Abstract
COVID-19 was first reported in Wuhan, China, in December 2019; it rapidly spread around the world and was declared a global pandemic by the World Health Organization in March 2020. The palliative care program at the Princess Margaret Cancer Centre, Toronto, Canada, provides comprehensive care to patients with advanced cancer and their families, through services including an acute palliative care unit, an inpatient consultation service, and an ambulatory palliative care clinic. In the face of a global pandemic, palliative care teams are uniquely placed to support patients with cancer who also have COVID-19. This may include managing severe symptoms such as dyspnea and agitation, as well as guiding advance care planning and goals of care conversations. In tandem, there is a need for palliative care teams to continue to provide care to patients with advanced cancer who are COVID-negative but who are at higher risk of infection and adverse outcomes related to COVID-19. This paper highlights the unique challenges faced by a palliative care team in terms of scaling up services in response to a global pandemic while simultaneously providing ongoing support to their patients with advanced cancer at a tertiary cancer center.
Keywords: COVID-19, Palliative care, Pandemic, Cancer, Supportive care
Background
COVID-19, caused by the novel coronavirus SARS-CoV2, was first reported in Wuhan, China, in December 2019 [1]. It has spread rapidly and was declared a global pandemic by the World Health Organization on March 11, 2020 [2]. High-risk patients, including those with advanced cancer, can experience severe symptoms including pneumonia, severe acute respiratory syndrome, and renal failure [1, 3]. Mortality rates among patients with advanced cancer have been estimated to be up to three times higher than among the general population [4].
Several papers have described potential challenges to cancer care in the context of COVID-19. These have focused primarily on decision-making around the initiation or continuation of anticancer therapies; delays in cancer surgery; enrollment in clinical trials; and the importance of clearly documented goals of care discussions for patients with cancer who may become infected with COVID-19 [5, 6]. The literature around palliative care provision in response to COVID-19 has mainly focused on managing resource limitations, educational initiatives for non-specialists, and ensuring that the psychosocial needs of patients, families, and healthcare providers are attended to [7–10]; there has been scant information around the provision of palliative care to patients with cancer during the COVID-19 pandemic.
This paper will outline the key operational and practical challenges faced by a palliative care team at a tertiary cancer center during the COVID-19 pandemic and how the team adapted to best manage their routine practice as well as the care of patients with advanced cancer and COVID-19.
General considerations
The Princess Margaret Cancer Centre (PM) is a tertiary cancer center in Toronto, Canada; it provides care to over 12,000 new patients with cancer per year and has 120 inpatient beds. PM forms part of the University Health Network (UHN), which also includes two acute care hospitals (Toronto General Hospital and Toronto Western Hospital); specialized palliative care is available at each of these sites. The oncology palliative care service at PM provides care across three areas: a 12-bed acute palliative care unit (PCU), an inpatient consultation service, and an ambulatory palliative care clinic. The palliative care team is well integrated across all aspects of the cancer center, through its clinical work, education programs, and research promoting the early integration of palliative care for patients with advanced cancer and their families [11].
Following the declaration of COVID-19 as a global pandemic, the cancer executive committee at PM developed a clinical response to each of three proposed phases (Table 1). During phase 1, the priority was to maintain a COVID-19-free cancer center for as long as possible. Patients with cancer and suspected COVID-19 were diverted to designated acute care inpatient units at Toronto General Hospital; in exchange, COVID-19-negative cancer patients admitted at Toronto General Hospital were transferred to PM for ongoing management. During phase 2, Priority A patients (defined as those with COVID-19 for whom active treatment could not be delayed or deferred) were admitted to a cohorted COVID-19-positive unit at the cancer center. A second unit was designated for patients under investigation (PUI) for COVID-19, who were subsequently transferred to COVID-positive or COVID-negative units, respectively, depending on their test results. Additional overflow units were identified to accommodate greater numbers of inpatients (both COVID-19-positive and COVID-19-negative). For phase 3, the use of unconventional space was proposed. Although to date phase 3 has not been activated, all inpatient spaces that had previously been converted for use for office space at UHN were reconfigured for inpatient use.
Table 1.
Phases of pandemic planning with associated PCU admission criteria
| Pandemic phase | Phase 1 | Phase 2 | Phase 3 |
|---|---|---|---|
| Description | COVID-free cancer center | Priority A cancer patients with COVID-19 cohorted on designated units; patients under investigation cohorted on a separate unit | COVID-19-positive patients throughout the cancer center |
| PCU admission criteria |
-No CPR -Patients agree to complete papers to transition to a longer-term PCU if unable to go home (3 choices) -Prioritize admissions from acute hospitals |
-No CPR -Patients agree to complete papers to transition to a longer-term PCU if unable to go home (1 choice) |
-No CPR -No need to complete papers to transition to a longer-term PCU -Consider admitting patients with non-malignant disease or bed-spacing patients with active goals of care including CPR |
Screening booths were set up at all entry points to the cancer center for staff, patients, and visitors. Patients screening positive (presenting with symptoms of cough, runny nose, sore throat, shortness of breath, fever, or travel within the previous 14 days) were diverted to a specially designated assessment area and tested for COVID-19 if clinically indicated. Staff were instructed to self-monitor for symptoms suspicious for COVID-19 and to self-isolate and present for testing if symptomatic. Test centers were set up adjacent to each hospital site, to fast track testing for symptomatic staff. Clinical staff were provided with two procedure masks per shift as well as a face shield and were instructed to wear these at all times while providing patient care. N95 respirators were available when engaged in aerosol-generating procedures.
Restrictions around visitors were initiated, with a strict no visitor policy across all inpatient areas. Pre-identified exceptions included patients who were actively dying; those who required a family member to provide care (based on cultural or religious practices); and those lacking capacity to make decisions relating to their care and for whom a virtual consultation with their substitute decision maker was not feasible.
Ambulatory palliative care clinics
PM has a large ambulatory palliative care clinic with approximately 1500 new patient visits and 4000 total visits annually. All nine of our MDs have an ambulatory practice, supported by 3.5 FTE dedicated oncology palliative care nurses and a patient flow coordinator; a social worker, spiritual care provider, and occupational therapist are shared with the inpatient service [12]. Typically, new patients attending our clinic spend the first 20–30 minutes of their consultation with a palliative care nurse, who introduces the role of palliative care, takes a detailed personal and medication history, and reviews patient-reported outcome measures (the Edmonton Symptom Assessment System (ESAS) [13] and patient-reported functional status [14]. They also discuss relevant community services, such as nursing, personal support workers, and other allied health professional supports, making referrals as appropriate. Patients are also provided with a binder of resources and contact information for the team between visits, including after-hours support [12].
Prior to COVID-19, almost all clinic visits were in-person. We were in the process of developing broad criteria to facilitate the introduction of telehealth visits, as well as installing the necessary equipment (monitors with webcameras, keyboards, and microphones) into the clinic, and training staff around the consent process and use of telehealth services, using the Ontario Telehealth Network (OTN) [15]. These efforts were accelerated in response to the pandemic. On March 16, we began to see our first patients using telehealth. In accordance with directives from the PM executive, we developed a plan to reduce our in-person visits by 25% on week 1, 50% on week 2, and 75% on week 3, exceeding these targets by week 2. By April 6, we were seeing approximately 90% of patients via telehealth, and our long-term plans are to continue to see up to 30% of patients via telehealth.
Ambulatory patients were triaged based on provincial guidelines and categorized into three groups: Priority A patients were defined as those with urgent or life-threatening symptoms (ESAS scores of > 7 for pain, nausea, and/or shortness of breath) requiring timely review and for whom in-person review may be required; Priority B patients as having non-critical needs but symptoms of moderate intensity (ESAS scores of 4–7 for pain, nausea, and shortness of breath or > 7 for other symptoms) for whom review was desirable and could be managed with telehealth; and Priority C patients as those with stable symptoms (typically < 4 on ESAS) under routine follow-up for whom a rescheduled or delayed visit was unlikely to change clinical outcomes [16](Table 2). Rescheduled visits were tracked using the cancer center’s newly developed virtual care monitoring system, which offered a standardized approach to determine how (in-person or virtual visits over the phone or video conference via OTN) and when patients were reviewed, as well as communication between physicians, their administrative assistants, and patient flow coordinators in clinics (responsible for scheduling follow-up appointments).
Table 2.
Pandemic plan for managing outpatients with cancer
| Priority level and definition | Examples |
|---|---|
| A: Patients who require urgent assessment and treatment due to an unstable clinical presentation, life-threatening symptoms, or significant distress related to physical or psychological symptoms |
-Patients with select ESAS scores ≥ 7 (pain, nausea, or shortness of breath) -Patients on or requiring continuous ambulatory delivery device pumps, methadone, or other interventions requiring specialist palliative care assessment or intervention -Patients exhibiting signs and symptoms of possible opioid toxicity -Patients with symptoms suggestive of an oncologic or non-oncologic emergency (e.g., spinal cord compression, bowel obstruction, SVC obstruction, pulmonary embolus) |
| B: Patients with non-critical needs |
-Patients with ESAS scores ≥ 7 not included under Priority A -Patients with select ESAS scores ≥ 4 but < 7 (pain, nausea, shortness of breath) -Patients requiring assessment or management of ascites or pleural effusions, where an intervention (e.g., point-of-care ultrasound) may be provided in clinic |
| C: Patients for whom services can be delayed without an anticipated change in clinical outcomes |
-Ambulatory patients who are stable seen in ongoing follow up (ESAS scores < 4) -Early palliative care referrals, including study patients |
Where possible, all patients were preferentially offered OTN or telephone visits. In-person visits were offered with suspected emergent symptoms potentially requiring further investigation or admission, e.g., spinal cord compression or bowel obstruction, or a severe pain crisis not manageable via telehealth or other virtual supports (Table 2). Patients were encouraged to continue to call our nursing line (for concerns during regular working hours) or the after-hours on-call team in the event of developing new or worsening symptomatology. We continued to triage and review new patient referrals, again via OTN, whenever possible. Written or verbal consent was obtained to communicate with patients via email or OTN.
With a move to telehealth visits, our clinical nurse specialists continued their role over the phone and emailed the relevant information to the appropriate attending physician as part of a detailed handover template. Physicians, working on site or remotely, followed up with each patient to develop a tailored plan to manage their symptoms, conduct advance care planning and goals of care discussions, provide ongoing emotional support, make referrals to other services as needed, and arrange follow-up at an appropriate time interval. With the patient’s consent, contact information and symptom management materials were emailed or mailed.
The rapid transition from in-person to telehealth visits has proven to be both feasible and successful at PM and will likely continue to be an acceptable option for select patient groups beyond the pandemic. Although there are important limitations to consider around the use of telehealth (in terms of the lack of a truly comprehensive multidisciplinary consultation and the inability to perform a physical examination, as well as technical and privacy issues), access to telehealth has allowed us to continue to support our community-based patients where in-person contact is not advisable. Although there is limited published data around the use of telehealth in palliative care to date [17], it has been shown to improve access to palliative care services (especially for patients living in remote areas); enhance communication between patients, families, and practitioners; and increase patient and family satisfaction, largely due to its convenience [18]. Further research around the use of telehealth by palliative care teams is needed, with a focus on both patient and provider perspectives.
Acute palliative care unit
Our inpatient service provides care on a dedicated, 12-bed (ten private rooms and one semi-private room) acute palliative care unit (PCU) as well as a consultation service for patients admitted to the oncology units at PM. Usually, attending physicians rotate on a monthly basis between the acute PCU and the consult service. For the duration of the pandemic, the inpatient teams were split into two distinct teams (one covering the PCU and one the consult service, each with four physicians) to minimize the risk of infection and exposure among the entire team. Physicians were assigned to cover either service on a weekly rotational basis, with back-up physicians available in the event of increased workload, illness, or exposure. There was broad acceptance at UHN that the role of palliative care teams would be a vital component of the response to COVID-19. Through the UHN redeployment program, volunteer family physicians were identified who could work alongside palliative care physicians to support the inpatient palliative care teams in the event of illness, exposure, or overwhelming numbers of patient referrals.
The PCU typically admits patients with acute symptom needs for a brief period of assessment and management. Admission criteria include acceptance of a no cardiopulmonary resuscitation (no CPR) order and a willingness to consider transfer to a longer-term PCU (and to complete applications to three such units) if unable to transfer home once the acute symptom issues have been resolved [19]. The average length of stay is typically 10–14 days [20]. Daily rounds are interdisciplinary, attended by nursing staff (three to four per shift), two staff physicians, a clinical nurse specialist, occupational and physiotherapists, social worker, music and art therapy, as well as learners (medical students, residents, and fellows). In order to maintain staff health and safety, social distancing measures were introduced for daily rounds. Team members phoned into rounds whenever possible, and nurses provided handover one-by-one instead of collectively.
Our PCU was designated as COVID-19-free. Our priority was to facilitate timely admissions from other hospitals or from the community and if possible to reduce the numbers of patients attending the emergency department. COVID-negative cancer patients with palliative care needs at our acute hospitals (Toronto General Hospital and Toronto Western Hospital) were preferentially transferred to the PM PCU to facilitate care of COVID-19-positive patients at these acute care hospitals. Stable inpatients in the PCU were transferred home or to longer-term PCUs when feasible to facilitate expedited admissions. Community patients continued to have access to the PCU as needed; these patients all underwent screening prior to and immediately upon admission. Where there was a concern about a potential diagnosis of COVID-19, patients were admitted temporarily to the PUI unit, while COVID testing was completed. Depending on test results, patients were moved to the PCU once a negative result was confirmed, or to a COVID-19 positive unit, where their needs were managed by our inpatient consultation team (see below).
Acknowledging that symptoms of COVID-19 may present at any point over the course of an admission, a low threshold was adopted to retest patients who developed any new or concerning symptoms for COVID-19. Private rooms were utilized preferentially, and patients were discouraged from leaving their room during their admission, except to undergo tests or procedures; when outside of their room, patients were provided with procedure masks. Patients who tested positive for COVID-19 while on the PCU (one to date) were transferred to a designated unit at Toronto General Hospital for ongoing care. Team members exposed to a COVID-19-positive patient were supported by occupational health, and appropriate contact tracing measures were undertaken to ensure all potentially exposed individuals (staff, patients, and visitors) were informed and supported. No patients or staff exposed to COVID-19 subsequently tested positive.
Our admission criteria were revised to accommodate the rapid transfer of patients (Table 1). Our unit was provided with an iPad to help patients to stay connected with family and friends and to facilitate family meetings; our music therapist offered virtual song writing sessions for interested patients. A major barrier to admissions was the restriction around visitor numbers and visiting hours at PM, with many patients opting to stay at home rather than be separated from loved ones. For patients on the PCU requiring support from a family member, one designated and pre-screened visitor per day for up to 2 h was permitted at the discretion of the unit manager. These hours were increased up to eight hours, including overnight, for patients considered to be in their last days or hours.
There is scant literature on changes in practice of hospices and PCUs during the COVID-19 pandemic. One other paper described approaches to admission criteria, in particular creating COVID-positive and COVID-negative hospices [21]. This paper and one other described changes to visitor policies and the challenges of balancing safety with compassion and grief, especially at the end-of-life [21, 22]. The first paper described how a daily phone call from the unit psychologist provided updates and psychological support to families unable to visit in-person [21]. The other paper described how additional challenges, including the suspension of volunteer services, can lead to even greater isolation for inpatients [22]. The use of technology to allow patients and team members to connect with each other and with families warrants further exploration in the palliative care literature.
Inpatient consultation service
The PM inpatient consultation service provides support to patients admitted to the malignant hematology and medical and radiation oncology units, with physicians working alongside two clinical nurse specialists. Referrals are made to the consultation team by hospitalists who are responsible for the daily care of inpatients on the oncology wards. These consults are usually for complex symptom management, goals of care conversations, and support around discharge planning with community palliative care supports.
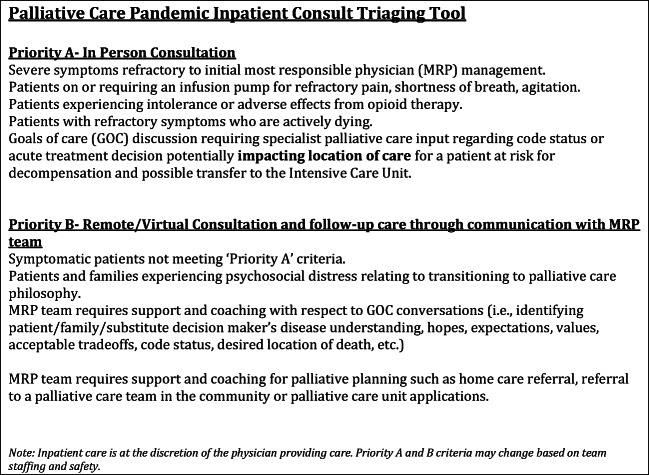
Daily team rounds were conducted via teleconference rather than in-person to maintain appropriate social distancing. A triage tool was developed along with the hospitalist team to identify those patients who might be managed with virtual support from the palliative care team and those who would continue to require face-to-face support (Fig. 1). One physician was assigned as the primary contact for the COVID-19 cohorted units and the PUI unit at the cancer center, rotating on a weekly basis, providing virtual and in-person supports as needed to the patients and teams covering these units, with back-up from a second physician as needed. In the event of large numbers of patients with COVID-19 requiring specialist palliative and end-of-life care on these units, we developed a plan to assume most responsible physician status for these patients rather than as consultants. Arrangements were made with each consulting unit to provide the palliative care team with the necessary PPE to review patients safely.
Fig. 1.
Inpatient consultation triage tool
PM does not have an intensive care unit (ICU); instead patients are transferred via a bridge to an ICU at an adjacent hospital. Provincial guidelines were disseminated and adopted outlining a triage process for accessing ICU beds and ventilators during the anticipated surge period of the pandemic; patients with advanced cancer and poor prognosis were identified as being unsuitable for ICU admission in these instances [23]. Detailed plans including order sets for end-of-life symptom management and continuous palliative sedation therapy for use by non-specialist physicians were developed to support patients from the cancer center and their families in the event of transfer out of the ICU (or lack of suitability for ICU admission) for end-of-life care. Conversation guides were developed to support goals of care discussions around the allocation of ICU beds based on best practice guidelines such as the VitalTalk program [24].
For patients on the inpatient consult service, minimizing team exposure to COVID-19 while maintaining a responsive and available service was the priority. There is very little literature around the specific role of palliative care consultation services during a pandemic [7]. It has been suggested that referral criteria should be reviewed in the context of COVID-19, especially for COVID-negative patients, and responsibilities shared with allied health professionals such as social workers (for assistance with disposition planning) or spiritual care for emotional support were possible [9]. Similar to our experiences, other centers have adopted segregated team models to minimize exposure [25] and developed local clinical guidelines to support non-specialist teams in the management of COVID-related symptoms such as dyspnea, delirium, and respiratory secretions [8] and engaged in educational opportunities across the cancer center to promote and highlight these guidelines.
Research and education
Research and education are at the cornerstone of activities at PM, which is affiliated with the University of Toronto. In response to the pandemic, non-essential research was immediately suspended at the PM as it was at other cancer centers [26]. Recruitment of new patients to any existing interventional studies was stopped, and follow-up visits with previously enrolled patients were conducted remotely or deferred where possible, with appropriate amendments to the research protocol as needed. Non-interventional research, including chart reviews and systematic or literature reviews, was continued at the discretion of the principal investigator. Research personnel were redeployed to work at screening centers or to assist with administrative data or non-patient facing research work including manuscript and report writing.
Palliative care educational endeavors prioritized the development and dissemination of resources for non-specialist teams around symptom management and communication skills. Videos, slide decks, and order sets were developed by the UHN palliative care team to assist frontline staff in the management of severe dyspnea and other symptoms at the end-of-life [27]. Palliative care residents and fellows helped with the development of these educational resources and became skilled in the use of telehealth. Learners were assigned to work either in the inpatient or outpatient setting, rather than rotating between settings, and teaching sessions continued either one-on-one with attending physicians or virtually, to ensure the educational experience of learners was not negatively impacted by the pandemic.
There was a focus on wellness and self-care for both trainees and staff, with support from our Department of Psychosocial Oncology. Trainees were excused from clinical duties to attend weekly wellness sessions, and an array of supports were developed for and shared among all team members including connected social distancing strategies; virtual yoga, and mindfulness sessions, as well as recommendations around diversions such as arts and culture apps.
Conclusions
Providing palliative care in oncology settings during the COVID-19 pandemic requires consideration regarding not only to how to respond to the pandemic itself but also how to continue to support patients with advanced cancer at risk of developing COVID-19. Maintaining existing services across both inpatient and outpatient settings, while simultaneously planning for a potential surge of highly symptomatic patients with complex end-of-life care needs, poses challenges in terms of resources, education, and service provision.
The vital role played by palliative care teams during the COVID-19 pandemic is clear, both in caring for patients with COVID-19 and in continuing to provide seamless oncology palliative care. Pandemic planning documents and guidelines developed for COVID-19 will be useful for future pandemics or natural disasters; sharing these between centers internationally may help to build collaborations. Further research around the use of telehealth by palliative care teams, both inpatient and outpatient, is required.
Acknowledgments
The authors would like to acknowledge the support and dedication of our clinical nurse specialists and advance practice nurses throughout the pandemic, both in the provision of direct patient care in-person and via telemedicine and in the development of guidelines and educational materials around the management of key symptoms related to COVID-19.
Authors’ contributions
All authors contributed to the study conception and design. Material preparation was performed by Breffni Hannon. The first draft of the manuscript was written by Breffni Hannon, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Code availability
Not applicable.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Guan W, Ni Z, Hu Y, Liang W, Ou C, He J, Liu L, Shan H, Lei CL, Hui DSC, du B, Li LJ, Zeng G, Yuen KY, Chen RC, Tang CL, Wang T, Chen PY, Xiang J, Li SY, Wang JL, Liang ZJ, Peng YX, Wei L, Liu Y, Hu YH, Peng P, Wang JM, Liu JY, Chen Z, Li G, Zheng ZJ, Qiu SQ, Luo J, Ye CJ, Zhu SY, Zhong NS, China Medical Treatment Expert Group for Covid-19 Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organisation. Coronavirus disease (COVID-19) pandemic [Internet]. 2020 [cited 2020 Apr 25]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019
- 3.Sidaway P (2020) COVID-19 and cancer: what we know so far. Nat Rev Clin Oncol. 0980:41571. Available from: http://www.ncbi.nlm.nih.gov/pubmed/32265531 [DOI] [PMC free article] [PubMed]
- 4.Liang W, Guan W, Chen R, Wang W, Li J, Xu K, Li C, Ai Q, Lu W, Liang H, Li S, He J. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21(3):335–337. doi: 10.1016/S1470-2045(20)30096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ueda M, Martins R, Hendrie PC, McDonnell T, Crews JR, Wong TL, et al. Managing cancer care during the COVID-19 pandemic: agility and collaboration toward a common goal. J Natl Compr Cancer Netw. 2020;18(4):1–4. doi: 10.6004/jnccn.2020.7560. [DOI] [PubMed] [Google Scholar]
- 6.Al-Shamsi HO, Alhazzani W, Alhuraiji A, Coomes EA, Chemaly RF, Almuhanna M et al (2020) A practical approach to the management of cancer patients during the novel coronavirus disease 2019 (COVID-19) pandemic: an international collaborative group. Oncologist. 10.1634/theoncologist.2020-0213 [DOI] [PMC free article] [PubMed]
- 7.Etkind SN, Ba B, Dtmh M, Bone AE, Ba M, Lovell N, et al. The role and response of palliative care and hospice services in epidemics and pandemics: a rapid review to inform practice during the COVID-19 pandemic. J Pain Symptom Manag. 2020;60:e31–e40. doi: 10.1016/j.jpainsymman.2020.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ferguson L, Barham D. Palliative care pandemic pack: a specialist palliative care service response to planning the COVID-19 pandemic. J Pain Symptom Manag. 2020;60:e18–e20. doi: 10.1016/j.jpainsymman.2020.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Powell VD, Silveira MJ. What should palliative care’s response be to the COVID-19 epidemic? J Pain Symptom Manag. 2020;60:e1–e3. doi: 10.1016/j.jpainsymman.2020.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arya A, Buchman S, Gagnon B, Downar J. Pandemic palliative care: beyond ventilators and saving lives. Can Med Assoc J. 2020;192(15):cmaj.200465. doi: 10.1503/cmaj.200465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zimmermann C, Swami N, Krzyzanowska M, Hannon B, Leighl N, Oza A, Moore M, Rydall A, Rodin G, Tannock I, Donner A, Lo C. Early palliative care for patients with advanced cancer: a cluster-randomised controlled trial. Lancet. 2014;383(9930):1721–1730. doi: 10.1016/S0140-6736(13)62416-2. [DOI] [PubMed] [Google Scholar]
- 12.Hannon B, Swami N, Pope A, Rodin G, Dougherty E, Mak E, Banerjee S, Bryson J, Ridley J, Zimmermann C. The oncology palliative care clinic at the Princess Margaret Cancer Centre: an early intervention model for patients with advanced cancer. Support Care Cancer. 2015;23(4):1073–1080. doi: 10.1007/s00520-014-2460-4. [DOI] [PubMed] [Google Scholar]
- 13.Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, et al. Toxicity and response criteria of the eastern cooperative oncology group. Am J Clin Oncol. 1982;5(6):649–655. doi: 10.1097/00000421-198212000-00014. [DOI] [PubMed] [Google Scholar]
- 14.Martin L, Watanabe S, Fainsinger R, Lau F, Ghosh S, Quan H, Atkins M, Fassbender K, Downing GM, Baracos V. Prognostic factors in patients with advanced cancer: use of the patient-generated subjective global assessment in survival prediction. J Clin Oncol. 2010;28(28):4376–4383. doi: 10.1200/JCO.2009.27.1916. [DOI] [PubMed] [Google Scholar]
- 15.https://otn.ca/ Accessed 07 May 20
- 16.Cancer Care Ontario Pandemic Plan Review Group. Pandemic planning clinical guideline for patients with cancer. Available at https://www.cancercareontario.ca/en/guidelines-advice/types-of-cancer/64736 Accessed 07 May 20
- 17.Hancock S, Preston N, Jones H, Gadoud A. Telehealth in palliative care is being described but not evaluated: a systematic review. BMC Palliat Care. 2019;18(1):114. doi: 10.1186/s12904-019-0495-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lloyd-Williams M. Out-of-hours palliative care advice line. Br J Gen Pract. 2001;51(469):677. [PMC free article] [PubMed] [Google Scholar]
- 19.Zimmermann C, Seccareccia D, Clarke A, Warr D, Rodin G. Bringing palliative care to a Canadian cancer center: the palliative care program at Princess Margaret Hospital. Support Care Cancer. 2006;14(10):982–987. doi: 10.1007/s00520-006-0093-y. [DOI] [PubMed] [Google Scholar]
- 20.Bryson J, Coe G, Swami N, Murphy-Kane P, Seccareccia D, le LW, Rodin G, Zimmermann C. Administrative outcomes five years after opening an acute palliative care unit at a comprehensive cancer centre. J Palliat Med. 2010;13(5):559–565. doi: 10.1089/jpm.2009.0373. [DOI] [PubMed] [Google Scholar]
- 21.Costantini M, Sleeman KE, Peruselli C, Higginson IJ (2020). Response and role of palliative care during the COVID-19 pandemic: a national telephone survey of hospices in Italy. medRxiv.2020.03.18.20038448 [DOI] [PMC free article] [PubMed]
- 22.Cheng HWB, Li CW, Chan KY, Sham MK. The first confirmed case of human avian influenza A(H7N9) in Hong Kong and the suspension of volunteer services: Impact on palliative care. J Pain Symptom Manage. 2014;47(6):2013–2015. doi: 10.1016/j.jpainsymman.2013.12.234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Health Ontario. Clinical triage protocol for major surge in COVID pandemic. Available at https://caep.ca/wp-content/uploads/2020/04/Clinical-Triage-Protocol-for-Major-Surge-in-COVID-Pandemic-March-28-202.pdf Accessed 07 May 20
- 24.COVID Resources VitalTalk. https://www.vitaltalk.org/guides/covid-19-communication-skills/ Accessed 17 May 2020
- 25.Ngoi N, Lim J, Ow S, Jen WY, Lee M, Teo W, et al. A segregated-team model to maintain cancer care during the COVID-19 outbreak at an academic center in Singapore. Ann Oncol. 2020;31:840–843. doi: 10.1016/j.annonc.2020.03.306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Waterhouse D, Harvey R, Hurley P, et al. Early impact of COVID-19 on the conduct of oncology clinical trials and long-term opportunities for transformation: findings from an American Society of Clinical Oncology Survey. JCO Oncology Practice. 2020;16:417–421. doi: 10.1200/OP.20.00275. [DOI] [PubMed] [Google Scholar]
- 27.www.criticalcarelearning.ca Accessed 07 May 20