Supplemental Digital Content is available in the text.
Background:
Nonexcisional facial skin tightening has long been an elusive goal in aesthetic surgery. The “treatment gap” includes cases who are not “severe” enough for excisions surgery but not “mild” enough for most traditional noninvasive aesthetic modalities. In this retrospective review, we present the largest evaluation to date of radiofrequency (RF) skin tightening technology combination including bipolar RF (FaceTite; InMode) and fractional bipolar RF (Fractora modified to Morpheus8; InMode).
Methods:
A multicenter retrospective study was conducted between January 2013 and December 2018 using a combination of bipolar RF and fractional bipolar RF for the treatment of facial aging. Data collection included demographic information, Baker Face/Neck Classification, amount of energy used, adverse events, and patient satisfaction. Four cadaver dissections were also conducted to correlate the underlying neuromuscular anatomy with RF treatment of the lower face and neck.
Results:
Two hundred forty-seven patients (234 women and 13 men) were included in the study. Average age was 55.1 years (SD, ±8), body mass index was 24.3 (±2.4), and 9% (23/247) of patients were active smokers at the time of treatment. Patients had an average Baker Face/Neck Classification score of 3.1 (SD, ±1.4). The procedure was performed under local anesthesia in 240/247 cases (97.2%). Patients objectively improved their Baker Face/Neck Classification score by 1.4 points (SD, ±1.1). Ninety-three percent of patients indicated that they were pleased with their results and would undergo the procedure again. Complications recorded for our cohort included prolonged swelling >6 weeks (4.8%, 12/247), hardened area >12 weeks (3.2%, 8/247), and marginal mandibular neuropraxia (1.2%, 3/247), which all resolved without further intervention. When considering possible control variables, age seems to be a significant factor. That is, older patients were more likely to benefit from a larger magnitude of the treatment effect (as demonstrated by a decrease in the Baker rating from pre- to posttreatment) when compared with younger patients. However, both groups did demonstrate significant improvements across time.
Conclusion:
While this combination RF treatment (FaceTite bipolar RF and fractional bipolar RF) does not aim to replace a facelift/necklift in appropriate candidates, it does broaden the plastic surgeons’ armamentarium to potentially fill a treatment gap.
INTRODUCTION
Nonexcisional correction of facial soft tissue laxity has long been an elusive goal in aesthetic surgery. Improvements in skin texture, dyschromias, and deflation are achievable with chemical peels, lasers, microneedling, and fillers. Areas of neck adiposity may be treated using liposuction, deoxycholic acid (Kybella; Allergan, Dublin, Ireland), and cryolipolysis (CoolSculpting; Allergan), with limited improvements in properly selected patients. However, even in cases where these treatments appear successful, skin and soft tissue laxity often remain uncorrected.
There are 3 groups of patients with facial skin laxity that we characterize as part of a “treatment gap”: (1) young patients whose skin redundancy is not “severe” enough to justify a traditional excision procedure (ie, facelift/necklift), but also not “mild” enough to treat with liposuction or noninvasive procedures alone; (2) patients who have already undergone a facelift or necklift, who present with recurrent laxity, and (3) patients who may benefit from traditional face/necklift but want to avoid surgery and are willing to accept a more modest improvement.
Energy-assisted skin tightening procedures have rapidly evolved over the past decade. Multiple technologies including laser, high-intensity focused ultrasound, and radiofrequency (RF) have been developed in an attempt to meet this rising demand.1–8 RF technology has steadily gained popularity since the early 2000s, with consecutive increases annually of 10% or more.9,10 These gains encompass aesthetic surgery and numerous nonaesthetic applications (tissue electrodissection, cardiac catheter ablation, ophthalmic surgery, etc).7 Through impedance of electromagnetic current, RF waves lead to differential heating across distinct tissue types, consistent with Ohm’s law (energy = current2 × impedance × time). For example, adipose tissue is less conductive than water (higher impedance) and leads to generation of temperatures higher than those generated by muscles. Once soft tissue temperatures reach 50°C and those of the skin surface reach 40°C–42°C, there is a trigger to induce neocollagenesis, angiogenesis, and elastogenesis. Through different applications of RF energy (ie, monopolar, bipolar, multipolar, microneedling), subdermal adipose remodeling and long-term soft tissue contraction can be safely and consistently achieved.
An increasingly popular soft tissue tightening technique of the lower face and neck has been a combination procedure (Embrace Protocol; InMode, Lake Forest, Calif.) using bipolar RF (FaceTite; InMode) and fractional bipolar RF (Fractora modified to Morpheus8; InMode Aesthetics, Lake Forest, Calif.).11 The purpose of this study was to evaluate this combination therapy in the largest study to date.
METHODS
A multicenter retrospective study was conducted evaluating treatments from January 2013 to December 2018 (New York, N.Y.; Dallas, Tex.; and Verona, Italy) using a combination of bipolar RF (FaceTite; InMode Aesthetics) and RF microneedling (Fractora modified to Morpheus8; InMode Aesthetics) for the treatment of facial aging. Procedures were performed by all the authors of this study (E.D., S.T., P.R., R.J.R., C.T.C, S.A.).
All the patients voluntarily presented to respective plastic surgery practices with a desire to improve facial aesthetics. Patients included in the study were deemed to fit into 1 of the 3 aforementioned treatment gaps. Exclusion criteria included active infection, collagen disorders, immunocompromised state, medications that mitigate inflammatory response, and propensity for keloids/hypertrophic scaring. Valcyclovir was given to patients with a history of herpes simplex. All Fitzpatrick types were included in this study.
Patients were all marked in a standardized manner, identifying first the mandibular border and jowls bilaterally. The jowls were subdivided into zone 1 (above the mandibular border) and zone 2 (below the mandibular border). Areas of localized adiposity in the lower face and neck region were marked. Nontreatment zones were identified by carrying a line inferiorly perpendicular to the lip commissures (ie, marionette lines). The area medial to these lines was avoided to preserve marginal mandibular innervation to the depressor anguli oris, mentalis, and depressor labii inferioris. Five access points were identified: (1) the submental midline, (2) 1–2 cm inferior to the mandibular parasymphysial/body junction, (3) postauricular (two of the access points were bilateral). (See Video 1 [online], which displays bipolar RF markings.)
Video 1. Video 1 from “Multimodal Radiofrequency Application for Lower Face and Neck Laxity: Subdermal Adipose Remodeling and Fibro Septal Network Contraction”.
Depending on clinical circumstances and patient desires, cases were performed either under general or under local anesthesia. In cases of local anesthesia, patients were premedicated with oxycodone (5 mg) and benzodiazepam (5 mg) or both. Access sites were each injected with 2–4 ml of 2% lidocaine with epinephrine. A 14-gauge needle was used to make access ports that were slightly dilated with Stevens scissors. A spinal needle was used to slowly infiltrate tumescent solution (1 g lidocaine per liter of lactate Ringer’s solution) from deep to superficial, starting in the pre-platysmal plane and moving to the subdermal plane (approximately 100–150 ml of tumescent total). At the conclusion of tumescent infiltration, the cannula was passed through the subdermal plane to confirm adequate analgesia.
In all cases, bipolar RF was performed first. The RF settings included an internal temperature cutoff of 68°C and external cutoff temperature of 38°C. The RF cannula was used to pretunnel treatment areas for ease of treatment. The predetermined treatment areas were systematically heated to avoid heat loss when treating wide areas. RF application was performed on retrograde movement of the cannula and stopped within 1 cm of the access port to prevent overheating this area. Audible and visual cues from the RF console were used to assess temperature of tissues, and treatment was stopped after 1 minute of reaching target internal and external temperatures. (See Video 2 [online], which displays the bipolar RF technique.)
Video 2. Video 2 from “Multimodal Radiofrequency Application for Lower Face and Neck Laxity: Subdermal Adipose Remodeling and Fibro Septal Network Contraction”.
Fractional bipoar RF (Fractora modified to Morpheus8; InMode Aesthetics) was subsequently used at a depth of 2 mm and energy of 30 with 50% overlap. The handpiece was applied firmly and perpendicular to the treatment area before delivery of RF energy pulses. (See Video 3 [online], which displays fractional RF technique.) In patients with thinner skin or darker Fitzpatrick types, energy settings were reduced by 20%. Patients were seen at 1-week and at 1, 3, and 6-month intervals.
Video 3. Video 3 from “Multimodal Radiofrequency Application for Lower Face and Neck Laxity: Subdermal Adipose Remodeling and Fibro Septal Network Contraction”.
Data evaluated included demographic information, prior procedural history, anesthesia, medications, Baker Face/Neck Classification, amount of energy used, and adverse events. The primary outcome evaluated was pre- and post-procedure Baker Face/Neck Classification. Three independent plastic surgeons graded the pre- and postprocedure photographs, and subsequently a t test was used to determine statistical significance. Repeated measured analysis of variance test was used to determine any impact of control variables.
Additionally, 4 cadaver dissections were conducted to correlate the underlying neurovascular anatomy to access points and application of RF energy. These cadaver specimens were treated with the combination procedure mentioned previously, and dissections were subsequently performed to identify proximity and the potential impact on underlying specific neurovascular structures (ie, marginal mandibular nerve, facial vessels, etc).
RESULTS
Two hundred forty-seven patients (234 women and 13 men) were included in the study. Average age was 55.1 years (SD, ±8), body mass index was 24.3 (±2.4), 9% (23/247) of patients were active smokers at the time of treatment, 2% (5/247) of patients had prior neck liposuction, and 8.5% (21/247) of patients had prior facelift/necklift. Patients had an average Baker Face/Neck Classification score of 3.1 (SD, ±1.4). The procedure was performed under local anesthesia in 240/247 cases (97.2%) (50 ml 2% lidocaine, 1.5 mg epinephrine, 1.5 ml bicarbonate, in 1 L or lactated Ringer’s solution), and 2.8% (7/247) of patients underwent the procedure under general anesthesia or intravenous sedation. Average procedure time was 58 minutes (SD, ±23). All patients were given Valium and cephalosporin antibiotics before the procedure.
Average energy used per jowl was 3.2 kJ (SD, 1.1). Patients objectively improved their Baker Face/Neck Classification score by 1.4 points (SD, ±1.1). Ninety-three percent of the patients indicated they were pleased with their results and would undergo the procedure again. Average follow-up time was 2.1 years (SD, ±1.1).
To test the efficacy of the treatment, a 1-way, repeated measure t test was conducted. A decrease in the mean values of pretest to posttest Baker Face/Neck Classification rating would indicate a positive effect of the treatment. Indeed, the t test demonstrated a favorable effect of the treatment in all the 247 patients. The pretest mean value was 2.66 (SD = 0.72), and the posttest mean value was 1.86 (SD = 0.64). This mean difference (μ = 0.81, SD = 0.46) was statistically significant: t(237) = 27.34, P < 0.001, and the effect size was large (D = 1.76). In other words, the mean values of the patients’ Baker Face/Neck Classification decreased as a result of the treatment. (See supplemental figure 1, Supplemental Digital Content 1, which displays pre- and posttreatment Baker Face/Neck Classification scores, http://links.lww.com/PRSGO/B410.)
However, it is also possible that several control variables may have had an unhypothesized effect on the relationship. Thus, a 1-way, repeated measures analysis of variance test was conducted, inclusive of control variables. These control variables were (1) gender, (2) smoking habit, (3) liposuction history, (4) weight, (5) age (dichotomized at the median value, 55), (6) body mass index, (7) right jowl energy (in kJ), (8) left jowl energy (in kJ), and (9) neck energy (in kJ). Although 247 valid cases were present, complete data were available for only 238 patients; thus, data from 9 patients were excluded in these analyses. The following table presents the mean values or percentages of the control variables in the overall fitted model. (See table, Supplemental Digital Content 2, which displays the descriptive statistics, http://links.lww.com/PRSGO/B411.)
When considering the overall model, it is clear from the analysis that the treatment was effective in reducing the Baker Face/Neck Classification rating: pretreatment Baker classification μ = 2.62 (SE = 0.03), pretreatment Baker classification μ = 1.84 (SE = 0.03); F(1, 208) = 11.36, P = 0.001. None of the control variables was statistically significant, except for age. A significant treatment by age interaction effect was present: F(1, 208) = 17.53, P < 0.001. This simply indicates that the Baker Face/Neck Classification pre- and posttreatment ratings are different at different age groups. The mean values demonstrates that while older patients seem to benefit from the treatment more than younger patients by a larger magnitude, both age groups still show marked and significant improvements in their Baker Face/Neck Classification scores from pretreatment to posttreatment, as evidenced by Supplemental Digital Content 3. (See supplemental figure 2, Supplemental Digital Content 3, which displays Baker Face/Neck Classification scores by treatment age, http://links.lww.com/PRSGO/B412.)
Complications recorded for our cohort included prolonged swelling >6 weeks (4.8%, 12/247), hardened area >12 weeks (3.2%, 8/247), and marginal mandibular neuropraxia (1.2% 3/247), which all resolved without further intervention. There were no repeat treatments or cases requiring operative interventions following RF treatment.
DISCUSSION
While this combination RF treatment (FaceTite bipolar RF and fractional bipolar RF) does not aim to replace a facelift/necklift in appropriate candidates, it does broaden the plastic surgeons’ armamentarium to potentially fill a treatment gap. Also, it provides patients with an option to improve facial soft tissue laxity without a traditional surgery.
In recent years, RF has emerged as an effective treatment to achieve nonablative skin tightening.6,7,10,12,13 Heating the dermal tissue to 42°C has been shown to trigger a healing cascade that leads to stimulation of new collagen and elastin formation.9,14–16 In animal studies, after 10 minutes of exposure to temperatures of 39°C–43°C, the amount of collagen increased from an average of 9% before therapy to 25.9% after a 3-month follow-up period compared with no change in the untreated areas.4,17 Clinical studies on RF-assisted liposuction have shown up to 25% area contraction at 6 months and 35%–40% area contraction achieved at 1 year.10,18–20 Other studies have similarly shown through electron microscopy that collagen fibrils had a greater diameter after RF treatment. In addition, Northern blot analysis has confirmed microinflammmatory stimulation of fibroblasts and other substances that enhance dermal structure.21 RF has not only been proved effective for skin tightening, but it has also been studied and proved effective in diminishing adipocytes.14
A number of RF applications are available to apply this energy in different ways (monopolar, bipolar, multipolar, and microneedling). The 2 RF delivery methods (bipolar RF and fractional bipolar RF) used in this study help achieve different treatment goals. The bipolar RF applicator uses a small 1.8-mm diameter, 13-cm long, silicone-coated RF-emitting probe. This directs electrical current flow from the internal to the external electrodes connected by the handpiece. As current is applied, the heat coagulates subcutaneous fat in close proximity to the internal probe and denatures the reticular dermis but preserves the papillary dermis. The controlled heating allows for immediate tightening of the collagen triple helix via breakdown of hydrogen bonds in the collagen, causing shrinkage of the normal collagen structure, as well as induction of the healing cascade, leading to neocollagenesis, elastin remodeling, and angiogenesis over the following 3–4 months.9 In addition, using a parachute analogy, the application of heat tightens the overlying fibroseptal networks (strings) and serves to uniformly contract the overlying skin (parachute). Complications are minimized by internal and external temperature, and impedance probes to rapidly detect (10×/ms) the soft tissue environment and automatically turns off RF energy if beyond the preset safety parameters (Figs. 1, 2).
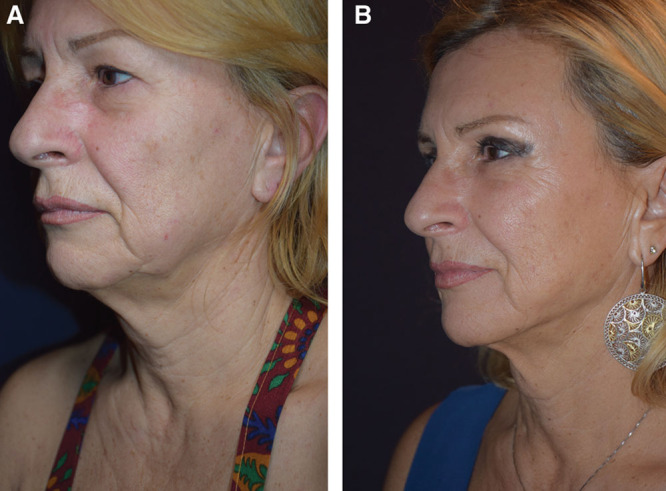
Fig. 1.

Results of radiofrequency-assisted liposuction with fractional bipolar radiofrequency. A, The patient pretreatment. B, The patient 12 months postoperative.
Fig. 2.
Results of radiofrequency-assisted lower face and neck treatment with fractional bipolar radiofrequency. A, the 64-year-old female patient pretreatment. B, results 24 months postoperative.
In bipolar RF, the penetration depth is half of the distance between the electrodes, meaning the energy does not reach beyond the epidermis. Many attempt to circumvent this limitation by combining RF with other technologies to penetrate deeper, such as application of a vacuum to thin skin, infrared light pretreatment to change impedance, or cooling procedures to increase the penetration depth.4 In this study, the effect of bipolar RF treatment was augmented by performing fractional bipolar RF in the same session. Fractional bipolar RF (Fractora modified to Morpheus8; InMode Aesthetics) deploys RF-emitting needles at variable programmable depths and energies depending on the region being treated. Unlike fractional CO2 or erbium, the fractional bipolar RF resurfacing can induce 3 types of effects—minimal superficial ablation for dyschromias and rhytids, controlled dermal coagulation for tissue renewal, and overall volumetric heating for collagen stimulation.4 Fractional photothermolysis creates thermal injury that tapers as it descends deeper. In contrast, fractional bipolar RF creates zones of dermal injury narrowest at the epidermis with conical enlargement as the microneedles descend.10 When the RF needles penetrate deep into the dermis, there is a “molding” component of the subdermal adipose tissue which we term “subdermal adipose remodeling.” Hruza et al16 reported that 90% of patients with skin types II–IV showed an improvement in smoothness and rhytids, and 87% had improved in skin tightness. Seo et al13 compared facial soft tissue laxity improvement with RF versus surgical facelift using blinded grading of photographs. They demonstrated a 49% improvement in skin laxity relative to baseline for the surgical facelift compared with 16% for the fractional bipolar RF. Further, the mean laxity improvement from a single fractional bipolar RF treatment was 37% of the surgical facelift.13 Peterson et al22 also studied objective measurements of mechanical skin properties and demonstrated a statistically significant improvement (5%–12% decrease in Young’s modulus and 10%–16% decrease in retraction time), as well as 1.42 grade improvement on the Fitzpatrick scale for wrinkles, and 0.66 on the Alexiades scale for skin laxity, increasing to 1.57 and 0.70 improvement at 6 months. Patient satisfaction was noted to be “very high” for >90% of patients.22 A clinical study of the microneedle fractional bipolar RF handpiece (Intensif handpiece; EndyMed, Caesarea, Israel) demonstrated a significant improvement after 2 sessions and after 4 and 12 weeks of follow-up.6 A similar system (Scarlet, Korea) was studied in 3 consecutive sessions 4 weeks apart. Immunohistochemical staining (fibrillin-1) showed a significant increase in dermal collagen content at 4 weeks after 3 sessions when compared with the baseline, as well as a significant increase in fibrillin-1 density from the dermal–epidermal junction to the deep dermis compared with the baseline.23
Other studies have demonstrated the efficacy of combined multimodal RF application for facial aesthetic purposes. Kaplan et al used 3 RF delivery methods together (nonablative skin tightening, RF fractional skin resurfacing, and microneedling RF) on 14 subjects, showing improvements (>50%) in skin texture, laxity, and rhytids in 43% of the cohort without adverse effects or a significant downtime.24 Previous studies have shown the efficacy of nonablative multisource RF as a single modality for face/body contouring.15,20,25 Other studies have shown the efficacy of RF microneedling as a single modality26 and the efficacy of a combination of nonablative RF and fractional skin resurfacing.27 Similarly to our findings, Mulholland in Hruza et al. identified the benefit of combining bipolar RF and fractional RF, stating that combining these applications allows for thermal stimulation for an “inside-outside dermal stimulation,” which can induce both an ablative rejuvenation of dyschromia, fine lines, and rhytides and a nonablative deeper dermal tightening.16 Our study findings were consistent with Mulholland’s conclusion that combination therapy can deliver safe and consistent soft tissue rejuvenation.
The anatomic dissections performed as part of this study demonstrated the important surgical anatomy relevant to this procedure. Specifically, the marginal mandibular nerve was found to be always above the inferior border of the mandible while anterior to the facial artery. The position was more variable posterior to the facial artery, in which case it was above the inferior border of the mandible in majority of cases. Importantly, consistent with prior anatomic studies, at approximately 2 cm from the oral commissure, the marginal mandibular nerve divides and subdivides to enter the lip depressors. At this anatomic location, the skin and underlying muscle planes are closely adherent. It is for this anatomic reason that we elect to not treat areas medial to the marionette lines. Using this anatomic knowledge and aforementioned access ports, we found no nerve injuries (ie, transection, neuropraxia) and no extension of the device heat signature in proximity to the marginal mandibular nerve, consistent with the relatively low complication rate in the clinical arm of the study.
CONCLUSIONS
Combination therapy of bipolar RF and fractional RF had a positive effect on reducing the Baker Face/Neck Classification rating. When considering possible control variables, older patients were more likely to benefit from a larger magnitude of the treatment effect (as demonstrated by a decrease in the Baker rating from pre- to posttreatment) compared to younger patients. However, both groups did demonstrate significant improvements across time.
PATIENT CONSENT
Patients provided written consent for the use of their images.
Supplementary Material
Footnotes
Published online 26 August 2020.
Disclosure: Dr. Dayan is consultant at InMode; he receives book royalties from Thieme & Elsevier and is a co-investigator of Allergan, Galderma, and MTF. Dr. Rovatti is consultant at InMode. Dr. Aston is consultant at InMode. Dr. Chia is consultant at InMode. Dr. Rohrich receives book royalties from Thieme and instrument royalties from Micrins. He is a co-investigator of Allergan, Galderma, MTF, and InMode. Dr. Theodorou is consultant at InMode.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Alster TS, Graham PM. Microneedling: a review and practical guide. Dermatol Surg. 2018;44:397. [DOI] [PubMed] [Google Scholar]
- 2.Brightman L, Weiss E, Chapas AM, et al. Improvement in arm and post-partum abdominal and flank subcutaneous fat deposits and skin laxity using a bipolar radiofrequency, infrared, vacuum and mechanical massage device. Lasers Surg Med. 2009;41:791–798 [DOI] [PubMed] [Google Scholar]
- 3.Chia CT, Theodorou SJ, Hoyos AE, et al. Radiofrequency-assisted liposuction compared with aggressive superficial, subdermal liposuction of the arms: a bilateral quantitative comparison. Plast Reconstr Surg Glob Open. 2015;3:e459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fritz K, Salavastru C. Ways of noninvasive facial skin tightening and fat reduction. Facial Plast Surg. 2016;32:276–282 [DOI] [PubMed] [Google Scholar]
- 5.Iriarte C, Awosika O, Rengifo-Pardo M, et al. Review of applications of microneedling in dermatology. Clin Cosmet Investig Dermatol. 2017;10:289–298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sadick NS, Makino Y. Selective electro-thermolysis in aesthetic medicine: a review. Lasers Surg Med. 2004;34:91–97 [DOI] [PubMed] [Google Scholar]
- 7.American Society of Plastic Surgeons. New statistics reveal the shape of plastic surgery. 2018. Available at https://www.plasticsurgery.org/news/press-releases/new-statistics-reveal-the-shape-of-plastic-surgery. Accessed November 10, 2018
- 8.American Society of Aesthetic Plastic Surgery. Cosmetic surgery national data bank statistics. Aesthet Surg J 2018;38:suppl 31–24 [DOI] [PubMed] [Google Scholar]
- 9.Hodgkinson DJ. Clinical applications of radiofrequency: nonsurgical skin tightening (thermage) Clin Plast Surg. 2009;36:261–268, viii [DOI] [PubMed] [Google Scholar]
- 10.Sadick N, Rothaus KO. Minimally invasive radiofrequency devices. Clin Plast Surg. 2016;43:567–575 [DOI] [PubMed] [Google Scholar]
- 11.Dayan E, Chia C, Burns AJ, et al. Adjustable depth fractional radiofrequency combined with bipolar radiofrequency: a minimally invasive combination treatment for skin laxity. Aesthet Surg J 2019;39:suppl 3S112–S119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Irvine Duncan D. Nonexcisional tissue tightening: creating skin surface area reduction during abdominal liposuction by adding radiofrequency heating. Aesthet Surg J 2013;33:1154–1166 [DOI] [PubMed] [Google Scholar]
- 13.Seo KY, Yoon MS, Kim DH, et al. Skin rejuvenation by microneedle fractional radiofrequency treatment in Asian skin: clinical and histological analysis. Lasers Surg Med. 2012;44:631–636 [DOI] [PubMed] [Google Scholar]
- 14.Hantash BM, Ubeid AA, Chang H, et al. Bipolar fractional radiofrequency treatment induces neoelastogenesis and neocollagenesis. Lasers Surg Med. 2009;41:1–9 [DOI] [PubMed] [Google Scholar]
- 15.Harth Y. Painless, safe, and efficacious noninvasive skin tightening, body contouring, and cellulite reduction using multisource 3DEEP radiofrequency. J Cosmet Dermatol. 2015;14:70–75 [DOI] [PubMed] [Google Scholar]
- 16.Hruza G, Taub AF, Collier SL, et al. Skin rejuvenation and wrinkle reduction using a fractional radiofrequency system. J Drugs Dermatol. 2009;8:259–265 [PubMed] [Google Scholar]
- 17.Weiss R, Weiss M, Beasley K, et al. Operator independent focused high frequency ISM band for fat reduction: porcine model. Lasers Surg Med. 2013;45:235–239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Theodorou SJ, Paresi RJ, Chia CT. Radiofrequency-assisted liposuction device for body contouring: 97 patients under local anesthesia. Aesthetic Plast Surg. 2012;36:767–779 [DOI] [PubMed] [Google Scholar]
- 19.Theodorou SJ, Del Vecchio D, Chia CT. Soft tissue contraction in body contouring with radiofrequency-assisted liposuction: a treatment gap solution. Aesthet Surg J 2018;38:suppl 2S74–S83 [DOI] [PubMed] [Google Scholar]
- 20.Royo de la Torre J, Moreno-Moraga J, Munoz E, et al. Multisource, phase-controlled radiofrequency for treatment of skin laxity: correlation between clinical and in-vivo confocal microscopy results and real-time thermal changes. J Clin Aesthet Dermatol. 2011;4:28–35 [PMC free article] [PubMed] [Google Scholar]
- 21.Zelickson BD, Kist D, Bernstein E, et al. Histological and ultrastructural evaluation of the effects of a radiofrequency-based nonablative dermal remodeling device: a pilot study. Arch Dermatol. 2004;140:204–209 [DOI] [PubMed] [Google Scholar]
- 22.Peterson JD, Palm MD, Kiripolsky MG, et al. Evaluation of the effect of fractional laser with radiofrequency and fractionated radiofrequency on the improvement of acne scars. Dermatol Surg. 2011;37:1260–1267 [DOI] [PubMed] [Google Scholar]
- 23.Seo KY, Kim DH, Lee SE, et al. Skin rejuvenation by microneedle fractional radiofrequency and a human stem cell conditioned medium in Asian skin: a randomized controlled investigator blinded split-face study. J Cosmet Laser Ther. 2013;15:25–33 [DOI] [PubMed] [Google Scholar]
- 24.Kaplan H, Kaplan L. Combination of microneedle radiofrequency (RF), fractional RF skin resurfacing and multi-source non-ablative skin tightening for minimal-downtime, full-face skin rejuvenation. J Cosmet Laser Ther. 2016;18:438–441 [DOI] [PubMed] [Google Scholar]
- 25.Elman M, Vider I, Harth Y, et al. Non-invasive therapy of wrinkles and lax skin using a novel multisource phase-controlled radio frequency system. J Cosmet Laser Ther. 2010;12:81–86 [DOI] [PubMed] [Google Scholar]
- 26.Elawar A, Dahan S. Non-insulated fractional microneedle radiofrequency treatment with smooth motor insertion for reduction of depressed acne scars, pore size, and skin texture improvement: a preliminary study. J Clin Aesthet Dermatol. 2018;11:41–44 [PMC free article] [PubMed] [Google Scholar]
- 27.Elman M, Harth Y. Novel multi-source phase-controlled radiofrequency technology for non-ablative and micro-ablative treatment of wrinkles, lax skin and acne scars. Laser Ther. 2011;20:139–144 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


