Introduction
The novel coronavirus disease 2019 (COVID-19) is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), a positive-sense, single-stranded RNA virus.1 The most common presenting symptoms include cough, fever, fatigue, shortness of breath, sore throat, and headache. Although respiratory failure is the primary complication seen in COVID-19, patients are at high risk of having multisystem involvement, including acute cardiac injury.2 We present an atypical case of COVID-19 infection with subclinical myocarditis and intermittent complete atrioventricular (AV) block to demonstrate the value of cardiac magnetic resonance imaging (cMRI) in detecting early cardiac involvement.
Key Teaching Points.
-
•
Atypical presentation of COVID-19 infection with high-grade atrioventricular block or complete heart block could be related to subclinical myocarditis.
-
•
Cardiac magnetic resonance imaging in suspected cases is the imaging modality of choice.
-
•
Owing to gaps in our knowledge of the effects and outcome of COVID-19 on the cardiac conduction system, permanent pacemaker insertion might be an indication in case of uncertainty of recovery of the conduction system.
Case report
A 58-year-old man, known to have essential hypertension, was kept in isolation owing to close contact with a case of novel coronavirus infection. He remained stable and asymptomatic, and his initial COVID-19 nasopharyngeal RNA PCR swab test was negative. However, on day 9 of isolation, he was found to have asymptomatic bradycardia with a pulse rate of 40 beats per minute (bpm); hence, he was transferred to our tertiary care hospital.
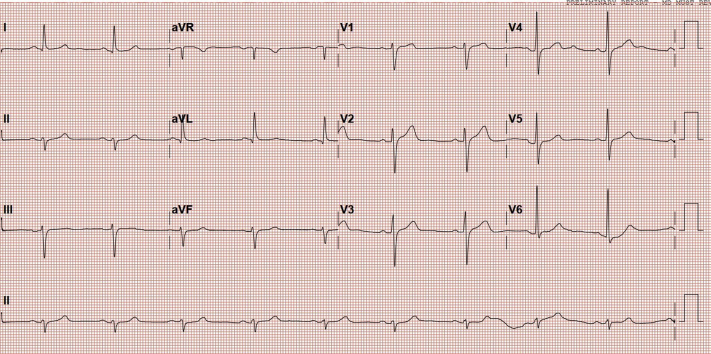
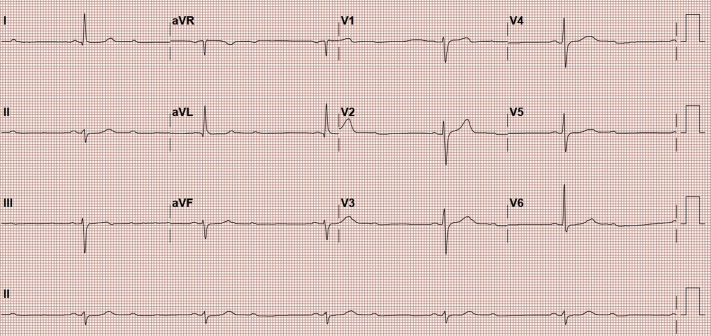
In the emergency department, patient was asymptomatic and his vitals were as follows: pulse rate of 38 bpm, blood pressure 150/114 mm Hg, respiratory rate 16 breaths per minute, and oxygen saturation 98% on room air. His initial electrocardiogram (ECG) showed sinus bradycardia with no ST–T wave changes (Figure 1), and a repeat ECG 1 hour later showed 2:1 second-degree AV block (Figure 2). On cardiac examination, patient had normal first and second heart sounds and no murmurs were appreciated. Systemic examination was otherwise unremarkable.
Figure 1.
Patient’s initial electrocardiogram showing sinus bradycardia with heart rate of 52 beats per minute.
Figure 2.
A repeat electrocardiogram an hour later showed 2:1 atrioventricular block.
A repeat PCR test for COVID-19 was positive. Laboratory investigations revealed normal ranges of the following: inflammatory markers, cardiac biomarkers, D-dimers, NT pro-BNP, LDH, and ferritin levels. Chest radiography showed no abnormality. The infectious disease service was consulted and advised not to start any medications, as our patient was asymptomatic.
The patient was admitted for cardiac observation and started on a prophylactic dose of enoxaparin and amlodipine.
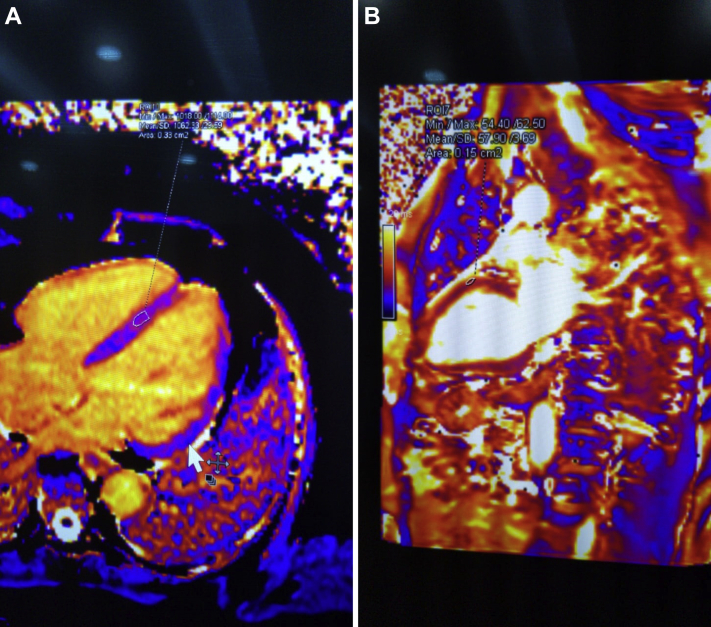
He remained asymptomatic except for multiple episodes of bradycardia, with the lowest recorded heart rate being 35 bpm. A repeat ECG showed persistence of 2:1 second-degree heart block. A cMRI with contrast was performed, which revealed edema of the interventricular septum indicative of myocarditis (Figure 3A and B). Owing to unavailability of continuous telemetry in the COVID-19 unit where the patient was admitted, an inpatient 24-hour Holter monitor was performed. The baseline rhythm was normal sinus rhythm with persistent 2:1 AV block and heart rate ranging between 31 and 46 bpm. Intermittent complete AV block was noted as well. Transthoracic echocardiography was an unremarkable study showing only a mildly dilated ascending aorta. The patient underwent coronary angiography, which revealed 70% disease in the proximal left anterior descending artery with no significant lesion in the left circumflex artery. His right coronary artery was small and nondominant.
Figure 3.
A: Cardiac magnetic resonance image (cMRI) with T1 mapping showing a high value of 1062, indicating myocarditis. B: cMRI with T2 mapping of the myocardium showing an abnormal value of 57, indicating edema.
Our patient was closely observed for 2 weeks as he recovered from COVID-19 infection with the aid of anti-inflammatory medications; however, the AV block did not resolve. The patient was asymptomatic at rest but, owing to the presence of intermittent complete heart block on 24-hour Holter, evidence of myocarditis on cMRI, and history of COVID-19 infection with uncertain long-term sequelae, he was scheduled for a permanent pacemaker implant, which was performed uneventfully. The patient was discharged in a stable condition. Pacemaker interrogation during follow-up showed right ventricular pacing percentage of 27%.
Discussion
Although respiratory failure is the primary complication seen in COVID-19, patients are at high risk of having multisystem involvement, including acute cardiac injury. Cardiac involvement of COVID-19 has ranged from asymptomatic myocardial injury to acute coronary syndrome, myocarditis, stress cardiomyopathy, and cardiogenic shock.1
A case series involving 138 hospitalized patients with COVID-19-infected pneumonia in Wuhan, China, reported 7.2% of patients developing acute cardiac injury (defined by elevated high-sensitivity cardiac troponin I levels or new ECG or echocardiographic abnormalities), and around 16.7% patients were noted to have developed arrhythmias.3
Several possible mechanisms for cardiac involvement have been reported in literature. The virus has been found to invade cells by binding to angiotensin-converting enzyme-2 receptors, which are found in cells of many organs, including the lungs, kidneys, intestines, and heart.1 Therefore, it has been hypothesized that angiotensin-converting enzyme-2-related signaling pathways might have a role to play in inducing cardiac injury. A few other mechanisms that have been thought to potentially induce cardiac damage are hypoxemia and systemic inflammatory response caused by COVID-19.4
Few cases have reported an association between AV block and COVID-19 infection. Interestingly, it has occurred in patients without any significant cardiac comorbidities or underlying conduction disease.5, 6, 7 Herein, we describe a patient who is known to have hypertension and a single vessel with 70% obstructive coronary artery disease, admitted to the hospital with COVID-19 infection and asymptomatic 2:1 second-degree AV block. Our patient was found to have no reversible cause of his AV block, such as thyroid dysfunction, electrolyte disturbances, acute myocardial infarction, or use of medications such as chloroquine and/or hydroxychloroquine, which are commonly prescribed to treat COVID-19 infection.
Our patient did not have extensive systemic or myocardial involvement; however, COVID-19 infection resulted in subclinical myocarditis, as demonstrated by cMRI.
Viral infections have been considered as one of the most common infectious causes of myocarditis, especially associated with influenza and parvovirus B-19 infection.8 However, very little is known about cardiac involvement as a complication of COVID-19 infection. Whether the development of arrhythmia is secondary to direct viral involvement or due to an exaggerated inflammatory response is unknown at this time.
The current recommendations for indications for cardiac pacemaker insertion according to the American College of Cardiology and American Heart Association for second-degree AV block are if it is associated with symptomatic bradycardia, regardless of the type or site of block. It is also recommended for third-degree AV block in symptomatic patients.
Currently, there are no data available regarding treatment of COVID-19 infection–related AV block. In this case a pacemaker was implanted based on our consensus decision, keeping in mind the instability of the second-degree heart block, which was intermittently progressing into complete heart block. Our patient was eventually discharged home in a stable condition, and pacemaker choice was later supported by the high percentage of pacing.
Conclusion
Patients with COVID-19 infection can present with high-degree AV block, and the course can either be intermittent or progressive. It can recover spontaneously or persist, as in our case, where it persisted beyond 2 weeks, even after recovery from COVID-19 infection. The etiology of development of AV block in our patient was likely due to subclinical myocarditis, as confirmed by cMRI. Permanent pacemaker insertion could be a reasonable mode of treatment in such cases.
Footnotes
Funding: There are no funding sources for this manuscript. Disclosures: The authors have no relationships relevant to the contents of this paper to disclose.
References
- 1.Zhou P., Yang X., Wang X. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vetter P., Vu D.L., L’Huillier A.G., Schibler M., Kaiser L., Jacquerioz F. Clinical features of covid-19. BMJ. 2020;369:m1470. doi: 10.1136/bmj.m1470. [DOI] [PubMed] [Google Scholar]
- 3.Wang D., Hu B., Hu C. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zheng Y.Y., Ma Y.T., Zhang J.Y., Xie X. COVID-19 and the cardiovascular system. Nat Rev Cardiol. 2020;17:259–260. doi: 10.1038/s41569-020-0360-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kir D., Mohan C., Sancassani R. Heart Brake—An unusual cardiac manifestation of Coronavirus disease 2019 (COVID-19) JACC Case Rep. 2020;2:1252–1255. doi: 10.1016/j.jaccas.2020.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eneizat Mahdawi T., Wang H., Haddadin F., Al-Qaysi D., Wylie J. Heart block in patients with coronavirus disease 2019: A case series of 3 patients infected with SARS-CoV-2. HeartRhythm Case Rep. 2020;6:652–656. doi: 10.1016/j.hrcr.2020.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Azarkish M., Laleh Far V., Eslami M., Mollazadeh R. Transient complete heart block in a patient with critical COVID-19. Eur Heart J. 2020;41:2131. doi: 10.1093/eurheartj/ehaa307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fung G., Luo H., Qiu Y., Yang D., McManus B. Myocarditis. Circ Res. 2016;118:496–514. doi: 10.1161/CIRCRESAHA.115.306573. [DOI] [PubMed] [Google Scholar]