Abstract
Many surgical procedures have been developed for the treatment of post-traumatic thoracolumbar kyphosis. But there is a significant controversy over the ideal management. The aim of this study was to illustrate the technique of modified grade 4 osteotomy for the treatment of post-traumatic thoracolumbar kyphosis and to evaluate clinical and radiographic results of patients treated with this technique.
From May 2013 to May 2018, 42 consecutive patients experiencing post-traumatic thoracolumbar kyphosis underwent the technique of modified grade 4 osteotomy, and their medical records were retrospectively collected. Preoperative and postoperative sagittal Cobb angle, visual analog scale (VAS), Oswestry disability index (ODI), and American Spinal Injury Association (ASIA) were recorded. The average follow-up period was 29.7 ± 14.2 months.
The operation time was 185.5 ± 26.8 minutes, the intraoperative blood loss was 545.2 ± 150.1 mL. The Cobb angles decreased from 38.5 ± 3.8 degree preoperatively to 4.2 ± 2.6 degree 2 weeks after surgery (P < .001). The VAS reduced from 6.5 ± 1.1 preoperatively to 1.5 ± 0.9 at final follow-up (P < .001), and the ODI reduced from 59.5 ± 15.7 preoperatively to 15.9 ± 5.8 at final follow-up (P < .001). Kyphotic deformity was successfully corrected and bony fusion was achieved in all patients. Neurologic function of 7 cases was improved to various degrees.
Modified grade 4 osteotomy, upper disc, and upper one-third to half of pedicle are resected, is an effective treatment option for post-traumatic thoracolumbar kyphosis. However, the long-term clinical effect still needs further studies.
Keywords: kyphosis, osteotomy, post-traumatic, thoracolumbar
1. Introduction
It is estimated that >50,000 people suffer from spinal traumatic fracture each year in the United States. The thoracolumbar junction from T11 to L2 is the most common area of spinal fracture.[1] Most traumatic thoracolumbar fractures have a good healing effect after complete and timely treatment. However, post-traumatic thoracolumbar kyphosis can occur in a proportion of thoracolumbar fractures due to delayed treatment, weight bearing too early, inadequate immobilization, incorrect surgical procedure, or fixation.[2] The main purpose of surgical treatment for kyphosis is to restore normal sagittal balance, perform nerve decompression, and improve pain and neurologic symptoms.[3]
Based on the standardized classification by Schwab, grade 4 osteotomy is defined as the resection of the pedicle, partial vertebral body, and adjacent disc.[4] Hu et al reported pedicle subtraction osteotomy (PSO) and disc resection with cage placement, classified in grade 4 osteotomy, in the treatment of post-traumatic thoracolumbar kyphosis.[5] We adopted modified grade 4 osteotomy which resected the upper one-third to half of pedicle of the target vertebra, partial vertebral body, and adjacent disc. The purpose of this retrospective study was to illustrate the technique of modified grade 4 osteotomy for the treatment of post-traumatic thoracolumbar kyphosis and to evaluate clinical and radiographic results of patients treated with this technique.
2. Materials and methods
2.1. Patients
From May 2013 to May 2018, 42 consecutive patients experiencing post-traumatic thoracolumbar kyphosis underwent 1-stage posterior modified grade 4 osteotomy. This study was conducted with approval from the Ethics Committee of The Third Hospital of Shijiazhuang. Written informed consent was obtained from all patients.
The main complaint of all patients was back pain. Seven patients also complained leg weakness and 3 patients with radiating pain. For 7 patients with neurological deficits, American Spinal Injury Association (ASIA) scale grade was C in 1 patient, D in 6 patients. All cases had been managed conservatively and all patients have no history of spinal surgery for the fractured vertebra. The mean time interval between fracture and kyphosis correction was 27.6 ± 17.2 months (range 6–72 months). The level of kyphotic apices was T11 in 4 cases, T12 in 20 cases, L1 in 12 cases, and L2 in 6 cases. The indications for surgery were as follows: sagittal Cobb angle exceeding 30 degree, pain refractory to conservative treatment for at least 3 months, and neurological deficit such as leg weakness or radiating pain.[5]
2.2. Surgical procedures
All spinal surgeries were performed with somatosensory-evoked potentials and transcranial motor-evoked potentials for neurophysiologic monitoring. The patients were placed prone on the operating table after general anesthesia. A posterior midline incision was made, and subperiosteal dissection performed to the tip of the transverse process of the vertebra or rib head at the predetermined level. With C-arm guidance, multiaxial pedicle screws (Weigao Orthopedic, Shandong, China) were then inserted by freehand technique 2 to 3 levels above and 2 to 3 levels below the damaged vertebral body. Bleeding was controlled by hemostatic gauze and electric cauterization.
The modified grade 4 osteotomy was then performed (Fig. 1). Partial spinous process of the target vertebrae and the proximal vertebrae were removed. Burr drill was used to completely resect bilateral inferior articular processes of the proximal vertebra, as well as partial lower edge of the lamina of the proximal vertebra. Rongeur was used to resect bilateral superior articular process of the target vertebra, as well as partial upper edge of the lamina of the target vertebra. Potential decompression of the lamina was performed to enlarge the volume of the spinal canal. The lamina should be resected finitely so that the lamina gap can be closed after the osteotomy is completed (Fig. 2). A temporary fixed rod was installed on 1 side. The dural sac was revealed after removing the ligamentum flavum. Care was taken to protect the exiting nerve root. Then, the upper one-third to half of pedicle of the target vertebra was resected with burr drill and osteotome. Subsequently, the damaged disc and the upper one-third to half of the target vertebral body were resected using an osteotome and curet. The thin posterior vertebral wall was removed later.
Figure 1.
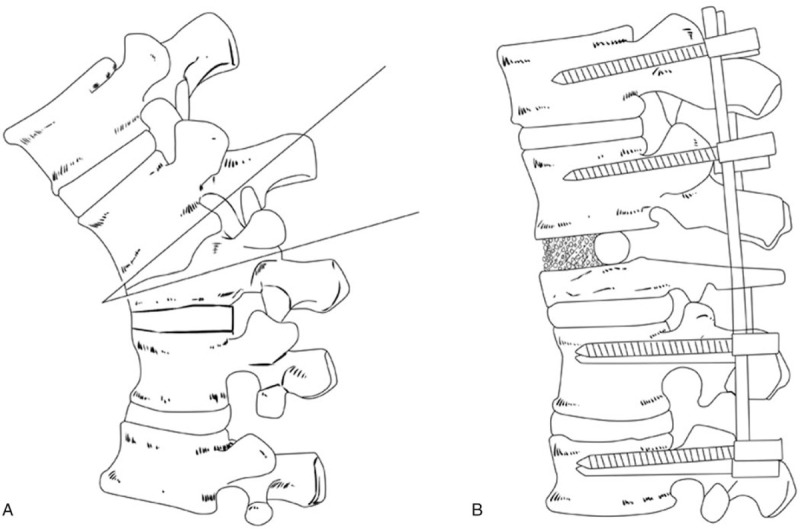
(A) The injured upper disc, the upper one-third to half of pedicle of the target vertebra, and posterior elements were removed. (B) Small bone particles were implanted in the anterior column and blocky spinous processes were implanted in the middle column, effective kyphosis correction was achieved, and the spinal column height was restored.
Figure 2.
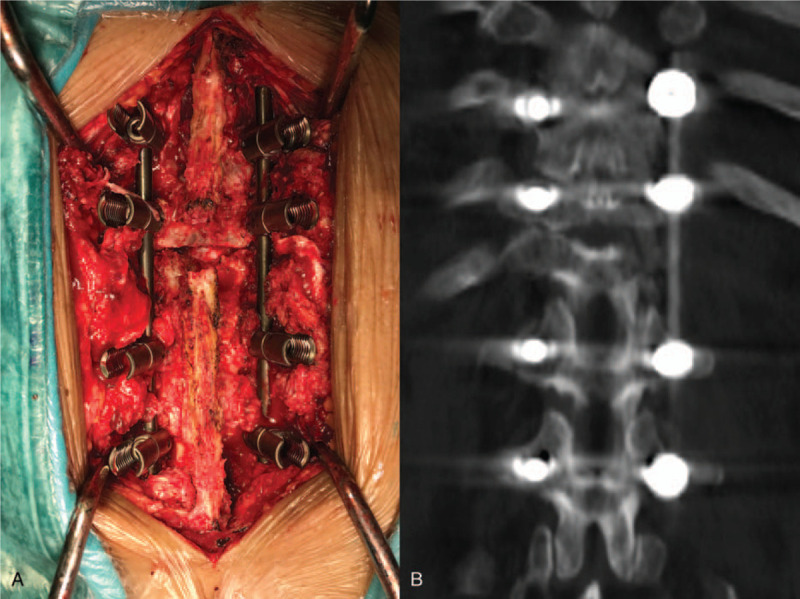
(A) Potential decompression of the lamina was performed to enlarge the volume of the spinal canal. (B) The lamina gap can be closed after the osteotomy is completed.
After the aforementioned procedure was performed on both sides, the osteotomy space was filled with adequate auto- and allograft bone to create “bone-to-bone" contact. Small bone particles were implanted in the anterior column through the bilateral gap. Blocky spinous processes were implanted in the middle column and serve as a fulcrum. The temporarily fixed rod was then replaced with 2 permanent orthopedic rods in accordance with sagittal physiological radian. The osteotomy space was closed gradually and alternately while confirming no compression to the spinal cord and nerve roots. Finally, posterolateral bone grafting at the fixation region was performed. Negative pressure drainage was applied and the wound was closed in layers.
Postoperatively, the drainage tube was removed when the drainage volume was <50 mL/24 hours after 3 to 5 days. Patients were allowed out of bed with a custom-made plastic orthosis at 5 to 7 days after operation. The plastic orthosis was kept for at least 3 months.[2,5–10]
2.3. Radiologic and clinical evaluation
Radiographs and clinical evaluation was performed preoperatively, 2 weeks after surgery, and at the final follow-up (Fig. 3). Radiographs of the standing full-length spine were available for all patients. The sagittal Cobb angle was measured to assess kyphosis deformity on lateral radiograph. The focal kyphotic angle was defined between the upper end plate of the vertebra 1 above the apical vertebra and the lower end plate of the vertebra one below the apical vertebra. As described by Brantigan et al, the presence of trabecular bone bridging at the osteotomy site was considered as fusion.[5,11–15] All radiological evaluations were performed by an independent surgeon who was not involved in patient treatment. A 3-dimensional computed tomography (CT) scan was performed to confirm it if the fusion was questionable. Clinical outcome and functional status were assessed using visual analog scale (VAS), Oswestry disability index (ODI), and ASIA. Operation time, blood loss, and complications were collected from the clinical notes.
Figure 3.
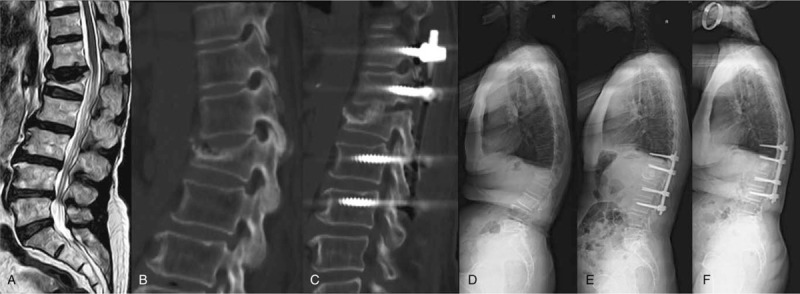
A 70-year-old female patient who is suffering from severe back pain for 1 year due failure of conservative treatment. Preoperative lateral radiograph (D), CT (B), and MRI (A) show that the apex of kyphosis is located at L1 and the Cobb angle is 36 degree. The Cobb angles at 2 weeks (E) and 1 year (F) after surgery were 6 and 7 degree, respectively. Postoperative CT (C) shows the technique of modified grade 4 osteotomy.
2.4. Statistical analysis
Each variable was presented as mean ± SD (standard deviation). Statistical analyses were performed using paired t tests (SPSS version 21.0, IBM). Normality was assumed, and a P value <.05 was considered significant.
3. Results
Modified grade 4 osteotomy was performed in all patients. The average follow-up period was 29.7 ± 14.2 months (range 12–72 months). The average operation time was 185.5 ± 26.8 minutes (range 140–250 minutes) with a mean intraoperative blood loss of 545.2 ± 150.1 mL (range 300–900 mL) (Table 1). Dural tear was encountered in 1 case. For this patient, the drainage tube was removed 7 days after operation and the incision of drainage tube was sutured. The patient recovered without further complications. One patient suffered wound infection and was recovered with conservative treatment, local wound care, and appropriate antibiotics. There was no other severe complication.
Table 1.
Summary of preoperative and intraoperative characteristics.

The mean VAS score was reduced from preoperative 6.5 ± 1.1 to 1.5 ± 0.9 at final follow-up (P < .001) (Table 2). The mean ODI decreased from 59.5 ± 15.7 preoperatively to 15.9 ± 5.8 at final follow-up (P < .001). Some patients exhibited improved neurological function at final follow-up. The preoperative ASIA grade was C in 1 patient and improved to grade D. The preoperative ASIA grade was D in 6 patients and all improved to grade E.
Table 2.
Summary of clinical and radiologic outcomes.
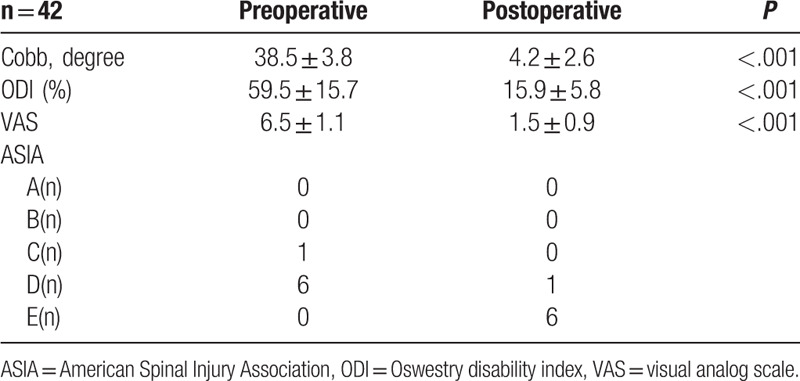
x-Ray radiographs showed that kyphotic Cobb angle was 38.5 ± 3.8 degree preoperatively, 4.2 ± 2.6 degree at 2 weeks after surgery, and 4.5 ± 2.5 degree at last follow-up. Data analyses indicated that Cobb angle after modified grade 4 osteotomy was significantly improved, compared to preoperative (P < .001). No obvious correction loss was noted at final follow-up. At final follow-up, solid fusion was obtained in all patients according to radiological evidence, and no implant failures were found.
4. Discussion
Local instability, muscle or disc degeneration, and canal compromise were the main pathological changes in post-traumatic thoracolumbar kyphosis. Symptoms of post-traumatic thoracolumbar kyphosis include local muscle fatigue or pain, focal deformity, and neurological deficits. There were several explanations for the causes of intractable pain: disc injury, bony nonunion, adjacent levels of apical vertebra bear greater stress due to compensatory kyphosis, excessive compensatory lumbar lordosis and the stress on facet joints cause low back pain.[2] Neurological deficits might derive from degenerative discs, the direct compression of the spinal cord caused by the apical vertebral body, kyphosis stretching the spinal cord, and hypertrophic ligaments.
Indications for surgical intervention include pain refractory to conservative treatment for at least 3 months, sagittal Cobb angle exceeding 30 degree, and neurological deficit such as leg weakness or radiating pain. Many surgical procedures have been developed for the treatment of post-traumatic thoracolumbar kyphosis. But there is a significant controversy over the ideal management.
Surgical approaches for kyphosis include anterior, posterior, and anterior-posterior combined approaches. Takenaka et al[16] compared 3 surgical approaches in the treatment of osteoporotic vertebral fractures. The operation time was significantly longer in anterior-posterior combined group than in the other 2 groups. The postoperative correction of kyphosis was significantly greater in posterior group than in anterior group. Better outcomes were obtained in posterior group in back pain relief at the end point, ambulatory ability at the end point, and average loss of correction. Suk et al[6] compared the surgical results between combined anterior-posterior procedures and posterior procedures in the treatment of post-traumatic kyphosis. They found that the posterior procedure demonstrated a better surgical result with significant less mean operative time and mean blood loss. Currently, the 1-stage posterior approach is more popular for the treatment of post-traumatic thoracolumbar kyphosis.
Several osteotomy forms have been taken to correct the post-traumatic thoracolumbar kyphosis. Frank Schwab comprehensively analyzed the osteotomy methods reported in the literature and divided the osteotomy technique into six grades.[4]
PSO, classified in grade 3 osteotomy, was first described by Thomasen[17] for the correction of kyphosis in ankylosing spondylitis patients. This technique shortens the posterior column but does not lengthen the anterior column, lowering the risk of spinal cord injury. Xi et al[7] performed PSO in 19 patients with post-traumatic kyphosis, achieved an average correction of 40.2 degree. Wu et al[18] performed posterior PSO in 13 patients with post-traumatic kyphosis to obtain an average correction angle of 38.8 degree.
However, all the posterior ligamentous structures and bony elements in osteotomy site were removed when performing PSO. Only the anterior longitudinal ligament and adjacent intervertebral discs were remained to maintain the stability of the spine in osteotomy site, which might lead to rod fracture. According to Smith et al,[19] the rate of rod fracture among cases that included a PSO was 22.0%, and the fracture occurred at or adjacent to the level of the PSO. Upadhyaya et al[20] reported a case with spondylolisthesis following a PSO. Moreover, in some cases, the injured upper level disc after fractures of the thoracolumbar spine may fall into the vertebrae through the collapsed end plate, in which PSO are not suitable.[21]
Gao et al[22] reported modified PSO, classified in grade 4 osteotomy, in the treatment of post-traumatic thoracolumbar kyphosis. In the process, upper disc and upper two-thirds of the index pedicle were resected and the lower facet joint were preserved. The mean correction of focal kyphotic deformity was 34 degree. The potential advantages of this modified PSO are that it not only promotes direct interbody fusion in the upper disc space, but it also provides better stability by preserving the integrity of the lower facet joint.[22]
The main advantages of resecting the upper disc are the added amount of correction, and the additional fusion surface. With a large interspace, however, the spinal column will be excessively shortened which may result in buckling of the dura and spinal cord.
Hu et al[5] reported PSO and disc resection with cage placement in the treatment of post-traumatic thoracolumbar kyphosis. In their procedure, after removing the upper disc and posterior elements, a cage containing autogenous bone was put at the anterior column between the lower endplate of the upper vertebra and the osteotomy surface to restore the spinal column height and avoid potential spinal cord curving or kinking. However, since the upper endplate of the fractured vertebral body has been removed, the intervertebral cage has a risk of sinking.[23] In addition, the osteotomy technique described by Hu et al was a traditional grade 4 osteotomy which the posterior elements including the spinous process, bilateral lamina, transverse process, and the adjacent facet joints at the level of apical vertebra were needed to be removed. So, only the anterior longitudinal ligament and adjacent intervertebral disc were remained to maintain the stability of the spine bellow the osteotomy site, which also had the risk of rod fracture. In addition, bilateral lamina of apical vertebra was resected completely. So the lamina gap cannot be closed after the osteotomy was completed. Posterolateral bone grafting in osteotomy site cannot be performed.
After comprehensive analysis of these osteotomy techniques, we adopted modified grade 4 osteotomy for the treatment of post-traumatic thoracolumbar kyphosis.
There were several technical points in modified grade 4 osteotomy. Firstly, the upper one-third to half of pedicle of the target vertebra was resected and the lower facet joint were preserved, which can provide better stability by preserving the integrity of the lower facet joint. Second, the lamina was resected finitely so that the lamina gap can be closed after the osteotomy was completed and posterolateral bone grafting in osteotomy site can be performed. Third, upper disc was resected, which can provide more correction of kyphosis and additional fusion surface. Fourth, the osteotomy space was filled with adequate auto- and allograft bone to create “bone-to-bone" contact, which can achieve solid fusion. At the same time, the same elastic modulus and larger bone contact area made it low risk of sinking. Fifth, small bone particles were implanted in the anterior column and blocky spinous processes were implanted in the middle column, which can restore the spinal column height and avoid potential spinal cord curving or kinking. Finally, like closing-opening wedge osteotomy, blocky spinous processes in the middle column serve as a fulcrum, the correction is achieved by closing the posterior column, and creating an open wedge of the anterior column.[8]
In our study, 42 patients were treated by modified grade 4 osteotomy, and the maximum correction angle was 40 degree with an average of 34.2 degree. The operation time was 185.5 ± 26.8 minutes, and the intraoperative blood loss was 545.2 ± 150.1 mL. The operation time was less than previous studies which reported grade 4 osteotomy (260.6 minutes reported by Hu et al[5] and 275 minutes reported by Jo et al[2]). The intraoperative blood loss was less than previous studies (643.3 mL reported by Hu et al[5] and 1585 mL reported by Jo et al[2]). So the modified grade 4 osteotomy is an effective and safe treatment option for the treatment of post-traumatic thoracolumbar kyphosis. There are several limitations in this study. First, it is a retrospective, single-institution study. Second, there is no control group and sample size is small. Third, follow-up time is insufficient.
5. Conclusions
Modified grade 4 osteotomy was a good choice for post-traumatic thoracolumbar kyphosis, which contributes to satisfactory kyphosis deformity correction and clinical results. Our study suggests that it was effective method to treat posttraumatic thoracolumbar kyphosis. However, the long-term clinical effect still needs further studies.
Level of evidence based on the Evidence-Based Guidelines of the North American Spine Society: Level IV, Grade I.[24]
Author contributions
Data curation: Zhen-Fang Gu.
Formal analysis: Zheng-Qi Zhao.
Investigation: Liang Ren.
Methodology: Jin-He Yu.
Software: Li-Min Wang.
Supervision: Wen-Yuan Ding.
Validation: Shu-Bing Hou.
Writing – original draft: Feng-Yu Liu, Xian-Ze Sun.
Writing – review & editing: Feng-Yu Liu, Wen-Yuan Ding.
Footnotes
Abbreviations: ASIA = American Spinal Injury Association, ODI = Oswestry Disability Index, PSO = pedicle subtraction osteotomy, SD = standard deviation, VAS = visual analogue scale.
How to cite this article: Liu FY, Gu ZF, Zhao ZQ, Ren L, Wang LM, Yu JH, Hou SB, Ding WY, Sun XZ. Modified grade 4 osteotomy for the correction of post-traumatic thoracolumbar kyphosis: a retrospective study of 42 patients. Medicine. 2020;99:37(e22204).
The authors report no conflicts of interest.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- [1].Vaccaro AR, Silber JS. Post-traumatic spinal deformity. Spine (Phila Pa 1976) 2001;26:111–8.. [DOI] [PubMed] [Google Scholar]
- [2].Jo DJ, Kim YS, Kim SM, et al. Clinical and radiological outcomes of modified posterior closing wedge osteotomy for the treatment of posttraumatic thoracolumbar kyphosis. J Neurosurg Spine 2015;23:510–7.. [DOI] [PubMed] [Google Scholar]
- [3].Munting E. Surgical treatment of post-traumatic kyphosis in the thoracolumbar spine: indications and technical aspects. Eur Spine J 2010;19:S69–73.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Diebo B, Liu S, Lafage V, et al. Osteotomies in the treatment of spinal deformities: indications, classification, and surgical planning. Eur J Orthop Surg Traumatol 2014;24: suppl 1: S11–20.. [DOI] [PubMed] [Google Scholar]
- [5].Hu W, Wang B, Run H, et al. Pedicle subtraction osteotomy and disc resection with cage placement in post-traumatic thoracolumbar kyphosis, a retrospective study. J Orthop Surg Res 2016;11:112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Suk SI, Kim JH, Lee SM, et al. Anterior-posterior surgery versus posterior closing wedge osteotomy in posttraumatic kyphosis with neurologic compromised osteoporotic fracture. Spine (Phila Pa 1976) 2003;28:2170–5.. [DOI] [PubMed] [Google Scholar]
- [7].Xi YM, Pan M, Wang ZJ, et al. Correction of post-traumatic thoracolumbar kyphosis using pedicle subtraction osteotomy. Eur J Orthop Surg Traumatol 2013;23: suppl 1: S59–66.. [DOI] [PubMed] [Google Scholar]
- [8].Chang KW, Cheng CW, Chen HC, et al. Closing-opening wedge osteotomy for the treatment of sagittal imbalance. Spine (Phila Pa 1976) 2008;33:1470–7.. [DOI] [PubMed] [Google Scholar]
- [9].Yang DL, Yang SD, Chen Q, et al. The treatment evaluation for osteoporotic Kummell disease by modified posterior vertebral column resection: minimum of one-year follow-up. Med Sci Monit 2017;23:606–12.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Kim KT, Lee SH, Suk KS, et al. Outcome of pedicle subtraction osteotomies for fixed sagittal imbalance of multiple etiologies: a retrospective review of 140 patients. Spine (Phila Pa 1976) 2012;37:1667–75.. [DOI] [PubMed] [Google Scholar]
- [11].Brantigan JW, Steffee AD, Geiger JM. A carbon fiber implant to aid interbody lumbar fusion. Mechanical testing. Spine (Phila Pa 1976) 1991;16: 6 suppl: S277–82.. [DOI] [PubMed] [Google Scholar]
- [12].Fogel GR, Toohey JS, Neidre A, et al. Fusion assessment of posterior lumbar interbody fusion using radiolucent cages: X-ray filmsand helical computed tomography scans compared with surgical exploration of fusion. Spine J 2008;8:570–7.. [DOI] [PubMed] [Google Scholar]
- [13].Takeuchi M, Wakao N, Kamiya M, et al. A compaction bone grafting technique leads to early bone fusion in cases of posterior lumbar interbody fusion. Oper Neurosurg (Hagerstown) 2016;12:31–8.. [DOI] [PubMed] [Google Scholar]
- [14].Han SH, Hyun SJ, Jahng TA, et al. A comparative radiographic analysis of fusion rate between L4-5 and L5-S1 in a single-level posterior lumbar interbody fusion. Korean J Spine 2015;12:60–7.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Min SH, Yoo JS. The clinical and radiological outcomes of multilevel minimally invasive transforaminal lumbar interbody fusion. Eur Spine J 2013;22:1164–72.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Takenaka S, Mukai Y, Hosono N, et al. Major surgical treatment of osteoporotic vertebral fractures in the elderly: a comparison of anterior spinal fusion, anterior-posterior combined surgery and posterior closing wedge osteotomy. Asian Spine J 2014;8:322–30.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Thomasen E. Vertebral osteotomy for correction of kyphosis in ankylosing spondylitis. Clin Orthop Relat Res 1985;194:142–52.. [PubMed] [Google Scholar]
- [18].Wu SS, Hwa SY, Lin LC, et al. Management of rigid post-traumatic kyphosis. Spine (Phila Pa 1976) 1996;21:2260–6.. [DOI] [PubMed] [Google Scholar]
- [19].Smith JS, Shaffrey E, Klineberg E, et al. Prospective multicenter assessment of risk factors for rod fracture following surgery for adultspinal deformity. J Neurosurg Spine 2014;21:994–1003.. [DOI] [PubMed] [Google Scholar]
- [20].Upadhyaya CD, Berven S, Mumaneni PV. Spondylolisthesis following a pedicle subtraction osteotomy. Case report. Neurosurg Focus 2010;28:E16. [DOI] [PubMed] [Google Scholar]
- [21].Oner FC, van der Rijt RR, Ramos LM, et al. Changes in the disc space after fractures of the thoracolumbar spine. J Bone Joint Surg Br 1998;80:833–9.. [DOI] [PubMed] [Google Scholar]
- [22].Gao R, Wu J, Yuan W, et al. Modified partial pedicle subtraction osteotomy for the correction of post-traumatic thoracolumbar kyphosis. Spine J 2015;15:2009–15.. [DOI] [PubMed] [Google Scholar]
- [23].Malham GM, Parker RM, Blecher CM, et al. Assessment and classification of subsidence after lateral interbody fusion using serial computed tomography. J Neurosurg Spine 2015;23:589–97.. [DOI] [PubMed] [Google Scholar]
- [24].Kaiser MG, Eck JC, Groff MW, et al. Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 1: Introduction and methodology. J Neurosurg Spine 2014;21:2–6.. [DOI] [PubMed] [Google Scholar]


