Supplemental Digital Content is available in the text.
Summary:
Although the great toe plays important roles in walking, loading, and maintaining balance when compared with other toes, there are few reports on great toe reconstruction, including the reconstruction of distal phalanx. This report aims to describe the use of a superficial circumflex iliac artery perforator (SCIP)–osteocutaneous flap for reconstructing a complex tissue defect of the great toe. A 62-year-old man presented with a crush injury to the forefoot. Because the great toe was severely crushed, the defect distal to the proximal phalanx of the great toe was reconstructed using a SCIP-osteocutaneous flap. The immediate postoperative course was uneventful; however, surgical revision was necessary. Signs of osseous union could be observed on radiographic images taken 2 months after the initial surgery. Twenty-four months after surgery, the patient could freely walk without resorption of the transferred bone. We demonstrated that SCIP-osteocutaneous flaps may be promising free flaps in complex tissue defect reconstruction of the great toe.
INTRODUCTION
The great toe plays an important role in intensive activities of daily living, including maintaining balance while standing, walking, and running,1 and significant dysfunction as a result of losing the great toe has been reported.2
Free iliac bone grafts, which have the disadvantage of being absorbed in the long term, have been used for the reconstruction of the distal phalanx of the great toe.3,4 A superficial circumflex iliac artery perforator (SCIP)–osteocutaneous flap is a versatile flap used for the reconstruction of the head and neck, as well as extremities, in which a well-vascularized iliac bone and relatively large soft tissue can be harvested from the same donor site.5–8 Herein, we present a case in which a SCIP-osteocutaneous flap was used to reconstruct the great toe.
CASE REPORT
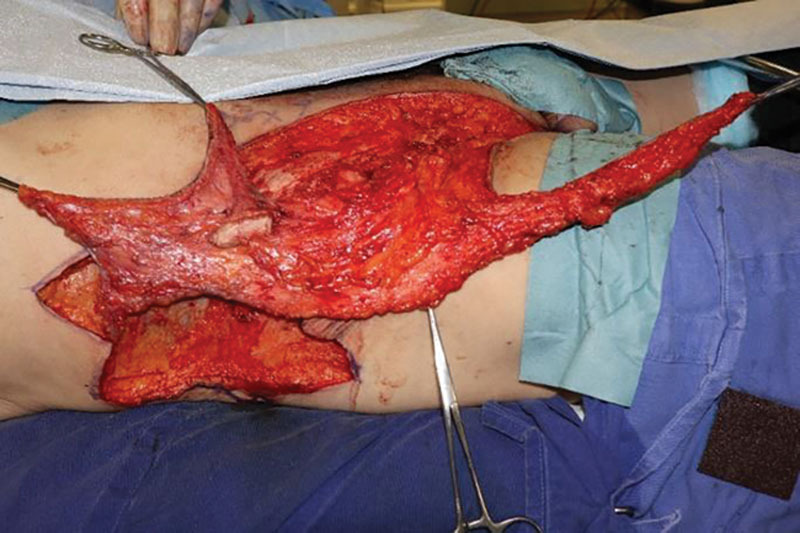
A 62-year-old man suffered a crush injury of the forefoot, caused by a 200-kg block that fell onto his right foot. The initial treatment was performed in the emergency department. As the great toe was severely crushed, the distal phalanx was removed and stump plasty was performed. Necrosis of the soft tissues of the great, second, and third toe and the dorsal foot progressed. Consequently, he was referred to our department, and a necrotic tissue debridement was performed (Fig. 1). The metatarsophalangeal (MTP) joint of the great toe was found to be intact.
Fig. 1.

A 62-year-old man who suffered a crush injury of the forefoot. Intraoperative appearance of the defect following removal of the necrotic tissue.
A SCIP-osteocutaneous flap, including a 32 × 9-cm2 skin paddle supplied by both the superficial and deep branches of the superficial circumflex iliac artery and a 2.5 × 1-cm2 iliac bone supplied by the deep branch of the superficial circumflex iliac artery, was elevated from the right iliac region (Fig. 2). The bone component was harvested along with the osseous branch running beside the iliac crest. The dorsalis pedis artery and the vena comitans were used as the recipient vessels.
Fig. 2.
SCIP-osteocutaneous flap composed of a 32 × 9-cm2 skin paddle perfused by the superficial branch of the superficial circumflex iliac artery (SCIA), the superficial circumflex iliac vein, and a 2.5 × 1-cm2 iliac bone (white arrowhead) perfused by the deep branch of the SCIA was elevated from the right iliac region.
The distal phalanx defect of the great toe was reconstructed using the vascularized iliac bone flap, and the soft-tissue defects of the great toe, second toe, and dorsal foot were filled with the skin paddle (See figure, Supplemental Digital Content 1, which displays (a) the vascularized iliac bone graft fixed to the proximal phalanx with Kirschner wires; (b) the skin paddle used for filling the defects in the forefoot, including the great and the second toes; (c) the appearance of the donor site; and (d) the assessment of the plantar foot pressure, http://links.lww.com/PRSGO/B457).
In the second stage, the connections between the flaps of the great toe and the second toe were separated, and the flap was fashioned according to the shape of the great toe. At the 24-month follow-up, the appearance of the great toe and the donor site was satisfactory (Fig. 3), and the x-ray image showed no bone resorption (Fig. 4 and See figure, Supplemental Digital Content 1, http://links.lww.com/PRSGO/B457). The patient could also walk wearing the commercially available shoes. (See Video 1 [online], which demonstrates the gait status of the patient 24 months postoperatively.) According to the plantar pressure measurements taken while walking, the patient was noted to bear the load of his weight sufficiently with the reconstructed toe. (See figure, Supplemental Digital Content 1, http://links.lww.com/PRSGO/B457).
Fig. 3.

Postoperative view of the forefoot 24 months after initial surgery.
Fig. 4.

X-ray image of the forefoot showing that bone union was achieved and that the bone flap was not resorbed.
Video 1. Video 1 from “Superficial Circumflex Iliac Perforator-Osteocutaneous Flap for Reconstruction of an Extensive Composite Defect in the Forefoot”.
DISCUSSION
The SCIP-osteocutaneous flap can be elevated as an osteocutaneous flap by including both a superficial branch (which mainly contributes to the blood flow of the skin paddle) and a deep branch (which nourishes both the iliac bone and the skin paddle). The versatility of this flap makes it suitable for head and neck as well as limb reconstruction.6–8
The indications for the reconstruction of the great toe must be carefully determined. Preoperative preservation of MTP joint function is required for successful ambulation, as in our case.
Reconstruction of the distal phalanx and the soft-tissue defects of the great toe is controversial. Toes are responsible for distributing the load of the body onto the metatarsal head during walking. In cases where the first MTP joint is preserved, reconstruction of the great toe may allow an enlargement of the weight-bearing area. Therefore, reconstruction of the distal phalanx reduces the burden on the metatarsal head by increasing the weight-bearing area. A potential drawback that occurs in a great toe with a fused interphalangeal (IP) joint is that it may interfere with walking without a functional MTP joint. Although the IP joint remains fused as in our case, further studies are needed to determine whether a single long phalanx without the IP joint is more beneficial than a shorter proximal phalanx with a functional MTP joint.
The iliac bone is used for reconstruction of defects in the distal phalanx.4 When used as a free bone graft, it has the disadvantage of being absorbed during the long postoperative course.3 Conversely, when used as a vascularized bone flap, there is no concern for absorption; however, raising the flap is more complicated.
The other commonly used options for vascularized bone flaps include the fibula, scapula, and iliac bone flaps established from the deep circumflex iliac artery. The donor-site morbidities of the fibula flap can be significant, including gait disturbance due to peroneal nerve injury or ischemia of the foot.9 Furthermore, this flap is unsuitable for treating small bone defects. The disadvantages of the iliac bone flaps include bulkiness, because of the size of the muscle involved, and uneven blood flow to the skin paddle due to loss of perforators arising from the deep circumflex iliac artery.10
The SCIP-osteocutaneous flap has various advantages. A relatively large skin paddle as large as 32 × 9 cm2 in our case can be included, and primary closure of the donor site can be achieved. Although smaller bone flaps can also be harvested, this flap is suitable for small- to moderate-sized bone defects such as a phalanx. This flap allows minimal donor-site morbidity without muscular dissection and can be constructed from an inconspicuous donor site. The drawback of this method is that it cannot be applied to large bone defects.
We herein report the successful reconstruction of a soft-tissue defect, including the great toe, using a SCIP-osteocutaneous flap. We believe that the SCIP-osteocutaneous flap is useful for the reconstruction of extensive soft-tissue defects with a small bone defect. The benefits of this flap are that it is not absorbed in the long term and that both the skin paddle and the bone graft can be harvested from the same donor site.
Supplementary Material
Footnotes
Published online 25 August 2020.
Disclosures: The authors have no financial interest to declare in relation to the content of this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Hughes J, Clark P, Klenerman L. The importance of the toes in walking. J Bone Joint Surg Br. 1990;72:245. [DOI] [PubMed] [Google Scholar]
- 2.Sosin M, Lin CH, Steinberg J, et al. Functional donor site morbidity after vascularized toe transfer procedures: a review of the literature and biomechanical consideration for surgical site selection. Ann Plast Surg. 2016;76:735–742 [DOI] [PubMed] [Google Scholar]
- 3.Kwon SH, Lao W, Yen CI, et al. Aesthetic multiple-toe reconstruction with combined iliac bone graft and wraparound free anterolateral thigh flap—a case report and literature review. Ann Plast Surg. 2017;78:3 suppl 2S37–S40 [DOI] [PubMed] [Google Scholar]
- 4.Yoshida A, Yajima H, Murata K, et al. Post-traumatic big toe reconstruction using free flaps. J Reconstr Microsurg. 2006;22:255–260 [DOI] [PubMed] [Google Scholar]
- 5.Taylor GI, Watson N. One-stage repair of compound leg defects with free, revascularized flaps of groin skin and iliac bone. Plast Reconstr Surg. 1978;61:494–506 [DOI] [PubMed] [Google Scholar]
- 6.Iida T, Narushima M, Yoshimatsu H, et al. A free vascularised iliac bone flap based on superficial circumflex iliac perforators for head and neck reconstruction. J Plast Reconstr Aesthet Surg. 2013;66:1596–1599 [DOI] [PubMed] [Google Scholar]
- 7.Yoshimatsu H, Iida T, Yamamoto T, et al. Superficial circumflex iliac artery-based iliac bone flap transfer for reconstruction of bony defects. J Reconstr Microsurg. 2018;34:719–728 [DOI] [PubMed] [Google Scholar]
- 8.Yoshimatsu H, Steinbacher J, Meng S, et al. Superficial circumflex iliac artery perforator flap: an anatomical study of the correlation of the superficial and the deep branches of the artery and evaluation of perfusion from the deep branch to the sartorius muscle and the iliac bone. Plast Reconstr Surg. 2019;143:589–602 [DOI] [PubMed] [Google Scholar]
- 9.Hartman EH, Spauwen PH, Jansen JA. Donor-site complications in vascularized bone flap surgery. J Invest Surg. 2002;15:185–197 [DOI] [PubMed] [Google Scholar]
- 10.Politi M, Toro C. Iliac flap versus fibula flap in mandibular reconstruction. J Craniofac Surg. 2012;23:774–779 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


