Abstract
Sequence analyses highlight a massive peptide sharing between immunoreactive Epstein-Barr virus (EBV) epitopes and human proteins that—when mutated, deficient or improperly functioning—associate with tumorigenesis, diabetes, lupus, multiple sclerosis, rheumatoid arthritis, and immunodeficiencies, among others. Peptide commonality appears to be the molecular platform capable of linking EBV infection to the vast EBV-associated diseasome via cross-reactivity and questions the hypothesis of the “negative selection” of self-reactive lymphocytes. Of utmost importance, this study warns that using entire antigens in anti-EBV immunotherapies can associate with autoimmune manifestations and further supports the concept of peptide uniqueness for designing safe and effective anti-EBV immunotherapies.
Keywords: EBV epitopes, systemic lupus erythematosus, cross-reactivity, autoimmunity, negative selection, self-reactive lymphocytes, pathogenic autoantibodies
Introduction
The connection between Epstein-Barr virus (EBV) and Burkitt's lymphoma (BL) was discovered in 1964. 1 Almost contemporaneously, high anti-EBV antibody levels were found in BL. 2 3 Since then, EBV infection has been associated with a wide spectrum of malignancies that, besides BL, comprehends different types of lymphomas, nasopharyngeal carcinoma (NPC), breast and brain cancer, and oral hairy leukoplakia, 4 5 6 7 8 among others. In addition, EBV has been implicated in a wide variety of diseases, including systemic lupus erythematosus (SLE), Sjögren's syndrome, multiple sclerosis (MS), myasthenia gravis (MG), rheumatoid arthritis (RA), autoimmune thyroid disorders, inflammatory bowel disease, celiac diseases, diabetes, Parkinson's disease, myopericarditis, dilated cardiomyopathy, and even death. 9 10 11 12 13 14
At the same time, anti-EBV antibody level was found to be higher in BL patients than in control subjects. 3 15 16 17 High level of anti-EBV immunoglobulin G antibodies were also found in subjects with NPC, 18 19 20 21 with IgG reactivity increasing significantly with tumor stage 21 ; Hodgkin and non-Hodgkin lymphomas 22 23 24 ; precancerous gastric lesions 25 ; MS 26 27 28 29 ; RA 30 31 32 ; MG 33 34 ; and SLE, 29 31 34 among others. In general, high antibody titers to EBV appeared to be related to a worse prognosis, a phenomenon that has been described by Coutinho's laboratory 35 as “the advantage of being low-respondents.” Currently, measurement of increased anti-EBV antibody titers is utilized to predict, to detect, and to monitor the progression of EBV-related cancers and progression of the various EBV-induced diseases. 36 37 38
Today, in front of such well known clinical context, the molecular mechanism(s) by which anti-EBV immune responses relate to the EBV diseasome, from lymphomas to Parkinson's disease, are still obscure. From a logical point of view, a central question remains unanswered and perhaps, as far as we know, has never been clearly posed: why the powerful anti-EBV immune responses herald cancers, autoimmune diseases, and death instead of eradicating the viral infection and re-establishing a healthy status?
In the clinical frame exposed above and on the basis of previous scientific reports 39 40 41 42 that have detailed a high level of peptide sharing between EBV and human proteins involved in crucial functions, this study investigates whether the immune responses that accompany active EBV infection have the potential to cross-react with and damage human proteins that, when altered, can lead to various cancer and autoimmune diseases. That is, the thesis is explored according to which the anti-EBV immune responses that should be a “protective defense” from EBV infection actually cross-react with human proteins, in this way setting up an anti-human protein assault with catastrophic pathologic sequelae in the body. Specifically, the present study used the pentapeptide as an antigenic and immunogenic unit, 43 44 45 46 47 48 and analyzed 3,197 experimentally validated immunoreactive EBV-derived epitopes for pentapeptide matches with the human proteome. Data are reported on a vast peptide sharing between EBV epitopes and proteins involved in tumorigenesis, autoimmune disorders, diabetes, and death, among others. The data suggest that cross-reactivity is the mechanism underlying the causal connection between EBV infection, immune response, and the EBV-associated diseases.
Methods
An EBV immunome formed by 3,197 immunopositive linear epitopes was assembled from Immune Epitope DataBase (IEDB, www.iedb.org ). 49 The immunopositive EBV epitopes are listed in Supplementary Table S1 (available in the online version). EBV epitope sequences were dissected into pentapeptides overlapped each other by four amino acid (aa) residues. The resulting 11,564 pentapeptides were analyzed for occurrence(s) within the human proteome using Pir Peptide Match Program. 50 Proteins related to EBV-induced diseases were annotated. UniProtKB database ( http://www.uniprot.org/ ) 51 PubMed, and OMIM resources were used.
Results
Quantitation of the Peptide Sharing between EBV Epitopes and the Human Proteome
Following matching analyses of the 11,564 pentapeptides composing the 3,197 experimentally validated immunoreactive EBV epitopes, it was found that almost all of the epitope-derived pentapeptides (i.e., 93%) are widespread among thousands of human proteins ( Table 1 ). From a mathematical point of view, if one considers that the probability of a pentapeptide to occur in two proteins is 20 −5 (or 1 out of 3,200,000 or 0.0000003125), then the peptide overlap existing between the EBV immunome and the human proteome is staggering.
Table 1. Numerical description of the pentapeptide sharing between the set of 3,197 immunopositive EBV epitopes and the human proteome.
| Pentapeptides composing the 3,197 EBV epitope immunome | 11,564 |
| EBV epitope pentapeptides not shared with the human proteome | 798 |
| EBV epitope pentapeptides shared with the human proteome | 10,766 |
| Human proteins sharing pentapeptides with EBV epitopes | 18,744 |
| Occurrences of EBV epitope pentapeptides in the human proteome (including multiple occurrences) | 137,805 |
Abbreviation: EBV, Epstein-Barr virus.
Distribution of the Peptide Sharing among EBV Epitopes
A synthetic snapshot (i.e., 201 EBV epitopes) of the immunoreactive peptide sharing is shown in Table 2 , where peptide sequences shared with the human proteins are given in capital format and peptide fragments uniquely present in EBV are given with aa in small bold format. Table 2 clearly shows that the immunoreactive EBV epitopes are predominantly composed by peptide sequences common to human proteins.
Table 2. Pentapeptide sharing between 201 immunoreactive EBV epitopes and human proteins a .
| IEDB ID b | EPITOPE c d | IEDB ID b | EPITOPE c d | IEDB ID b | EPITOPE c d |
|---|---|---|---|---|---|
| 950 | AEGLRALLARSHVER | 45499 | NPTQAPVIQLVHAVY | 127195 | TEMYIMYAM |
| 1518 | AGGAGAGGGAGGA | 46498 | NVTQVGSEPISPEIG | 127369 | WEMRAGREI |
| 1716 | AGVFVYGGSKTSLYN | 47613 | PGAPGGSGSGP | 127392 | WPTPKTHPV |
| 2390 | ALA ipqcr L | 47760 | PGTGPGNGLGEKGDT | 127408 | yamai RQAI |
| 2742 | ALLVLYSFAL | 48320 | PLFDRKSDAK | 137773 | YNLRRGIAL |
| 2743 | ALLVLYSFALMLIIIILIIF | 48486 | PLSRLPFGM | 138854 | GAGAGAGA |
| 3005 | ALWNLHGQALFLGIVL | 48852 | PPPGRRP ffhpv GE | 138856 | GRGRGRGR |
| 3600 | apify PPVL | 48876 | PPP qapyq GY | 138882 | MTAASYARY |
| 3782 | APRLPDDPI | 49864 | PVFDRKSDAK | 138873 | LMARRARSL |
| 3951 | AQEILSDNSEISVFPK | 50298 | QAKWRLQTL | 141342 | LLDFVRMGV |
| 5316 | AVFDRKSDAK | 51685 | QNGALAINTF | 144799 | TLNLT |
| 5317 | AVFDRKSVAK | 51946 | QPRAPIRPI | 167590 | GPQRR |
| 5326 | AVFNRKSDAK | 52142 | QQ rpvmfv SRVPAKK | 186702 | PQPRAPIRPIPT |
| 5439 | AVLL heesm | 53195 | RARGRGRGRGEKRP | 191290 | FIVFLQTHI |
| 8120 | DEPASTEPVHDQLL | 54367 | RKIYDLIEL | 227777 | HPVAEADYFEY |
| 8905 | DKI vqapify PPVLQ | 54728 | RLRAEAQVK | 230640 | ASDYSQGAF |
| 9644 | DP hgpvq LSYYD | 55251 | R ppifi RLL | 230798 | FYPPVLQPI |
| 10448 | DTPLIPLTIF | 55298 | RPQKRPSCI | 231136 | LAYA rgqam |
| 10858 | DYDASTESEL | 55327 | RPRPPARSL | 231402 | RRVRRRVLV |
| 10963 | DYSQGAFTPL | 55529 | RRARSLSAERY | 231547 | TVFY nippm |
| 11804 | EENLLDFVRF | 55619 | RRIYDIEL | 231696 | YRTATLRTL |
| 12183 | EGGVGWRHW | 56506 | RYAREAEVRF | 231699 | YSQGAFTPL |
| 13628 | EPDVPPGAIEQGPAD | 56523 | RYEDPDAPL | 231800 | AQPAPQAPY |
| 16876 | FLRGRAYGI | 56650 | RYSIFFDY | 231839 | DSIMLTATF |
| 17110 | FMVFLQTHI | 56651 | RYSIFFDYM | 231840 | DTR aidqf F |
| 17600 | FRKAQIQGL | 57755 | SFFDRKSDAK | 231880 | FLQRTDLSY |
| 18328 | FVYGGSKTSL | 59084 | SLFDRKSDAK | 231966 | HVIQNAFRK |
| 18438 | FY nippm PL | 59432 | SLREWLLRI | 232020 | KPWLRAHPV |
| 18946 | GDDGDDGDEGGDGDE | 62305 | SVRDRLARL | 232021 | KQRKPGGPW |
| 19674 | GGAGGAGGAGAGGGAG | 67456 | TYSAGIVQI | 232030 | KTIG nfkpy |
| 19737 | GGGAGAGGAGAGGGGR | 68561 | VFSDGRVAC | 232074 | LPTPMQLAL |
| 20023 | GGSKTSLYNLRRGTA | 69558 | VLKDAIKDL | 232076 | LQALSNLIL |
| 21719 | GPPAA | 70251 | VPAPAGPIV | 232078 | LQSSSYPGY |
| 21723 | GPPAAGPPAAGPPAA | 70624 | VQPPQLTQV | 232080 | LS aeryt LF |
| 21870 | GQGGSPTAM | 70932 | VSFI efvgw | 232081 | LSVIPSNPY |
| 22159 | GRPAVFDRKSDAKST | 71968 | VYAASFSPNL | 232086 | LTQAAGQAF |
| 22976 | GVFVYGGSKTSLYNL | 72028 | VYGGSKTSL | 232095 | LVSSGNTLY |
| 23324 | G ydvgh GPL | 72251 | WAPSV | 232096 | LVSSSAPSW |
| 23449 | GYRTATLRTL | 73221 | WVPSV | 232103 | MEQRVMATL |
| 23994 | H hiwqnll | 74120 | yhliv DTDSL | 232177 | QEPGPVGPL |
| 24170 | HLAAQGMAY | 75188 | YNLRRGTAL | 232178 | QEQLSDTPL |
| 24533 | HPV geady | 75189 | YNLRRGTALAIPQ | 232199 | RESIVCYFM |
| 24666 | HRCQAIRK | 75356 | YPL heqhg M | 232214 | RLHRLLLMR |
| 24667 | HRCQAIRKK | 75360 | YPLHKQHGM | 232232 | RPAP pkiam |
| 26480 | IIFIFRRDLLCPLGAL | 75731 | YSFALMLIIIILIIFIFRRD | 232276 | SEPCEALDL |
| 26538 | IIIILIIFI | 79634 | QPRAPIRPIT | 232308 | SQISNTEMY |
| 27103 | ILIIFIFRRDLLCPLGALCI | 93251 | LLARSHVER | 232332 | TE dnvppwl |
| 27301 | ILRQLLTGGVKKGRP | 94034 | THIFAEVLKD | 232416 | VTFSAGTFK |
| 27375 | ILTDFSVIK | 97317 | fwemr AGREITQ | 232419 | VTTQRQSVY |
| 29618 | IYLLEMLWRL | 98084 | GVFVYGGSK | 232427 | waqig HIPY |
| 30430 | KEHVIQNAF | 101654 | FVYGGSKTSLY | 232437 | WQRRYRRIY |
| 30431 | KEHVIQNAFRK | 101878 | LQTHIFAEV | 232473 | YQEPPAHGL |
| 33207 | KR ppifi RR | 102253 | YPL heqyg M | 237896 | QTAAAVVF |
| 33866 | KTSLYNLRRGTALA | 106084 | RPRSPSSQSSSSGSPPRRP | 237920 | RYKNRVASR |
| 35162 | LDFVRFMGV | 107724 | AARQRLQDI | 540571 | QPRLTPPQPL |
| 35533 | LEKARGSTY | 107869 | GPKVKRPPI | 540583 | RPTELQPTP |
| 37153 | LLDFVRFMGV | 108006 | LLDFV rfmgy | 540628 | TSSPSMPEL |
| 38514 | LPGPQVTAVLLHEES | 108191 | VMATLLPPV | 548981 | LLDFVRFMG |
| 39102 | lrgkw QRRYR | 118970 | PPPGRRP | 548987 | NGALAINTF |
| 39634 | LSRLPFGMA | 124861 | WNLHGQALFL | 548994 | QNGALAINT |
| 41113 | MARRARSLS aeryt L | 126528 | LA samrm LW | 595247 | FGLVLFPAQI |
| 41147 | MATLLPPVPQQPRAG | 126967 | RPRP rtpew | 653929 | AAQGMAY |
| 41841 | mkkaw LSRAQQADAG | 126980 | RRAALSGHL | 672845 | PIFIRRL |
| 42525 | MSDEGPGTGPGNGLG | 126985 | RRLHRLLLM | 674203 | R amsfi ATY |
| 42941 | MVFLQTHIFAEVLKD | 126986 | RRRRRRAAL | 675184 | R ppifi R |
| 44181 | NIAEGLRAL | 126991 | RRYRRIYDL | 676208 | RRIYDLI |
| 45378 | N pkfen IAEGLRALL | 127118 | SQAAFGLPI | 695961 | QAPYPGYEE |
Abbreviations: EBV, Epstein-Barr virus; IEDB, Immune Epitope DataBase.
Epitopes assembled from IEDB ( www.iedb.org ). 49 Epitope experimental details and references are available at www.iedb.org .
Epitopes listed according to IEDB ID number. 49
Epitope sequences given in 1-letter code.
Pentapeptides shared between EBV epitopes and human proteins are given in capital letters, while pentapeptides present only in EBV are given in bold small format.
Immunologically, Tables 1 and 2 document that the experimentally validated immunoreactive EBV epitopes mostly consist of pentapeptides that also occur in human proteins, in this way indicating a highest cross-reactivity potential, given the fact that a pentapeptide is a minimal immune determinant that contains the immunological information in terms of both immunogenicity and antigenicity. 43 44 45 46 47 48
The Pathological Implications of the Peptide Sharing between EBV Epitopes and Human Proteins: Lymphomas and Leukemias
Numerous cancer-related proteins share peptides with the here analyzed self-reactive EBV epitopes. Reasons of space do not permit a detailed peptide-by-peptide description of the sharing and only a few examples are described in Tables 3 and 4 . Specifically, Table 3 shows the peptide sharing between the immunoreactive EBV epitopes and human proteins that—when mutated, modified, improperly functioning or deficient—are implicated in lymphomagenesis/leukemogenesis. 52 53 54 55 56 57 58 59 60 61 62 63 64 65 66 67 68 69 70 71 72 73 74 75 76 77 78 79 80 81 82 83 84 85 86 87 88 89 90 91 It can be seen that the extent of the peptide sharing is very high and comes to the fore with glaring evidence when focusing on histone-lysine N -methyltransferase 2D (KMT2D), the disruption of which perturbs germinal center B cell development and promotes lymphomagenesis. 77 78 KMT2D alterations are involved in follicular lymphoma and diffuse large B-cell lymphoma, 92 cutaneous T-cell lymphoma and Sézary syndrome, 93 ocular adnexal MALT-type marginal zone lymphomas, 79 and chronic myeloid leukemia. 94 Moreover, KMT2D alterations are involved in intraocular medulloepithelioma, 95 small cell lung cancer, 96 bladder cancer, 97 98 and non-small-cell lung cancer. 99 Of not less importance, alterations of KMT2D have a causal role in Kabuki syndrome 100 that is characterized by skeletal and visceral abnormalities and cardiac anomalies, 101 hyperinsulinism, 102 epilepsy, 103 desmoid fibromatosis, 104 immunopathological manifestations, 105 lupus, 106 and oriental alterations, 107 among others.
Table 3. Pentapeptide sharing between immunoreactive EBV epitopes and human proteins implicated in lymphomagenesis/leukemogenesis.
| Shared peptides | Lymphoma/Leukemia-related proteins containing EBV epitope peptide(s) a | Ref b |
|---|---|---|
| LSPLL, RRQKR, LALRA, KEVLE, LGLGD, GNLVT, SLESV, LPTLL, PETVP, ALYLQ, ARVKE, PSLKL, KILLA, NPETL, EGLKD, LYLQQ, QKRPS, VAKVA, DRHSD, LQAIG, LSQVC, RPSCI | ATM: Serine-protein kinase ATM | 52 |
| PLPPP, PPLPP, LPTLL, REAIL, AERHG, CKKDH | BANK1: B-cell scaffold protein with ankyrin repeats | 53 54 |
| EEEEE, PPLPP, GAGGG, AGAGG, GAGGA, AGGGA, GRGGG, PPPVS, LSAAS, PPLGP, PPVSP, EPGPA, PVSPG, SSLTP, TPPPQ, GDDDD, AVAQS, DPSLG, GNSST, PGLFP, SEPVE, DDAGG, DDDAG | BC11B: B-cell lymphoma/leukemia 11B | 55 56 57 |
| SSSEE, GPPSP, APAST, GPEAR, PCPQA, PQARL, RFIQA | BCL6B: B-cell/lymphoma 6 member B protein | 58 59 60 61 62 |
| SPSPP, PLPPV, GSGAG, PAGSL, PVPPP, EPGPA, EQASL, EGTRL, LDLDF, LNQNL, VLQKL | BIN1: Myc box-dependent-interacting protein 1 | 63 |
| LLLLL, LRLLL, RLRLL, KEDDG, EGGQN | CADM1: Cell adhesion molecule 1 | 64 |
| PPPPP, LPPPP, GSGSG, GGGSG, GAGGG, GSGGS, SGGSG, GGSGS, SGSGG, LPPVP, PPVPA, PVPPT, QQGSG, CTPGD, PYILD | CBL: E3 ubiquitin-protein ligase CBL | 65 |
| PPPLP, PPGPS, LSPLS, SSPQP, ATSGA, ENLLD, EENLL, SPVLG, AFEEV, GPQDP, YDAPG | CRTC2: CREB-regulated transcription coactivator 2 | 66 |
| LLARL, GASGS, VAGLL, PLHAL, LARLR, SGASP, CGLLR, VPKPR, FIRRL, TDGKT, TPLLT, ALIKT, SSCNS | DAPK1: Death-associated protein kinase 1 | 67 68 |
| EEEAE, FGLSR, SDLSR, SLESV, KAIEE, VIQLV, IIAVV, VMDLL, IAVVA, IKAIE, ESFTQ, QDVGA, RLFAA, TTGGK, VIKAI, SFTQG | EPHA7: Ephrin type-A receptor 7 (998 aa) | 69 |
| LLLLL, PPPPP, LPPPP, ALLLL, LALLL, PPPPS, PPLPP, FPPPP, SLSST, GSPPR, PPQVP, SPSDS, TLSPS, TSEPV, SEDDP, ESVDV, GTPPQ, TDGGG, TSVVQ, VYAAS, EDDPQ, PSELD, DLRPL, FVGDY, KGTPP, PRLFA, VCSVA, HSPVV, ILQIS, LYEAS, PYEAF | FAT1: Protocadherin Fat 1 | 70 71 |
| PPPPP, GGGGG, EEEEA, AAAAV, SSSEE, GGSGS, GGGGD, RGGSG, GAPGG, ASGPG, LPGVP, VSPAV, PGGLG, VEAHV, GGDGD, LRAAT, ERPLA, FPEGV, GGDKV | HIC1: Hypermethylated in cancer 1 protein | 72 |
| PPRPP, RRRKG, ATAAA, SVSQP, AEVLK, LLQTE, SHTAT | KDM6A: Lysine-specific demethylase 6A | 73 74 |
| PPPPP, QPPPP, SPPPP, SSSSA, SSSAP, PTPPP, GAPAA, KKRKR, RGGRG, GGRGR, PPPPY, SSSAG, GRGGR, LPPTP, APPTP, PPLGP, PTPLP, SGSPP, PQPPL, SQASA, DDEDL, STSVP, LPGVS, SSGTA, LTPRP, RPRGA, RQRSR, SGLGT, TPRPP, TPRPS, TSVPS, VTLPL, DLILQ, GTPRP, TPRPV, IAVSS, LDTED, TPRPR, LGATI, SAPRK, EGVEV, LSPAN, LSSCP, MQPPP, SLIQL, AKIEA, EDLFG, EEVEN, QGVQV, TPRSQ, VEDLF, LGLYA, PQSGP, DSREG, VSTAD, GPADD, PADDP, QSLIQ, VFPKD, DTDSL, GTFKP, IPQTL, PLQHW, TGQGK, EQHGM, IDDNS, LRPQW, QRHSD, TFKPP, GPRHT | KMT2C: Histone-lysine N -methyltransferase 2C | 75 76 |
| EEEEE, QPPPP, PLPPP, SAAAA, LRLLL, PAPAA, PAAAP, PTPPP, APPAP, GRGRG, PPSPG, PSPGS, PSPPP, RGRGR, SPLLP, AAPPA, GPAGP, LLAAL, PAQPP, SLGLA, LAPSP, LSPLL, PGPAG, SPSQS, SQSSS, GGRGR, GLPPP, PQGPP, RLRLL, LPPTP, LRSLG, PTLLL, SPSSQ, TPPPS, ALAPS, EGLRA, GPQPP, PEPPT, PLTEP, SSGSP, AASED, APVAP, AVGPP, DDEEL, ESPAR, GAHGG, GPPRL, KKRKR, LTPRP, PALDD, PPPGR, PPQGP, PPQVP, PPTQH, PTLGK, SDEAE, SPLLG, TPHTK, APYPG, ARPPE, ASDRL, CPSLD, DAAAR, EERPP, EGEGD, EGPST, EPRLA, FPDTK, FPEGL, GPLAI, GPWDP, GTQDP, IKVIE, LGLYA, LRLTP, LSPVI, PLLTV, PMSPP, PPTHP, PPVPQ, PQPLM, PQQPM, PSRPQ, QALAP, QEPPP, QTNQA, RGAFG, RPEFV, SDALG, SPVTP, SQTEL, SRVPA, SYTDP, TGSGG, TTPAG | KMT2D: Histone-lysine N -methyltransferase 2D | 77 78 79 |
| GGGGG, GGGGS, GGGGA, AGGGG, GGSGG, GGGSG, GAGGG, GGAGG, AGAGA, PPPEP, LRALL, LALRA, LTPPS, RALLA, RLLLK, PQAPE, TPLDL, GPETR, RVGAD | NFKB2: Nuclear factor NF-kappa-B p100 subunit | 80 81 82 83 |
| AAAPA, GAAAS, PAPGL, LLGGG, TPSPS, SLPHP, PHLPP, GSPTA, PLTSE, RDSYA, TTLAA, YPGYA, HRDSY, SYPGY | PRDM1: PR domain zinc finger protein 1 | 84 |
| EEEEE, PSPPP, APAAA, SPSPP, PSPSP, SPSPS, PLDLS, DEGEE, LDLSV, LLTPV, PTVSP, KQLLQ, VLDLS, LTPVT, TVSPS, VTEDL, AIEEE, TSEET, PAPTV, TPVTV, EAVSF, FKPPP, SFKPP, NIPQT, YSLRL, PALRD, RSQVK, PFVGD | PRDM2: domain zinc finger PR protein 2 | 85 86 87 88 |
| SSSSA, SPLLP, SSSAP, LSPLL, GTPSG, LQSET, PVSRF, AEGKL, PLRPT | SOCS6: Suppressor of cytokine signaling 6 | 68 |
| KKRKR, AGAAR, LQSLA, TSPTS, RSLLT, LSLVF, AGPSV, DPVHG, GPSVA, QATLG, TQLTQ, DLQDP, LEKQS, PVQGE, QERDV, PKTAS, PLTQP, NIEEF, TPHQP, SHETP | TET1: Methylcytosine dioxygenase TET1 | 89 |
| PPPLP, PPPPS, SPPPP, SSSEE, ELLEK, SASGS, QSSHL, APGGS, LQAPG, KLSSL, PPSQL, APPSQ, HLLQH, QQASV, VTKQE, VTVLT, PPTQH, PVTVL, GIKRT | TET2: Methylcytosine dioxygenase TET2 | 90 |
| PPPPP, LPPPP, PLPPP, PPPLP, PPLPP, PPPPS, GGGRG, APGGG, GLPAP, QPPPQ, PAPGP, PRGPP, PPSSG, SLGLA, LPAPG, LPPVP, PLPPV, PPPSR, GGRPG, PPPGR, DLRSL, VGPLS, PMPPP, SEGLV, SGNGP, ADIGA, DIGAP, GGDQG, PVGPL | WASP: Wiskott-Aldrich syndrome protein | 91 |
Human proteins reported by UniProt entry names.
Further references on the function/disease association at www.uniprot.org , OMIM, and PubMed resources.
Table 4. Quantitative pentapeptide matching between immunoreactive EBV epitopes and human proteins related to various cancers and diseases.
| Pentapeptides: | Human proteins sharing pentapeptides with EBV epitopes, and disease involvement c d | Refs. | |
|---|---|---|---|
| A a | B b | ||
| 3 | − | ACHA: Acetylcholine receptor subunit α. MG. | 117 |
| 7 | − | ACHD: Acetylcholine receptor subunit delta. MG. | 117 |
| 8 | − | ACHE: Acetylcholine receptor subunit epsilon. MG. | 117 |
| 9 | 11 | ACHG: Acetylcholine receptor subunit gamma. MG. | 117 |
| 31 | 42 | AGRB1: Adhesion G protein-coupled receptor B1. Inhibits glioma growth. | 118 119 |
| 15 | − | AKA12: A-kinase anchor protein 12. MG autoantigen. Involved in breast cancer. | 120 |
| 27 | − | APC: Adenomatous polyposis coli protein. Relates to colorectal adenomas and breast cancer. | 121 122 123 |
| 64 | 68 | APCL: Adenomatous polyposis coli protein 2. Its repression promotes ovarian cancer. | 123 124 |
| 57 | 68 | ARI1A: AT-rich interactive domain-containing protein 1A. Bladder, colorectal, endometrial, esophageal, gastric, kidney, liver, lung, ovarian cancers. | 108 |
| 68 | 92 | ARI1B: AT-rich interactive domain-containing protein 1B. Liver cancer. | 108 |
| 33 | − | ARID2: AT-rich interactive domain-containing protein 2. Liver, lung, melanoma cancers. | 108 |
| 23 | − | BCOR: BCL-6 corepressor. Tumor suppressor in endometrial cancer and medulloblastoma. | 108 125 |
| 9 | − | C1S: Complement C1s subcomponent precursor. SLE. | 126 |
| 20 | − | CHD4: Chromodomain-helicase-DNA-binding protein 4. Endometrial cancer. | 108 |
| 32 | 34 | CHD6. Chromodomain-helicase-DNA-binding protein 6. Bladder cancer. | 108 |
| 38 | − | CHD8: Chromodomain-helicase-DNA-binding protein 8. glioblastoma. | 108 |
| 10 | − | CLAT: Choline O-acetyltransferase. Myasthenic syndrome. | 127 |
| 17 | − | CO4A: Complement C4-A precursor. SLE. | 128 |
| 29 | 56 | CO4A1: Collagen α-1(IV) chain. Tumor suppressor; anti-angiogenic. | 129 |
| 17 | − | CO4B: Complement C4-B precursor. SLE. | 128 |
| 12 | 13 | CUL7: Cullin-7. 3M syndrome with growth restriction, skeletal abnormalities and dysmorphisms. | 130 |
| 25 | 26 | DCC: Netrin receptor DCC. Required for axon guidance. Colorectal cancer suppressor. | 131 |
| 16 | 66 | DMBT1: Deleted in malignant brain tumors 1 protein. Suppressed in human lung cancer. | 132 133 |
| 59 | − | DYST: Dystonin. Bullous pemphigoid. | 134 135 |
| 42 | − | FAT4: Protocadherin Fat 4. Involved in hepatocellular carcinoma. and in gastric cancer risk. | 136 137 |
| 34 | 38 | FUBP2: Far upstream element-binding protein 2. | 138 |
| 11 | − | IGF1R: Insulin-like growth factor 1 receptor. Intrauterine and postnatal growth retardation. | 139 |
| 14 | − | INSR: Insulin receptor. Insulin resistance syndrome with pineal hyperplasia. | 140 |
| 13 | − | INSR2: Insulin, isoform 2. Diabetes. | 141 |
| 27 | 31 | IRS1: Insulin receptor substrate 1. Diabetes. cognitive impairment and Alzheimer's disease. | 142 |
| 42 | 45 | IRS2: Insulin receptor substrate 2. Diabetes. cognitive impairment and Alzheimer's disease. | 142 143 144 |
| 38 | 50 | IRS4: Insulin receptor substrate 4. Diabetes. cognitive impairment and Alzheimer's disease. | 142 |
| 20 | − | KDM5A: Lysine-specific demethylase 5A. Intellectual disability. Inhibits glioma cells migration. | 145 146 |
| 2 | − | LA: Lupus La protein. SLE. | 147 |
| 16 | − | LRP1B: Low-density lipoprotein receptor-related protein 1B precursor 4599. | 148 |
| 6 | − | MAG: Myelin-associated glycoprotein precursor. MS. | 149 |
| 4 | − | MOG: Myelin-oligodendrocyte glycoprotein precursor. MS. | 150 |
| 13 | 19 | MYRF: Myelin regulatory factor. MS. | 151 |
| 17 | 12 | MYT1L: Myelin transcription factor 1-like protein. MS. | 152 |
| 45 | 47 | NBEL2: Neurobeachin-like protein 2 Role in neutrophil and NK cell function and pathogen defense. | 153 |
| 27 | − | NF1: Neurofibromin. neurofibromatosis. | 154 |
| 44 | 47 | NMDE4, Glutamate receptor ionotropic, NMDA 2D. Epileptic encephalopathy. | 155 |
| 97 | 113 | Obscurin: Heart disease. | 156 |
| 26 | 39 | SMCA4: Transcription activator BRG1. Esophageal, medulloblastoma, lung cancers. | 157 |
| 62 | 113 | SRRM2: Serine/arginine repetitive matrix protein 2. Thyroid carcinoma; Parkinson's disease. | 158 159 |
| 15 | − | STA13: StAR-related lipid transfer protein 13. Deleted in liver cancer 2 protein. | 160 |
| 8 | 9 | TGFB1: Transforming growth factor β-1 proprotein. Lupus nephritis in SLE Patients. | 161 |
| 250 | 341 | TITIN: Titin. Myocarditis, acute myocardial ischemia, cardiac arrest. | 162 |
| 32 | 34 | TRNK1: TPR and ankyrin repeat-containing protein 1. SLE. Neural development and differentiation. | 163 |
| 12 | − | TSP1: Thrombospondin-1. Inhibits tumor angiogenesis and suppresses tumor growth. | 164 |
| 24 | − | ZAN: Zonadhesin . Crucial role in sperm-zona adhesion. Sterility. | 165 |
| 40 | − | ZEP1: Zinc finger protein 40. Tum or-suppressive effects in prostate and nonsmall cell lung cancer. | 166 167 |
Abbreviations: EBV, Epstein-Barr virus; DNA, deoxyribonucleic acid; MG, myasthenia gravis; MS, multiple sclerosis; SLE, systemic lupus erythematosus.
Column A: number of shared peptides.
Column B: number of shared peptides including multiple occurrences.
Human proteins reported by UniProt entry names. Protein details, sequence, and aa length available at www.uniprot.org .
Further references on the function/associated disease are available at UniProt, OMIM, and PubMed resources.
Also, the intense peptide sharing between immunoreactive EBV epitopes and KMT2C is of relevance. KMT2C not only may act as a tumor suppressor in leukemias and T-cell lymphomas, 75 76 but it is also implicated in bladder, breast, colorectal, endometrial, gastric, head and neck, lung, and liver cancer, and in medulloblastoma. 108
Then, in spite of the lack of space, it is mandatory noting the harmful cross-reactivity platform represented by the peptide commonality between the immunoreactive EBV epitopes and Wiskott-Aldrich syndrome protein (WASP) ( Table 4 ). The 29 pentapeptides shared with EBV epitopes mainly occur throughout the central and COOH regulatory domains of the WASP primary sequence ( Fig. 1 , shared peptides in underlined bold character) and produce a “bull” for the EBV-activated immune system that is practically impossible not to hit. Hitting WASP can lead to lymphomagenesis. Indeed, WASP is a tumor suppressor frequently low or absent in anaplastic large cell lymphoma. 92 WASP deficiency relates to Wiskott-Aldrich syndrome (WAS). 109 110 111 112 WAS is characterized by eczema, thrombocytopenia, recurrent infections, immunodeficiency, neutropenia, and bloody diarrhea. 113 A large proportion of WAS patients develop autoimmunity and allergy since WASP appears to play an important role in the activation of CD4(+)CD25(+)FOXP3(+) natural regulatory T cells. 114 Even in the absence of typical clinical manifestations of WAS, a low expression of WASP associates with the pathogenesis of a subtype of inflammatory bowel disease. 115 Furthermore, deficiency of WASP associates with exacerbated experimental arthritis. 116
Fig. 1.
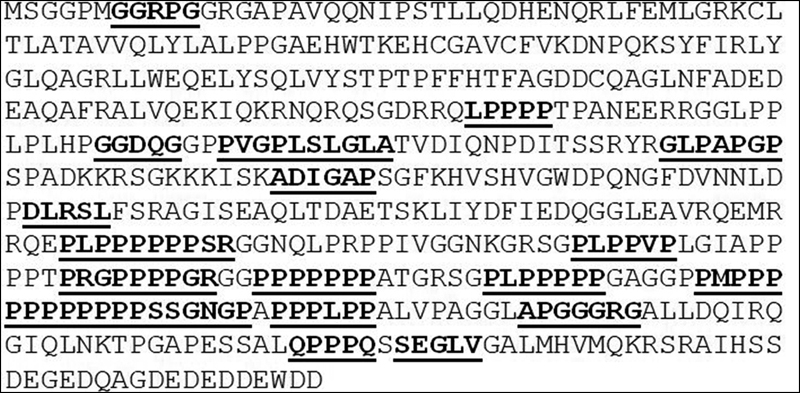
Distribution of EBV epitope-derived peptides throughout WASP primary aa sequence. WASP sequence from Uniprot ( http://www.uniprot.org/) . 51 EBV epitope-derived peptides are underlined and bold marked. EBV, Epstein-Barr virus; WASP, Wiskott-Aldrich syndrome protein.
Overall, the peptide sharing between the immunoreactive EBV epitopes and KMT2D, KMT2C, and WASP proteins suffices to define the constellation of human diseases associated with EBV infection.
The Pathological Implications of the Peptide Sharing between EBV Epitopes and Human Proteins: Various Cancers and Diseases
Table 4 illustrates that the EBV epitope-derived pentapeptides are widespread among the most disparate human proteins able to cause, when altered, a vast spectrum of diseases, from diabetes and sterility to myocarditis and death, 117 118 119 120 121 122 123 124 125 126 127 128 129 130 131 132 133 134 135 136 137 138 139 140 141 142 143 144 145 146 147 148 149 150 151 152 153 154 155 156 157 158 159 160 161 162 163 164 165 166 167 the latter two being possibly associated with the Titin imposing peptide sharing (250 shared pentapeptides).
Discussion
We summarize here the vast peptide platform that, with impressive mathematical unexpectedness, connects immunoreactive EBV epitopes and human proteins.
Quantitatively, Table 1 shows that the peptide sharing does not obey to any theoretical probability expectations or constraints such as, for example, protein dimension. The case is best illustrated by the far upstream element-binding protein 2 (FUBP2; 711 aa) and the low-density lipoprotein receptor-related protein 1B (LRP1B; 4,599 aa). FUBP2 has 34 pentapeptides in common with the herpesviral proteome, whereas the much longer LRP1B shares 16 pentapeptides ( Table 4 ). That is, a high number of shared pentapeptides can be found in a protein irrespective of the protein length.
Pathologically, the peptide sharing between the immunoreactive EBV epitopes and the human proteome implies the possibility of cross-reactions and of a consequent wide spectrum of diseases, from lymphomas and leukemias to diabetes and spermatogenesis ( Tables 3 and 4 ). From this point of view, Tables 3 and 4 offer a scientific explanation of the clinical fact that EBV infection can trigger so many and so various diseases in so different and distant parts of the body. Moreover, given the number of human proteins involved in the sharing, the possibility of cross-reacting with a specific protein or group of proteins and inducing a specific disease or group of diseases will depend on the “when and where” the disease-associated protein(s) will be expressed. Consequently, the EBV diseasome will manifest with different diseases depending on the age of the subjects and on the immunological imprinting by previous pathogen infections, 168 thus explaining also why, once the immune system has been activated by EBV, some subjects will develop a lymphoma while other subjects contract diabetes or lupus or will die.
Immunologically, the vast peptide sharing between immunoreactive EBV epitopes and human proteins fails to support the theory of microbial or of human immunological specificity and nullifies the current concept of self-tolerance. Indeed, it was advanced in the “50s and still persists today the Burnet's hypothesis according to which self-tolerance is achieved by the so-called negative selection” of self-reactive lymphocytes. 169 170 171 That is, lymphocytes with specificity for peptide sequences that are expressed in the human host are hypothesized to be deleted from the immunological repertoire during fetal or early life to avoid self-reactivity and the consequent autoimmunity. Clearly, such a hypothesis breaks down in front of the pervasive peptide overlap between immunoreactive EBV epitopes and human proteins. If the “negative selection” assumptions were true, the self-reactive lymphocytes targeting the experimentally validated EBV epitopes described here and almost exclusively composed by peptides common to human proteins would have had to be eliminated from the immunological repertoire in the fetal life. It seems that the postulated deletion of potentially self-reactive lymphocytes did not occur. Similar results have been obtained analyzing hepatitis C virus and human papillomavirus immunoreactive epitopes. 172 173 Altogether, our data indicate that potentially self-reactive lymphocytes are regularly produced by the immune system. It seems that the immune system, under physiological conditions, does not engage reactions with self-proteins or pathogens just in virtue of their peptide commonality. As already discussed, 174 175 176 it seems that it is just the vast peptide commonality to confer or, better, to reify protein immunotolerance.
As a collateral note, we observe that, while Tables 1 and 2 militate against the assumption of a “negative selection” of self-reactive lymphocytes, Tables 3 and 4 also question the defensive role of the immune response. By definition, immune system attacks pathogenic enemies and protects self-entities. That is, it is assumed that the immune system is endowed with the capacity of discerning a pathogen antigen from a self-protein and of behaving consequentially by attacking the “foes” and defending the “friends.” Instead of being analyzed and defined as an aggregate of molecules organized into functional biological pathways, the immune system is considered as a “thinking entity” that sees, discriminates, decides, and then attacks. Against such an anthropomorphous view, the present mathematical and biochemical data document that pathogenic immune responses can routinely occur following infections, as already experimentally demonstrated. 177 178 Pathogenic autoantibodies—that are usually considered as rare phenomena due to the so-called “immunological holes” deriving from an incomplete negative selection of the self-reactive lymphocytes 169 170 171 or that, even, have been denied as pure fantasies 179 —seem to be the rule.
Tables 3 and 4 show that anti-EBV immunoreactivity can hit a myriad of human proteins that, when (epi)genetically altered, can lead to cancers, autoimmune diseases, and even death. Such cross-reactive potential explains why higher the anti-EBV IgG antibody titer, worse may be the disease prognosis and faster the disease progression as described by a continuum of reports since the 1970s. 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 That is, autoimmunity is not a matter of “rare immunological holes,” but it is intrinsic to the immune response that involves most of the human proteome by being most of the human proteome shared with microbial entities as a result of a long evolutionary path that from viruses and bacteria led to the eukaryotic cell. 180
In conclusion, this study highlights the necessity of reviewing the hypothesis of the “negative selection” of self-reactive lymphocytes and, at the same time, emphasizes the importance of the “peptide uniqueness” concept to develop immunotherapies against EBV infection, and infections in general. Only immunotherapies based on peptides uniquely owned by the infectious agents would offer high specificity as well as the advantage of a lack of adverse events in the human host. 39 181 182 183
Funding Statement
Funding None.
Footnotes
Conflict of Interest D.K. declares no conflicts. Y.S. is a medical consultant in vaccine compensation court, United States.
Supplementary Material
References
- 1.Epstein M A, Achong B G, Barr Y M.Virus particles in cultured lymphoblasts from Burkitt's lymphoma Lancet 19641(7335):702–703. [DOI] [PubMed] [Google Scholar]
- 2.Old L J, Boyse E A, Oettgen H F. Precipitating antibody in human serum to an antigen present in cultured Burkitt's lymphoma cells. Proc Natl Acad Sci U S A. 1966;56(06):1699–1704. doi: 10.1073/pnas.56.6.1699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Henle G, Henle W, Clifford P. Antibodies to Epstein-Barr virus in Burkitt's lymphoma and control groups. J Natl Cancer Inst. 1969;43(05):1147–1157. [PubMed] [Google Scholar]
- 4.Gunvén P, Klein G, Henle G, Henle W, Clifford P.Epstein-Barr virus in Burkitt's lymphoma and nasopharyngeal carcinoma. Antibodies to EBV associated membrane and viral capsid antigens in Burkitt lymphoma patients Nature 1970228(5276):1053–1056. [DOI] [PubMed] [Google Scholar]
- 5.Harley B, Shivapathasundram G, Astradsson A, Muthurajah V, Wickremesekera A. An unusual presentation of cerebellar lymphoma. J Clin Neurosci. 2018;57:177–180. doi: 10.1016/j.jocn.2018.08.022. [DOI] [PubMed] [Google Scholar]
- 6.Yahia Z A, Adam A A, Elgizouli M. Epstein Barr virus: a prime candidate of breast cancer aetiology in Sudanese patients. Infect Agent Cancer. 2014;9(01):9. doi: 10.1186/1750-9378-9-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fołtyn S, Strycharz-Dudziak M, Drop B, Boguszewska A, Polz-Dacewicz M. Serum EBV antibodies and LMP-1 in Polish patients with oropharyngeal and laryngeal cancer. Infect Agent Cancer. 2017;12:31. doi: 10.1186/s13027-017-0141-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Khammissa R A, Fourie J, Chandran R, Lemmer J, Feller L. Epstein-Barr virus and its association with Oral Hairy Leukoplakia: a short review. Int J Dent. 2016;2016:4.941783E6. doi: 10.1155/2016/4941783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kivity S, Agmon-Levin N, Blank M, Shoenfeld Y. Infections and autoimmunity—friends or foes? Trends Immunol. 2009;30(08):409–414. doi: 10.1016/j.it.2009.05.005. [DOI] [PubMed] [Google Scholar]
- 10.Maślińska M. The role of Epstein-Barr virus infection in primary Sjögren's syndrome. Curr Opin Rheumatol. 2019;31(05):475–483. doi: 10.1097/BOR.0000000000000622. [DOI] [PubMed] [Google Scholar]
- 11.Dittfeld A, Gwizdek K, Michalski M, Wojnicz R. A possible link between the Epstein-Barr virus infection and autoimmune thyroid disorders. Cent Eur J Immunol. 2016;41(03):297–301. doi: 10.5114/ceji.2016.63130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Woulfe J M, Gray M T, Gray D A, Munoz D G, Middeldorp J M. Hypothesis: a role for EBV-induced molecular mimicry in Parkinson's disease. Parkinsonism Relat Disord. 2014;20(07):685–694. doi: 10.1016/j.parkreldis.2014.02.031. [DOI] [PubMed] [Google Scholar]
- 13.Di Loreto S, Fabiano C, Nigro G. High prevalence of streptococcal or Epstein-Barr virus infections in children with acute non-septic monoarthritis. New Microbiol. 2014;37(01):81–86. [PubMed] [Google Scholar]
- 14.Hasegawa D, Kaji M, Takeda H. Fatal degeneration of specialized cardiac muscle associated with chronic active Epstein-Barr virus infection. Pediatr Int. 2009;51(06):846–848. doi: 10.1111/j.1442-200X.2009.02925.x. [DOI] [PubMed] [Google Scholar]
- 15.Henle W, Hummeler K, Henle G. Antibody coating and agglutination of virus particles separated from the EB3 line of Burkitt lymphoma cells. J Bacteriol. 1966;92(01):269–271. doi: 10.1128/jb.92.1.269-271.1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Henle W, Henle G, Gunvén P, Klein G, Clifford P, Singh S. Patterns of antibodies to Epstein-Barr virus-induced early antigens in Burkitt's lymphoma. Comparison of dying patients with long-term survivors. J Natl Cancer Inst. 1973;50(05):1163–1173. doi: 10.1093/jnci/50.5.1163. [DOI] [PubMed] [Google Scholar]
- 17.Asito A S, Piriou E, Odada P S. Elevated anti-Zta IgG levels and EBV viral load are associated with site of tumor presentation in endemic Burkitt's lymphoma patients: a case control study. Infect Agent Cancer. 2010;5:13. doi: 10.1186/1750-9378-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu M Y, Shih Y Y, Chou S P. Antibody against the Epstein-Barr virus BHRF1 protein, a homologue of Bcl-2, in patients with nasopharyngeal carcinoma. J Med Virol. 1998;56(03):179–185. doi: 10.1002/(sici)1096-9071(199811)56:3<179::aid-jmv1>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 19.Cheng W M, Chan K H, Chen H L. Assessing the risk of nasopharyngeal carcinoma on the basis of EBV antibody spectrum. Int J Cancer. 2002;97(04):489–492. doi: 10.1002/ijc.1641. [DOI] [PubMed] [Google Scholar]
- 20.Fachiroh J, Schouten T, Hariwiyanto B. Molecular diversity of Epstein-Barr virus IgG and IgA antibody responses in nasopharyngeal carcinoma: a comparison of Indonesian, Chinese, and European subjects. J Infect Dis. 2004;190(01):53–62. doi: 10.1086/421245. [DOI] [PubMed] [Google Scholar]
- 21.Guo X, Li T, Li F. Intermittent abortive reactivation of Epstein-Barr virus during the progression of nasopharyngeal cancer as indicated by elevated antibody levels. Oral Oncol. 2019;93:85–90. doi: 10.1016/j.oraloncology.2019.04.024. [DOI] [PubMed] [Google Scholar]
- 22.Johansson B, Klein G, Henle W, Henle G. Epstein-Barr virus (EBV)-associated antibody patterns in malignant lymphoma and leukemia. I. Hodgkin's disease. Int J Cancer. 1970;6(03):450–462. doi: 10.1002/ijc.2910060316. [DOI] [PubMed] [Google Scholar]
- 23.Mueller N, Evans A, Harris N L. Hodgkin's disease and Epstein-Barr virus. Altered antibody pattern before diagnosis. N Engl J Med. 1989;320(11):689–695. doi: 10.1056/NEJM198903163201103. [DOI] [PubMed] [Google Scholar]
- 24.Mueller N E, Lennette E T, Dupnik K, Birmann B M. Antibody titers against EBNA1 and EBNA2 in relation to Hodgkin lymphoma and history of infectious mononucleosis. Int J Cancer. 2012;130(12):2886–2891. doi: 10.1002/ijc.26334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schetter A J, You W C, Lennette E T, Gail M T, Rabkin C S. Association of Epstein-Barr virus antibody levels with precancerous gastric lesions in a high-risk cohort. Cancer Sci. 2008;99(02):350–354. doi: 10.1111/j.1349-7006.2007.00668.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sumaya C V, Myers L W, Ellison G W, Ench Y. Increased prevalence and titer of Epstein-Barr virus antibodies in patients with multiple sclerosis. Ann Neurol. 1985;17(04):371–377. doi: 10.1002/ana.410170412. [DOI] [PubMed] [Google Scholar]
- 27.Farrell R A, Antony D, Wall G R. Humoral immune response to EBV in multiple sclerosis is associated with disease activity on MRI. Neurology. 2009;73(01):32–38. doi: 10.1212/WNL.0b013e3181aa29fe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jakimovski D, Ramanathan M, Weinstock-Guttman B. Higher EBV response is associated with more severe gray matter and lesion pathology in relapsing multiple sclerosis patients: a case-controlled magnetization transfer ratio study. Mult Scler. 2020;26(03):322–332. doi: 10.1177/1352458519828667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lossius A, Johansen J N, Torkildsen Ø, Vartdal F, Holmøy T. Epstein-Barr virus in systemic lupus erythematosus, rheumatoid arthritis and multiple sclerosis—association and causation. Viruses. 2012;4(12):3701–3730. doi: 10.3390/v4123701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alspaugh M A, Henle G, Lennette E T, Henle W. Elevated levels of antibodies to Epstein-Barr virus antigens in sera and synovial fluids of patients with rheumatoid arthritis. J Clin Invest. 1981;67(04):1134–1140. doi: 10.1172/JCI110127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Toussirot E, Roudier J. Epstein-Barr virus in autoimmune diseases. Best Pract Res Clin Rheumatol. 2008;22(05):883–896. doi: 10.1016/j.berh.2008.09.007. [DOI] [PubMed] [Google Scholar]
- 32.Cavalcante P, Serafini B, Rosicarelli B. Epstein-Barr virus persistence and reactivation in myasthenia gravis thymus. Ann Neurol. 2010;67(06):726–738. doi: 10.1002/ana.21902. [DOI] [PubMed] [Google Scholar]
- 33.Csuka D, Banati M, Rozsa C, Füst G, Illes Z. High anti-EBNA-1 IgG levels are associated with early-onset myasthenia gravis. Eur J Neurol. 2012;19(06):842–846. doi: 10.1111/j.1468-1331.2011.03636.x. [DOI] [PubMed] [Google Scholar]
- 34.Draborg A H, Lydolph M C, Westergaard M. Elevated concentrations of serum immunoglobulin free light chains in systemic lupus erythematosus patients in relation to disease activity, inflammatory status, B cell activity and Epstein-Barr virus antibodies. PLoS One. 2015;10(09):e0138753. doi: 10.1371/journal.pone.0138753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Martínez-A C, Marcos M A, de la Hera A.Immunological consequences of HIV infection: advantage of being low responder casts doubts on vaccine development Lancet 19881(8583):454–457. [DOI] [PubMed] [Google Scholar]
- 36.Fachiroh J, Paramita D K, Hariwiyanto B. Single-assay combination of Epstein-Barr Virus (EBV) EBNA1- and viral capsid antigen-p18-derived synthetic peptides for measuring anti-EBV immunoglobulin G (IgG) and IgA antibody levels in sera from nasopharyngeal carcinoma patients: options for field screening. J Clin Microbiol. 2006;44(04):1459–1467. doi: 10.1128/JCM.44.4.1459-1467.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Paramita D K, Fachiroh J, Haryana S M, Middeldorp J M. Evaluation of commercial EBV RecombLine assay for diagnosis of nasopharyngeal carcinoma. J Clin Virol. 2008;42(04):343–352. doi: 10.1016/j.jcv.2008.03.006. [DOI] [PubMed] [Google Scholar]
- 38.Levin L I, Chang E T, Ambinder R F. Atypical prediagnosis Epstein-Barr virus serology restricted to EBV-positive Hodgkin lymphoma. Blood. 2012;120(18):3750–3755. doi: 10.1182/blood-2011-12-390823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Capone G, Calabrò M, Lucchese G. Peptide matching between Epstein-Barr virus and human proteins. Pathog Dis. 2013;69(03):205–212. doi: 10.1111/2049-632X.12066. [DOI] [PubMed] [Google Scholar]
- 40.Capone G, Fasano C, Lucchese G, Calabrò M, Kanduc D. EBV-associated cancer and autoimmunity: searching for therapies. Vaccines (Basel) 2015;3(01):74–89. doi: 10.3390/vaccines3010074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Calabrò M. Bari: University of Bari; 2015. Epstein Barr Virus Immunoevasion. Sequence Similarity between Human Proteins and Epstein Barr Virus [PhD thesis] [Google Scholar]
- 42.Kanduc D. Proteome-wide Epstein-Barr virus analysis of peptide sharing with human systemic lupus erythematosus autoantigens. Isr Med Assoc J. 2019;21(07):444–448. [PubMed] [Google Scholar]
- 43.Reddehase M J, Rothbard J B, Koszinowski U H.A pentapeptide as minimal antigenic determinant for MHC class I-restricted T lymphocytes Nature 1989337(6208):651–653. [DOI] [PubMed] [Google Scholar]
- 44.Zeng W, Pagnon J, Jackson D C. The C-terminal pentapeptide of LHRH is a dominant B cell epitope with antigenic and biological function. Mol Immunol. 2007;44(15):3724–3731. doi: 10.1016/j.molimm.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 45.Kanduc D. Homology, similarity, and identity in peptide epitope immunodefinition. J Pept Sci. 2012;18(08):487–494. doi: 10.1002/psc.2419. [DOI] [PubMed] [Google Scholar]
- 46.Raychaudhuri S, Sandor C, Stahl E A. Five amino acids in three HLA proteins explain most of the association between MHC and seropositive rheumatoid arthritis. Nat Genet. 2012;44(03):291–296. doi: 10.1038/ng.1076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kanduc D. Pentapeptides as minimal functional units in cell biology and immunology. Curr Protein Pept Sci. 2013;14(02):111–120. doi: 10.2174/1389203711314020003. [DOI] [PubMed] [Google Scholar]
- 48.Hao S S, Zong M M, Zhang Z. The inducing roles of the new isolated bursal hexapeptide and pentapeptide on the immune response of AIV vaccine in mice. Protein Pept Lett. 2019;26(07):542–549. doi: 10.2174/0929866526666190405123932. [DOI] [PubMed] [Google Scholar]
- 49.Vita R, Mahajan S, Overton J A.The Immune Epitope Database (IEDB): 2018 update Nucleic Acids Res 201947(D1):D339–D343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chen C, Li Z, Huang H, Suzek B E, Wu C H. A fast Peptide Match service for UniProt Knowledgebase. Bioinformatics. 2013;29(21):2808–2809. doi: 10.1093/bioinformatics/btt484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.UniProt Consortium. UniProt: a worldwide hub of protein knowledge Nucleic Acids Res 201947(D1):D506–D515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Grønbaek K, Worm J, Ralfkiaer E, Ahrenkiel V, Hokland P, Guldberg P. ATM mutations are associated with inactivation of the ARF-TP53 tumor suppressor pathway in diffuse large B-cell lymphoma. Blood. 2002;100(04):1430–1437. doi: 10.1182/blood-2002-02-0382. [DOI] [PubMed] [Google Scholar]
- 53.Yan J, Nie K, Mathew S. Inactivation of BANK1 in a novel IGH-associated translocation t(4;14)(q24;q32) suggests a tumor suppressor role in B-cell lymphoma. Blood Cancer J. 2014;4:e215. doi: 10.1038/bcj.2014.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Dam E M, Habib T, Chen J. The BANK1 SLE-risk variants are associated with alterations in peripheral B cell signaling and development in humans. Clin Immunol. 2016;173:171–180. doi: 10.1016/j.clim.2016.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kurosawa N, Fujimoto R, Ozawa T, Itoyama T, Sadamori N, Isobe M. Reduced level of the BCL11B protein is associated with adult T-cell leukemia/lymphoma. PLoS One. 2013;8(01):e55147. doi: 10.1371/journal.pone.0055147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Punwani D, Zhang Y, Yu J. Multisystem anomalies in severe combined immunodeficiency with mutant BCL11B. N Engl J Med. 2016;375(22):2165–2176. doi: 10.1056/NEJMoa1509164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gutierrez A, Kentsis A, Sanda T. The BCL11B tumor suppressor is mutated across the major molecular subtypes of T-cell acute lymphoblastic leukemia. Blood. 2011;118(15):4169–4173. doi: 10.1182/blood-2010-11-318873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Greipp P T, Smoley S A, Viswanatha D S. Patients with chronic lymphocytic leukaemia and clonal deletion of both 17p13.1 and 11q22.3 have a very poor prognosis. Br J Haematol. 2013;163(03):326–333. doi: 10.1111/bjh.12534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Xu L, Li X, Chu E S. Epigenetic inactivation of BCL6B, a novel functional tumour suppressor for gastric cancer, is associated with poor survival. Gut. 2012;61(07):977–985. doi: 10.1136/gutjnl-2011-300411. [DOI] [PubMed] [Google Scholar]
- 60.Yang Q, Gao J, Xu L, Zeng Z, Sung J J, Yu J. Promoter hypermethylation of BCL6B gene is a potential plasma DNA biomarker for gastric cancer. Biomarkers. 2013;18(08):721–725. doi: 10.3109/1354750X.2013.853839. [DOI] [PubMed] [Google Scholar]
- 61.Deng J, Liang H, Dong Q. The survival decrease in gastric cancer is associated with the methylation of B-cell CLL/lymphoma 6 member B promoter. Open Biol. 2014;4(07):140067. doi: 10.1098/rsob.140067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wang J, Dong L, Xu L. B cell CLL/lymphoma 6 member B inhibits hepatocellular carcinoma metastases in vitro and in mice. Cancer Lett. 2014;355(02):192–200. doi: 10.1016/j.canlet.2014.08.025. [DOI] [PubMed] [Google Scholar]
- 63.Esmailzadeh S, Huang Y, Su M W, Zhou Y, Jiang X. BIN1 tumor suppressor regulates Fas/Fas ligand-mediated apoptosis through c-FLIP in cutaneous T-cell lymphoma. Leukemia. 2015;29(06):1402–1413. doi: 10.1038/leu.2015.9. [DOI] [PubMed] [Google Scholar]
- 64.Fu L, Gao Z, Zhang X. Frequent concomitant epigenetic silencing of the stress-responsive tumor suppressor gene CADM1, and its interacting partner DAL-1 in nasal NK/T-cell lymphoma. Int J Cancer. 2009;124(07):1572–1578. doi: 10.1002/ijc.24123. [DOI] [PubMed] [Google Scholar]
- 65.Martinelli S, Checquolo S, Consoli F. Loss of CBL E3-ligase activity in B-lineage childhood acute lymphoblastic leukaemia. Br J Haematol. 2012;159(01):115–119. doi: 10.1111/j.1365-2141.2012.09245.x. [DOI] [PubMed] [Google Scholar]
- 66.Fang M, Pak M L, Chamberlain L, Xing W, Yu H, Green M R. The CREB coactivator CRTC2 is a lymphoma tumor suppressor that preserves genome integrity through transcription of DNA mismatch repair genes. Cell Reports. 2015;11(09):1350–1357. doi: 10.1016/j.celrep.2015.04.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Shawky S A, El-Borai M H, Khaled H M. The prognostic impact of hypermethylation for a panel of tumor suppressor genes and cell of origin subtype on diffuse large B-cell lymphoma. Mol Biol Rep. 2019;46(04):4063–4076. doi: 10.1007/s11033-019-04856-x. [DOI] [PubMed] [Google Scholar]
- 68.Küçük C, Hu X, Jiang B. Global promoter methylation analysis reveals novel candidate tumor suppressor genes in natural killer cell lymphoma. Clin Cancer Res. 2015;21(07):1699–1711. doi: 10.1158/1078-0432.CCR-14-1216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Oricchio E, Nanjangud G, Wolfe A L. The Eph-receptor A7 is a soluble tumor suppressor for follicular lymphoma. Cell. 2011;147(03):554–564. doi: 10.1016/j.cell.2011.09.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Laginestra M A, Cascione L, Motta G. Whole exome sequencing reveals mutations in FAT1 tumor suppressor gene clinically impacting on peripheral T-cell lymphoma not otherwise specified. Mod Pathol. 2020;33(02):179–187. doi: 10.1038/s41379-019-0279-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hu X, Zhai Y, Kong P. FAT1 prevents epithelial mesenchymal transition (EMT) via MAPK/ERK signaling pathway in esophageal squamous cell cancer. Cancer Lett. 2017;397:83–93. doi: 10.1016/j.canlet.2017.03.033. [DOI] [PubMed] [Google Scholar]
- 72.Stöcklein H, Smardova J, Macak J. Detailed mapping of chromosome 17p deletions reveals HIC1 as a novel tumor suppressor gene candidate telomeric to TP53 in diffuse large B-cell lymphoma. Oncogene. 2008;27(18):2613–2625. doi: 10.1038/sj.onc.1210901. [DOI] [PubMed] [Google Scholar]
- 73.Chang S, Yim S, Park H. The cancer driver genes IDH1/2, JARID1C/ KDM5C, and UTX/ KDM6A: crosstalk between histone demethylation and hypoxic reprogramming in cancer metabolism. Exp Mol Med. 2019;51(06):1–17. doi: 10.1038/s12276-019-0230-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Schulz W A, Lang A, Koch J, Greife A. The histone demethylase UTX/KDM6A in cancer: progress and puzzles. Int J Cancer. 2019;145(03):614–620. doi: 10.1002/ijc.32116. [DOI] [PubMed] [Google Scholar]
- 75.Yang W, Ernst P. Distinct functions of histone H3, lysine 4 methyltransferases in normal and malignant hematopoiesis. Curr Opin Hematol. 2017;24(04):322–328. doi: 10.1097/MOH.0000000000000346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Fernandez-Pol S, Ma L, Joshi R P, Arber D A. A survey of somatic mutations in 41 genes in a cohort of T-cell lymphomas identifies frequent mutations in genes involved in epigenetic modification. Appl Immunohistochem Mol Morphol. 2019;27(06):416–422. doi: 10.1097/PAI.0000000000000644. [DOI] [PubMed] [Google Scholar]
- 77.Froimchuk E, Jang Y, Ge K. Histone H3 lysine 4 methyltransferase KMT2D. Gene. 2017;627:337–342. doi: 10.1016/j.gene.2017.06.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Zhang J, Dominguez-Sola D, Hussein S. Disruption of KMT2D perturbs germinal center B cell development and promotes lymphomagenesis. Nat Med. 2015;21(10):1190–1198. doi: 10.1038/nm.3940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Johansson P, Klein-Hitpass L, Grabellus F. Recurrent mutations in NF-κB pathway components, KMT2D, and NOTCH1/2 in ocular adnexal MALT-type marginal zone lymphomas. Oncotarget. 2016;7(38):62627–62639. doi: 10.18632/oncotarget.11548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Wang Y, Cui H, Schroering A. NF-kappa B2 p100 is a pro-apoptotic protein with anti-oncogenic function. Nat Cell Biol. 2002;4(11):888–893. doi: 10.1038/ncb872. [DOI] [PubMed] [Google Scholar]
- 81.Keller U, Huber J, Nilsson J A. Myc suppression of Nfkb2 accelerates lymphomagenesis. BMC Cancer. 2010;10:348. doi: 10.1186/1471-2407-10-348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Thakur S, Lin H C, Tseng W T. Rearrangement and altered expression of the NFKB-2 gene in human cutaneous T-lymphoma cells. Oncogene. 1994;9(08):2335–2344. [PubMed] [Google Scholar]
- 83.Klemann C, Camacho-Ordonez N, Yang L. Clinical and immunological phenotype of patients with primary immunodeficiency due to damaging mutations in NFKB2. Front Immunol. 2019;10:297. doi: 10.3389/fimmu.2019.00297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zhang T, Ma J, Nie K. Hypermethylation of the tumor suppressor gene PRDM1/Blimp-1 supports a pathogenetic role in EBV-positive Burkitt lymphoma. Blood Cancer J. 2014;4:e261. doi: 10.1038/bcj.2014.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Johansson P, Klein-Hitpass L, Choidas A. SAMHD1 is recurrently mutated in T-cell prolymphocytic leukemia. Blood Cancer J. 2018;8(01):11. doi: 10.1038/s41408-017-0036-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Geli J, Kiss N, Kogner P, Larsson C. Suppression of RIZ in biologically unfavourable neuroblastomas. Int J Oncol. 2010;37(05):1323–1330. doi: 10.3892/ijo_00000784. [DOI] [PubMed] [Google Scholar]
- 87.Xie W, Li X, Chen X, Huang S, Huang S. Decreased expression of PRDM2 (RIZ1) and its correlation with risk stratification in patients with myelodysplastic syndrome. Br J Haematol. 2010;150(02):242–244. doi: 10.1111/j.1365-2141.2010.08186.x. [DOI] [PubMed] [Google Scholar]
- 88.Sasaki O, Meguro K, Tohmiya Y, Funato T, Shibahara S, Sasaki T. Altered expression of retinoblastoma protein-interacting zinc finger gene, RIZ, in human leukaemia. Br J Haematol. 2002;119(04):940–948. doi: 10.1046/j.1365-2141.2002.03972.x. [DOI] [PubMed] [Google Scholar]
- 89.Cimmino L, Dawlaty M M, Ndiaye-Lobry D. TET1 is a tumor suppressor of hematopoietic malignancy. Nat Immunol. 2015;16(06):653–662. doi: 10.1038/ni.3148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Kosmider O, Gelsi-Boyer V, Ciudad M. TET2 gene mutation is a frequent and adverse event in chronic myelomonocytic leukemia. Haematologica. 2009;94(12):1676–1681. doi: 10.3324/haematol.2009.011205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Menotti M, Ambrogio C, Cheong T C. Wiskott-Aldrich syndrome protein (WASP) is a tumor suppressor in T cell lymphoma. Nat Med. 2019;25(01):130–140. doi: 10.1038/s41591-018-0262-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Morin R D, Mendez-Lago M, Mungall A J.Frequent mutation of histone-modifying genes in non-Hodgkin lymphoma Nature 2011476(7360):298–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.da Silva Almeida A C, Abate F, Khiabanian H. The mutational landscape of cutaneous T cell lymphoma and Sézary syndrome. Nat Genet. 2015;47(12):1465–1470. doi: 10.1038/ng.3442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Rabello D DA, Ferreira V DDS, Berzoti-Coelho M G. MLL2/KMT2D and MLL3/KMT2C expression correlates with disease progression and response to imatinib mesylate in chronic myeloid leukemia . Cancer Cell Int. 2018;18:26. doi: 10.1186/s12935-018-0523-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Sahm F, Jakobiec F A, Meyer J. Somatic mutations of DICER1 and KMT2D are frequent in intraocular medulloepitheliomas. Genes Chromosomes Cancer. 2016;55(05):418–427. doi: 10.1002/gcc.22344. [DOI] [PubMed] [Google Scholar]
- 96.Augert A, Zhang Q, Bates B. Small cell lung cancer exhibits frequent inactivating mutations in the histone methyltransferase KMT2D/MLL2: CALGB 151111 (Alliance) J Thorac Oncol. 2017;12(04):704–713. doi: 10.1016/j.jtho.2016.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Sun P, Wu T, Sun X. KMT2D inhibits the growth and metastasis of bladder cancer cells by maintaining the tumor suppressor genes. Biomed Pharmacother. 2019;115:108924. doi: 10.1016/j.biopha.2019.108924. [DOI] [PubMed] [Google Scholar]
- 98.Ding B, Yan L, Zhang Y. Analysis of the role of mutations in the KMT2D histone lysine methyltransferase in bladder cancer. FEBS Open Bio. 2019;9(04):693–706. doi: 10.1002/2211-5463.12600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Ardeshir-Larijani F, Bhateja P, Lipka M B, Sharma N, Fu P, Dowlati A. KMT2D mutation is associated with poor prognosis in non-small-cell lung cancer. Clin Lung Cancer. 2018;19(04):e489–e501. doi: 10.1016/j.cllc.2018.03.005. [DOI] [PubMed] [Google Scholar]
- 100.Ng S B, Bigham A W, Buckingham K J. Exome sequencing identifies MLL2 mutations as a cause of Kabuki syndrome. Nat Genet. 2010;42(09):790–793. doi: 10.1038/ng.646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Cheon C K, Ko J M. Kabuki syndrome: clinical and molecular characteristics. Korean J Pediatr. 2015;58(09):317–324. doi: 10.3345/kjp.2015.58.9.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Yap K L, Johnson A EK, Fischer D. Congenital hyperinsulinism as the presenting feature of Kabuki syndrome: clinical and molecular characterization of 9 affected individuals. Genet Med. 2019;21(01):233–242. doi: 10.1038/s41436-018-0013-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Kurahashi N, Miyake N, Mizuno S. Characteristics of epilepsy in patients with Kabuki syndrome with KMT2D mutations. Brain Dev. 2017;39(08):672–677. doi: 10.1016/j.braindev.2017.03.025. [DOI] [PubMed] [Google Scholar]
- 104.Scala M, Morana G, Sementa A R. Aggressive desmoid fibromatosis in Kabuki syndrome: expanding the tumor spectrum. Pediatr Blood Cancer. 2019;66(09):e27831. doi: 10.1002/pbc.27831. [DOI] [PubMed] [Google Scholar]
- 105.Margot H, Boursier G, Duflos C. Immunopathological manifestations in Kabuki syndrome: a registry study of 177 individuals. Genet Med. 2020;22(01):181–188. doi: 10.1038/s41436-019-0623-x. [DOI] [PubMed] [Google Scholar]
- 106.Arsov T, Sestan M, Cekada N. Systemic lupus erythematosus: a new autoimmune disorder in Kabuki syndrome. Eur J Med Genet. 2019;62(06):103538. doi: 10.1016/j.ejmg.2018.09.005. [DOI] [PubMed] [Google Scholar]
- 107.Porntaveetus T, Abid M F, Theerapanon T. Expanding the oro-dental and mutational spectra of Kabuki Syndrome and expression of KMT2D and KDM6A in human tooth germs. Int J Biol Sci. 2018;14(04):381–389. doi: 10.7150/ijbs.23517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Herz H M. Enhancer deregulation in cancer and other diseases. BioEssays. 2016;38(10):1003–1015. doi: 10.1002/bies.201600106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Sullivan K E, Mullen C A, Blaese R M, Winkelstein J A.A multiinstitutional survey of the Wiskott-Aldrich syndrome J Pediatr 1994125(6 Pt 1):876–885. [DOI] [PubMed] [Google Scholar]
- 110.Thrasher A J, Burns S O. WASP: a key immunological multitasker. Nat Rev Immunol. 2010;10(03):182–192. doi: 10.1038/nri2724. [DOI] [PubMed] [Google Scholar]
- 111.Rivers E, Thrasher A J. Wiskott-Aldrich syndrome protein: emerging mechanisms in immunity. Eur J Immunol. 2017;47(11):1857–1866. doi: 10.1002/eji.201646715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.MacCarthy-Morrogh L, Gaspar H B, Wang Y C. Absence of expression of the Wiskott-Aldrich syndrome protein in peripheral blood cells of Wiskott-Aldrich syndrome patients. Clin Immunol Immunopathol. 1998;88(01):22–27. doi: 10.1006/clin.1998.4557. [DOI] [PubMed] [Google Scholar]
- 113.Candotti F. Clinical manifestations and pathophysiological mechanisms of the Wiskott-Aldrich Syndrome. J Clin Immunol. 2018;38(01):13–27. doi: 10.1007/s10875-017-0453-z. [DOI] [PubMed] [Google Scholar]
- 114.Marangoni F, Trifari S, Scaramuzza S. WASP regulates suppressor activity of human and murine CD4(+)CD25(+)FOXP3(+) natural regulatory T cells. J Exp Med. 2007;204(02):369–380. doi: 10.1084/jem.20061334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Ohya T, Yanagimachi M, Iwasawa K. Childhood-onset inflammatory bowel diseases associated with mutation of Wiskott-Aldrich syndrome protein gene. World J Gastroenterol. 2017;23(48):8544–8552. doi: 10.3748/wjg.v23.i48.8544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Bouma G, Carter N A, Recher M. Exacerbated experimental arthritis in Wiskott-Aldrich syndrome protein deficiency: modulatory role of regulatory B cells. Eur J Immunol. 2014;44(09):2692–2702. doi: 10.1002/eji.201344245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Huang G Z, Lo Y L. Correlation between acetylcholine receptor antibody levels and thymic pathology in myasthenia gravis: a review. J Clin Neuromuscul Dis. 2013;14(04):209–217. doi: 10.1097/CND.0b013e31828a0090. [DOI] [PubMed] [Google Scholar]
- 118.Cork S M, Kaur B, Devi N S. A proprotein convertase/MMP-14 proteolytic cascade releases a novel 40 kDa vasculostatin from tumor suppressor BAI1. Oncogene. 2012;31(50):5144–5152. doi: 10.1038/onc.2012.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Kaur B, Cork S M, Sandberg E M. Vasculostatin inhibits intracranial glioma growth and negatively regulates in vivo angiogenesis through a CD36-dependent mechanism. Cancer Res. 2009;69(03):1212–1220. doi: 10.1158/0008-5472.CAN-08-1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Soh R YZ, Lim J P, Samy R P, Chua P J, Bay B H. A-kinase anchor protein 12 (AKAP12) inhibits cell migration in breast cancer. Exp Mol Pathol. 2018;105(03):364–370. doi: 10.1016/j.yexmp.2018.10.010. [DOI] [PubMed] [Google Scholar]
- 121.Bortlik M, Vitkova I, Papezova M. Deficiency of adenomatous polyposis coli protein in sporadic colorectal adenomas and its associations with clinical phenotype and histology. World J Gastroenterol. 2006;12(24):3901–3905. doi: 10.3748/wjg.v12.i24.3901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Carson D J, Santoro I M, Groden J. Isoforms of the APC tumor suppressor and their ability to inhibit cell growth and tumorigenicity. Oncogene. 2004;23(42):7144–7148. doi: 10.1038/sj.onc.1207954. [DOI] [PubMed] [Google Scholar]
- 123.Daly C S, Shaw P, Ordonez L D. Functional redundancy between Apc and Apc2 regulates tissue homeostasis and prevents tumorigenesis in murine mammary epithelium. Oncogene. 2017;36(13):1793–1803. doi: 10.1038/onc.2016.342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Ying X, Li-ya Q, Feng Z, Yin W, Ji-hong L. MiR-939 promotes the proliferation of human ovarian cancer cells by repressing APC2 expression. Biomed Pharmacother. 2015;71:64–69. doi: 10.1016/j.biopha.2015.02.020. [DOI] [PubMed] [Google Scholar]
- 125.Tiberi L, Bonnefont J, van den Ameele J. A BCL6/BCOR/SIRT1 complex triggers neurogenesis and suppresses medulloblastoma by repressing Sonic Hedgehog signaling. Cancer Cell. 2014;26(06):797–812. doi: 10.1016/j.ccell.2014.10.021. [DOI] [PubMed] [Google Scholar]
- 126.Dragon-Durey M A, Quartier P, Frémeaux-Bacchi V. Molecular basis of a selective C1s deficiency associated with early onset multiple autoimmune diseases. J Immunol. 2001;166(12):7612–7616. doi: 10.4049/jimmunol.166.12.7612. [DOI] [PubMed] [Google Scholar]
- 127.Ohno K, Tsujino A, Brengman J M. Choline acetyltransferase mutations cause myasthenic syndrome associated with episodic apnea in humans. Proc Natl Acad Sci U S A. 2001;98(04):2017–2022. doi: 10.1073/pnas.98.4.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Lokki M L, Circolo A, Ahokas P, Rupert K L, Yu C Y, Colten H R. Deficiency of human complement protein C4 due to identical frameshift mutations in the C4A and C4B genes. J Immunol. 1999;162(06):3687–3693. [PubMed] [Google Scholar]
- 129.Nyberg P, Xie L, Sugimoto H. Characterization of the anti-angiogenic properties of arresten, an alpha1beta1 integrin-dependent collagen-derived tumor suppressor. Exp Cell Res. 2008;314(18):3292–3305. doi: 10.1016/j.yexcr.2008.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Shaikh S, Shettigar S KG, Kumar S, Kantharia S, Kurva J, Cherian S. Novel mutation in Cul7 gene in a family diagnosed with 3M syndrome . J Genet. 2019;98:21. [PubMed] [Google Scholar]
- 131.Hedrick L, Cho K R, Fearon E R, Wu T C, Kinzler K W, Vogelstein B. The DCC gene product in cellular differentiation and colorectal tumorigenesis. Genes Dev. 1994;8(10):1174–1183. doi: 10.1101/gad.8.10.1174. [DOI] [PubMed] [Google Scholar]
- 132.Mollenhauer J, Wiemann S, Scheurlen W. DMBT1, a new member of the SRCR superfamily, on chromosome 10q25.3-26.1 is deleted in malignant brain tumours. Nat Genet. 1997;17(01):32–39. doi: 10.1038/ng0997-32. [DOI] [PubMed] [Google Scholar]
- 133.Takeshita H, Sato M, Shiwaku H O. Expression of the DMBT1 gene is frequently suppressed in human lung cancer. Jpn J Cancer Res. 1999;90(09):903–908. doi: 10.1111/j.1349-7006.1999.tb00833.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Baldari U, Raccagni A A, Celli B, Righini M G. Chronic bullous disease of childhood following Epstein-Barr virus seroconversion: a case report. Clin Exp Dermatol. 1996;21(02):123–126. [PubMed] [Google Scholar]
- 135.Sugi T, Hashimoto T, Hibi T, Nishikawa T. Production of human monoclonal anti-basement membrane zone (BMZ) antibodies from a patient with bullous pemphigoid (BP) by Epstein-Barr virus transformation. Analyses of the heterogeneity of anti-BMZ antibodies in BP sera using them. J Clin Invest. 1989;84(04):1050–1055. doi: 10.1172/JCI114266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Huang F Y, Wong D K, Tsui V W. Targeted genomic profiling identifies frequent deleterious mutations in FAT4 and TP53 genes in HBV-associated hepatocellular carcinoma. BMC Cancer. 2019;19(01):789. doi: 10.1186/s12885-019-6002-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Sun H, Zhou H, Zhang Y. Aberrant methylation of FAT4 and SOX11 in peripheral blood leukocytes and their association with gastric cancer risk . J Cancer. 2018;9(13):2275–2283. doi: 10.7150/jca.24797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Lu Y J, Wu C S, Li H P. Aberrant methylation impairs low density lipoprotein receptor-related protein 1B tumor suppressor function in gastric cancer. Genes Chromosomes Cancer. 2010;49(05):412–424. doi: 10.1002/gcc.20752. [DOI] [PubMed] [Google Scholar]
- 139.Abuzzahab M J, Schneider A, Goddard A. IGF-I receptor mutations resulting in intrauterine and postnatal growth retardation. N Engl J Med. 2003;349(23):2211–2222. doi: 10.1056/NEJMoa010107. [DOI] [PubMed] [Google Scholar]
- 140.Longo N, Wang Y, Pasquali M. Progressive decline in insulin levels in Rabson-Mendenhall syndrome. J Clin Endocrinol Metab. 1999;84(08):2623–2629. doi: 10.1210/jcem.84.8.5902. [DOI] [PubMed] [Google Scholar]
- 141.Kanatsuna N, Delli A, Andersson C. Doubly reactive INS-IGF2 autoantibodies in children with newly diagnosed autoimmune (type 1) diabetes. Scand J Immunol. 2015;82(04):361–369. doi: 10.1111/sji.12325. [DOI] [PubMed] [Google Scholar]
- 142.Tanokashira D, Fukuokaya W, Taguchi A. Involvement of insulin receptor substrates in cognitive impairment and Alzheimer's disease. Neural Regen Res. 2019;14(08):1330–1334. doi: 10.4103/1673-5374.253535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Norquay L D, D'Aquino K E, Opare-Addo L M. Insulin receptor substrate-2 in beta-cells decreases diabetes in nonobese diabetic mice. Endocrinology. 2009;150(10):4531–4540. doi: 10.1210/en.2009-0395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Arai T, Hashimoto H, Kawai K. Fulminant type 1 diabetes mellitus observed in insulin receptor substrate 2 deficient mice. Clin Exp Med. 2008;8(02):93–99. doi: 10.1007/s10238-008-0163-1. [DOI] [PubMed] [Google Scholar]
- 145.Vallianatos C N, Iwase S. Disrupted intricacy of histone H3K4 methylation in neurodevelopmental disorders. Epigenomics. 2015;7(03):503–519. doi: 10.2217/epi.15.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Dai B, Huang H, Guan F. Histone demethylase KDM5A inhibits glioma cells migration and invasion by down regulating ZEB1. Biomed Pharmacother. 2018;99:72–80. doi: 10.1016/j.biopha.2018.01.020. [DOI] [PubMed] [Google Scholar]
- 147.Gaidamakov S, Maximova O A, Chon H. Targeted deletion of the gene encoding the La autoantigen (Sjögren's syndrome antigen B) in B cells or the frontal brain causes extensive tissue loss. Mol Cell Biol. 2014;34(01):123–131. doi: 10.1128/MCB.01010-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Cam J A, Zerbinatti C V, Knisely J M, Hecimovic S, Li Y, Bu G. The low density lipoprotein receptor-related protein 1B retains beta-amyloid precursor protein at the cell surface and reduces amyloid-beta peptide production. J Biol Chem. 2004;279(28):29639–29646. doi: 10.1074/jbc.M313893200. [DOI] [PubMed] [Google Scholar]
- 149.Herrendorff R, Hänggi P, Pfister H. Selective in vivo removal of pathogenic anti-MAG autoantibodies, an antigen-specific treatment option for anti-MAG neuropathy. Proc Natl Acad Sci U S A. 2017;114(18):E3689–E3698. doi: 10.1073/pnas.1619386114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Ramanathan S, Dale R C, Brilot F. Anti-MOG antibody: the history, clinical phenotype, and pathogenicity of a serum biomarker for demyelination. Autoimmun Rev. 2016;15(04):307–324. doi: 10.1016/j.autrev.2015.12.004. [DOI] [PubMed] [Google Scholar]
- 151.Duncan G J, Plemel J R, Assinck P. Myelin regulatory factor drives remyelination in multiple sclerosis. Acta Neuropathol. 2017;134(03):403–422. doi: 10.1007/s00401-017-1741-7. [DOI] [PubMed] [Google Scholar]
- 152.Shi Y, Shao Q, Li Z. Myt1L promotes differentiation of oligodendrocyte precursor cells and is necessary for remyelination after lysolecithin-induced demyelination. Neurosci Bull. 2018;34(02):247–260. doi: 10.1007/s12264-018-0207-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Sowerby J M, Thomas D C, Clare S. NBEAL2 is required for neutrophil and NK cell function and pathogen defense. J Clin Invest. 2017;127(09):3521–3526. doi: 10.1172/JCI91684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Abramowicz A, Gos M. Neurofibromin in neurofibromatosis type 1—mutations in NF1gene as a cause of disease. Dev Period Med. 2014;18(03):297–306. [PubMed] [Google Scholar]
- 155.Li D, Yuan H, Ortiz-Gonzalez X R. GRIN2D recurrent de novo dominant mutation causes a severe epileptic encephalopathy treatable with NMDA receptor channel blockers. Am J Hum Genet. 2016;99(04):802–816. doi: 10.1016/j.ajhg.2016.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Grogan A, Kontrogianni-Konstantopoulos A. Unraveling obscurins in heart disease. Pflugers Arch. 2019;471(05):735–743. doi: 10.1007/s00424-018-2191-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Schneppenheim R, Frühwald M C, Gesk S. Germline nonsense mutation and somatic inactivation of SMARCA4/BRG1 in a family with rhabdoid tumor predisposition syndrome. Am J Hum Genet. 2010;86(02):279–284. doi: 10.1016/j.ajhg.2010.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Tomsic J, He H, Akagi K. A germline mutation in SRRM2, a splicing factor gene, is implicated in papillary thyroid carcinoma predisposition. Sci Rep. 2015;5:10566. doi: 10.1038/srep10566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Shehadeh L A, Yu K, Wang L. SRRM2, a potential blood biomarker revealing high alternative splicing in Parkinson's disease. PLoS One. 2010;5(02):e9104. doi: 10.1371/journal.pone.0009104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Ching Y P, Wong C M, Chan S F. Deleted in liver cancer (DLC) 2 encodes a RhoGAP protein with growth suppressor function and is underexpressed in hepatocellular carcinoma. J Biol Chem. 2003;278(12):10824–10830. doi: 10.1074/jbc.M208310200. [DOI] [PubMed] [Google Scholar]
- 161.Rashad N M, El-Shabrawy R M, Said D, El-Shabrawy S M, Emad G. Serum levels of transforming growth factor beta -1 (TGF-β1) as an early no invasive marker for diagnosis of lupus nephritis in systemic lupus erythematosus patients. Egypt J Immunol. 2019;26(01):31–42. [PubMed] [Google Scholar]
- 162.Pérez-Serra A, Toro R, Sarquella-Brugada G. Genetic basis of dilated cardiomyopathy. Int J Cardiol. 2016;224:461–472. doi: 10.1016/j.ijcard.2016.09.068. [DOI] [PubMed] [Google Scholar]
- 163.Jiang X, Detera-Wadleigh S D, Akula N. Sodium valproate rescues expression of TRANK1 in iPSC-derived neural cells that carry a genetic variant associated with serious mental illness. Mol Psychiatry. 2019;24(04):613–624. doi: 10.1038/s41380-018-0207-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Miyanaga K, Kato Y, Nakamura T.Expression and role of thrombospondin-1 in colorectal cancer Anticancer Res 200222(6C):3941–3948. [PubMed] [Google Scholar]
- 165.Tardif S, Cormier N. Role of zonadhesin during sperm-egg interaction: a species-specific acrosomal molecule with multiple functions. Mol Hum Reprod. 2011;17(11):661–668. doi: 10.1093/molehr/gar039. [DOI] [PubMed] [Google Scholar]
- 166.Ghosh A K, Steele R, Ray R B. Carboxyl-terminal repressor domain of MBP-1 is sufficient for regression of prostate tumor growth in nude mice. Cancer Res. 2005;65(03):718–721. [PubMed] [Google Scholar]
- 167.Ghosh A K, Steele R, Ryerse J, Ray R B. Tumor-suppressive effects of MBP-1 in non-small cell lung cancer cells. Cancer Res. 2006;66(24):11907–11912. doi: 10.1158/0008-5472.CAN-06-2754. [DOI] [PubMed] [Google Scholar]
- 168.Kanduc D, Shoenfeld Y. Inter-pathogen peptide sharing and the original antigenic sin: solving a paradox. Open Immunol J. 2018;8:16–27. [Google Scholar]
- 169.Cohn M. Two unresolved problems facing models of the self-nonself discrimination. J Theor Biol. 2015;387:31–38. doi: 10.1016/j.jtbi.2015.09.021. [DOI] [PubMed] [Google Scholar]
- 170.Rose N R. Negative selection, epitope mimicry and autoimmunity. Curr Opin Immunol. 2017;49:51–55. doi: 10.1016/j.coi.2017.08.014. [DOI] [PubMed] [Google Scholar]
- 171.Rose N R. Learning from myocarditis: mimicry, chaos and black holes. F1000Prime Rep. 2014;6:25. doi: 10.12703/P6-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Kanduc D. From hepatitis C virus immunoproteomics to rheumatology via cross-reactivity in one table. Curr Opin Rheumatol. 2019;31(05):488–492. doi: 10.1097/BOR.0000000000000606. [DOI] [PubMed] [Google Scholar]
- 173.Kanduc D, Shoenfeld Y.Human papillomavirus epitope mimicry and autoimmunity: the molecular truth of peptide sharing Pathobiology 201986(5–6):285–295. [DOI] [PubMed] [Google Scholar]
- 174.Kanduc D. HCV: written in our DNA. Self Nonself. 2011;2(02):108–113. doi: 10.4161/self.2.2.15795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Kanduc D. The self/nonself issue: a confrontation between proteomes. Self Nonself. 2010;1(03):255–258. doi: 10.4161/self.1.3.11897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Kanduc D. Immunogenicity, immunopathogenicity, and immunotolerance in one graph. Anticancer Agents Med Chem. 2015;15(10):1264–1268. doi: 10.2174/1871520615666150716105543. [DOI] [PubMed] [Google Scholar]
- 177.Ray S K, Putterman C, Diamond B. Pathogenic autoantibodies are routinely generated during the response to foreign antigen: a paradigm for autoimmune disease. Proc Natl Acad Sci U S A. 1996;93(05):2019–2024. doi: 10.1073/pnas.93.5.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Ruiz J T, Luján L, Blank M, Shoenfeld Y. Adjuvants- and vaccines-induced autoimmunity: animal models. Immunol Res. 2017;65(01):55–65. doi: 10.1007/s12026-016-8819-5. [DOI] [PubMed] [Google Scholar]
- 179.Whitton J L, Fujinami R S. Viruses as triggers of autoimmunity: facts and fantasies. Curr Opin Microbiol. 1999;2(04):392–397. doi: 10.1016/s1369-5274(99)80069-1. [DOI] [PubMed] [Google Scholar]
- 180.Kanduc D. The comparative biochemistry of viruses and humans: an evolutionary path towards autoimmunity. Biol Chem. 2019;400(05):629–638. doi: 10.1515/hsz-2018-0271. [DOI] [PubMed] [Google Scholar]
- 181.Kanduc D, Lucchese A, Mittelman A. Non-redundant peptidomes from DAPs: towards “the vaccine”? Autoimmun Rev. 2007;6(05):290–294. doi: 10.1016/j.autrev.2006.09.004. [DOI] [PubMed] [Google Scholar]
- 182.Kanduc D. Peptide cross-reactivity: the original sin of vaccines. Front Biosci (Schol Ed) 2012;4:1393–1401. doi: 10.2741/s341. [DOI] [PubMed] [Google Scholar]
- 183.Kanduc D, Shoenfeld Y. From HBV to HPV: designing vaccines for extensive and intensive vaccination campaigns worldwide. Autoimmun Rev. 2016;15(11):1054–1061. doi: 10.1016/j.autrev.2016.07.030. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


