Abstract
Background:
Several studies reported short-term analgesic efficacy of obturator nerve block (ONB), as in comparison with the femoral nerve block (FNB) in the treatment of postoperative pain after the total knee replacement (TKR). The optimal method remains under debate. The purpose of our current work is to compare the safety and efficacy of FNB and ONB for postoperative analgesia after TKR.
Methods:
This prospective, randomized, and controlled study was performed from January 2018 to December 2019. It was authorized via the Institutional Review Committee in NO.971 Hospital of the People's Liberation Army Navy (2019-PLAN-132).
Two hundred patients were divided randomly into 2 groups, the control group (n = 100) and study group (n = 100). The experimental group received FNB and control groups received ONB. Primary outcome included pain at different time point (Visual Analogue Scale score of anterior knee pain at rest and in motion). The Visual Analogue Scale scores were marked by patients themselves on a paper with a graduated line starting at 0 (no pain) and ending at 10 (the most painful). Opioid consumption was converted to equivalents of oral morphine uniformly for statistical analysis. Secondary outcomes included the knee range of motion, the hospital stay length as well as the postoperative complications such as pulmonary embolism and deep vein thrombosis.
Results:
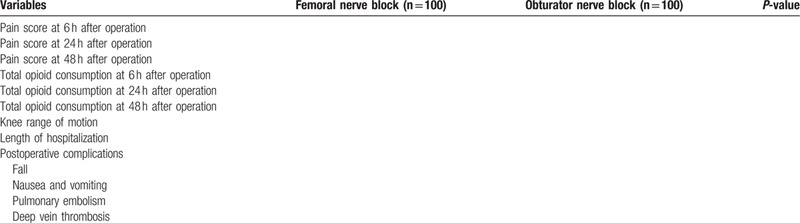
Table 1 will show the clinical outcomes between the 2 groups.
Conclusion:
This trial would provide an evidence for the use of different types of peripheral nerve blocks in TKR.
Keywords: femoral nerve block, obturator nerve block, pain management, protocol, total knee replacement
1. Introduction
The total knee replacement (TKR) is regarded as a successful method option for treating the end-stage knee osteoarthritis, with satisfactory functional recovery, significant deformity correction effect, and outstanding postoperative pain relief.[1,2] With the aging of the US population, the number of TKR is expected to obviously increase by 2030, reaching estimated 3.48 million a year.[3,4] In the acute stage after surgery, TKR can lead to obvious pain, and the postoperative knee pain has become a familiar and persistent chief complaint after the TKR, leading to patient poor life quality and dissatisfaction. The reported incidence of severe postoperative knee pain after TKR ranges from 10.3% to 36.8%.[5,6] Opioid is frequently used for postoperative pain management. However, it may be associated with many adverse effects, including headache, nausea, vomiting, respiratory depression, retention of urine, and constipation.[7–9] Specific medical diseases related to the inadequate pain control involved myocardial infarction, coronary ischemia, venous thrombosis, and pneumonia. Effective postoperative analgesia can reduce opioid consumption and promote rehabilitation.
Several methods have been applied to reduce postoperative pain after TKR including the peripheral nerve block and the local infiltration anesthesia, intravenous analgesics as well as the epidural anesthesia.[10–13] The optimal method remains under debate. Femoral nerve block (FNB) was reported to reduce postoperative pain and has increased in popularity because of its opioid sparing effects, and consistency with anticoagulatory therapy. However, some articles reported that FNB may decrease the strength of quadriceps femoris, which causes risk of fall.[14] Recently, several studies reported short-term analgesic efficacy of obturator nerve block (ONB), as in comparison with the FNB in the treatment of postoperative pain after TKR. Bergeron et al[15] reported that there was no significant difference between FNB and ONB in terms of functional outcomes. Currently, there is no reliable evidence to support the clinical application for pain control. The purpose of our current work is to compare the safety and efficacy of FNB and ONB for postoperative analgesia after TKR.
2. Methods
2.1. Study design
This controlled, randomized, and prospective research was performed from January 2018 to December 2019 which was performed in accordance with the SPIRIT Checklist for randomized studies. It was authorized via the Institutional Review Committee in NO.971 Hospital of the People's Liberation Army Navy (2019-PLAN-132) and then was registered in research registry (researchregistry5849).
2.2. Recruitment and consent
All patients participating in the TKR will be treated in our orthopedic outpatient department. The surgeon will explain the details of trial, afterward, patiently answer all the patient's questions. The patient is then presented with the written information of our trial. Each of patient received a written informed consent. Since all patients participated voluntarily, they could withdraw at any time during the trial.
2.3. Inclusion of exclusion criteria
The subjects in this research were 200 primary TKR patients from our Hospital. The inclusion criteria were:
-
(1)
patients prepared for primary unilateral TKR;
-
(2)
the age were above 50 years.
The exclusion criteria were as follows:
-
(1)
the body mass index of the patients was more than 40 kg/m2;
-
(2)
allergies or contraindications to the opioid analgesics;
-
(3)
a history of deep vein thrombosis or pulmonary embolism 3 months before the operation.
2.4. Randomization and Blinding
Two hundred patients were divided randomly into 2 groups, namely, control group (n = 100) and the study group (n = 100), respectively. A table of random numbers hidden in the 1:1 ratio was computer-formed. A researcher who did not take part in the trial used the website Randomization.com to generate a random distribution sequence, which was hidden in sealed opaque sequence numbered envelopes that were allocated to investigators. The surgeons, investigator, anesthetist, and nurses were all kept blinded to allocation results.
2.5. Intervention of each group
All patients were given the spinal anesthesia. The surgical procedures were performed by the senior surgeon. In the process of operation, pneumatic tourniquet was utilized. An incision was made in the center of the knee and then extended to the medial side of patella. A posterior stabilized prosthesis (Attune, DePuy, Warsaw, IN) was implanted. The experimental group received FNB and control groups received ONB. Other procedures were the same: removing excess peri-patella synovium and osteophytes, trimming the patella with a narrow oscillating saw and circumferential electrocautery of the patella. Multimodal postoperative pain management of our center were administered to all the patients. Analgesic protocol: after admission, patients were given 200 mg celecoxib orally every 12 hours for preemptive analgesia until the morning of the operation day. Intraoperatively, patients were given 20 mg ropivacaine diluted with 60 mL normal saline by topical injection to the joint capsule and collateral ligaments. Intravenous patient-controlled analgesia was given after TKR.
2.6. Outcome measures
Post-operative clinical data were assessed by an independent senior surgeon blinded to the patient's randomization. Primary outcome included pain at different time point (Visual Analogue Scale score of anterior knee pain at rest and in motion). The Visual Analogue Scale scores were marked by patients themselves on a paper with a graduated line starting at 0 (no pain) and ending at 10 (the most painful). Opioid consumption was converted to equivalents of oral morphine uniformly for statistical analysis. Secondary outcomes included the knee range of motion, the hospital stay length as well as the postoperative complications such as pulmonary embolism and deep vein thrombosis.
2.7. Statistical analysis
The calculations of sample size are conducted utilizing the software of PASS 2011 (NCSS, LLC, Kaysville, UT). All the needed analyses are implemented through utilizing SPSS for Windows Version 20.0. All the data are represented with proper characteristics as median, mean, percentage as well as standard deviation. Mann–Whitney U test or the independent samples t-test were used to analyze the inter-group comparison. Chi-square detection was utilized to compare the categorical variables among the groups. The analysis of repeated measurement of the variance was applied to analyze the repeated data. A P < .05 was regarded the significant in statistics.
3. Result
Table 1 will show the clinical outcomes between the 2 groups.
Table 1.
Outcome measures between femoral nerve block and obturator nerve block.
4. Discussion
Pain management after the TKR is still challenging, but is important due to good pain management can improve the outcomes of patient. About half of patients who undergo the TKR experience moderate to serious postoperative pain.[16] The postoperative pain is caused by inflammation resulted from direct nerve injury or the tissue injury. Patients can perceive the pain through afferent pain pathway, this is the target of a variety of drugs. Direct anesthetics or the drugs that reduce the response of local hormones to injury (nonsteroidal anti-inflammatory drugs, such as ibuprofen or aspirin) can be utilized to block the activity of pain receptors, thereby reducing the activity of pain receptors. The various management programs of postoperative pain and the lack of a definitive “gold standard” indicate that there is room for improving the standard of care.[17]
Peripheral nerve block with continuous or single infusion of local anesthetics has been extensively utilized in TKR field. The more familiar forms of peripheral nerve block in the TKA are the sciatic nerve, obturator nerve, and the FNBs.[18,19] Despite muscle weakness after surgery, there is evidence that the patients receiving the peripheral nerve block can recover faster than the patients receiving patient-controlled analgesia. Thus, we performed this protocol to compare the efficacy of FNB and ONB for pain management in patients undergoing TKR.
5. Conclusion
This trial would provide an evidence for the use of different types of peripheral nerve blocks in TKR.
Author contributions
Data curation: Peng Lin.
Investigation: Fuheng Zhang.
Methodology: Fuheng Zhang.
Writing – original draft: Wei Zhang.
Footnotes
Abbreviations: FNB = femoral nerve block, ONB = obturator nerve block, TKR = total knee replacement.
How to cite this article: Zhang W, Lin P, Zhang F, Wang J. Femoral nerve block versus obturator nerve block for pain management after total knee replacement: A randomized controlled trial protocol. Medicine. 2020;99:37(e21956).
WZ and PL contributed equally to the study.
The protocol was registered in Research Registry (researchregistry5849).
Provide the name of the repository and a persistent web link to the datasets.
Funding was provided by the Qingdao Medical Research Project 2019 (2019-WJZD164).
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are publicly available.
References
- [1].Raynauld JP, Martel-Pelletier J, Dorais M, et al. Total knee replacement as a knee osteoarthritis outcome: predictors derived from a 4-year long-term observation following a randomized clinical trial using chondroitin sulfate. Cartilage 2013;4:219–26.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Rat AC, Guillemin F, Osnowycz G, et al. Total hip or knee replacement for osteoarthritis: mid- and long-term quality of life. Arthritis Care Res 2010;62:54–62.. [DOI] [PubMed] [Google Scholar]
- [3].Hootman JM, Helmick CG. Projections of US prevalence of arthritis and associated activity limitations. Arthritis Rheum 2006;54:226–9.. [DOI] [PubMed] [Google Scholar]
- [4].Malcolm T, Szubski CR, Schiltz NK, et al. Prevalence and perioperative outcomes of off-label total hip and knee arthroplasty in the united states, 2000-2010. J Arthroplasty 2015;30:1872–8.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Kim DH, Pearson-Chauhan KM, McCarthy RJ, et al. Predictive factors for developing chronic pain after total knee arthroplasty. J Arthroplasty 2018;33:3372–8.. [DOI] [PubMed] [Google Scholar]
- [6].Elmallah RK, Chughtai M, Khlopas A, et al. Pain control in total knee arthroplasty. J Knee Surg 2018;31:504–13.. [DOI] [PubMed] [Google Scholar]
- [7].Christo PJ. Opioid effectiveness and side effects in chronic pain. Anesthesiol Clin North Am 2003;21:699–713.. [DOI] [PubMed] [Google Scholar]
- [8].Mercadante S. Opioid analgesics adverse effects: the other side of the coin. Curr Pharm Des 2019;25:3197–202.. [DOI] [PubMed] [Google Scholar]
- [9].Martin CM, Forrester CS. Anticipating and managing opioid side effects in the elderly. Consult Pharm 2013;28:150–9.. [DOI] [PubMed] [Google Scholar]
- [10].Li C, Qu J, Pan S, et al. Local infiltration anesthesia versus epidural analgesia for postoperative pain control in total knee arthroplasty: a systematic review and meta-analysis. J Orthop Surg Res 2018;13:112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Tammachote N, Kanitnate S. Intravenous dexamethasone injection reduces pain from 12 to 21 hours after total knee arthroplasty: a double-blind, randomized, placebo-controlled trial. J Arthroplasty 2020;35:394–400.. [DOI] [PubMed] [Google Scholar]
- [12].Yayac M, Li WT, Ong AC, et al. The efficacy of liposomal bupivacaine over traditional local anesthetics in periarticular infiltration and regional anesthesia during total knee arthroplasty: a systematic review and meta-analysis. J Arthroplasty 2019;34:2166–83.. [DOI] [PubMed] [Google Scholar]
- [13].Hwang JW, Jeon YT. Effect of peripheral nerve block on length of stay after total knee arthroplasty. Anesthesiology 2017;127:718–9.. [DOI] [PubMed] [Google Scholar]
- [14].Kwofie MK, Shastri UD, Gadsden JC, et al. The effects of ultrasound-guided adductor canal block versus femoral nerve block on quadriceps strength and fall risk: a blinded, randomized trial of volunteers. Reg Anesth Pain Med 2013;38:321–5.. [DOI] [PubMed] [Google Scholar]
- [15].Bergeron SG, Kardash KJ, Huk OL, et al. Functional outcome of femoral versus obturator nerve block after total knee arthroplasty. Clin Orthop Relat Res 2009;467:1458–62.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Ma J, Zhang W, Yao S. Liposomal bupivacaine infiltration versus femoral nerve block for pain control in total knee arthroplasty: a systematic review and meta-analysis. Int J Surg 2016;36:44–55.. [DOI] [PubMed] [Google Scholar]
- [17].McDonald LT, Corbiere NC, DeLisle JA, et al. Pain management after total joint arthroplasty. AORN J 2016;103:605–16.. [DOI] [PubMed] [Google Scholar]
- [18].Sato K, Sai S, Shirai N, et al. Ultrasound guided obturator versus sciatic nerve block in addition to continuous femoral nerve block for analgesia after total knee arthroplasty. Jpn Clin Med 2011;2:29–34.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Kardash K, Hickey D, Tessler MJ, et al. Obturator versus femoral nerve block for analgesia after total knee arthroplasty. Anesth Analg 2007;105:853–8.. [DOI] [PubMed] [Google Scholar]


