Summary:
Tendon transfer for radial nerve palsy is a common procedure done under general anesthesia. We describe a surgical technique of triple tendon transfer with wide awake local anesthesia no tourniquet (WALANT). We transfer flexor carpi radialis to extensor digitorum communis, palmaris longus to extensor pollicis longus, and pronator teres to extensor carpi radialis brevis. This is commonly known as the Brand transfer. Our anesthetic or WALANT solution consists of up to 200 mL of 1:400,000 epinephrine, 0.25% lidocaine buffered with sodium bicarbonate. This technique overcomes the problem of judging the appropriate amount of transfer tension by observing awake patients actively extend their fingers, thumb, and wrist during the surgery and making adjustments before we close the wound. In our experience, there is no need of brain retraining because a patient is able to immediately use the flexor muscles to perform extension movements. WALANT is a safe and viable option for radial nerve tendon transfers.
INTRODUCTION
Surgery under wide awake local anesthesia no tourniquet (WALANT) continues to gain popularity. WALANT tendon transfers in the hand and distal part of the forearm have been described. They are extensor indicis proprius to extensor pollicis longus (EPL) transfers,1,2 flexor digitorum superficialis (FDS) to flexor pollicis longus transfers,3 and FDS to flexor digitorum profundus transfers.4 In patients with leprosy, Mohammed and Lalonde5 published an article on 63 cases of tendon transfers, describing the local anesthetic methods for direct lasso, indirect lasso, half flexor pollicis longus to EPL, and opponensplasty.
Bezuhly et al2 reported on 7 cases of extensor indicis proprius to EPL transfers, with a successful outcome after a 15-month follow-up. One case had a rupture, and they proceeded to an extensor carpi radialis longus to EPL transfer. They used 20 mL of 1% lidocaine with 1:200,000 epinephrine. Other hand surgeons transfer FDS to flexor digitorum profundus using 0.5% lidocaine with 1:200,000 epinephrine.4
Bony fixation of the distal radius, mid-shaft ulna, and olecranon has been reported by Ahmad and Ikram6 and Ahmad et al,7,8 but there is still a very little account on proximal forearm WALANT tendon transfers. This article describes, with illustrations and video, the Brand tendon transfer with WALANT for radial nerve palsy.
ANESTHETIC AND SURGICAL TECHNIQUE
Three incisional sites are marked (Figs. 1, 2). The WALANT solution consists of buffered 1:400,000 epinephrine (0.25% lidocaine). If you have no premixed lidocaine and epinephrine, use 50 mL of 1% lidocaine, 0.5 mL of 1:1,000 epinephrine, 5 mL of 8.4% bicarbonate, and 150 mL of saline to provide up to 200 mL of solution and deliver a 7 mg/kg dosage range of lidocaine with epinephrine in a 70-kg patient. Otherwise, use 50 mL of premixed 1% lidocaine and epinephrine with 5 mL of bicarbonate and 150 mL of saline. If you use 2% pure lidocaine, mix 25 mL of 2% lidocaine, 0.5 mL of 1:1,000 epinephrine, 5 mL of 8.4% bicarbonate, and 175 mL of saline to provide up to 200 mL of solution. A table of the various concentrations is shown in Video 1. [See Video 1 (online), which displays the local anesthetic injection. Injections are given subcutaneously for pronator teres (PT, together with deep periosteal injection), followed by EPL, extensor digitorum communis (EDC), and extensor carpi radialis brevis (ECRB); and then palmaris longus (PL), flexor carpi radialis (FCR), and finally PT-ECRB.]
Fig. 1.
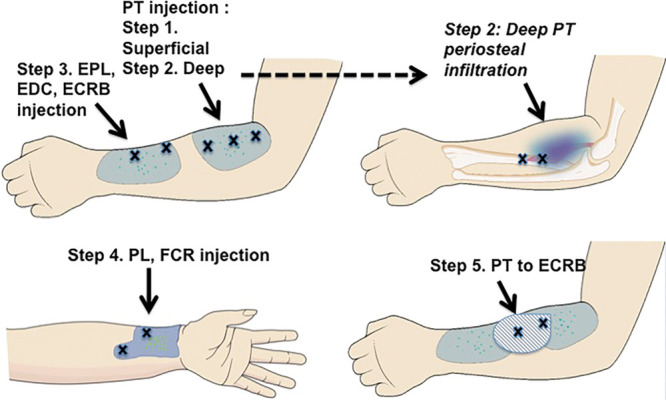
Diagram of regions where the WALANT solution is infiltrated. We inject at least 10 mL of solution subcutaneously at each spot marked with an “X” without moving the needle until all tissues to be dissected are visibly and palpably tumesced.
Fig. 2.

Markings on the patient for infiltration with the WALANT solution. A, Dorsoradial aspect of the forearm. B, Volar aspect of the forearm.
Video 1. Local anaesthetic injection video.
Inject each area with enough local anesthesia that the dissected tissues are visibly and palpably swollen with tumescent solution. All injections are in the subcutaneous fat except for the PT injection periosteal insertion points (Fig. 1). It is better to err on the side of over injecting to eliminate unnecessary “top ups” of local anesthesia because of intraoperative pain.
The proposed incisions are marked out to guide the area for injections (Fig 2). Inject the patient on a stretcher outside the operating theater; so the local anesthesia has ≥30 minutes to work before you make your first incision (See Video 1 [online], which demonstrates injections given subcutaneously for PT [together with deep periosteal injection] followed by EPL, EDC, ECRB; then PL, FCR and finally PT-ECRB.).
Injection for PT
We used 27-gauge needles for injections, start with ≥30 mL over the proximal forearm (see step 1, Fig. 1) and then palpate the radius and inject 10 mL each at 2 different sites at the periosteal level. These deep injections ensure painless stripping of the periosteal insertion of PT.
Injection for EPL, EDC, and ECRB
Inject ≥20 mL of local anesthesia over the second region around Lister’s tubercle to the base of the left thumb (see step 3, Fig. 1).
Injection for PL and FCR
Inject ≥20 mL of local anesthesia at the volar part of the distal forearm corresponding to the underlying FCR and PL.
Injection for PT-ECRB Tunnel
Finally, inject ≥20 mL of local anesthesia in the area where PT will be sutured to ECRB. The surgical procedure is the standard Brand transfer.9 After the PL to EPL and FCR to EDC transfers, patients are able to actively extend the thumb and all fingers (Fig. 3). We then incise deep down to the bone to release the periosteal insertion of PT (Fig. 4). Figure 5 shows that the PT is ready to be sutured to ECRB with a Pulvertaft weave. (See Video 2 [online], which displays an intraoperative field on the dorsum of the wrist, showing EPL and EDC dissected out. Next, the volar forearm is shown with PL and FCR isolated. PL is then sutured to EPL, followed by FCR to EDC. Finally, PT, including its periosteal region, and ECRB are dissected and sutured.)
Fig. 3.

Patient actively extending his thumb and fingers fully after transfer of PL to EPL and FCR to EDC.
Fig. 4.
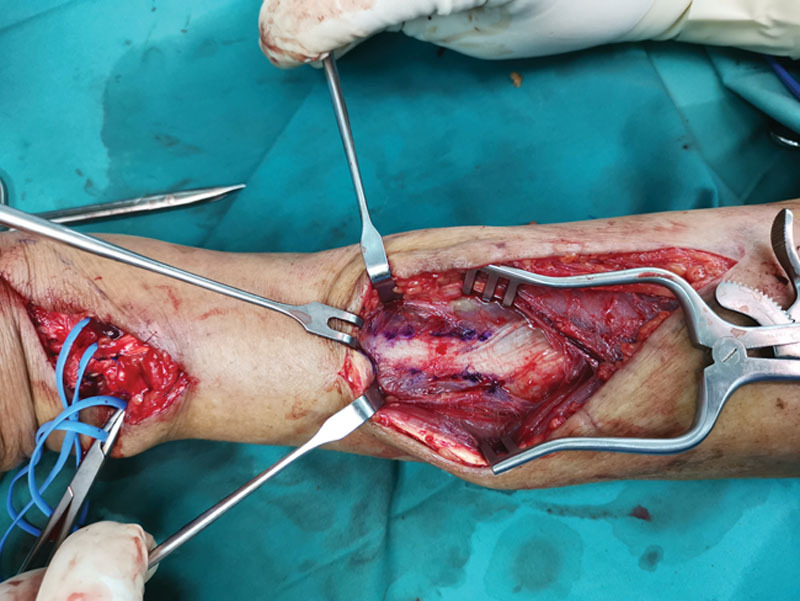
Demarcation of periosteal extension of pronator teres.
Fig. 5.

Pronator teres with periosteal extension has been stripped off the bone and is ready to be sutured to ECRB.
Video 2. Operative video.
At his 6-month follow-up, the patient in the surgical videos demonstrates good function and range of movement in Video 3 (See Video 3 [online], which displays follow-up at 6 months. This video shows the excellent progress of the patient in the injection and surgical videos who is now able to fully extend his fingers, thumb, and wrist).
Video 3. Follow-up at 6 months.
DISCUSSION
This article describes WALANT Brand tendon transfers with illustrations and video for radial nerve palsy. For forearm tendon transfer, Lalonde has suggested a highly safe dosage range of up to 200 mL of 0.25% lidocaine with 1:400,000 epinephrine to eliminate pain.4 Our experience reveals that a volume as little as 110 mL of 0.25% lidocaine with 1:400,000 epinephrine can be effective in lean patients. We prefer not to use bupivacaine because it generates annoying numbness long after the pain sensation returns.10
One of the most difficult aspects of tendon surgery is judging the tension of the transfer. We have found active movement by the awake patient during the surgery to be helpful in the finer adjustments of correct transfer tension.
We can observe a full range of active flexion and extension before skin closure. This allows us to adjust tendon transfer tension and lets the patient see the result during the surgery.
We tension the extensor repairs by first placing at least 2 temporary sutures between the powering donor tendon and the weak recipient tendon. We then ask patients to extend the affected wrist, fingers, or thumb. If they do not extend enough, we tighten the transfer by replacing the sutures more proximally on the powering tendon. If they are not able to flex the joints enough because the transfer is too tight, we move the sutures distally on the powering tendon. With the patient awake, we can immediately assess the outcome with the patient.
We use the following strategies to avoid nerve damage during the injections. We stay either in the superficial fat or on the bone with our needle tip. When we are near the median or ulnar nerves, we try not to get too close. We attempt to never elicit paresthesias. If we do elicit paresthesias, we do not inject in the nerves. We let the large volume of tumescent fluid find the nerves with passive diffusion.
One of the limitations of this technique might be trying it in the highly anxious patient who would do better with sedation during the surgery. This technique may also not be suitable to a surgeon who is not willing to inject local anesthesia slowly enough to avoid unnecessary painful local anesthesia. Surgeons who prefer not to speak to patients during surgery may also not prefer this approach because calm, reassuring communication between the surgeon and the patient helps make this an enjoyable experience for all.
We score ourselves during the injection of local anesthesia, so we know how often each patient feels pain.11 We feel that patient pain scoring of the injector is a very important part of the technique. With patient feedback, injectors get better and better at decreasing the pain of injections; therefore, we improve the patients’ experience because the injection technique becomes less painful with patient feedback and injector learning.
We have also seen that the brain is able to immediately perform the required new tendon functions at the time of WALANT with triple tendon transfer for radial nerve palsy. We feel that our success with radial nerve palsy triple tendon transfer suggests that other forearm tendon transfers can also be done wide awake.
CONCLUSION
Wide-awake surgery can be used as a safe, comfortable, and reliable method for triple tendon transfers for radial nerve palsies.
Footnotes
Published online 11 August 2020.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Lalonde DH. Wide-awake extensor indicis proprius to extensor pollicis longus tendon transfer. J Hand Surg Am. 2014;39:2297. [DOI] [PubMed] [Google Scholar]
- 2.Bezuhly M, Sparkes GL, Higgins A, et al. Immediate thumb extension following extensor indicis proprius-to-extensor pollicis longus tendon transfer using the wide-awake approach. Plast Reconstr Surg. 2007;119:1507–1512 [DOI] [PubMed] [Google Scholar]
- 3.Lalonde D. Lalonde D. Chapter 39: tendon transfers. In Wide Awake Hand Surgery: Thieme. 2016;New York, N.Y.: CRC Press, Taylor & Francis Group; 227–231 [Google Scholar]
- 4.Tang JB. Wide-awake primary flexor tendon repair, tenolysis and tendon transfer. Clin Orthop Sug. 2015;7:275–281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mohammed AK, Lalonde DH. Wide awake tendon transfers in leprosy patients in India. Hand Clin. 2019;35:67–84 [DOI] [PubMed] [Google Scholar]
- 6.Ahmad AA, Ikram MA. Plating of an isolated fracture of shaft of ulna under local anaesthesia and periosteal nerve block. Trauma Case Rep. 2017;12:40–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ahmad AA, Sabari SS, Ruslan SR, Abdullah S, Ahmad AR. Wide-awake anesthesia for olecranon fracture fixation. Hand (N.Y) 2019[E-pub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ahmad AA, Yi LM, Ahmad AR. Plating of distal radius fracture using the wide-awake anesthesia technique. J Hand Surg Am. 2018;43:1045.e1–1045.e5 [DOI] [PubMed] [Google Scholar]
- 9.Sammer DM, Chung KC. Tendon transfers part 1: principles of transfer and transfers for radial nerve palsy. Plast Recons Surg. 2009;123:169e–177e [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Calder K, Chung B, O’Brien C, et al. Bupivacaine digital blocks: how long is the pain relief and temperature elevation? Plast Reconstr Surg. 2013;131:1098–1104 [DOI] [PubMed] [Google Scholar]
- 11.Lalonde DH. “Hole-in-one” local anesthesia for wide-awake carpal tunnel surgery. Plast Reconstr Surg. 2010;126:1642–1644 [DOI] [PubMed] [Google Scholar]


