this is the first US study comparing outcomes among homeless and housed patients with NSCLC within the same institution; we found homeless patients had longer delays to biopsy, increased rates of missed appointments, and a trend toward decreased survival. This study shows potential areas where interventions could be implemented to improve lung cancer outcomes in this patient population.
INTRODUCTION
Lung cancer remains the leading cause of cancer death in the United States despite groundbreaking advancements in treatment. Although the rate of deaths resulting from lung cancer is declining overall in the United States, some populations are not benefiting from this trend.1 It is possible that poorer outcomes among vulnerable populations, such as transient homeless persons, contribute to the limited improvement in overall lung cancer mortality rates. Although homeless rates are decreasing, this demographic group may still represent a significant percentage of those seeking oncologic care, because > 500,000 individuals experience homelessness on a given night in the United States.2 The barriers faced by these patients in meeting their basic food, shelter, and medical needs are compounded by the logistic and cognitive complexity of multidisciplinary oncologic care.
There are few data regarding outcomes and barriers to care among homeless patients with cancer. This is troublesome, given their higher rate of malignancy; in a large Massachusetts-based cohort study, cancer of the lung or bronchus was 2.3 times more likely to develop in homeless individuals than in the general population, and homeless patients were also 2.3 times more likely to die of that cancer as compared with the general population.3
Homeless individuals have high rates of mental illness and substance use disorder (SUD), with estimates from a recent meta-analysis demonstrating pooled rates of depression, psychosis, drug abuse, and alcohol abuse of 11.4%, 12.7%, 24.4%, and 37.9%, respectively.4 Despite similar rates of cancer incidence, those with mental illness and cancer are 30% more likely to die of their cancer and are significantly more likely to be diagnosed at a more-advanced stage.5,22 Increased smoking rates in populations with mental illness likely contribute to poor cancer outcomes. Those with schizophrenia have smoking rates as high as 80%, compared with the national average of 15.5%.6
Those with mental illness have decreased rates of medication compliance; patients with major depressive disorder are 3 times as likely to be noncompliant than nondepressed patients.7,21 Homelessness itself is associated with decreased medication compliance, with data showing self-reported noncompliance of 26%, and cost is reported to be a driver in 15% of these patients; true rates of noncompliance are likely much higher.8,19,20
Another potential barrier to appropriate oncologic care is that homeless patients have higher rates of SUD than do housed patients. The 2017 National Coalition for the Homeless report estimated 38% of homeless persons were dependent on alcohol and 26% abused other drugs.9,17,18 Rates of SUD are possibly higher today, considering the growing opioid epidemic. A recent Oklahoma City–based outreach survey found that 39.7% of homeless individuals self-reported a history of alcohol problems, and a Toronto-based survey showed that 27% of the homeless population reported recent cocaine use.10,11
To our knowledge, no studies have compared the outcomes of housed patients with NSCLC with those of homeless persons in the same community. To address this knowledge disparity, we conducted a retrospective review from 2012 to 2018 of outcomes and delays in care among all patients with NSCLC who were treated at Harborview Medical Center, a county hospital affiliated with the University of Washington in Seattle. We hypothesized that homeless patients would have longer delays to biopsy and treatment and have shorter times from diagnosis to last-known contact than would housed patients. As a secondary aim, we hypothesized that homeless patients would have a decreased median overall survival (OS) rate compared with housed patients diagnosed with advanced-stage NSCLC.
METHODS
Study Design and Patient Population
To investigate disparities in cancer outcomes among housed versus homeless patients, we performed a retrospective analysis of patients, using a prospectively maintained database of patients with lung cancer treated at Harborview Medical Center (HMC) in Seattle, WA, between September 2012 and September 2018. HMC is part of the University of Washington health care network and Seattle’s premier county hospital. HMC prioritizes care for the non–English-speaking poor, uninsured or underinsured, those who are homeless, or those with mental illness, and supports 413 beds. This mission has facilitated numerous outpatient low-income clinics, outreach programs, a homeless shelter on campus, and substantial social and logistical support for patients. Patients were included if they were aged 18 years or older and had a diagnosed, pathologically staged, stage I-IV NSCLC. They must have had at least 1 clinical visit with an oncologist or radiation oncologist between September 2012 and September 2018.
This database contained demographic variables and cancer type. The primary outcome was delays in care and loss to follow-up. Secondary outcomes were mortality rates and quality measures, including percentage of patients with stage IV adenocarcinoma in whom tumor molecular profiling was obtained.
These data, as well as other descriptive data, including homelessness during treatment, substance abuse during treatment, history of SUD, history of mental illness, working at time of diagnosis, and social living situation, were collected through extensive chart review. Insurance status at time of diagnosis was not available in retrospect, although uninsured patients at HMC typically enroll in Medicaid after diagnosis. Data on the percentage of appointments missed, number of hospital admissions, and number of emergency department visits were provided by the Harborview Quality Improvement Department. Institutional review board approval was obtained to analyze the quality improvement data.
Statistical Analysis
Descriptive statistics were provided to summarize the patient population. Differences in outcomes between the homeless and housed groups were determined using Fisher exact test for categorical variables and 2-sample t test for continuous variables. The association between being homeless during time of treatment and death was determined using a Kaplan-Meier curve, as were many other risk factors. We used a multivariable Cox proportional hazard model to analyze the effect of delays in undergoing biopsy and interventions on OS. Delays were modeled as a time-dependent covariate. P < .05 was used to determine statistical significance.
RESULTS
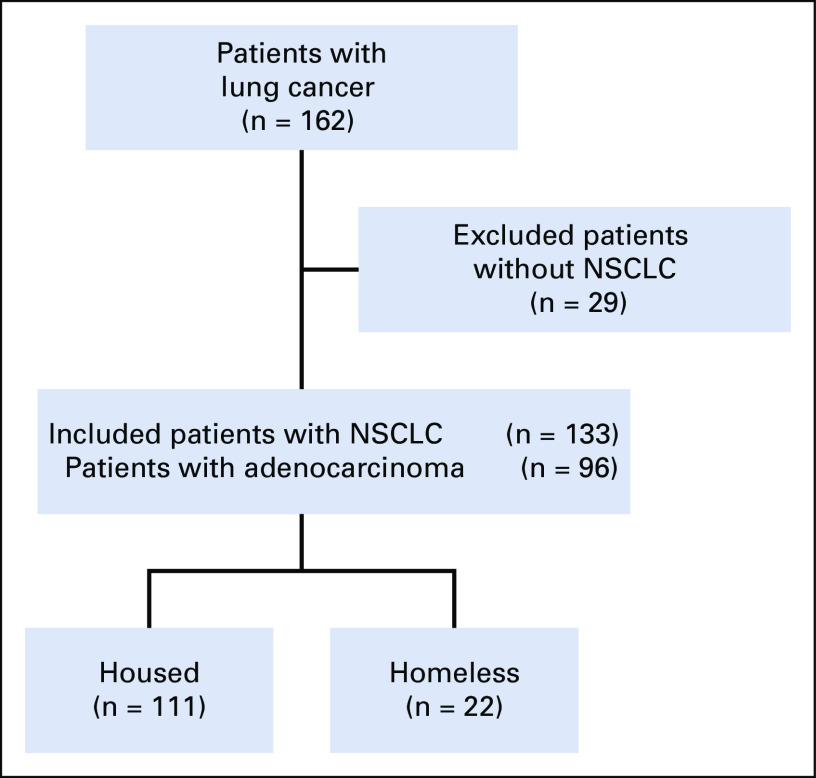
A total of 162 patients with lung cancer were included from the prospectively maintained lung cancer database at HMC from September 2012 to September 2018. Of these, 29 cases were not definitively squamous cell or adenocarcinoma and thus were excluded, leaving 133 patients with NSCLC to be included in the study: 96 with adenocarcinoma and 37 with squamous-cell carcinoma. Among the 133 patients, 22 were homeless during their cancer therapy and 111 were housed. Given the potential for different populations presenting with localized or advanced disease, demographics in localized and advanced disease were analyzed separately. There were 52 patients (n = 9 homeless) with stage I or II disease at diagnosis and 81 patients (n = 13 homeless) with stage III or IV disease at diagnosis (Appendix Fig A1; online only).
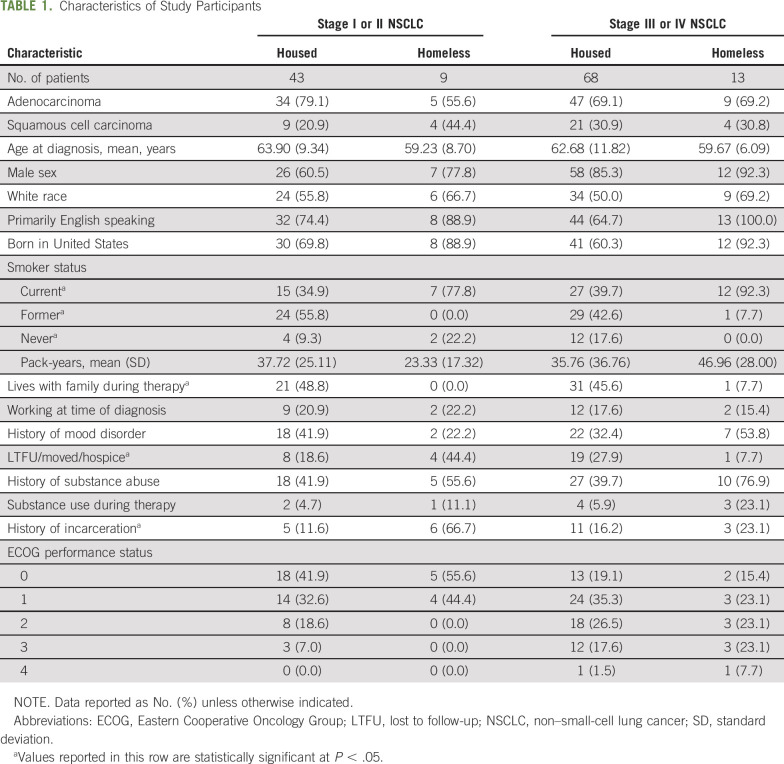
We found no difference in tumor type, age, sex, race, or rates of English as primary language between housed and homeless patients with localized disease. Homeless patients were more likely to be current smokers, less likely to live with family, more likely to have a history of incarceration, and more likely to have ultimately been lost to follow-up than housed patients. Homeless patients diagnosed with advanced disease were also less likely to live with family, more likely to be lost to follow-up, more likely to have a history of substance or alcohol use disorder, but equally likely to have mental illness, when compared with housed patients. Among those diagnosed with advanced disease, homeless patients were more likely to be born in the United States, be current smokers, live without family, and have a history of SUD. Rates of homeless and housed patients diagnosed with localized and advanced disease were similar (Table 1).
TABLE 1.
Characteristics of Study Participants
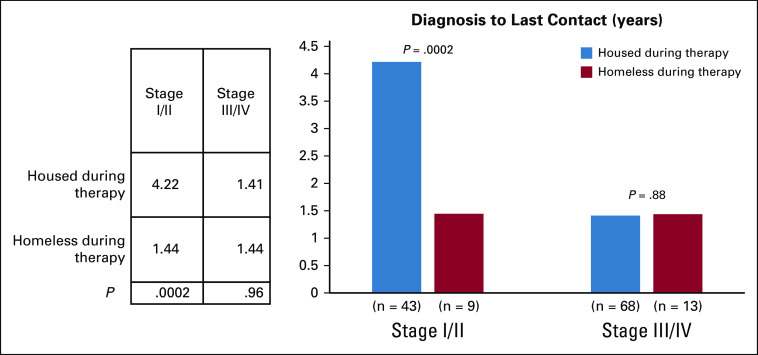
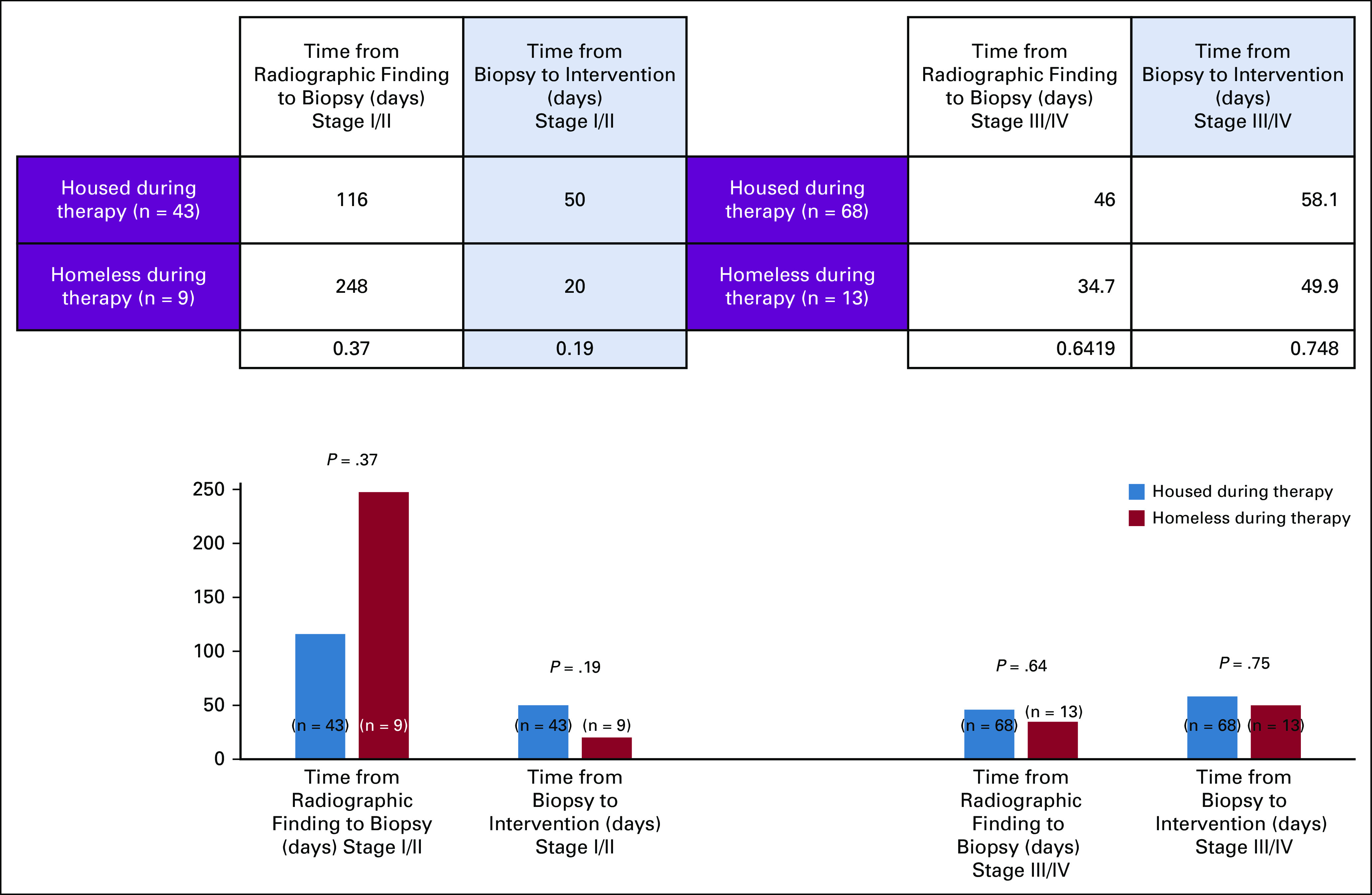
To evaluate delays in diagnosis, time from first radiographic appearance of a nodule to biopsy specimen–proven NSCLC was collected. Among those with localized disease, the number of days from radiographic finding to biopsy among homeless patients was more than twice that of housed patients on average (mean, 248 v 116 days; P = .37; Appendix Fig A2; online only). Once the diagnosis was made, both housed and homeless groups had short times to treatment (50 v 20 days; P = .19). The time from pathologic diagnosis to last known contact was significantly longer among housed than homeless patients (mean, 1,539 v 527 days; P = .0004; Appendix Fig A3; online only).
Of the 9 homeless patients with localized malignancy, 7 (78%) had completed definitive therapy, defined as tumor resection or definitive radiation, as opposed to 42 of 43 (97.8%) among housed patients (P = .02). The 2 homeless patients who did not complete definitive therapy were the only homeless patients who underwent radiation treatment rather than resection, and both were unable to complete a definitive course. One housed patient did not complete curative intent therapy; this patient’s course was complicated by concurrent lymphoma, and the patient died 3 months after diagnosis. Among the 13 homeless patients with advanced malignancy, 4 received chemotherapy.
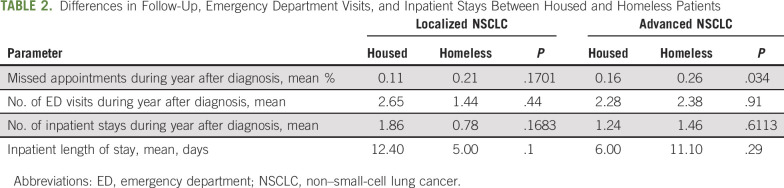
Differences between rates of missed appointments between housed and homeless patients with localized disease did not meet statistical significance; housed patients missed 11% of appointments compared with 21% of homeless patients (P = .17). However, significance was met among those diagnosed with advanced disease (homeless who missed appointments, 26%; housed patients who missed appointments, 16%; P = .03). There was no statistical difference between the number of inpatient stays, total length of inpatient stay, or number of emergency department visits in the year after diagnosis for housed versus homeless patients with advanced or localized disease (Table 2).
TABLE 2.
Differences in Follow-Up, Emergency Department Visits, and Inpatient Stays Between Housed and Homeless Patients
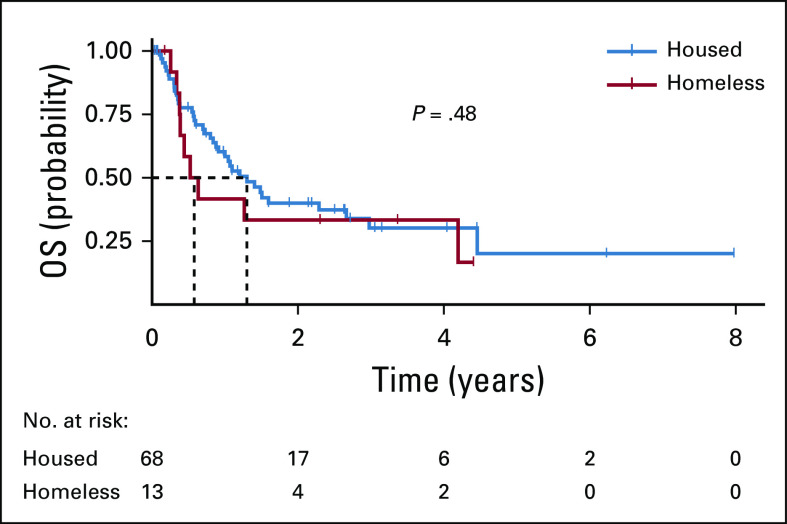
A total of 42 patients were diagnosed with stage IV adenocarcinoma, 6 of whom were homeless. All homeless patients underwent molecular testing for determination of targeted therapy eligibility, as did 91.7% of housed patients. Of the homeless patients, 1 had a targetable mutation but did not receive targeted therapy or any other type of treatment. Of the 36 housed patients, 30.3% had targetable mutations and all received targeted therapy (Appendix Table A1; online only).Kaplan-Meier curve to assess OS among patients with advanced disease demonstrated a median survival of 0.58 years versus 1.30 years for homeless and housed patients, respectively (P = .48), with a hazard ratio of 1.3 (P = .49; Fig 1).
Fig 1.
Kaplan-Meier curve of overall survival (OS) among housed and homeless patients in this study.
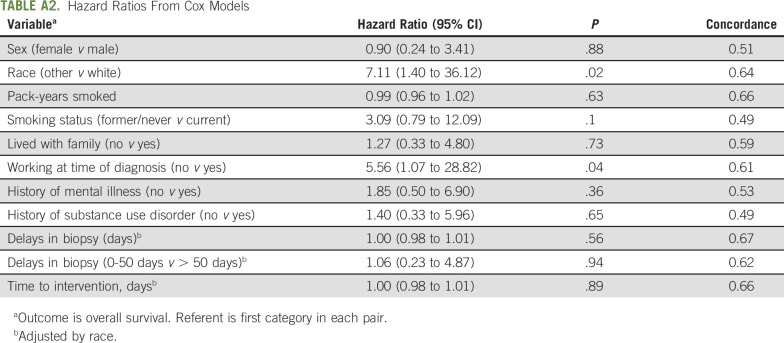
The correlation between independent variables and median OS was determined by Kaplan-Meier curve as well, which showed a statistically significant decrease in median survival among those identified as being white and those working at the time of diagnosis. Delays in biopsy, living with family, history of mental illness, history of SUD, sex, and current smoking status were not associated with changes in median survival (Appendix Fig A4; online only).
To best assess the potential adjustment variables for multivariate analysis, we fit univariate Cox models and found that white race had the highest correlation with decreased OS (hazard ratio [HR], 7.11; P = .02). Multivariable Cox models adjusted for race demonstrated no effect on OS from radiographic finding to diagnosis time (HR, 1.0; P = .56) or diagnosis to intervention time (HR, 1.0; P = .89; Appendix Table A2; online only).
DISCUSSION
In this retrospective study of 133 patients with NSCLC presenting at a county hospital in Seattle, WA, we found that homeless patients with localized cancer had significantly shorter time from diagnosis to last known contact than did housed patients (527 v 1,539 days, respectively) and a nonsignificant longer time from radiographic finding of malignancy to biopsy or resection, as compared with housed patients (248 v 116 days, respectively).There was a trend suggesting that homeless patients with advanced-stage NSCLC had worse outcomes, with median survival of 6.9 months compared with 14.4 months in the housed group.
To our knowledge, this is the first study to characterize the delays in care or survival outcomes among homeless patients with NSCLC in the United States. Multiple barriers undoubtedly contribute to these outcomes, including navigating transportation, food insecurity, competing appointments that are not health care related, lack of phones, mistrust of the medical community, lower health care literacy, mental health decompensation, SUD, toxicity management, and lack of social support for daily needs. Surprisingly, these delays were not observed when homeless patients were diagnosed at an advanced-stage of disease, likely because they were symptomatic, necessitating that their health care rise within the list of competing priorities. Of note, homeless and housed patients with NSCLC are all treated as outpatients at HMC.
Homeless patients with localized disease lost contact with the medical team (lost to follow-up, moved out of the area, or transitioned to hospice) at twice the rate of housed patients (44.4% v 18.6%), indicating poorer outcomes and confounded OS data. Although the outcome of these patients is unknown, the transient nature of the homeless population suggests they are less likely to receive recommended follow-up and may not inform outside providers of this history. Furthermore, we suspect homeless patients choose hospice over treatment to avoid overwhelming medical complexity and treatment adverse effects at greater rates than the housed population.
All housed patients with localized disease completed definitive therapy, whereas 2 of 9 homeless patients were unable to finish therapy and were the only homeless patients who underwent radiation therapy with curative intent. The reason for this lapse is suggested by the doubled rate of missed appointments by the homeless patients compared with the housed patients (21% v 11%). Patients with economic or health-associated barriers are provided transportation assistance via bus pass or HMC-associated taxi, but meeting with social workers to navigate income or need-based assistance adds another level of complexity. These patients were particularly vulnerable because none of them lived with family members who could assist with these or other matters during therapy. This discrepancy in follow-up did not result in higher rates of emergency department visits or inpatient stays in our health care system; however, this statistic may be confounded by patients receiving acute care at one of the many other Seattle hospitals, which is common among the Seattle homeless population.
Homeless patients did not have significantly higher rates of reported drug use during therapy but did have higher rates of SUD historically. We suspect true rates of drug use during therapy is higher because this is frequently not documented. Surprisingly, homeless patients did not have increased rates of previously documented mental health disorders in our study.4 It is important to note that the barriers of retrospective chart review do not allow for accurate measurement of rates of decompensation or severity of drug use or mental illness. We recommend concurrent mental health and SUD treatment among this high-risk group while undergoing cancer care.
The significantly higher rate of current tobacco use in the homeless population suggests most cases are tobacco attributable, although there was no difference in total pack-years between the homeless and housed groups.16 Although a causal link between lung cancer and inhaled illicit drugs is suspected, the concomitant use of tobacco products is confounding. Data regarding marijuana use were not collected, given challenges in quantification and its legal status in Washington state, which limits documentation of recreational use.
As a quality metric, we collected the data on rates of tumor molecular profiling among those with stage IV adenocarcinoma and found that homeless and housed patients get adequate testing and targeted treatment in this setting. The consistency in treatment course among those with metastatic disease suggests the standard of care is being delivered to all patients and that metastatic NSCLC has universally poor outcomes.
Among all patients with NSCLC, the only independent risk factors associated with decreased OS were white race and being employed at the time of diagnosis. This was influenced by the association between white race and other predictors of poor outcomes (eg, homelessness, mental illness, SUD) among the HMC population, among whom many nonwhite patients are immigrants who do not have these comorbidities. The correlation between employment and worsened survival among the HMC population may demonstrate the impact of financial reliance on employment during treatment leading to worse outcomes, whereas those not reliant on employment income are more able to engage in health care.
We found that homeless patients had increased rates of missed appointments, increased loss to follow-up, and a trend toward decreased survival. White patients and those who were employed at the time of diagnosis had statistically significant decreased median survival times, whereas patients with delays in biopsies or treatment, history of SUD or mental illness, or those living without family support did not. There were several limitations to this study because it was retrospective, had a small sample size, and was a single institution at a county hospital.
There is a significant need for prospective studies to better characterize the disparities encountered by vulnerable populations with lung cancer and develop sustainable strategies to overcome these barriers. We believe a multifactorial approach will be necessary to improve the care of these populations, requiring innovative strategies, including housing for those undergoing diagnosis and treatment; advancement in lower-barrier diagnostic strategies, such as peripheral blood-based assays instead of invasive biopsies; concurrent mental health and substance abuse treatment; and lowering of economic and logistic barriers.12-24
Appendix
Fig A1.
Flow diagram of housed and homeless patients with non–small-cell lung cancer (NSCLC).
Fig A2.
Time between diagnosis and last known contact.
Fig A3.
Delays in biopsy and intervention.
Fig A4.
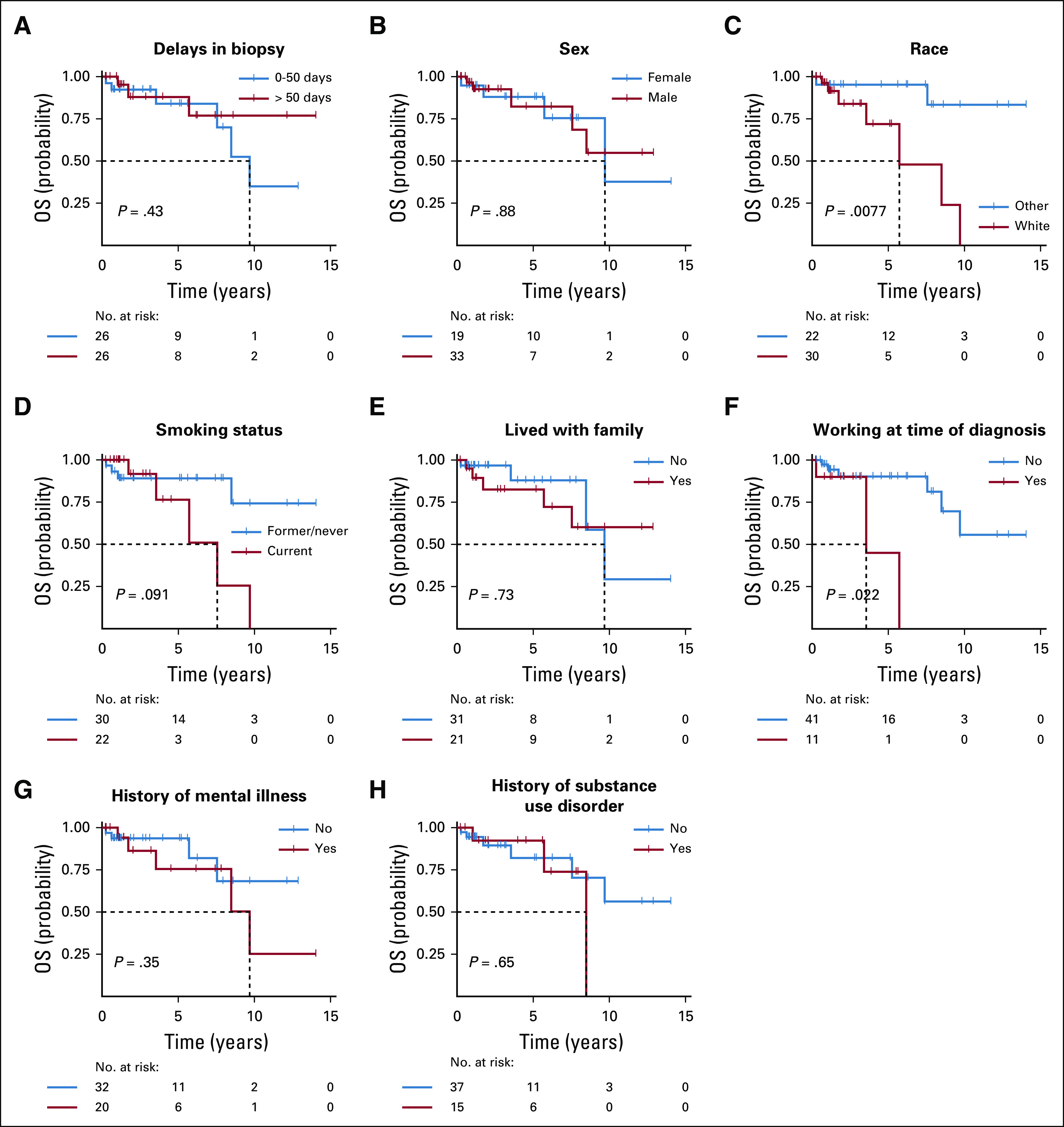
Single-variable Kaplan-Meier curves for overall survival in years; variables analyzed include delays in biopsy, sex, race, smoking status, living with family, working at time of diagnosis, history of mental illness, and history of substance use disorder.
TABLE A1.
Molecular Tumor Analysis in Stage IV Adenocarcinoma
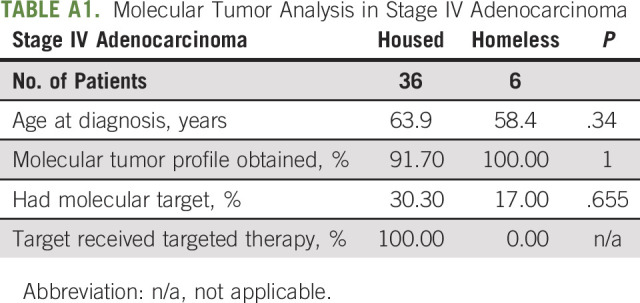
TABLE A2.
Hazard Ratios From Cox Models
PRIOR PRESENTATION
Presented at Multidisciplinary Thoracic Cancers Symposium, San Diego, CA, March 14-16, 2019; Binaytara Foundation Annual International Conference on Advances in Hematology and Oncology, Seattle, WA, June 29-30, 2019; and ASCO Annual Meeting, Chicago, IL, May 31-June 4, 2019.
AUTHOR CONTRIBUTIONS
Conception and design: Kyle F. Concannon, Christina S. Baik, Hannah M. Linden
Administrative support: Hannah M. Linden
Provision of study material or patients: Hannah M. Linden
Collection and assembly of data: Kyle F. Concannon, John H. Thayer, Hannah M. Linden
Data analysis and interpretation: Kyle F. Concannon, Qian V. Wu, Isaac C. Jenkins, Christina S. Baik, Hannah M. Linden
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Outcomes Among Homeless Patients with Non–Small-Cell Lung Cancer: A County Hospital Experience
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/op/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Qian V. Wu
Stock and Other Ownership Interests: Gilead Sciences (I)
Research Funding: Juno Therapeutics
Christina Baik
Consulting or Advisory Role: AstraZeneca
Research Funding: Roche (Inst), Novartis (Inst), Celgene (Inst), Loxo (Inst), AstraZeneca (Inst), Pfizer (Inst), MedImmune (Inst), SWOG (Inst), Spectrum Pharmaceuticals (Inst), Blueprint Medicines (Inst), Daiichi Sankyo (Inst), Rain Therapeutics (Inst),: AbbVie (Inst), TP Therapeutics (Inst), Hoosier Cancer Research Network (Inst)
Hannah Linden
Leadership: Evolentt (I)
Stock and Other Ownership Interests: Evolent (I)
Consulting or Advisory Role: Genomic Health, Context Therapeutics, Syndax, AstraZeneca, Eisai
Research Funding: Eisai, Sanofi/Aventis (Inst), GTx (Inst)
No other potential conflicts of interest were reported.
REFERENCES
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68:7–30. doi: 10.3322/caac.21442. [DOI] [PubMed] [Google Scholar]
- 2. https://files.hudexchange.info/resources/documents/2018-AHAR-Part-1.pdf Henry M, Mahathey A, Morrill T, et al: The 2018 Annual Homeless Assessment Report (AHAR) to Congress. Part 1: Point-in-Time Estimates of Homelessness. December 2018.
- 3.Baggett TP, Chang Y, Porneala BC, et al. Disparities in cancer incidence, stage, and mortality at Boston Health Care for the Homeless Program. Am J Prev Med. 2015;49:694–702. doi: 10.1016/j.amepre.2015.03.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. doi: 10.1371/journal.pmed.0050225. Fazel S, Khosla V, Doll H, et al: The prevalence of mental disorders among the homeless in western countries: Systemic review and meta-regression analysis. PLoS Med 5:e225, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kisely S, Crowe E, Lawrence D. Cancer-related mortality in people with mental illness. JAMA Psychiatry. 2013;70:209–217. doi: 10.1001/jamapsychiatry.2013.278. [DOI] [PubMed] [Google Scholar]
- 6.Irwin KE, Henderson DC, Knight HP, et al. Cancer care for individuals with schizophrenia. Cancer. 2014;120:323–334. doi: 10.1002/cncr.28431. [DOI] [PubMed] [Google Scholar]
- 7.DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: Meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000;160:2101–2107. doi: 10.1001/archinte.160.14.2101. [DOI] [PubMed] [Google Scholar]
- 8.Hunter CE, Palepu A, Farrell S, et al. Barriers to prescription medication adherence among homeless and vulnerably housed adults in three Canadian cities. J Prim Care Community Health. 2015;6:154–161. doi: 10.1177/2150131914560610. [DOI] [PubMed] [Google Scholar]
- 9. https://nationalhomeless.org/wp-content/uploads/2017/06/Substance-Abuse-and-Homelessness.pdf National Coalition for the Homeless: Substance Abuse and Homelessness. June 2017.
- 10.Neisler J, Shree S, Reitzel LR, et al. Characterizing alcohol use behaviors among homeless men and women. Am J Health Behav. 2019;43:37–49. doi: 10.5993/AJHB.43.1.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. doi: 10.1186/1471-2458-10-94. Grinman MN, Chiu S, Redelmeier DA, et al: Drug problems among homeless individuals in Toronto, Canada: Prevalence, drugs of choice, and relation to health status. BMC Public Health: 10:94, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Reference deleted.
- 13. Reference deleted.
- 14. Reference deleted.
- 15. Reference deleted.
- 16. https://www.cdc.gov/tobacco/data_statistics/fact_sheets/adult_data/cig_smoking/index.htm Centers for Disease Control and Prevention: Current cigarette smoking among adults in the United States.
- 17.Paull DE, Updyke GM, Baumann MA, et al. Alcohol abuse predicts progression of disease and death in patients with lung cancer. Ann Thorac Surg. 2005;80:1033–1039. doi: 10.1016/j.athoracsur.2005.03.071. [DOI] [PubMed] [Google Scholar]
- 18.Grant BF, Goldstein RB, Saha TD, et al. Epidemiology of DSM-5 alcohol use disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry. 2015;72:757–766. doi: 10.1001/jamapsychiatry.2015.0584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Conti V, Lora A, Cipriani A, et al. Persistence with pharmacological treatment in the specialist mental healthcare of patients with severe mental disorders. Eur J Clin Pharmacol. 2012;68:1647–1655. doi: 10.1007/s00228-012-1298-2. [DOI] [PubMed] [Google Scholar]
- 20.Coodin S, Staley D, Cortens B, et al. Patient factors associated with missed appointments in persons with schizophrenia. Can J Psychiatry. 2004;49:145–148. doi: 10.1177/070674370404900210. [DOI] [PubMed] [Google Scholar]
- 21.Sullivan DR, Ganzini L, Duckart JP, et al. Treatment receipt and outcomes among lung cancer patients with depression. Clin Oncol (R Coll Radiol) 2014;26:25–31. doi: 10.1016/j.clon.2013.09.001. [DOI] [PubMed] [Google Scholar]
- 22.Holowatyj AN, Heath EI, Pappas LM, et al. The epidemiology of cancer among homeless adults in metropolitan Detroit. JNCI Cancer Spectr. 2019;3:pkz006. doi: 10.1093/jncics/pkz006. [DOI] [PMC free article] [PubMed] [Google Scholar]