Abstract
The new coronavirus, SARS-CoV-2, has spread internationally and whilst the current focus of those dealing with the COVID-19 pandemic is understandably restricting its direct transmission, the potential for secondary transmission via wastewater should not be underestimated. The virus has been identified in human fecal and wastewater samples from different countries and potential cases of transmission via wastewater have been reported. Our recommendations for hospital wastewater treatment, municipal wastewater plants, sewage sludge, water reuse and aquatic environments are designed to reduce the risk of such transmission, and contribute to limiting the resurgence of COVID-19 as current restrictions are relaxed. A particular urgent recommendation focusses on supporting low-income countries in tackling the potential for secondary transmission via wastewater.
Keywords: SARS-CoV-2, COVID-19, Wastewater, Secondary transmission, Low-income countries
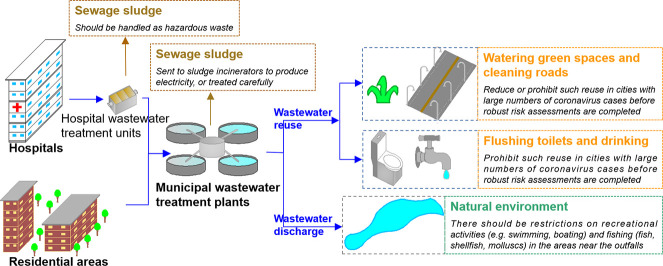
Graphical abstract
1. Introduction
Effective water, sanitation, waste and wastewater management are important for public health. This has been highlighted during the ongoing COVID-19 pandemic (World Health Organization and the United Nations Children's Fund (WHO and UNICEF), 2020a, World Health Organization and the United Nations Children's Fund (WHO and UNICEF), 2020b; World Bank, 2020). As of 16 August 2020, the number of confirmed cases of the novel coronavirus, SARS-CoV-2, has risen to a global total of 21.29 million (WHO, 2020a). The primary modes of the virus transmission are through respiratory droplets and direct or indirect contact (Li and Gao, 2020). However, a particular concern in managing the current pandemic is potential secondary transmission of SARS-CoV-2 via wastewater.
SARS-CoV-2 and its sequence have been identified and isolated in human fecal samples (Chinese Center for Disease Control and Prevention, 2020; Guan et al., 2020; Holshue et al., 2020; Wang et al., 2020a). To date, the virus has been detected in wastewater in Australia, China, France, Japan, Italy, Spain, the Netherlands, and the United States of America and Turkey (see Table 1 ). The potential for onward transmission of SARS-CoV-2 via human waste has been demonstrated via a case reported from Guangzhou, China. Here several individuals from different households became infected via wastewater leaking from a broken sewer from the apartment of a confirmed patient with whom they had no other contact (Guangzhou Center for Disease Control and Prevention, 2020). As the virus has spread, to now over 200 countries, territories and areas (WHO, 2020a), many more cases can be expected in low-income countries with weaker health and waste management systems. This increases our concerns regarding potential further escalation of the crisis and the need to recognize the importance of wastewater management in tackling COVID-19.
Table 1.
Recent work of detection of SARS-CoV-2 in wastewater.
| Sampling site | Sampling time | Sample | Positive/total samples | Concentration range for positive samples (gene copies/L) | Availiable online | References |
|---|---|---|---|---|---|---|
| Brisbane, Australia | 24/02/2020–01/04/2020 | Untreated wastewater (M) | 2/9 | 1.9 × 101–1.2 × 102 | 18/04/2020 (Pub) | Ahmed et al. (2020) |
| Zhejiang, China | 19/02/2020–24/02/2020 | Untreated wastewater (H) | 3/3 | / | 24/04/2020 (Pub) | Wang et al. (2020b) |
| Treated by preprocessing disinfection (H) | 1/1 | / | ||||
| Final effluent (H) | 0/1 | / | ||||
| Valencia, Spain | 12/03/2020–14/04/2020 | Untreated wastewater (M) | 35/42 | 1.4 × 105–3.4 × 105 | 16/05/2020 (Pub) | Randazzo et al. (2020) |
| Secondary Treated (M) | 2/18 | <2.5 × 105 | ||||
| Tertiary Treated (M) | 0/12 | / | ||||
| Milan and Rome, Italy | 03/02/2020–02/04/2020 | Untreated wastewater (M) | 6/12 | / | 23/05/2020 (Pub) | La Rosa et al. (2020b) |
| Amersfoort, Tilburg, Utrecht, etc., Netherlands | 05/02/2020–25/03/2020 | Untreated wastewater (M) | 20/29 | 2.6 × 103–2.2 × 106 | 20/05/2020 (Pub) | Medema et al. (2020) |
| Yamanashi, Japan | 17/03/2020–07/05/2020 | Untreated wastewater (M) | 0/5 | / | 20/06/2020 (Pub) | Haramoto et al. (2020) |
| Secondary Treated (M) | 1/5 | 2.4 × 103 | ||||
| River water | 0/3 | / | ||||
| Wuhan, China | 26/02/2020–10/03/2020 | Influent of septic tank (H) | 0/4 | / | 23/06/2020 (Pub) | Zhang et al. (2020) |
| Effluent of septic tank (H) | 7/9 | 4.7 × 103–1.7 × 104 | ||||
| Louisiana, USA | 13/01/2020–08/04/2020 | Untreated wastewater (M) | 2/7 | 3.1 × 103–7.5 × 103 | 30/06/2020 (Pub) | Sherchan et al. (2020) |
| Secondary Treated (M) | 0/4 | / | ||||
| Final effluent (M) | 0/4 | / | ||||
| Milano, Italy | 14/04/2020, 22/04/2020 | Untreated wastewater (M) | 4/8 | / | 14/07/2020 (Pub) | Rimoldi et al. (2020) |
| Final effluent (M) | 0/4 | / | ||||
| River water | 4/6 | / | ||||
| Massachusetts, USA | 18/03/2020–25/03/2020 | Untreated wastewater (M) | 10/10 | / | 07/04/2020 (Pre) | Wu et al. (2020) |
| Paris, France | 05/03/2020–23/04/2020 | Untreated wastewater (M) | / | 5.0 × 104–3.0 × 106 | 17/04/2020 (Pre) | Wurtzer et al. (2020) |
| Bozeman, USA | 23/03/2020–13/05/2020 | Untreated wastewater (M) | 10/12 | / | 20/04/2020 (Pre) | Nemudryi et al. (2020) |
| Haifa, Shafdan et c, Israel | 10/03/2020–21/04/2020 | Untreated wastewater (M) | 3/17 | / | 01/05/2020 (Pre) | Bar-Or et al. (2020) |
| Sewer network (H) | 7/9 | |||||
| Istanbul, Turkey | 21/04/2020, 25/04/2020 | Untreated wastewater (M) | 5/7 | 2.9 × 103–1.8 × 104 | 06/05/2020 (Pre) | Kocamemi et al. (2020a) |
| Istanbul, Turkey | 07/05/2020 | Primary sludge (M) | 2/2 | 1.3 × 104–2.3 × 104 | 16/05/2020 (Pre) | Kocamemi et al. (2020b) |
| Waste activated sludge (M) | 7/7 | 1.2 × 104–4.0 × 104 |
M: municipal wastewater; H: hospital wastewater; Pub: published, Pre: preprint.
In order to treat huge, and rapidly growing, numbers of COVID-19 patients, many hospitals and civil buildings have been transformed to infectious disease hospitals with new facilities being constructed over a short period of time (Wang et al., 2020b; Zhang et al., 2020). These tremendous efforts are laudable and necessary in order to control the spread of the virus whilst treating those directly impacted. A concern is whether the wastewater systems of the transformed and new hospitals, as well as municipal wastewater treatment plants, are able to meet the necessary to eradicate the virus and prevent secondary transmission. This is a particular issue in situations where there are large numbers of patients, and consequently large volumes of viral wastewater, and where existing wastewater systems are underdeveloped.
Effective waste management of health care facilities is an often-neglected problem (Harhay et al., 2009; Maina et al., 2019). There are major differences in healthcare waste and wastewater management around the world. Management regulations and standards are, for example, strict in Europe (e.g. Hansen et al., 2014; Nessa et al., 2001), China (Ministry of Ecology and Environment of China, 2005; The State Council, 2011) and the United States of America (Council of State Government, 1992; Nessa et al., 2001). During the early stages of the pandemic, the Ministry of Ecology and Environment of China stressed that hospitals, including those which were upgraded or newly established, should process waste and wastewater according to the established rules and standards (Ministry of Ecology and Environment of China, 2020a, Ministry of Ecology and Environment of China, 2020b). However, healthcare facilities in many less developed countries and regions, including for example much of Africa and South-East Asia, have far less stringent measures in place whilst waste and wastewater infrastructure is often lacking (Nessa et al., 2001).
Globally 2 billion people are without basic sanitation (WHO, 2019), and effective wastewater management is rare in major urban areas of less developed countries (Moe and Rheingans, 2006). An estimated 1.5 billion use medical facilities with no sanitation services (WHO and UNICEF, 2019). In most cases, waste and wastewater from such facilities, including patient's excreta, is not treated safely. As of 16 August 2020, the number of confirmed cases in Africa stands at nearly 1 million (WHO, 2020a), although given the difficulties in obtaining reliable data it could be considerably larger, and there is huge potential for this to increase considerably. In sub-Saharan Africa, 709 million people live without basic sanitation (WHO, 2019), and non-sewered sanitation system are common throughout the region (Street et al., 2020). Furthermore, large populations share toilet facilities with, on average across Sub-Saharan Africa, 33% of urban populations relying on shared sanitation (Rheinländer et al., 2015). At the best of times, poor basic sanitary infrastructure has significant implications for human health (World Bank, 2020) but during a global pandemic, there are significant concerns that it could promote secondary transmission.
2. Viruses in waters and wastewater
It is well known that viruses eliminated by feces can be found in wastewater, and may not be completely removed by conventional secondary treatment of sewage (Carducci et al., 2008; Carducci and Verani, 2013; Wigginton et al., 2015). As a result, they can be released into natural waters and can be bioaccumulated within aquatic species such as shellfish (Farkas et al., 2018). Humans can, in turn, be infected by viruses in natural waters by drinking contaminated water or eating contaminated food as well as by bathing or inhaling bioaerosols from polluted waters (Cook, 2013; Rodríguez-Lázaro et al., 2012). Decline in viral load within aquatic environments depends upon the time since their release, the viral resistance to natural and artificial disinfection factors, as well as dilution. In contrast to the majority of enteric viruses normally found in wastewaters, coronaviruses are enveloped and are considered less resistant in the environment (Wigginton et al., 2015; Ye et al., 2016).
Although waterborne transmission was not considered a concern during the 2003 SARS epidemic, the potential for transmission via toilet systems was recognized in Hong Kong (Yu et al., 2004). It was also suggested in a recent study on SARS-COV-2 environmental monitoring in Singapore (Ong et al., 2020), where positive surface samples were found from exhaust air outlets, although air samples were negative. Studies of coronavirus survival in sewage and water have usually been undertaken using surrogates. These have demonstrated persistence from days to weeks depending on the surrogate virus, type of water and temperature (Casanova et al., 2009; Gundy et al., 2009). An experimental study showed that SARS-CoV persistence of infectivity was only 2 days at 20 °C, but 14 days at 4 °C (Wang et al., 2005). Studies of coronavirus resistance in fresh produce (lettuce and strawberries) have also been carried out with results suggesting persistence of some days at low temperatures (Mullis et al., 2012; Yépiz-Gómez et al., 2013).
Although studies on coronavirus presence and persistence in sewage and natural waters are growing daily, knowledge is still relatively scarce (Carducci et al., 2020). However, as stated above, SARS-CoV-2 has been identified in wastewater samples from different countries (Table 1). The potential exists, therefore, for secondary transmission of COVID-19 via wastewater systems. This possibility has been debated in reviews and commentaries (Amirian, 2020; La Rosa et al., 2020a) with the first potential case now being reported (Guangzhou Center for Disease Control and Prevention, 2020). In the meantime, the WHO has recommended “safely managing water and sanitation services and applying good hygiene practices” in order to prevent infection (WHO and UNICEF, 2020b). The following sections provide recommendations for reducing the risk of transmission via wastewater, and thereby contributing to limiting the resurgence of COVID-19 as current restrictions are relaxed.
3. Hospital wastewater treatment
The wastewater systems of hospitals treating COVID-19 patients, including the collection and transport subsystems, wastewater treatment units and disinfection methods (e.g. chlorine, ClO2, sodium hypochlorite, O3 or UV) must be built and operated in line with strict standards for infectious disease hospitals. Chlorine-based disinfectants are strong oxidizers and are commonly used for hospital wastewater disinfection due to their high inactivation efficiency and relatively low cost (How et al., 2017; Ma et al., 2010). Sodium hypochlorite has been used as a disinfectant in the Cabin Fangcang temporary hospital created in Wuhan's stadium and designated for COVID-19 patients (Zhang et al., 2020). Meanwhile, enhanced maintenance of infrastructure, including pipe and sewer system, should be undertaken to avoid wastewater leaks. Regular and robust monitoring of all wastewater systems should be in place. Oversight of monitoring by environmental authorities will limit opportunities for manipulating data in cases where systems do not meet the required standards.
If the wastewater systems of COVID-19 inpatient wards within a regular hospital that has been upgraded in response to the ongoing coronavirus outbreak is not separate from other wastewater systems, fecal material could be first disinfected on-site using sodium hypochlorite. Coronavirus is sensitive to temperature (Li and Gao, 2020; Wang et al., 2005) with the persistence of infectivity extending under low temperature conditions (Wang et al., 2005). In accordance with the adoption of precautionary principles, and especially in hospitals located in middle to high latitudes, increasing the temperature of wastewater treatment by 5–10 °C in winter or other cold periods as a temporary measure would be desirable. According to the actual conditions of each hospital, this could be achieved using electrical or steam heating of equipment. After China's new environmental law came into effect in 2016 (Liu, 2015), civil coal burning boilers have been prohibited in many cities. Given the pressing need to address the coronavirus emergency, local authorities should provide temporary exemptions for coal boilers being used in hospital. Similar temporary relaxation of such regulations is recommended in other countries where short-term declines in air quality could be countenanced in the face of COVID-19. Meanwhile, given the presence of vapor from warm wastewater, the operators of treatment facilities should wear personal protective equipment.
Where current infrastructure is poor, such as in low-income countries, and where complete wastewater treatment systems cannot be built in a short time, the use of mobile treatment facilities with disinfection devices could be considered. Rural solar toilets (Moe and Izurieta, 2003; Oswald et al., 2009) may be an appropriate choice in low-income countries. They can achieve temperatures up to 44 °C which can help in the removal of pathogens (Moe and Izurieta, 2003). If these options are not available, inspired by the common approach of disposing of waste in sanitary landfills (Zamorano et al., 2007), treating fecal material with cheap but effective disinfectants, such as sodium hypochlorite, and then storing and burying (or covering) them with soil could be an alternative. This should, however, only be done at carefully controlled sites that include anti-seepage measures. The key rule should be to prohibit the virus from entering the natural environment via healthcare wastewater.
4. Municipal wastewater treatment plants, sewage sludge and water reuse
Municipal wastewater treatment plants receive wastewater from residential areas, office buildings, education institutions, factories, and hospitals. In these plants the water is treated before being discharged to the environment. However, these plants are not designed specifically to treat hospital wastewater, and should therefore strengthen their disinfection procedures using chlorine, ClO2, sodium hypochlorite, O3 or UV treatments during the current period.
Viruses survive longer with suspended particles within wastewater (Gundy et al., 2009). Some of these suspended particles eventually settle in sewage sludge. As a result, sewage sludge from hospitals treating coronavirus should be handled as hazardous waste. For the same reasons, during this period sewage sludge from municipal wastewater plants in cities which have large numbers of coronavirus cases, should, if not used within sludge incinerators to produce electricity, be buried in carefully regulated landfill sites. The use of this sewage sludge as a fertilizer should be prohibited.
Water discharged from municipal wastewater plants in many cities and elsewhere is often reused for watering green spaces (tree, shrubs and grassland), cleaning roads and flushing toilets. In some cases, such as in Singapore, it is even used for drinking (Tortajada and van Rensburg, 2020). We suggest that during the current period, governments should reduce or prohibit such reuse of waste water for watering and cleaning, and prohibit its use for flushing toilets and drinking in cities with large number of coronavirus cases until robust risk assessments focusing on the potential for secondary transmission have been undertaken.
5. Aquatic environments
Discharge of wastewater to recreational waters was recently suggested as a potential transmission pathway for the novel coronavirus (Cahill and Morris, 2020). Where wastewater is discharged into aquatic environments, there should be restrictions on recreational activities (e.g. swimming, boating, fishing) in areas near to outfalls whilst harvesting of aquatic-based products including fish, shellfish, and molluscs should be curtailed. Given the different stages of the pandemic in different countries, some nations or regions have lifted the restrictions that were imposed to tackle the spread of COVID-19. People who have been locked-down for long periods are often seeking relaxation by rivers, lakes or the sea. Our proposed restrictions should, nevertheless, be implemented and only slowly removed in order to avoid virus transmission and the potential for local resurgence and second waves.
As with population virus-testing, there is also an urgent need to modify and further develop the present analytical methods to quickly identify the novel coronavirus in surface waters, groundwater, tap water, wastewater and sewage sludge, as well as within aquatic animals such as fish and shellfish. Detection in wastewater could assist in refining estimates of the virus's spread at the community level and for providing early warnings (Medema et al., 2020; Street et al., 2020). This will be critical for managing the pandemic especially when extensive human testing is not available. Testing should not only include the presence of the virus but also its potential infectivity. However, there are considerable worldwide variations in the capacities of organizations responsible for wastewater monitoring. Less developed regions, most notably in Africa where our concerns related to poorly developed health and sanitation systems are greatest, are also characterized by relatively limited resources in terms of laboratory equipment and technicians. For example, Schroeder and Amukele (2014) suggested that less that 1% of laboratories met international standards in Kampala, Uganda. There is an important role for international cooperation in improving local capacity in this area. National and regional laboratories in developed countries have started surveillance of SARS-CoV-2 in wastewater (WHO, 2020b). To date, international aid has focused on supporting laboratories in less developed countries in testing human samples (BGI, 2020) and there is a need to expand this support for monitoring SARS-CoV-2 in the environment.
Although the evidence for secondary transmission of COVID-19 via wastewater is currently limited (WHO and UNICEF, 2020a), the case from Guangzhou suggests that it is possible (Guangzhou Center for Disease Control and Prevention, 2020). Future scientific research should focus on the status of the virus in different aquatic environments and food chains with the data being made openly available to the scientific community. These data could support the use of ecological models to simulate the potential spread of SARS-CoV-2 through environments and in the preparation of risk assessments. This would, in turn, aid official decisions and policy making. In addition, the effects of residual chlorine (Zhang et al., 2020) and other disinfectants, which are likely to increase in response to their greater use in treating wastewater during the pandemic, on aquatic ecosystem should be researched.
6. Conclusions
The current focus of the medical and public health experts dealing with the SARS-CoV-2 is understandably restricting its direct transmission and the care of those who are infected. However, the potential for secondary transmission should not be underestimated. Secondary transmission could otherwise damage the hard-won achievements of current transmission control measures and possibly contribute to a resurgence of COVID-19. The potential for secondary transmission is perhaps greater in those low-income that have relatively poorly developed heath, sanitation and wastewater infrastructure, monitoring and policies. International cooperation therefore has a significant role to play in curbing the risks of secondary transmission.
CRediT authorship contribution statement
Dasheng Liu: Conceptualization, Writing - original draft, Writing - review & editing. Julian R. Thompson: Writing - original draft, Writing - review & editing. Annalaura Carducci: Writing - original draft, Writing - review & editing. Xuejun Bi: Writing - review & editing.
Declaration of competing interest
The authors declare no competing financial interest.
Acknowledgments
The work was supported by the Creative Society Project of Shandong Association for Science & Technology. We are grateful to our peer reviewers for their comments. Thanks are also due to the discussions and assistance from Profs. Dong Jinyue and Cock van Oosterhout, and Mr. Meng Fanjin.
Editor: Damia Barcelo
References
- Ahmed W., Angel N., Edson J., Bibby K., Bivins A., O’Brien J.W., Choi P.M., Kitajima M., Simpson S.L., Li J., Tscharke B., Verhagen R., Smith W.J.M., Zaugg J., Dierens L., Hugenholtz P., Thomas K.V., Mueller J.F. First confirmed detection of SARS-CoV-2 in untreated wastewater in Australia: a proof of concept for the wastewater surveillance of COVID-19 in the community. Sci. Total Environ. 2020;728:138764. doi: 10.1016/j.scitotenv.2020.138764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amirian E.S. Potential fecal transmission of SARS-CoV-2: current evidence and implications for public health. Int. J. Infect. Dis. 2020;95:363–370. doi: 10.1016/j.ijid.2020.04.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bar-Or I., Yaniv K., Shagan M., Ozer E., Erster O., Mendelson E., Mannasse B., Shirazi R., Kramarsky-Winter E., Nir O., Abu-Ali H., Ronen Z., Rinott E., Lewis Y., Friedler E.F., Paitan Y., Bitkover E., Berchenko Y., Kushmaro A. Regressing SARS-CoV-2 sewage measurements onto COVID-19 burden in the population: a proof-of-concept for quantitative environmental surveillance. medRxiv 2020.04.26.20073569. 2020 doi: 10.1101/2020.04.26.20073569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BGI BGI to assist Angola government to build “Huo-Yan” laboratories to help fight pandemic. 2020. https://www.genomics.cn/news/info_itemid_5825.html
- Cahill N., Morris D. Recreational waters - a potential transmission route for SARS-CoV-2 to humans? Sci. Total Environ. 2020;740:140122. doi: 10.1016/j.scitotenv.2020.140122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carducci A., Verani M. Effects of bacterial, chemical, physical and meteorological variables on virus removal by a wastewater treatment plant. Food Environ. Virol. 2013;5(1):69–76. doi: 10.1007/s12560-013-9105-5. [DOI] [PubMed] [Google Scholar]
- Carducci A., Morici P., Pizzi F., Battistini R., Rovini E., Verani M. Study of the viral removal efficiency in a urban wastewater treatment plant. Water Sci. Technol. 2008;58(4):893–897. doi: 10.2166/wst.2008.437. [DOI] [PubMed] [Google Scholar]
- Carducci A., Federigi I., Liu D., Thompson J.R., Verani M. Making waves: coronavirus detection, presence and persistence in the water environment: state of the art and knowledge needs for public health. Water Res. 2020;179:115907. doi: 10.1016/j.watres.2020.115907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casanova L., Rutala W.A., Weber D.J., Sobsey M.D. Survival of surrogate coronaviruses in water. Water Res. 2009;43(7):1893–1898. doi: 10.1016/j.watres.2009.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chinese Center for Disease Control and Prevention The novel coronavirus are isolated in human fecal samples. 2020. http://www.chinacdc.cn/yw_9324/202002/t20200214_212635.html
- Cook N. Woodhead Publishing; UK: 2013. Viruses in Food and Water: Risks, Surveillance and Control. [Google Scholar]
- Council of State Governments Model guidelines for state medical waste management. 1992. https://www.epa.gov/sites/production/files/2016-02/documents/model_guidelines_for_state_medical_waste_management.pdf
- Farkas K., Cooper D.M., McDonald J.E., Malham S.K., de Rougemont A., Jones D.L. Seasonal and spatial dynamics of enteric viruses in wastewater and in riverine and estuarine receiving waters. Sci. Total Environ. 2018;634:1174–1183. doi: 10.1016/j.scitotenv.2018.04.038. [DOI] [PubMed] [Google Scholar]
- Guan W., Ni Z., Hu Y., Liang W., Ou C., He J., Liu L., Shan H., Lei C., Hui D., Du B., Li L., Zeng G., Yuen K., Chen R., Tang C., Wang T., Chen P., Xiang J., Li S., Wang J., Liang Z., Peng Y., Wei L., Liu Y., Hu Y., Peng P., Wang J., Liu J., Chen Z., Li G., Zheng Z., Qiu S., Luo J., Ye C., Zhu S., Zhong N. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guangzhou Center for Disease Control and Prevention Guangzhou 125th news conference of COVID-19 Control and Prevention on 12 June 2020 organized by Guangzhou Information Office. 2020. http://special.gznews.gov.cn/2020/node_5914/index.shtml
- Gundy P.M., Gerba C.P., Pepper I.L. Survival of coronaviruses in water and wastewater. Food Environ. Virol. 2009;1(1):10. doi: 10.1007/s12560-008-9001-6. [DOI] [Google Scholar]
- Hansen D., Mikloweit U., Ross B., Popp W. Healthcare waste management in Germany. Int. J. Infect. Control. 2014;10(1):1–5. doi: 10.3396/IJIC.v10i1.006.14. [DOI] [Google Scholar]
- Haramoto E., Malla B., Thakali O., Kitajima M. First environmental surveillance for the presence of SARS-CoV-2 RNA in wastewater and river water in Japan. Sci. Total Environ. 2020;737:140405. doi: 10.1016/j.scitotenv.2020.140405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harhay M.O., Halpern S.D., Harhay J.S., Olliaro P.L. Health care waste management: a neglected and growing public health problem worldwide. Tropical Med. Int. Health. 2009;14(11):1414–1417. doi: 10.1111/j.1365-3156.2009.02386.x. [DOI] [PubMed] [Google Scholar]
- Holshue M.L., DeBolt C., Lindquist S., Lofy K.H., Wiesman J., Bruce H., Spitters C., Ericson K., Wilkerson S., Tural A., Diaz G., Cohn A., Fox L., Patel A., Gerber S.I., Kim L., Tong S., Lu X., Lindstrom S., Pallansch M.A., Weldon W.C., Biggs H.M., Uyeki T.M., Pillai S.K. First case of 2019 novel coronavirus in the United States. N. Engl. J. Med. 2020;382(10):929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- How Z.T., Kristiana I., Busetti F., Linge K.L., Joll C.A. Organic chloramines in chlorine-based disinfected water systems: a critical review. J. Environ. Sci. 2017;58:2–18. doi: 10.1016/j.jes.2017.05.025. [DOI] [PubMed] [Google Scholar]
- Kocamemi B.A., Kurt H., Hacıoglu S., Yarali C., Saatci A.M., Pakdemirli B. First data-set on SARS-CoV-2 detection for Istanbul wastewaters in Turkey. MedRxiv 2020.05.03.20089417. 2020 doi: 10.1101/2020.05.03.20089417. [DOI] [Google Scholar]
- Kocamemi B.A., Kurt H., Sait A., Sarac F., Saatci A.M., Pakdemirli B. SARS-CoV-2 detection in Istanbul wastewater treatment plant sludges. medRxiv 2020.05.12.20099358. 2020 doi: 10.1101/2020.05.12.20099358. [DOI] [Google Scholar]
- La Rosa G., Bonadonna L., Lucentini L., Kenmoe S., Suffredini E. Coronavirus in water environments: occurrence, persistence and concentration methods - a scoping review. Water Res. 2020;179:115899. doi: 10.1016/j.watres.2020.115899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- La Rosa G., Iaconelli M., Mancini P., Bonanno Ferraro G., Veneri C., Bonadonna L., Lucentini L., Suffredini E. First detection of SARS-CoV-2 in untreated wastewaters in Italy. Sci. Total Environ. 2020;736:139652. doi: 10.1016/j.scitotenv.2020.139652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X., Gao F. People’s Medical Publishing House; Beijing: 2020. Guidelines of Public Protection for Pneumonia Associated With Novel Coronavirus. [Google Scholar]
- Liu D. New environment law shows its fangs. Nature. 2015;525(7569):321. doi: 10.1038/525321a. [DOI] [PubMed] [Google Scholar]
- Ma Y., Zhao W., Liu H. Application progress of hospital wastewater treatment methods. Occup. Health. 2010;26:1180–1182. doi: 10.13329/j.cnki.zyyjk.2010.10.001. [DOI] [Google Scholar]
- Maina M., Tosas-Auguet O., McKnight J., Zosi M., Kimemia G., Mwaniki P., Hayter A., Montgomery M., Schultsz C., English M. Extending the use of the world health organisations’ water sanitation and hygiene assessment tool for surveys in hospitals - from WASH-FIT to WASH-FAST. PLoS One. 2019;14(12) doi: 10.1371/journal.pone.0226548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medema G., Heijnen L., Elsinga G., Italiaander R., Brouwer A. Presence of SARS-Coronavirus-2 RNA in sewage and correlation with reported COVID-19 prevalence in the early stage of the epidemic in the Netherlands. Environ. Sci. Technol. Lett. 2020;7:511–516. doi: 10.1021/acs.estlett.0c00357. [DOI] [PubMed] [Google Scholar]
- Ministry of Ecology and Environment of China Discharge standard of water pollution for medical organization (GB 18466-2005) 2005. http://www.mee.gov.cn/ywgz/fgbz/bz/bzwb/shjbh/swrwpfbz/200601/t20060101_69193.shtml
- Ministry of Ecology and Environment of China Technical proposal for emergency treatment to COVID-19 hospital wastewater (trial implementation) 2020. http://www.mee.gov.cn/xxgk2018/xxgk/xxgk06/202002/t20200201_761163.html
- Ministry of Ecology and Environment of China Technical proposal for emergency treatment to COVID-19 hospital solid waste (trial implementation) 2020. http://www.mee.gov.cn/ywdt/xwfb/202001/t20200129_761043.shtml
- Moe C.L., Izurieta R. Proceedings of the Second International Symposium on Ecological Sanitation, Lubeck, Germany. 2003. Longitudinal study of double vault urine diverting toilets and solar toilets in El Salvador; pp. 295–302. [Google Scholar]
- Moe C.L., Rheingans R.D. Global challenges in water, sanitation and health. J. Water Health. 2006;4(S1):41–57. doi: 10.2166/wh.2006.0043. [DOI] [PubMed] [Google Scholar]
- Mullis L., Saif L.J., Zhang Y., Zhang X., Azevedo M.S.P. Stability of bovine coronavirus on lettuce surfaces under household refrigeration conditions. Food Microbiol. 2012;30:180–186. doi: 10.1016/j.fm.2011.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nemudryi A., Nemudraiam A., Surya K., Wiegand T., Buyukyoruk M., Wilkinson R., Wiedenheft B. Temporal detection and phylogenetic assessment of SARS-CoV-2 in municipal wastewater. medRxiv 2020.04.15.20066746. 2020 doi: 10.1101/2020.04.15.20066746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nessa K., Quaiyum M.A., Barkat-e-Khuda . Center for Health and population Research; Bangladesh: 2001. Waste Management in Healthcare Facilities: A Review. Working paper No. 144, ICDDR, B.http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.565.6826&rep=rep1&type=pdf [Google Scholar]
- Ong S.W.X., Tan Y.K., Chia P.Y., Lee T.H., Ng O.T., Wong M.S.Y., Marimuthu K. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA-J. Am. Med. Assoc. 2020;323(16):1610–1612. doi: 10.1001/jama.2020.3227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oswald W.E., Suntura O., Velasco M., Caravati K., Moe C.L. Proceedings of the International Water Association 1st Development Congress: Water and Sanitation Services: What works for Developing Countries, Mexico. 2009. Dry sanitation design and delivery innovations for rural, urban, and emergency settings in bolivia. [Google Scholar]
- Randazzo W., Truchado P., Cuevas Ferrando E., Simon P., Allende A., Sanchez G. SARS-CoV-2 RNA titers in wastewater anticipated COVID-19 occurrence in a low prevalence area. Water Res. 2020;181:115942. doi: 10.1016/j.watres.2020.115942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rheinländer T., Konradsen F., Keraita B., Apoya P., Gyapong M. Redefining shared sanitation. Bull. World Health Organ. 2015;93(7):509–510. doi: 10.2471/BLT.14.144980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rimoldi S.G., Stefani F., Gigantiello A., Polesello S., Comandatore F., Davide M., Maresca M., Longobardi C., Mancon A., Romeri F., Pagani C., Cappelli F., Roscioli C., Moja L., Gismondo M.R., Salerno F. Presence and infectivity of SARS-CoV-2 virus in wastewaters and rivers. Sci. Total Environ. 2020;744:140911. doi: 10.1016/j.scitotenv.2020.140911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodríguez-Lázaro D., Cook N., Ruggeri F.M., Sellwood J., Nasser A., Nascimento M.S.J., D’Agostino M., Santos R., Saiz J.C., Rzeżutka A., Bosch A., Gironés R., Carducci A., Muscillo M., Kovač K., Diez-Valcarce M., Vantarakis A., von Bonsdorff C.H., Husman A.M.D., Hernández M., van der Poel W.H.M. Virus hazards from food, water and other contaminated environments. FEMS Microbiol. Rev. 2012;36(4):786–814. doi: 10.1111/j.1574-6976.2011.00306.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schroeder L.F., Amukele T. Medical laboratories in Sub-Saharan Africa that meet in ternational quality standards. Am. J. Clin. Pathol. 2014;141(6):791–795. doi: 10.1309/AJCPQ5KTKAGSSCFN. [DOI] [PubMed] [Google Scholar]
- Sherchan S.P., Shahin S., Ward L.M., Tandukar S., Aw T.G., Schmitz B., Ahmed W., Kitajima M. First detection of SARS-CoV-2 RNA in wastewater in North America: a study in Louisiana, USA. Sci. Total Environ. 2020;743:140621. doi: 10.1016/j.scitotenv.2020.140621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Street R., Malema S., Mahlangeni N., Mathee A. Wastewater surveillance for Covid-19: an African perspective. Sci. Total Environ. 2020;743:140719. doi: 10.1016/j.scitotenv.2020.140719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The State Council of China Regulations for the management of medical waste. 2011. http://www.gov.cn/gongbao/content/2011/content_1860802.htm
- Tortajada C., van Rensburg P. Drink more recycled wastewater. Nature. 2020;577(7788):26–28. doi: 10.1038/d41586-019-03913-6. [DOI] [PubMed] [Google Scholar]
- Wang J., Feng H., Zhang S., Ni Z., Ni L., Chen Y., Zhuo L., Zhong Z., Qu T. SARSCoV-2 RNA detection of hospital isolation wards hygiene monitoring during the Coronavirus Disease 2019 outbreak in a Chinese hospital. Int. J. Infect. Dis. 2020;94:103–106. doi: 10.1016/j.ijid.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X., Li J., Jin M., Zhen B., Kong Q., Song N., Xiao W., Yin J., Wei W., Wang G., Si B., Guo B., Liu C., Ou G., Wang M., Fang T., Chao F., Li J. Study on the resistance of severe acute respiratory syndrome-associated coronavirus. J. Virol. Methods. 2005;126(1–2):171–177. doi: 10.1016/j.jviromet.2005.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang W., Xu Y., Gao R., Lu R., Han K., Wu G., Tan W. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA-J. Am. Med. Assoc. 2020;323(18):1843–1844. doi: 10.1001/jama.2020.3786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wigginton K.R., Ye Y., Ellenberg R.M. Emerging investigators series: the source and fate of pandemic viruses in the urban water cycle. Environ. Sci. Water Res. Technol. 2015;1(6):735–746. doi: 10.1039/c5ew00125k. [DOI] [Google Scholar]
- World Bank WASH (water, sanitation & hygiene) and COVID-19. 2020. https://www.worldbank.org/en/topic/water/brief/wash-water-sanitation-hygiene-and-covid-19
- World Health Organization (WHO) Progress on household drinkingwater, sanitation and hygiene 2000–2017: special focus on inequalities. 2019. https://www.who.int/water_sanitation_health/publications/jmp-report-2019/en/
- World Health Organization (WHO) Novel coronavirus disease (COVID-19) situation report-209. 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200816-covid-19-sitrep-209.pdf?sfvrsn=5dde1ca2_2
- World Health Organization (WHO) Status of environmental surveillance for SARS-CoV-2 virus. 2020. https://www.who.int/publications/i/item/WHO-2019-nCoV-sci-brief-environmentalSampling-2020-1
- World Health Organization and the United Nations Children'’s Fund (WHO and UNICEF) WASH in health care facilities. 2019. https://apps.who.int/iris/bitstream/handle/10665/311620/9789241515504-eng.pdf?ua=1
- World Health Organization and the United Nations Children'’s Fund (WHO and UNICEF) Water, sanitation, hygiene and waste management for COVID-19 virus technical brief. WHO/2019-nCoV/IPC_WASH/2020.1. 2020. https://apps.who.int/iris/bitstream/handle/10665/331305/WHO-2019-NcOV-IPC_WASH-2020.1-eng.pdf?sequence=1&isAllowed=y
- World Health Organization and the United Nations Children'’s Fund (WHO and UNICEF) water, sanitation, hygiene and waste management for COVID-19 virus interim guidance. WHO/2019-nCoV/IPC_WASH/2020.2. 2020. https://www.who.int/publications-detail/water-sanitation-hygiene-and-waste-management-for-covid-19
- Wu F., Xiao A., Zhang J., Gu X., Lee W.L., Kauffman K., Hanage W., Matus M., Ghaeli N., Endo N., Duvallet C., Moniz K., Erickson T., Chai P., Thompson J., Alm E. SARS-CoV-2 titers in wastewater are higher than expected from clinically confirmed cases. medRxiv 2020.04.05.20051540. 2020 doi: 10.1101/2020.04.05.20051540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wurtzer S., Marechal V., Mouchel J.-M., Maday Y., Teyssou R., Richard E., Almayrac J.L., Moulin L. Evaluation of lockdown impact on SARS-CoV-2 dynamics through viral genome quantification in Paris wastewaters. medRxiv 2020.04.12.20062679. 2020 doi: 10.1101/2020.04.12.20062679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye Y., Ellenberg R.M., Graham K.E., Wigginton K.R. Survivability, partitioning, and recovery of enveloped viruses in untreated municipal wastewater environ. Sci. Technol. 2016;50(10):5077–5085. doi: 10.1021/acs.est.6b00876. [DOI] [PubMed] [Google Scholar]
- Yépiz-Gómez M.S., Gerba C.P., Bright K.R. Survival of respiratory viruses on fresh produce. Food Environ. Virol. 2013;5(3):150–156. doi: 10.1007/s12560-013-9114-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu I.T.S., Li Y., Wong T.W., Tam W., Chan A.T., Lee J.H.W., Leung D.Y.C., Ho T. Evidence of airborne transmission of the severe acute respiratory syndrome virus. N. Engl. J. Med. 2004;350(17):1731–1739. doi: 10.1056/nejmoa032867. [DOI] [PubMed] [Google Scholar]
- Zamorano M., Pérez J.I.P., Pavés I.A., Ridao A.R. Study of the energy potential of the biogas produced by an urban waste landfill in southern Spain. Renew. Sust. Energ. Rev. 2007;11(5):909–922. doi: 10.1016/j.rser.2005.05.007. [DOI] [Google Scholar]
- Zhang D., Ling H., Li J., Li W., Yi C., Zhang T., Jiang Y., He Y., Deng S., Zhang X., Liu Y., Li G., Qu J. Potential spreading risks and disinfection challenges of medical wastewater by the presence of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) viral RNA in septic tanks of Fangcang Hospital. Sci. Total Environ. 2020;741:140445. doi: 10.1016/j.scitotenv.2020.140445. [DOI] [PMC free article] [PubMed] [Google Scholar]