Abstract
PURPOSE
We aimed to explore the imaging findings of computed tomography (CT) in diagnosing coronavirus disease 2019 (COVID-19) and its clinical value for further evaluation of suspected cases.
METHODS
Files of 155 patients visiting the fever clinics at our hospital and affiliated hospitals from January 20th to February 9th, 2020 were searched. Among them, 140 cases (including 82 males and 58 females) were included as suspected COVID-19 cases based on clinical and epidemiological history; the CT image features of 70 cases with suggestive findings on CT, confirmed by positive nucleic acid test were analyzed and evaluated. The sensitivity and specificity of CT in diagnosing COVID-19 were evaluated in patients with epidemiological history.
RESULTS
Of the 70 patients, 84.3% showed bilateral lung involvement on CT; 27 cases (38.6%) showed ground-glass opacity (GGO), which was mostly distributed in the subpleural area (55.7%), and this sign was mainly observed in early COVID-19 patients. In addition, 41 cases (58.6%) manifested GGO combined with focal consolidation opacity, 2 (2.8%) had flake-like consolidation opacity, with involvements of the periphery of lung field and the central zone (44.3%), and this sign was mostly observed in severe or critical patients. Concomitant signs such as pleural effusion and mediastinal lymph node enlargement were rare. Among patients with epidemiological history, the sensitivity of CT in diagnosing COVID-19 was 89.7% (70/78), and the specificity was 88.7% (55/62).
CONCLUSION
CT shows high sensitivity and specificity in diagnosing COVID-19. CT is an important examination method in evaluation of suspected cases and assessment of disease severity.
In December 2019, coronavirus disease 2019 (COVID-19) pneumonia occurred in Wuhan of China, and the virus spread quickly. By January 2020, the epidemic had spread to the whole nation and multiple countries and areas in the world. According to the 2019 Novel Coronavirus Pneumonia Diagnosis and Treatment Scheme (6th edition) released by the National Health Commission (1), the diagnostic criteria should be determined based on epidemiology, clinical manifestations, computed tomography (CT) findings, and COVID-19 nucleic acid test. Nucleic acid test has been considered as the gold standard for confirming COVID-19, which is in line with the latest opinion published by the American College of Radiology (ACR) (2). Throat swab is adopted as the routine specimen collection mode at present, which has false negatives to some extent (3); as a result, COVID-19 should be confirmed through repeated detection, and this process is time-consuming. Chest CT examination has the features of convenience, efficiency, and being able to intuitively display the lesion, which can make up for the lack of nucleic acid testing effectively, but the value of CT for early diagnosis of suspected patients is unclear. Therefore, this paper aimed to summarize and explore the CT findings of COVID-19, as well as the application value of CT in the early diagnosis of suspected cases, so as to achieve early segregation and treatment for COVID-19.
Methods
This investigation was a retrospective study and was approved by our institutional review board (protocol number: 2020-013). The informed consent requirement was waived.
Patients
A total of 155 patients visiting the fever clinics at our hospital and affiliated hospitals from January 20th to February 9th, 2020 were screened. Among the 155 patients, 92 cases showed positive sign on CT examination and were suspected with COVID-19; finally, 70 of them were confirmed using the nucleic acid test (Fig. 1). The patient inclusion criteria were as follows: contact history with the epidemic area or COVID-19 patients; chest CT examination before treatment; presence of COVID-19 nucleic acid detection results; no other infectious disease; no artifact in CT images; and satisfying the observation conditions.
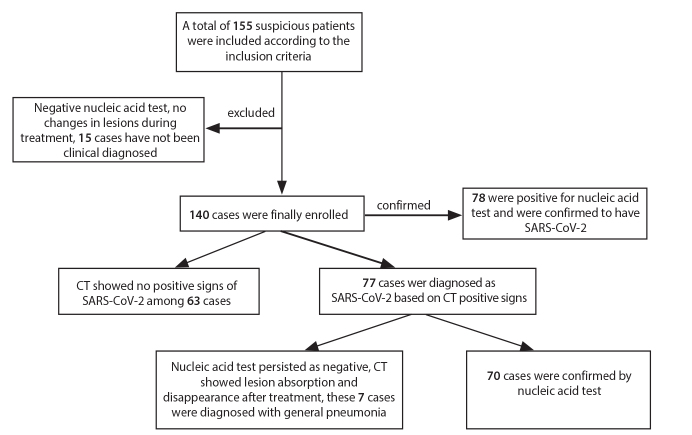
Figure 1.
Flowchart of nucleic acid detection and CT diagnosis in 155 patients.
Finally, 140 cases were included in this study, including 82 males and 58 females, with the age of onset of 19–79 years, and the median age of 49 years. Of 140 cases, 8 were diagnosed as positive by nucleic acid test, but CT showed no positive signs; 7 were diagnosed as negative by first-time nucleic acid test, but had positive signs on CT, and repeat nucleic acid tests confirmed COVID-19.
CT examination
Chest CT examinations were performed using the Siemens 64 slice and Philips 128 slice spiral CT scanners. CT examination was performed with all patients wearing surgical masks, in head-first supine position, under breath-hold. The scanned area was from the superior aperture of thorax to the base of the lung. The scanning parameters were as follows: tube voltage 120 kV, automatic tube current, layer thickness 2 mm, interlamellar spacing 1 mm, matrix 512×512.
For the examination of patients with COVID-19, the Radiology department has set a dedicated CT scan machine and opened a dedicated examination access. All patients were required to wear medical protective masks during examinations, and technicians adopted second-level protection (disposable working caps, protective glasses, medical protective masks, protective clothing, disposable latex gloves, disposable shoe covers and strict hand hygiene). Positioning technicians worked in the contaminated area and could not enter the clean area before changing jobs in a specified time. To prevent cross-infection, the equipment and surfaces were disinfected after every examination. We used 75% ethanol to wipe and disinfect the CT scanner. The floor of the scan room was disinfected with 2000 mg/L chlorine. When there were visible contaminants, disposable absorbent materials were used to completely remove stains before disinfecting. The air disinfection machine was used for continuous disinfection in the equipment room. In addition, the air disinfection used ultraviolet radiation under unmanned state, which needed to be continuously irradiated for more than 30 minutes, followed by opening the window to ventilate for at least another 30 minutes.
Image analysis
The images were analyzed and evaluated by two senior physicians in the cardio-thoracic section at the radiology department, and any disagreement was settled through mutual negotiation. The following CT findings were recorded for each patient: scope of lesion involvement (unilateral or bilateral lungs); lesion distribution (peripheral zone, central zone or both); lesion number (single, double, or multiple lesions); lesion density (ground-glass density, consolidation density or mixed density); other thoracic signs (mediastinal and lung hilar lymph node enlargement, pleural thickening and pleural effusion).
The sensitivity and specificity of CT in diagnosing COVID-19 were calculated.
Results
Patients were clinically categorized into light, normal, heavy, and critical condition according to the 2019 Novel Coronavirus Pneumonia Diagnosis and Treatment Scheme (6th edition) released by the National Health Commission. Among the 78 cases confirmed as COVID-19 by nucleic acid testing, 8 were categorized as light, 36 as normal, 23 as heavy, and 11 as critical. Except for 3 patients who were identified as close contacts of confirmed cases and had no obvious clinical symptoms at the time of isolation and screening, the other 75 patients had different clinical symptoms at the time of consultation (Table 1). At the time of writing, 35 of the 78 COVID-19 patients had been cured, 40 were still under observation and treatment in the hospital, and 3 died (Table 2).
Table 1.
Clinical characteristics of COVID-19 patients (n=77)
| Disease condition | Number of cases | Clinical manifestation | Laboratory inspection | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fever | Cough | Sore throat | Fatigue | Diarrhea | Difficulty breathing | White blood cell count | Lymphocyte ratio | |||||
| Reduced | Normal | High | Reduced | Normal | ||||||||
| Light | 8 | 5 | 4 | 2 | 2 | 0 | 0 | 2 | 6 | 0 | 6 | 2 |
| Normal | 36 | 32 | 28 | 19 | 32 | 9 | 0 | 10 | 26 | 0 | 20 | 16 |
| Heavy | 23 | 23 | 23 | 11 | 16 | 0 | 3 | 18 | 5 | 0 | 19 | 4 |
| Critical | 11 | 11 | 11 | 0 | 11 | 3 | 11 | 6 | 0 | 5 | 11 | 0 |
COVID-19, coronavirus disease 2019.
Table 2.
Diagnostic findings and outcome according to the condition of COVID-19 patients (n=77)
| Disease condition | Number of cases | First PCR test | CT findings | PCR test after CT | Outcome | |||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||||
| Positive | Negative | Positive | Negative | Positive | Negative | Cured | Hospitalized | Death | ||
| Light | 8 | 8 | 0 | 0 | 8 | 8 | 0 | 7 | 1 | 0 |
|
| ||||||||||
| Normal | 36 | 29 | 7 | 36 | 0 | 36 | 0 | 22 | 14 | 0 |
|
| ||||||||||
| Heavy | 23 | 23 | 0 | 23 | 0 | 23 | 0 | 6 | 17 | 0 |
|
| ||||||||||
| Critical | 11 | 11 | 0 | 11 | 0 | 11 | 0 | 0 | 8 | 3 |
COVID-19, coronavirus disease 2019; PCR, polymerase chain reaction; CT, computed tomography.
Seventy patients suspected with COVID-19 upon CT and finally confirmed through nucleic acid test were analyzed. The detailed CT findings are displayed in Table 3.
Table 3.
CT findings of COVID-19 patients confirmed by nucleic acid test (n=70)
| Imaging features | n (%) |
|---|---|
| Lung involvement | |
| Unilateral | 11 (15.7) |
| Bilateral | 59 (84.3) |
|
| |
| Distribution | |
| Peripheral | 39 (55.7) |
| Peripheral and central | 31 (44.3) |
|
| |
| Number | |
| Single lesion | 14 (20.0) |
| Two lesions | 9 (12.9) |
|
| |
| Multiple lesions | 47 (67.1) |
|
| |
| Density | |
| Ground glass density | 27 (38.6) |
| Consolidation density | 2 (2.8) |
| Mixed density | 41 (58.6) |
|
| |
| Other signs | |
| Pleural thickening | 12 (17.1) |
| Pleural effusion | 4 (5.7) |
| Mediastinal lymph node enlargement | 2 (2.8) |
CT, computed tomography; COVID-19, coronavirus disease 2019.
According to the Imaging Diagnosis Guidelines for Novel Coronavirus Pneumonia (1st edition in 2020) released by the Infectious Disease Section of Radiology Society of Chinese Medical Association, COVID-19 can be divided into early, progressive, critical and termination stages based on the onset and course of disease. There are overlaps in the imaging findings between different stages. Early CT findings include multiple flake-like ground-glass opacities in bilateral lungs, accompanying with or without local consolidation opacity, which is mainly distributed along the bronchovascular bundle and subpleural area, and the thickened blood vessel opacity or bronchus meteorology (Fig. 2). At progressive stage, the lesion manifests with enlarged lesion scope and co-existence of multiple properties; meanwhile, ground-glass opacity, consolidation, nodule and strip opacities are also observed, which are mainly distributed in central and peripheral lung zones, subpleural area and base of lung, and fibrosis may also be seen (Figs. 3, 4). At critical stage, the lesion can progress into bilateral diffuse consolidation, and flake-like ground-glass opacity can be seen in non-consolidation area. In 4 of our cases, the majority of the lungs were involved bilaterally, and the “white lung” manifestation (Fig. 5) was observed, while pleural effusion (5.7%) and mediastinal lymph node enlargement (2.8%) were rare.
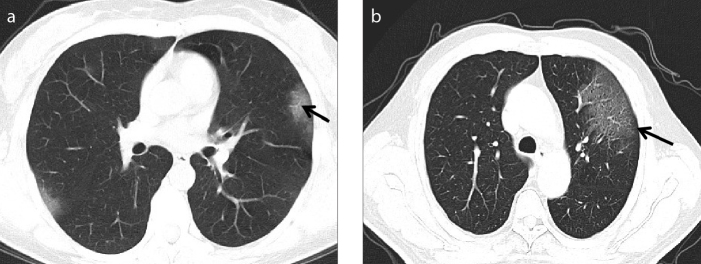
Figure 2. a, b.
Early stage CT findings of COVID-19. Axial CT image (a) of a 46-year-old female presenting with fever for 3 days. Flake-like ground-glass opacities are observed in the subpleural areas of upper lobes of bilateral lungs, in which thickened small vessels (black arrows) are seen. Axial CT image (b) of a 34-year-old male presenting with fever and cough for 6 days. A large sheet-like ground-glass opacity is seen in the upper lobe of left lung, in which the grid opacities are observed with the slabstone sign (black arrows).
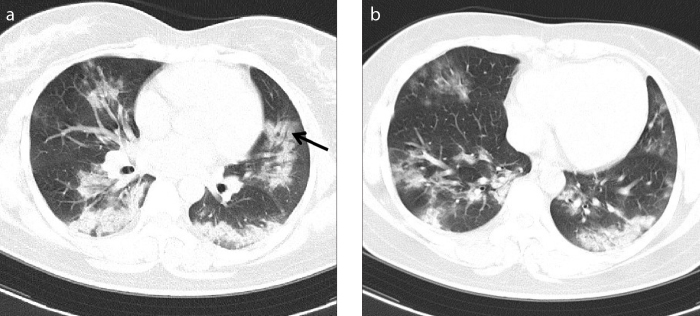
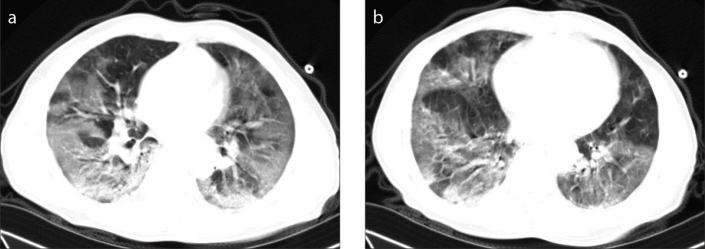
Figure 3. a, b.
Progressive stage CT findings of COVID-19. Axial CT images (a, b) of a 28-year-old female presenting with fever and cough for 7 days. Multiple flake-like ground-glass opacities and consolidation opacity are observed in bilateral lungs, most remarkably in the lower lobes; bronchial meteorology (black arrow) is seen in local lesion.
Figure 4. a, b.
Progressive stage CT findings of COVID-19. Axial CT images (a, b) of a 52-year-old male presenting with fever for 5 days and diarrhea. Multiple sheet-like ground-glass opacities are observed in both lungs, which are more obvious in the right lung.
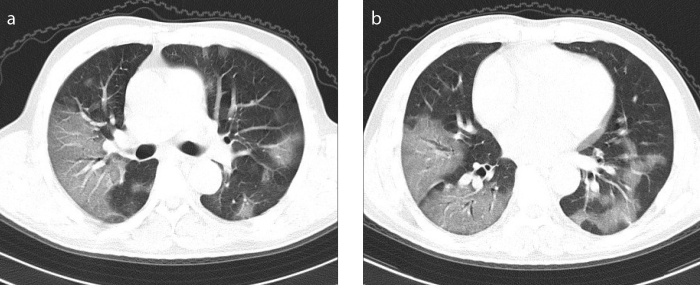
Figure 5. a, b.
Critical stage CT findings of COVID-19. Axial CT images (a, b) of a 69-year-old male presenting with fever and dry cough for 6 days. Multiple diffuse ground-glass opacities and consolidation opacity are observed in both lungs, which show “white lung” sign.
Among the 140 patients included in this study, 77 were initially diagnosed with COVID-19 based on CT, and 70 of them were confirmed with COVID-19 through nucleic acid test, while the remaining 7 cases had lesion disappearance after treatment and were discharged after recovery. The nucleic acid tests for these 7 patients remained negative during this process, and they were clinically diagnosed with common pneumonia (Fig. 6). Consequently, the positive and negative predictive values of CT in diagnosing COVID-19 were 90.9% (70/77) and 87.3 (55/63), the sensitivity and specificity of CT in diagnosing COVID-19 were 89.7% (70/78) and 88.7% (55/62), respectively, in patients with epidemiological history during the epidemic period (Table 4).
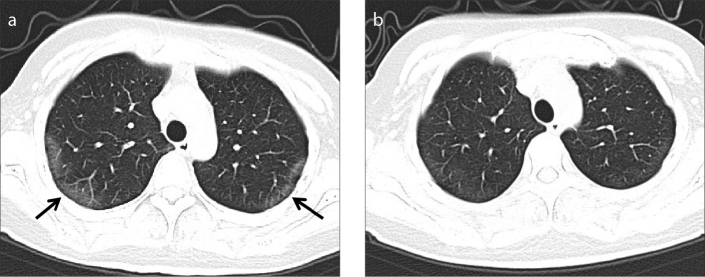
Figure 6. a, b.
CT findings of common pneumonia. Axial CT image (a) of a 34-year-old female presenting with fever and cough for 4 days. Strip-like ground-glass opacities are observed in the subpleural areas of the upper lobes of bilateral lungs (black arrows), and thickened small vessels are observed inside. Axial CT image (b) from re-examination after 5 days of treatment. The lesion in subpleural areas of the upper lobes of bilateral lungs are obviously absorbed. The patient was clinically diagnosed with common pneumonia.
Table 4.
Sensitivity and specificity of CT in diagnosing COVID-19 (n=140)
| Diagnosis based on nucleic acid test | Total | |||
|---|---|---|---|---|
|
| ||||
| Positive | Negative | |||
| Possible diagnosis based on CT | Positive | 70 | 7 | 77 |
| Negative | 8 | 55 | 63 | |
|
| ||||
| Total | 78 | 62 | 140 | |
CT, computed tomography; COVID-19, coronavirus disease 2019.
Discussion
The novel coronavirus belongs to the β-genus coronavirus, which is shown in current research to share over 85% homology with the severe acute respiratory syndrome (SARS) coronavirus carried by bats. At present, the source of infection is mainly the COVID-19 patient, and respiratory tract droplet transmission is the major route of transmission, with general susceptibility. COVID-19 exhibits an extremely potent transmission capacity, and cases are reported in all countries around the world (4, 5). Early discovery, early diagnosis and early segregation are important means to suppress the spread of epidemic; in this regard, chest CT is a convenient and simple method that displays the lesion features intuitively, making it a vital examination tool.
The imaging findings of COVID-19 are similar to those of SARS and Middle East respiratory syndrome (MERS) induced by other coronaviruses. The lesion is dominated by pulmonary interstitial inflammation (6–8), with the major manifestations of flake-like or nodule-like ground-glass opacities and local consolidation opacity in the lung. The main CT finding of the 70 COVID-19 patients included in this study was involvement of bilateral lungs (84.3%); 27 cases (38.6%) showed ground-glass opacities mostly distributed in the subpleural area (55.7%), with thickening lung vessel opacity or “slabstone” sign seen inside. This sign was mainly seen in early COVID-19 patients or those with mild symptoms. Currently, the pathogenesis of COVID-19 remains unclear. Based on analysis of SARS coronavirus with 85% homology, the virus is colonized in alveolus and respiratory bronchial epithelium (9) at the early stage, which results in alveolar wall swelling, serous inflammatory exudation in the alveolus, thus manifesting as ground-glass opacity on imaging, and the “slabstone” sign is seen at the time of alveolar interstitial inflammatory thickening. In this study, 41 cases (58.6%) showed ground-glass opacities combined with local consolidation opacity, while 2 cases (2.8%) exhibited flake-like consolidation opacity, which was mainly seen in severe or critical patients. Upon analysis, these different imaging findings may be related to the fact that disease aggravation can lead to acute diffuse lung injury to various degrees (10) and the inflammatory exudation increases in the alveolus, which results in the co-existence of ground-glass opacity, consolidation and strip opacities on CT images. In addition, signs such as pleural effusion and mediastinal lymph node enlargement are rare, which are only seen in critical elderly patients, and this may be related to underlying comorbidities usually present in the elderly patients.
Routine use of CT in this pandemic is still controversial due to difficulties in its disinfection process. In order to prevent cross-infection during the epidemic, protection measures must be strictly implemented in the hospital. The radiology department should establish an independent medical imaging examination area or special radiological examination equipment, and clearly define the contaminated area, semi-contaminated area and clean area according to the requirements of nosocomial infection control, and each area should be strictly disinfected. During examination, following points should be minded: 1) Patients should wear a medical protective mask throughout the examination; 2) The positioning technician should strictly implement second-level protection, instruct the patient to lie on the examination bed and operate the rack to complete the positioning work; 3) CT technician should operate the machine to complete the examination and then perform rapid hand disinfection after the examination is completed before opening the shielding door; 4) and the medical personnel who escort the patient should return the patient back to the ward or clinic according to the designated route; 5) After the examination is completed, the machine, the ground and the air should be disinfected. The escort of patients should be coordinated with the Infection Department, Radiology Department, medical services and wards to establish a path for sending and returning COVID-19 confirmed patients. Before the examination starts, there should be no unnecessary person around the designated CT and the transportation path in cooperation with the hospital security and logistics staff, and the transportation personnel should use 75% alcohol or 1000 mg/L chlorine disinfectant spray as necessary. Under these strict protective measures, no cross-infection caused by CT examination was found in this study during the epidemic.
Additionally, there are some circumstances in which CT use is not suitable: patients who cannot strictly implement hospital protective measures, patients who are restless, patients with critical illnesses such as major bleeding, and pregnant women.
In this study, 8 patients were diagnosed positive by nucleic acid tests, but no positive signs were found on chest CT. These patients had mild clinical symptoms such as low fever, cough or fatigue. According to the sixth COVID-19 diagnosis and treatment guidance, these patients are clinically classified as mild cases. Therefore, CT has no positive signs in patients with mild clinical symptoms and positive nucleic acid test for COVID-19, so CT scan may not be performed at an early stage. CT scan can be used to detect the progress of the disease, which is consistent with the views of ACR and Fleischner Society (2, 11).
Initial nucleic acid tests were negative for 7 patients, but chest CT showed positive signs, and COVID-19 was confirmed on subsequent nucleic acid tests. Four of these patients had clinical symptoms such as fever and respiratory symptoms, while the other three had no obvious clinical symptoms, but chest CT showed a patchy ground glass density lesion under pleura, suggesting that such patients can be easily missed. Therefore, for patients with high suspicion of epidemiological contact history but negative nucleic acid test, chest CT scan can further assist diagnosis, effectively isolate the infected person at an early stage, and control the spread of the epidemic. Sverzellati et al. (12) and other recent studies pointed out that during the pandemic, CT scan can be used for classifying patients with symptoms of respiratory tract infection into non-COVID-19 infection, suspected COVID-19 and confirmed COVID-19, which has important significance in the outpatient and emergency settings, alleviating the stress of isolation treatment for COVID-19 patients in the hospital. This is similar to our research.
According to our results, the sensitivity and specificity of CT in diagnosing COVID-19 were 89.7% and 88.7%, respectively, among patients with epidemiological history, which is of vital clinical application value.
There are some limitations to this study. The sample size included in the study is limited, and can be expanded in a later stage. This study summarizes the clinical features and the main CT imaging findings of COVID-19 patients at the initial diagnosis, and does not summarize the follow-up images after treatment.
In conclusion, the CT findings of COVID-19 are specific, and CT represents an important examination method to aid diagnosis in the presence of COVID-19 suspicion and assess the severity of disease. Detailed knowledge on CT features of COVID-19 contributes to early diagnosis, segregation, and treatment of patients, as well as limiting the spread of COVID-19.
Main points.
COVID-19 pneumonia shows typical signs on CT, and CT has high sensitivity and specificity in diagnosis.
In the severe situation of epidemic, CT can effectively make up for the problem of insufficient nucleic acid detection ability.
Strict implementation of protective measures can effectively prevent cross-infection during the process of CT examination.
Footnotes
Conflict of interest disclosure
The authors declared no conflicts of interest.
References
- 1.National Health Commission. [Accessed: Feb 19, 2020];Novel Coronavirus Pneumonia Diagnosis and Treatment Scheme (trial, 6th edition) Available at: http://www.nhc.gov.cn/yzygj/s7653p/202002/8334a8326dd94d329df351d7da8aefc2.shtml. [Google Scholar]
- 2.American College of Radiology (ACR) ACR Recommendations for the use of chest radiography and computed tomography (CT) for suspected COVID-19 Infection. Mar 11, 2020. [Accessed Mar 13, 2020]. Available at: www.acr.org/Advocacy-and-Economics/ACR-Position-Statements/Recommendations-for-Chest-Radiography-and-CT-for-SuspectedCOVID19-Infection.
- 3.Xie X, Zhong Z, Zhao W, et al. Chest CT for typical COVID-19 pneumonia: relationship to negative RT-PCR. Radiology. 2020 Feb 12;:200343. doi: 10.1148/radiol.2020200343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Phan LT, Nguyen TV, Luong QC, et al. Importation and human-to-human transmission of a novel coronavirus in Vietnam. N Engl J. 2020;382:872–874. doi: 10.1056/NEJMc2001272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Holshue ML, DeBolt C, Lindquist S, et al. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382:929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Das KM, Lee EY, Langer RD, et al. Middle east respiratory syndrome coronavirus: What does a radiologist need to know? AJR Am J Roentgenol. 2016;206:1193–1201. doi: 10.2214/AJR.15.15363. [DOI] [PubMed] [Google Scholar]
- 7.Choi WJ, Lee KN, Kang EJ, et al. Middle east respiratory syndrome-coronavirus infection: A case report of serial computed tomographic findings in a young male patient. Korean J Radiol. 2016;17:166–170. doi: 10.3348/kjr.2016.17.1.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xuezhe Zhang, Wu Wang, Yan Lu, et al. CT study on the chest manifestations and complications of SARS. Chinese J Radiol. 2003;37:775–779. [Google Scholar]
- 9.Koo HJ, Lim S, Choe J, et al. Radiographic and CT features of viral pneumonia. Radiographics. 2018;38:719–739. doi: 10.1148/rg.2018170048. [DOI] [PubMed] [Google Scholar]
- 10.Pan Y, Guan H, Zhou S, et al. Initial CT findings and temporal changes in patients with the novel coronavirus pneumonia (COVID-19): a study of 63 patients in Wuhan, China. Eur Radiol. 2020. Feb 13, [DOI] [PMC free article] [PubMed]
- 11.Rubin GD, Ryerson CJ, Haramati LB, et al. The role of chest imaging in patient management during the COVID-19 pandemic: a multinational consensus statement from the Fleischner Society. Radiology. 2020 Apr 7; doi: 10.1148/radiol.2020201365. 201365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sverzellati N, Milanese G, Milone F, et al. Integrated radiologic algorithm for COVID-19 pandemic. J Thorac Imaging. 2020. Apr 7, [DOI] [PMC free article] [PubMed]