Background:
Revision facelift is a very challenging operation. The goal of our study was to examine the most common problems that the facelift surgeon has to face in a revision case and to suggest ways of solving them.
Methods:
A review of all patients from 2012 to 2017 in whom rhytidectomy was performed by the senior author was conducted.
Results:
During the 5-year study period, the author performed 552 face lifts. After the review to confirm revision procedures, a total of 72 revision facelifts were found. On reviewing the most common problems encountered in our facelifts, we found that in addition to the stigmata of the primary facelift, which are thoroughly analyzed in our article, a new type of stigmata has been added nowadays to the revision facelift—that of the various noninvasive interventions that patients undergo after their first facelift, in their effort to postpone or avoid a second operation. In all the abovementioned cases, the surgeon has to modify his basic surgical plan accordingly, to be able to improve or solve all of those problems during the revision surgery.
Conclusions:
The modern facelift surgeon often has to face much more than the stigmata of the primary facelift or the natural aging process. Thus, he/she should be appropriately trained to solve any problem we might encounter in a revision case.
INTRODUCTION
The efficacy and longevity of the principles of face and neck lifting techniques are well-established. Therefore, young plastic surgeons may choose a technique from a wide variety of proven methods to suit their aesthetics and individual abilities.
Methods based on Superficial Musculo Aponeurotic System (SMAS) and Platysma manipulation have been shown to ensure and prolong the longevity of the results,1–4 and most of the facelift techniques in the literature are modifications of these basic techniques. Therefore, we stand on the shoulders of giants, who have provided all the knowledge needed to produce consistently good or excellent facelift results. However, facelift surgeons often operate on patients who previously had poorly performed facelifts with undesirable results5–14 or on those who underwent multiple injectable therapies after the initial facelift, producing unnatural results, or on those who had noninvasive treatments with devices or threads in an effort to correct the recurrent laxity.15–17 All of the abovementioned procedures render the revision facelift more difficult.
A secondary facelift is a challenge on its own; even when the primary facelift was well-executed, the only issue requiring intervention is the natural aging process that occurs several years later. This is because there is always a variable amount of scar tissue, a thinned SMAS and platysma layer and a variability of skin incisions used in the primary procedure, and, of course, more medical problems because these patients are approximately a decade older.7, 18–30 At this point, it is interesting to state that Guyuron22 had observed in another study that secondary facelift patients tend to have a higher level of satisfaction when compared with the primary cases. Consequently, a facelift surgeon today has to face multiple challenges when performing a revision case, partly due to the primary operation and often because of the noninvasive treatments that the patient underwent after the primary procedure. A comprehensive review was performed on a large number of the author’s patients to examine the most common intraoperative problems the author faced during his revision cases, their causes, and the methods used to solve (or avert) them.
PATIENTS AND METHODS
A study of a retrospective series of cases in which rhytidectomy is performed by the author (G.S.) from 2012 to 2017 was conducted. Revision facelifts were defined as cases where both a preauricular and a postauricular cervicofacial flap was elevated a second time, and SMAS and platysma work was performed. All cases, including secondary and tertiary cases, were included; however, scar revisions were not considered revision rhytidectomies and were excluded. Those patients who had their primary procedure performed by another surgeon were not excluded. In secondary cases, 2 different categories were included: (1) secondary facelifts for the correction of problems resulting from the natural aging process. In this type of patients, no significant flaws were observed after the primary procedure, and the second intervention was usually required several years later; (2) secondary facelifts for the patients returning to the clinic a few months after the primary facelift due to neck or midface undercorrection during the primary procedure.
The aim of our study was to examine the author’s revision facelifts regarding the problems created by the primary procedure alone or by possible noninvasive interventions that followed the primary procedure. Patients who underwent only noninvasive therapies but no prior surgery, thus were operated on for the first time, were not included in our study. As we have already mentioned, in all of our cases, both a preauricular and a postauricular cervicofacial flap was elevated.
The basic surgical technique consisted of SMASectomy or SMAS plication as well as lateral platysmaplasty. In all patients with significant medial platysma bands or excessive skin laxity in the neck, the neck was opened as well, and a medial platysmaplasty was performed. This is the surgical technique followed by the author in primary cases as well. In revision cases, as will be discussed in the results section more thoroughly, the author modified several operative steps, according to the problems caused by the primary procedure or by the noninvasive therapies taken by the patient after the primary procedure. However, the vector of SMAS plication or SMASectomy does not change in the author’s revision cases. SMAS resection is always performed parallel to the nasolabial fold, and the vector of elevation is perpendicular to the nasolabial fold, as described by Daniel C. Baker.31 The author did not perform any subplatysmal modification to either primary or secondary cases, with the exception of conservative subplatysmal fat reduction, when indicated. In all cases, the critical tension sutures are 2: 1 in the temple area, at the lower border of the temporal hairline, and 1 in the upper border of the postauricular incision. Nylon 2-0 was used as the suture material.
Regarding the preauricular incision, in 65 of the 72 cases studied, the senior author used the preexisting incision, whether it was an intratragal or a pretragal. In 7 cases, he changed the pretragal to an intratragal judging that there was a similarity of color and texture between the skin of the tragus and the cheek skin.
RESULTS
During the 5-year study period, the author performed 552 facelifts. After review to confirm revision procedures, a total of 72 revision facelifts were found. Of these, 64 were women and 8 were men.
The average age of the patients included in our study varied. Twenty-seven patients of the 72 included in our study (categories 5, 6, and 7) underwent noninvasive treatments between the 2 procedures, in an effort to delay or avoid a secondary facelift. The average age of these patients at the time of the secondary procedure was 66 years old. The average age of the 45 remaining patients was 60 years.
Regarding the time between first and second rhytidectomy, the results were as follows: for the 27 patients of the categories 5, 6, and 7, the average time was 14 years, and for the remaining 45 patients, the time was 9 years (Table 1).
Table 1.
Characteristics of Patients
| Characteristics | Values |
|---|---|
| Patients who underwent noninvasive treatments between the 2 procedures | 27 |
| Age, y (range) | 66 (54–75) |
| Sex | |
| Male, n (%) | 2 (7%) |
| Female, n (%) | 25 (93%) |
| Time between first and second rhytidectomy, y (range) | 14 (5–26) |
| Patients who did not undergo any noninvasive treatment between the 2 procedures | 45 |
| Age, years(range) | 60 (50–74) |
| Sex | |
| Male, n (%) | 6 (13%) |
| Female, n (%) | 39 (87%) |
| Time between first and second rhytidectomy, y (range) | 9 (1–19) |
The author also revised 2 patients whose scar migration was observed in the postauricular area and around the lobule. In these 2 cases, he raised a small preauricular and postauricular flap to let it redrape and to be able to remove the scars and suture without tension. No deep tissue work was performed, and those cases were not included in our study.
After reviewing the problems most commonly encountered in the senior surgeon’s facelifts, we have categorized them as follows (Table 2):
Table 2.
Problems Most Commonly Encountered in Secondary Facelifts
| Problems | Value, n (%) |
|---|---|
| No stigmata from primary facelift | 15 (20%) |
| Neck/midface undercorrection during primary facelift | 10 (14%) |
| Temporal and/or occipital hairline distortion, poorly designed incisions | 48 (67%) |
| Pixie ear deformity | 10 (14%) |
| Cheek fat atrophy because of previous energy-based treatments | 2 (3%) |
| Significant scar tissue formation because of previous energy-based treatments or thread lifting | 20 (28%) |
| Large-volume injectables | 5 (7%) |
-
Secondary facelift with no significant deformities from the primary facelift but the natural aging process required intervention several years later (15 cases). Two of these cases had had the primary facelift performed by the author and underwent a secondary facelift 5 years later. These cases are usually more straightforward for the experienced facelift surgeons. However, there is usually a thinner SMAS layer and less skin to be excised.5,6 The skin flap is supposed to be more robust because of the delay phenomenon in secondary cases. However, this assumption should, in no case, justify more aggressive surgical manoeuvres because there is a variability of factors influencing the blood supply of the skin flap in each patient.
Surgical Program
In secondary cases with no deformities from the primary procedure, there are no significant modifications to the basic operative method. Of course, the incisions of the primary facelift are taken into consideration and are usually also used in the revision case, to avoid adding new scars to the patient’s face. As far as the underlying tissues are concerned, the thickness of the SMAS and platysma is always examined, and in cases where it has become really thin because of the prior facelift, plication is often performed instead of formal elevation of the platysma.
-
Secondary facelift performed a few months after the primary procedure due to neck or midface undercorrection (10 cases). Of these 10 cases, 2 patients decided to have the revision surgery 1 year after their first procedure, while the rest decided to wait for some years to be reoperated. One of these cases had the primary facelift performed by the author and complained about recurrent laxity 1 year later and so the author had to revise it. This is a separate group of patients in comparison to the first category because they are unhappy patients. They blame the primary procedure and not the aging process.
Surgical Program
In cases with neck undercorrection, the neck is usually opened during the secondary procedure and a medial platysmaplasty is performed along with a strong lateral pull. In all cases with midface undercorrection, we observed intraoperatively that the area of the skin undermining during the primary procedure (as shown by the extent of scar tissue during our secondary dissection) was minimal. Thus, by doing a much wider undermining during the secondary facelift, it was possible to lift the SMAS and correct the midface laxity and jowls. In those cases of laxity undercorrection during the primary surgery, the patient is advised to wait for at least 1 year in order for any residual swelling to resolve completely.
-
Temporal and/or occipital hairline distortion, poorly designed incisions (48 of our 72 revision cases).
Surgical Program
In cases with distortion of the temporal hairline, an anterior hairline incision (along the posterior border of the existing hairline) is always chosen, to not further distort the hairline. In these cases, it is very important to bevel the incision to maintain the hair follicles. By beveling, hair will grow postoperatively through the incision and diminish its visibility. In addition, beveling is mandatory to not further distort the temporal hairline. In cases of severe distortion of the temporal hairline, hair transplantation is recommended.
In cases with distortion of the occipital hairline, including significantly stair stepped occipital hairline, a wide undermining of the cervical flap is necessary, along with lateral platysmaplasty, to release all tension from the skin flap and allow the correct inset of the flap at the end of the procedure.
When the senior surgeon encounters bad scarring, he corrects the deformity, if possible. In his revision cases, he has mostly encountered 2 types:
(a) Widened scars due to prior pure skin lifts, with narrow undermining and no SMAS or platysma work in the primary procedure, thus widened scars because of skin closure under tension. This is corrected with excision of the scars, wide undermining of the skin flap, SMAS and platysma work, and closure under no tension.
(b) Double incision in the occipital or temporal area in tertiary cases. This phenomenon occurs when the surgeon performing the secondary facelift does not use the preexisting incisions of the first surgery and, therefore, the patient is left with scars from 2 surgeries.
When two incisional scars are encountered in the occipital region, the highest of the 2 is selected for incision placement, and the goal is to remove both preexisting ones at the end of the procedure. The accomplishment of this goal depends on the existing laxity.
When 2 incisional scars exist in the temporal region, usually the one is pre-hairline and the other inside the temporal hair. In these cases, the pre-hairline incision is selected to preserve the sideburn, beveling the incision, as we mentioned above.
-
“Pixie ear” deformity (10 cases).
Surgical Program
Pixie ear deformity is caused by excessive tension on the lobule, also associated with placing too much force on skin closure and not depending on SMAS-based techniques. This problem is solved by releasing the lobule, making a wide skin undermining and placing the tension on the SMAS and platysma.
-
Cheek fat atrophy because of previous energy-based treatments, performed after the primary facelift (2 cases).
Surgical Program
Fat atrophies due to previous energy-based treatments are corrected with fat grafting. However, these treatments compromise the microcirculation, and this can have a negative effect on fat survival. The patient should be informed about this fact preoperatively.
-
Significant scar tissue formation because of previous energy-based treatments or thread lifting (some years after the primary facelift, because of recurrent laxity) (20 cases). The term “significant” was determined clinically, by the dissection level of difficulty, which was much higher in all of these cases.
It is interesting to state that, in cases where the patient had had submental liposuction in combination with radiofrequency (RF) devices, the plane was very stiff and the dissection was much more difficult in comparison to patients who had had plain liposuction in their submental area in the past. And the submental area is a common area of focus for RF treatments. These treatments can compromise the microcirculation, and patients who have had treatments with energy-based devices are similar to smokers. Interestingly, these patients often have 4 or 5 such treatments and years of filler injections to their face. So, in these cases, we are dissecting through a lot of compromised areas. It is interesting to see that the scar in these cases often extends in the sub-SMAS plane as well, which becomes white and fibrous instead of diaphanous in a virgin patient. It is claimed that these treatments trigger collagen production. It is claimed that RF builds collagen. Scar tissue comprises collagen; so all these noninvasive treatments result in the formation of scar tissue subcutaneously. Threads, on the other hand, do not usually limit the ability to finish the flap release. The problem is you cannot always remove them. They can either be stuck to the skin or wrapped around vital structures.
Surgical Program
Significant scar tissue makes the dissection tedious and tricky. The surgeon can easily get too deep and injure a nerve branch or too superficial and harm the blood supply of the flap. The surgeon must be very careful and be patient during the dissection of the flap. When the scars are due to energy-based devices, the surgeon should keep in mind that these treatments result in skin and soft tissue ischemia, and the patients who have had them are somewhat similar to smokers. Therefore, he should be sure to keep a robust skin flap and sometimes even limit the skin undermining.
In some other revision cases, the scar tissue was produced by threads placed in the past. In general, the threads encountered during the dissection should be removed if possible; otherwise, the surgeon should just work around them. It is unnecessary to completely remove them for several reasons. First of all, they usually do not affect the aesthetic outcome of the operation. In addition, some of them are going to extrude later on when they break. Last but not least, they might be wrapped around a vital structure, such as the parotid duct, which can be injured by the surgeon’s effort to remove them.
It is of the essence to say that, in 10 of the patients in our study, there were symphyses between different anatomical planes of the face because of previous thread lifting. This manifested as abnormal dimpling during our SMAS or platysma plication intraoperatively, requiring excessive skin dissection to release the tethering.
-
Large-volume injectables (especially nonabsorbable). The senior surgeon performed a revision facelift on 5 patients who had distorted facial features because of large-volume injectables. He has performed a primary facelift on many more patients with distorted features due to injectable therapies, but only revision cases are included in this study, as we have already mentioned. In most of them, especially those with nonabsorbable injectables (silicone), the result of the facelift was not optimal.
Regarding the dissection, it was difficult in all cases, the plane having a gray translucent color.
In one of them, the surgeon had to stop the dissection in the cheek area about 2 cm in front of the tragus, upon reaching the nonabsorbable substance (silicone), because it felt like cutting on stone.
Of course, there were many more patients with minor problems due to previous injectable therapies, like granulomas, which caused less limitation to the procedure.
Surgical Program
Large-volume injectables should be dissolved a week or 2 before the surgery. However, this is not always possible because patients often do not know the kind of products that have been injected to their face.
In cases where the surgeon was operating on overfilled faces, the operative plan depended on the kind of injectable filler that had been used. When it was fat, liposuction was used in conjunction with the facelift. When it was hyaluronic, hyaluronidase was used 2–3 weeks before the procedure to dissolve it. When it was silicone, there was nothing to be done, and in some cases, this limited significantly the dissection intraoperatively. Despite his efforts, in the author’s experience, overfilled faces never go back to normal.
In patients with overfilled faces, the senior surgeon is always very careful in the preoperative consultation. It is important for them to understand the limitations of this surgery, as to the correction of their facial laxity. Almost all of these patients operated by the author were mostly concerned preoperatively by the laxity in the neck and that is what they wanted to correct using the surgery. So, the laxity in the neck is mostly addressed in this group of patients.
DISCUSSION
By reviewing the overall results of the patients included in our study, we can come to the following conclusions: patients undergoing a secondary or revision facelift, who have not undergone any type of noninvasive facial procedures, can usually obtain a good surgical result with a much rejuvenated face and neck. The recurrent laxity is corrected, and the deformities of the primary facelift are usually eliminated. Regarding these cases, the receding temporal hairline was the hardest to correct. As we have already mentioned, in these patients, it is very important to bevel the temporal hairline incision to maintain the hair follicles and not further distort the temporal hairline. Ten patients in our study had a receding temporal hairline, which was impossible for the senior author to correct.
On the other hand, noninvasive treatments can render a subsequent facelift much more difficult and even affect its outcome. Fat grafting in cases of fat atrophy caused by energy-based devices may fail because of fat reabsorption. Scar tissue produced by energy-based devices or threads may limit the flap release. Last but not least, as has been already mentioned, overfilled faces never go back to normal.
CASE REPORTS
Case 1
A 65-year-old female patient presented to the senior author’s office after 2 previous facelifts, a blepharoplasty and a rhinoplasty. She was bothered by the recurrent laxity of her face and neck, as well as the appearance of her nose.
Upon examining her face, she had a receding temporal hairline, distortion of the tragus, and occipital hairline distortion with 2 different incisional scars (due to poorly designed occipital incision during her secondary facelift).
Because of these side effects of the previous procedures, the operative plan was organized as follows:
Pre-hairline incision in the temporal area, to not further distort the temporal hairline
intertragal incision, as was performed in her 2 previous procedures.
The author selected the highest of the 2 occipital scars to place the postauricular incision to remove them both, judging that there was enough skin to allow that.
Intraoperatively, the author also encountered thinned SMAS and platysma layers; so he plicated them (did not do a SMASectomy or formal elevation of the lateral platysma border).
A revision rhinoplasty was also performed (Figs. 1–7).
Fig. 1.

Preoperative picture of a patient (case 1) who had undergone 2 previous facelifts: a blepharoplasty and a rhinoplasty. She presented to the senior author’s office, complaining about the recurrent laxity of her face and neck, as well as the appearance of her nose.
Fig. 7.

Postoperative picture of the same patient: oblique view.
Fig. 2.

Preoperative picture of the same patient: oblique view.
Fig. 3.

The patient had occipital hairline distortion with 2 different incisional scars.
Fig. 4.
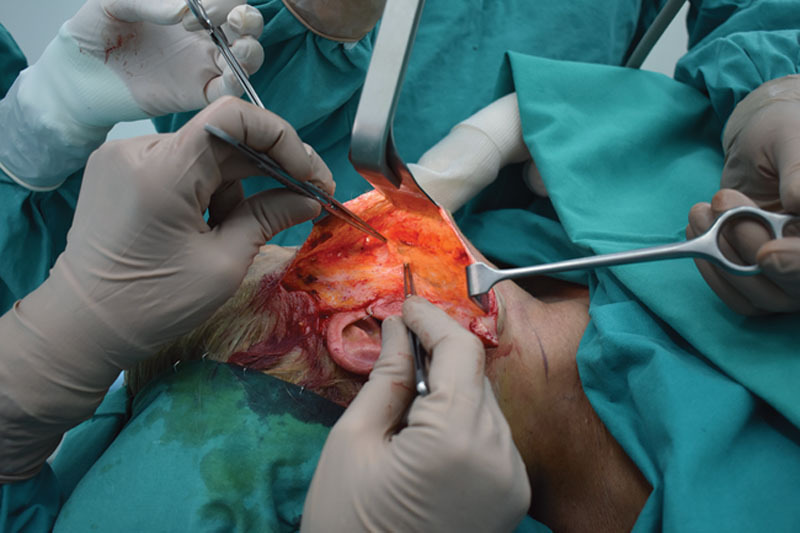
Intraoperatively, we encountered thinned SMAS and platysma layers, so we just plicated them.
Fig. 5.

Because of the stigmata of the previous procedures, the operative plan was organized as follows: (1) pre-hairline incision in the temporal area, to not further distort the temporal hairline; (2) intertragal incision, as was performed in her 2 previous procedures; (3) I selected the highest of the 2 occipital scars to place my postauricular incision to remove them both, judging that there was enough skin to allow that.
Fig. 6.

The same patient is shown 6 months postoperatively. She underwent a tertiary facelift and a revision rhinoplasty.
Case 2
A 63-year-old female patient presented to the senior author’s office after having multiple invasive and noninvasive treatments in her face. She had had a facelift 10 years ago and 5 years later, she felt like there was recurrent laxity in her face; so she visited a different doctor who advised her to do energy-based treatments (the patient said it was an ultrasound-based device). After a series of treatments, she developed fat atrophy in both of her cheeks.
Subsequently, she complained both about the fat atrophy in her cheeks and about the recurrent laxity in her face, jowls, and neck. The author conducted a face and neck lift and fat grafted her cheeks to improve the overall aesthetic image of her face (Figs. 8–13).
Fig. 8.

Preoperative picture of a patient (case 2) who had undergone a facelift 10 years ago. Five years after that, the patient had energy-based treatments to her face, which produced bilateral fat atrophy in her cheeks. She came to the senior author’s office, complaining both about the fat atrophy in her cheeks and about the recurrent laxity in her face, jowls, and neck.
Fig. 13.

Postoperative picture of the same patient: left lateral view.
Fig. 9.

Preoperative picture of the same patient: right lateral view.
Fig. 10.

Preoperative picture of the same patient: left lateral view.
Fig. 11.

Six-month postoperative picture of the same patient. Face and neck lifting was performed, as well as fat grafting to the cheeks.
Fig. 12.

Postoperative picture of the same patient: right lateral view.
Case 3
A 65-year-old female patient came to the author’s office to correct her face and neck laxity. She has had a facelift 12 years before and had bad scarring and a receding temporal hairline. Five years after her facelift, she had some permanent threads placed in her face due to recurrent laxity.
A revision facelift was performed. A pre-hairline incision was used in the temporal region. After wide undermining of the flap, it was possible to excise all the bad scarring around the ears. During flap release, the extent of the previous narrow skin undermining was obvious. This was partly the cause of bad scarring because it led to skin closure under tension.
We also removed as many of the threads as we could (Figs. 14–21).
Fig. 14.

Preoperative picture of a patient (case 3 ) who had a facelift 12 years ago and 5 years after, some permanent threads were placed into her face.
Fig. 21.

Postoperative picture of the same patient: oblique view.
Fig. 15.

Preoperative picture of the same patient: oblique view.
Fig. 16.

The patient had bad scarring and a receding temporal hairline.
Fig. 17.

The extent of the previous narrow undermining during the primary facelift has been outlined. This contributed to tension closure and scars. Also a nonabsorbable thread is revealed, which is stuck into the SMAS.
Fig. 18.
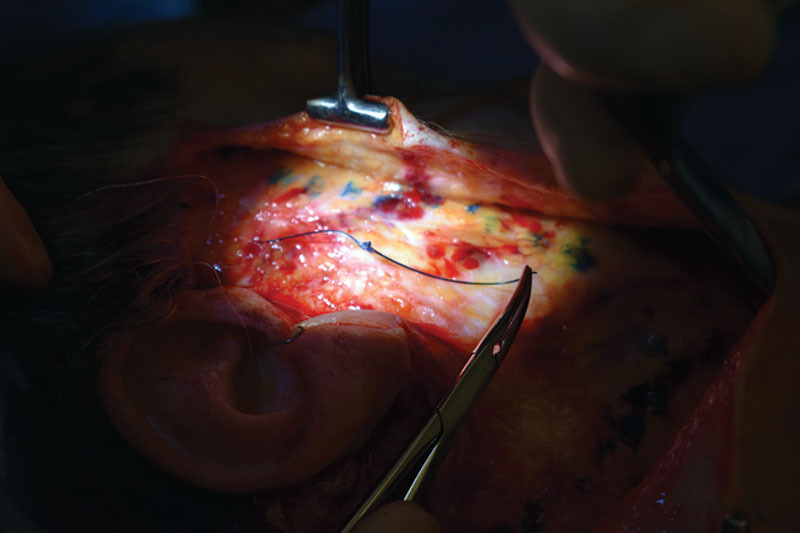
The thread is carefully removed without injuring the surrounding tissues.
Fig. 19.

Total amount of threads removed.
Fig. 20.

One-year postoperative picture of the patient. She had a facelift and a browlift.
CONCLUSIONS
Revision facelift has nowadays become an even more demanding operation. A facelift surgeon today often encounters much more than the side effects of the primary facelift or the natural aging process. The popularity of multiple noninvasive therapies, which are constantly increasing in number, has led many patients, who have already undergone a facelift in the past, to seek nonsurgical options to treat their recurrent laxity in the face and neck. The fillers and Botox, as well as other noninvasive treatments, are indeed very good in prolonging the results of a facelift. However, the fact that they are often used in a wrong or abusive way leads to scar formation, granulomas, or even distortion of facial features. A thorough preoperative examination is always warranted in all of the abovementioned cases to determine the problems caused by any previous procedure—surgical or nonsurgical.
Those problems must be pointed out to the patient preoperatively, along with the limitations and potential risks of the upcoming surgery. It is interesting that a big number of patients come for a consultation regarding the recurrent laxity, not having observed the receding hairline or misplaced incisions. Analyzing these problems becomes even more important, taking into account that many of the patients have the tendency of observing their face in detail much more after the surgery than before. Thus, the surgeon could falsely be accused of causing a deformity that already existed. Good communication between surgeon and patient, as well as setting realistic expectations regarding the result, will be the cornerstone of an outcome, which will satisfy both the patient and the surgeon.
It is essential to say that as surgeons, we have the opportunity to observe with our own eyes all the effects that each noninvasive treatment has on our patients’ skin and underlying tissues. This is an advantage that other nonsurgical specialties, performing noninvasive therapies as well, do not have. We should use this advantage to the patients’ benefit, selecting those therapies that are safe and have consistent, reproducible results; of course, we should be appropriately trained to solve any problem we might encounter in a revision case.
PATIENT CONSENT
Patients provided written consent for the use of their images.
Footnotes
Published online 20 August 2020.
Presented at the Live Makeover 5 Aesthetic Surgery Symposium, August 31 and September 1 and 2, 2018, Athens, Greece, and at the Live Makeover 6 Aesthetic Surgery Symposium, June 21–23, 2019, Athens, Greece.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
REFERENCES
- 1.Chang S, Pusic A, Rohrich RJ. A systematic review of comparison of efficacy and complication rates among face-lift techniques. Plast Reconstr Surg. 2011;127:423. [DOI] [PubMed] [Google Scholar]
- 2.Connell BF. Pushing the clock back 15 to 20 years with facial rejuvenation. Clin Plast Surg. 2008;35:553–566 [DOI] [PubMed] [Google Scholar]
- 3.Guyuron B. An evidence-based approach to face lift. Plast Reconstr Surg. 2010;126:2230–2233 [DOI] [PubMed] [Google Scholar]
- 4.Owsley JQ., Jr SMAS-platysma face lift. Plast Reconstr Surg. 1983;71:573–576 [DOI] [PubMed] [Google Scholar]
- 5.Beale EW, Rasko Y, Rohrich RJ. A 20-year experience with secondary rhytidectomy: a review of technique, longevity and outcomes. Plast Reconstr Surg. 2013;131:625–634 [DOI] [PubMed] [Google Scholar]
- 6.Rasko YM, Beale E, Rohrich RJ. Secondary rhytidectomy: comprehensive review and current concepts. Plast Reconstr Surg. 2012;130:1370–1378. [DOI] [PubMed] [Google Scholar]
- 7.Hatef DA, Sclafani AP. Secondary rhytidectomy. Semin Plast Surg. 2009;23:257–263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Miller TR, Eisbach KJ. SMAS facelift techniques to minimize stigmata of surgery. Facial Plast Surg Clin North Am. 2005;13:421–431 [DOI] [PubMed] [Google Scholar]
- 9.Moyer JS, Baker SR. Complications of rhytidectomy. Facial Plast Surg Clin North Am. 2005;13:469–478 [DOI] [PubMed] [Google Scholar]
- 10.Niamtu J., III Complications in facelift surgery and their prevention. Oral Maxillofac Surg Clin North Am. 2009;21:59–80, vi [DOI] [PubMed] [Google Scholar]
- 11.Owsley JQ. Face lifting: problems, solutions, and an outcome study. Plast Reconstr Surg. 2000;105:302–313; discussion 314–315 [DOI] [PubMed] [Google Scholar]
- 12.Thompson DP, Ashley FL. Face-lift complications: a study of 922 cases performed in a 6-year period. Plast Reconstr Surg. 1978;61:40–49 [DOI] [PubMed] [Google Scholar]
- 13.Man D. Reducing the incidence of ear deformity in facelift. Aesthet Surg J 2009;29:264–271 [DOI] [PubMed] [Google Scholar]
- 14.Mowlavi A, Meldrum DG, Wilhelmi BJ, et al. The “pixie” ear deformity following face lift surgery revisited. Plast Reconstr Surg. 2005;115:1165–1171 [DOI] [PubMed] [Google Scholar]
- 15.Sarigul Guduk S, Karaca N. Safety and complications of absorbable threads made of poly-L-lactic acid and poly lactide/glycolide: experience with 148 consecutive patients. J Cosmetic Dermatol. 2018;17:1189–1193 [DOI] [PubMed] [Google Scholar]
- 16.Gülbitti HA, Colebunders B, Pirayesh A, et al. Thread-lift sutures: still in the lift? A systematic review of the literature. Plast Reconstr Surg. 2018;141:341e–347e [DOI] [PubMed] [Google Scholar]
- 17.Kasai H, Yashiro K, Kawahara Y. Multiple ulcers on the face due to infection after thread-lifting. J Dermatol. 2018;45:e336–e337 [DOI] [PubMed] [Google Scholar]
- 18.Bernard RW, Aston SJ, Casson PR, et al. Secondary face lift. Aesthet Surg J 2002;22:277–283 [DOI] [PubMed] [Google Scholar]
- 19.de Castro CC, Braga L. Secondary rhytidoplasty. Ann Plast Surg. 1992;29:128–135 [DOI] [PubMed] [Google Scholar]
- 20.Funk E, Adamson PA. A comparison of primary and secondary rhytidectomy results. Aesthetic Plast Surg. 2011;35:96–99 [DOI] [PubMed] [Google Scholar]
- 21.Guyuron B. Secondary rhytidectomy. Plast Reconstr Surg. 2004;114:797–800 [DOI] [PubMed] [Google Scholar]
- 22.Guyuron B, Bokhari F, Thomas T. Secondary rhytidectomy. Plast Reconstr Surg. 1997;100:1281–1284 [DOI] [PubMed] [Google Scholar]
- 23.Haiavy J. Reoperative face and neck lifts. Oral Maxillofac Surg Clin North Am. 2011;23:109–118, vi [DOI] [PubMed] [Google Scholar]
- 24.Hamra ST. Prevention and correction of the “face-lifted” appearance. Facial Plast Surg. 2000;16:215–229 [DOI] [PubMed] [Google Scholar]
- 25.Hamra ST. Correcting the unfavorable outcomes following face lift surgery. Clin Plast Surg. 2001;28:621–638 [PubMed] [Google Scholar]
- 26.Hamra ST. Frequent face lift sequelae: hollow eyes and the lateral sweep: cause and repair. PlastReconstrSurg. 1998;102:1658–1666 [DOI] [PubMed] [Google Scholar]
- 27.Matarasso A, Wallach SG, Difrancesco L, et al. Age-based comparisons of patients undergoing secondary rhytidectomy. Aesthet Surg J 2002;22:526–530 [DOI] [PubMed] [Google Scholar]
- 28.Morales P. Repeating rhytidoplasty with SMAS, malar fat pad, and labiomandibular fold treatment: the NO primary procedure. Aesthetic Plast Surg. 2000;24:364–374 [DOI] [PubMed] [Google Scholar]
- 29.Sundine MJ, Kretsis V, Connell BF. Longevity of SMAS facial rejuvenation and support. Plast Reconstr Surg. 2010;126:229–237 [DOI] [PubMed] [Google Scholar]
- 30.Ramirez OM, Pozner JN. Subperiosteal endoscopic techniques in secondary rhytidectomy. Aesthet Surg J 1997;17:22–26 [DOI] [PubMed] [Google Scholar]
- 31.Baker DC. Lateral SMASectomy, plication and short scar facelifts: indications and techniques. Clin Plast Surg. 2009;35:533–550 [DOI] [PubMed] [Google Scholar]


