Abstract
Background
Severe measures have been implemented around the world to reduce COVID-19 spread with a significant impact on family dynamics.
Aim
To assess the impact of the pandemic on fear, dietary choices and oral health perceptions of parents.
Design
questionnaire containing 19 questions was remotely applied to 1003 parents of children aged 0–12 years. The questions addressed topics regarding changes in daily routine, dietary habits, fear level, oral health, and variation of income during the pandemic. Data analysis included the description of the relative and absolute frequencies of the variables. Association tests were performed using Fisher's exact and Kruskal-Wallis tests.
Results
73% of respondents reported income loss. Five hundred sixty-eight people denied seeking medical or dental care. 61.5% of respondents revealed changes in the dietary pattern; most of them mentioned an increase in food intake. Most parents (66.6%) would only seek urgent dental care. There was an association between parents’ willingness to take their children to dental appointments with the fear level (p < 0.001).
Conclusions
Most families have experienced changes in daily routine and eating habits during the pandemic. Parents fear COVID-19 and it impacts their behavior regarding seeking dental care for their children.
Keywords: COVID-19, Pandemic, Pediatric dentistry, Oral health, Child care, Dietary pattern
1. Introduction
On March 11th 2020, The World Health Organization (WHO) characterized the Coronavirus Disease 2019 (COVID-19) as a pandemic. The disease was first reported in December 2019 to WHO China Office as pneumonia of unknown cause. In January 2020, a novel coronavirus (SARS-CoV-2) was identified, and its genome sequencing was released (World Health Organization, 2020c). By September 07th, the world had registered 27,150,797 COVID-19 cases and 889,256 deaths (Centre, 2020), numbers widely higher than those reported during the two outbreaks with coronaviruses in the recent past. During 2002–2003, 8098 cases of the severe acute respiratory syndrome (SARS) and 774 deaths were registered (World Health Organization, 2003), while 2519 laboratory-confirmed cases of the Middle East respiratory syndrome (MERS) were reported between 2012 and 2020 with 866 deaths (World Health Organization, 2020a).
COVID-19 has high contagiousness and rapid spread (Sanche et al., 2020), mainly through small droplets from the nose and mouth expelled when an infected person speaks, coughs or sneezes (World Health Organization, 2020b). Even patients with no symptoms seem to be able to transmit the virus (World Health Organization, 2020b). The majority of the infections are mild or asymptomatic (80%), while about 5% are critical infections (World Health Organization, 2020b). Governments have established policy responses to combat the coronavirus pandemic, including measures to restrict people’s transit, business operations, social distancing, cancellation of services, reservations and events (Coulthard, 2020, Ministry of Economics, 2020, Peloso et al., 2020a). Those measures have led to stay-at-home orders, social distancing, lockdowns, job losses, insecurity, concerns, fears, and a decrease in the quality of life of families worldwide (Ornell, Schuch, Sordi, & Kessler, 2020).
The suspension of school programs and sports activities during the pandemic has led children and adolescents to spend longer periods at home. The new routine may result in an increase in food intake, including ultra-processed and calorie-dense foods (Creswell et al., 2020, Di Renzo et al., 2020). Pietrobelli et al. (2020) suggested that potato chips, red meat, and sugary drink intakes significantly increased in Italy during the lockdown. High-carbohydrates diets may lead to several health issues, such as obesity, diabetes, as well as poor oral health. Frequent sugar intake favors dental biofilm accumulation and contributes to the development of caries lesions and periodontal disease (Colombo & Tanner, 2019). Meanwhile, the pandemic has challenged health professions such as Dentistry. Concerns regarding dentist’s and patient’s safety pushed to the reduction of routine dental care (Cotrin et al., 2020a, Coulthard, 2020, Faccini et al., 2020, Pereira et al., 2020), compromising preventive appointments.
Brazil is the second country in the number of confirmed cases of COVID-19, with one of the fastest growing coronavirus epidemics in the world (Candido et al., 2020). The increasing number of cases has divided opinions regarding the economy reopening and resumption of once-routine daily life. It has directly affected habits, bringing concerns toward the future in general. The changes in diet, economic issues, general concerns, fear, added to the lack of preventive dental care, could impact the oral health of children during the enforced stay-at-home orders. Thus, this study aimed to assess the fear level, dietary choices and parent’s oral health perceptions during the stay-at-home orders period in Brazil.
2. Material and methods
A cross-sectional study was carried out using non-probabilistic sampling, with parents of children aged 0–12 years, from all 5 geographic regions of Brazil (North, Northeast, Southeast, South, and Center-West). This study was conducted after approval by the Research Ethics Committee of Ingá University Center Uningá (Protocol # 4.002.200).
The representative sample size was estimated using a 95% confidence level and margin of error of 5%. The sample calculation considered 35.5 million children aged 0–12 years in Brazil in 2018 (IBGE, 2018). The sample size was estimated at a minimum of 385 respondents.
A structured questionnaire was developed according to the CHERRIES recommendations (Eysenbach, 2004). A pilot study was performed to verify the functionality of the questionnaire. For the pilot study, 38 parents (10% of the sample size calculation) were randomly selected from the files of the patients of a single private dental office and they were not included in the final sample.
The questionnaire contained 19 mandatory questions about socioeconomic and demographic dates, fear income variability, eating habits and parent’s oral health perceptions. The original questionnaire was an open survey, written in Brazilian Portuguese using the Google Forms platform and forwarded to parents and caregivers of children aged 0–12 years through social media and message apps from May 12th to June 9th, 2020. It was available for 29 days. All parents who fit the criteria of having children under 12 years of age could answer the questionnaire. The translated questionnaire is shown in Table 1 . All the respondents had access to the Consent Statement and requested to agree with it before being included in the present study. The informed consent included the object of the study, the responsible researchers and their contact information. The approximate time for the answer to the questionnaire was informed, being about five minutes. The answers and data obtained were stored by the researchers and used only for this study. To ensure the anonymity of each respondent, no identifying information was collected. Before sending the questionnaire, participants could change their answers many times as they wish. No duplicate response control tool was used, but if identical responses in sequence were observed, one was excluded.
Table 1.
Translated questionnaire sent to parents and legal guardians of children aged 0–12 years old.
| Question | Options |
|---|---|
| 1. What city and state do you live in? | |
| 2. How old are you? | |
| 3. Regarding minors living in your house. You are: | Mother; Father; Other (the volunteer could write the answer) |
| 4. How many people live in your house (consider you)? | 2; 3; 4; 5 or more people |
| 5. Which activities you used to do and have not done during the pandemic due to fear of getting COVID-19 (volunteer could select one or more options). | Go to health offices/clinics (doctor, dentist, psychologist, etc.); Go to grocery stores; Go out for leisure; Visit relatives and friends; Go to work; Go to school/college; I am not doing any of the listed activities; I am doing all the activities I used to do; other (the volunteer could write the answer). |
| 6. On a scale of 0 to 10, where 0 is no fear and 10 is terror, indicate the option that best describes your fear of the pandemic. | 0; 1; 2; 3; 4; 5; 6; 7; 8; 9; 10 |
| 7. Which alternative best describes the impact of the pandemic on your family income. | Family income not impacted; Slightly reduced; Drastically reduced; Total loss of income; Increased during the pandemic. |
| 8. There has been any change in food consumption in your home during the pandemic? | Yes, we are eating cheaper foods; Eating less than before; Eating more than before; There was no change in food intake; Other (the volunteer could write the answer). |
| 9. There has been any change in eating habits at your home during the pandemic? (volunteer could select one or more options). | We are consuming more processed food with sugar such as soft drinks, sweets and cookies; Consuming more pasta and carbohydrates; Consuming more healthy food such as fruits and vegetables; Consuming more snacks and/or frozen food; Nothing has changed. |
| 10. How is your family's daily routine during the pandemic? | We are not leaving the house for anything; Leaving the minimum necessary (pharmacy, supermarket, etc.); Leaving just to work; Leaving the house as usual. |
| 11. Do you or anyone in your household have had symptoms of COVID-19? | Yes, but the person was not tested; Yes, the test was negative for COVID-19; Yes, the test was positive for COVID-19; No one has had symptoms or has been diagnosed with COVID-19. |
| 12. How many children between 0 and 12 years old do you? | 1; 2; 3; 4 or more. |
| 13. Were any of your children (0–12 years old) undergoing dental treatment before the pandemic? (volunteer could select one or more options). | No; Yes, orthodontic treatment; Yes, caries treatment; Yes, because of toothache; Yes, because of dental trauma; Other (the volunteer could write the answer). |
| 14. Would you take your child to a dental appointment during the pandemic? | Yes, for any procedure; Yes, but only for urgent treatments; No; Other (the volunteer could write the answer). |
| 15. If not, for what reason? | Risk of contracting COVID-19; the dental treatment is not urgent; My child/I has/have symptoms of COVID-19. |
| 16. Have you been able to brush your children's teeth during the pandemic? | Yes; No; Sometimes. |
| 17. Has any of your children experienced dental trauma during the pandemic? | No; Yes, I sought care right after the trauma and my child was assisted; Yes, but I did not seek care; Yes, I sought care, but we were not assisted; Other (the volunteer could write the answer). |
| 18. Have you noticed any cavities/caries in your children's teeth during the pandemic? | No; Yes, I sought care and my child was assisted; Yes, but I did not seek care; Yes, I sought care, but we were not assisted; Other (the volunteer could write the answer). |
| 19. Has any of your children experienced toothache during the pandemic? | No; Yes, I sought, and my child was assisted; Yes, but I did not seek care; Yes, I sought care, but we were not assisted; Other (the volunteer could write the answer). |
The answers obtained were tabulated in Excel (Microsoft Corp., Redmond, USA), and the statistical analysis was performed using the IBM-SPSS 22.0 software. For statistical analysis, some variables were categorized. The ‘State’ variables were scored according to the number of cases per 100,000 inhabitants, according to national data at the time of the study, being ‘up to 100,000 cases’, ‘101,000 to 300,000 cases’, ‘301,000 to 500,000 cases’ and ‘over 500,000 cases’. The fear level was categorized into ‘0 to 2’, ‘3 to 5’, ‘6 to 8’ and ‘9 to 10’. Fear levels 6–8 and 9–10 were considered moderate and high fear, respectively.
Data analysis included the description of the relative and absolute frequencies of the variables. Association tests were performed using Fisher's exact and Kruskal-Wallis tests for ordinal variables.
3. Results
A total of 1003 questionnaires were filled in by people from 25 states and the Federal District. No response was obtained from the State of Acre (North). The great majority of respondents (97.2%) were parents (mother/father), with an average age of 36.6 years (s.d. = ±6.97). Most families (73%) disclosed a reduction in income, with 52.9% reporting a slight reduction and 20.1% drastic reduction or total loss of income.
Regarding the number of people living in each house, 82.6% of the households had three to four people, and 94.1% of respondents had 1 or 2 children aged 0 to 12 years. No association was found between these variables and the reported presence of caries lesions, dental pain or dental trauma (p > 0.05). Only 1.8% of respondents had confirmed COVID-19, and 6.9% had symptoms but were not tested.
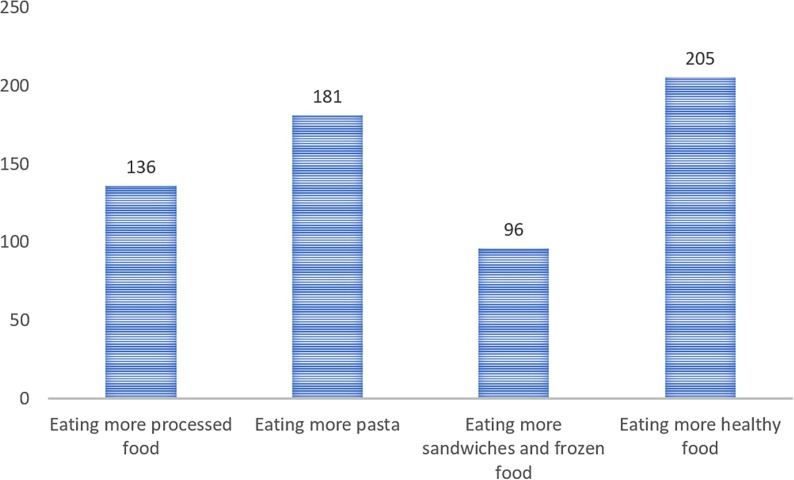
Five hundred sixty-eight people declared not leaving their houses for medical or dental appointments, and 876 were not doing leisure activities. Forty-three percent said they were leaving their houses only when necessary, and 52.8% stated leaving their houses to work. 61.5% of respondents reported changes in eating habits during the pandemic; most of them revealed an increase in food intake (Fig. 1 ). Of those who claimed changes in eating habits, only 33.1% said they were choosing healthier foods, while the others increased the consumption of processed foods, pasta and snacks (Fig. 2 ). Families with drastic or total loss of income are eating less than before or opting for cheaper food (p < 0.001) (Table 2 ). No association was found between the caries perception of parents and changes in food consumption (p = 0.53).
Fig. 1.
Changes in eating habits during the pandemic.
Fig. 2.
Changes in food intake during the pandemic.
Table 2.
Association between eating habits and income during the pandemic in Brazilian families with children aged 0–12 years (n = 1003).
| Income | Food intake pattern |
||||
|---|---|---|---|---|---|
| Eating cheaper foods | Eating less than before | Eating more than before | No change in food consumption | p-value* | |
| N (%) | n (%) | n (%) | n (%) | ||
| Not impacted | 20 (12.6) | 0 (0.0) | 129 (29.7) | 111 (28.8) | <0.001 |
| Slightly reduced | 75 (47.2) | 13 (52.0) | 233 (53.7) | 210 (54.5) | |
| Drastically reduced | 55 (34.6) | 8 (32.0) | 66 (15.2) | 58 (15.0) | |
| Total loss | 6 (3.8) | 4 (16.0) | 3 (0.7) | 2 (0.5) | |
| Increased | 3 (1.9) | 0 (0.0) | 3 (0.7) | 4 (1.0) | |
| Total | 159 | 25 | 434 | 385 | |
Fisher's exact test.
Regarding their children’s oral hygiene, 83.5% of parents reported brushing their children’s teeth during the pandemic, 14.7% brushed sometimes and only 1.8% did not brush. There was no significant association between brushing the teeth and the variables tooth pain, presence of dental caries and change in dietary pattern.
Regarding oral health, 24.4% of parents/caregivers reported their children were undergoing dental treatment before the pandemic. However, only 17.8% of total respondents are willing to take their children to dental care regardless of the procedure; 66.6% would only seek urgent care, and 15.1% would not seek dental care at all. The frequency of distribution of dental pain reports, the presence of caries lesions and dental trauma are shown in Table 3 .
Table 3.
Distribution of parents' report regarding dental trauma, their perception of caries and dental pain in children aged 0–12 years. Brazil (n = 1003).
| No | Yes, I sought care and we were assisted | Yes, but I did not seek care | Yes, I sought care, but we were not assisted | |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | |
| PAIN | 943 (93.9) | 31 (3.1) | 22 (2.2) | 4 (0.4) |
| TRAUMA | 942 (93.8) | 17 (1.7) | 44 (4.4) | 1 (0.1) |
| CARIES | 904 (90.1) | 44 (4.4) | 46 (4.6) | 10 (1.0) |
Fifty-one people declared their children experienced dental trauma during the pandemic. However, 86% of them did not seek dental care. Association was found among parents/caregivers’ willingness to take their children to dental appointments, fear level (p < 0.001), and the local number of COVID-19 cases (p < 0.001) (Table 4 ). When the fear level was assessed, 49.2% of respondents reported a level of fear between 6 and 8, while 16.1% said their fear level is between 9 and 10.
Table 4.
Association between parents' willingness to take their children to dental appointments during the pandemic, prevalence of COVID-19 and fear levels. Brazil (n = 1003).
| Would you take your child to a dental appointment during the pandemic? | ||||
|---|---|---|---|---|
| Yes, for any procedure | Yes, but only for urgent treatments | No | p-value* | |
| n (%) | n (%) | n (%) | ||
| COVID-19 cases per 100,000 people | ||||
| Up to 100 cases | 112 (62.6) | 286 (42.8) | 60 (38.4) | |
| 101 to 300 cases | 53 (29.6) | 259 (38.7) | 54 (34.6) | <0.001 |
| 301 to 500 cases | 11 (6.1) | 85 (12.7) | 32 (20.5) | |
| Above 501 cases | 3 (1.7) | 39 (5.8) | 10 (6.4) | |
| Fear score | ||||
| 0–2 | 35 (19,6) | 25 (3.7) | 9 (5.7) | |
| 3–5 | 74 (41.3) | 174 (26.0) | 31 (19.8) | <0.001 |
| 6–8 | 67 (37.4) | 356 (53.2) | 71 (45.5) | |
| 9–10 | 3 (1.7) | 114 (17.0) | 45 (28.8) | |
| Total | 179 | 669 | 156 | |
Kruskal-Wallis test.
4. Discussion
For billions of people across the world, daily life has changed dramatically in the past months. The coronavirus pandemic has required adaptations from adults, youth and children in the way they study, work and interact with others. The new routine may impact family well-being by reducing its income, raising fears, increasing anxiety, stress, and instability (Cotrin et al., 2020b, Ornell et al., 2020, Parsons, 2020, Peloso et al., 2020b). In the course of the present work, Brazil recorded an increasing number of daily cases of COVID-19, reaching its highest number of new confirmed cases (54,771) on June 19th. This compelled the extension of stay-at-home orders, social distancing and restrictions, exacerbating the risk of an economic recession. This study found that 73% of the participants from 25 states and the Federal District of Brazil lost income during the pandemic, 20.1% of them reported drastic reductions in family income. In a single-hit scenario, Brazil’s GDP is expected to fall by 7.4%, while a decrease by 9.1% may be experienced if a second wave of the pandemic imposes further lockdowns.
Financial instability, unemployment, economic crises, social distancing, self-isolation, and potentially life-threatening diseases are impacting people’s concerns and mental health around the world (Knipe, Evans, Marchant, Gunnell, & John, 2020). In the present study, over 65% of respondents reported fear levels equal to or higher than 6 when the Likert scale was applied, while 16.1% declared fear levels 9 or 10. Fear is present since the early stages of human development (Papalia & Feldman, 2013). It is a non-pathological emotion, consequence of real or imagined threat (Burnham & Gullone, 1997) and results from risk assessments (Papalia & Feldman, 2013). However, high levels of fear may produce negative health outcomes and ultimately may cause emotional and physical damage, as it impedes people from naturally performing daily activities (Balan, Moise, Moldoveanu, Leordeanu, & Moldoveanu, 2019). A significant association was found between the level of fear, the local number of contaminated and seeking dental care. Families living in areas with higher numbers of COVID-19 cases fear more for safety than those living in less affected areas. It results in greater precaution regarding the seek for dental treatments since parents with higher levels of fear are also those who would either take their children to the dentist only in dental urgencies (66.6%) or would not take them at all (15.1%). The concerns of parents/caregivers regarding COVID-19 may be especially high when it comes to children since its sign and symptoms are not well established at young ages (Mallineni et al., 2020). Adverse manifestations of COVID-19 have been reported in children, such as the Kawasaki disease-like illness related to the infection by SARS-CoV-2 observed in Europe and the United States (Choi, 2020). However, Ludvigsson (2020) found, in a systematic review, that infected children presented milder symptoms of COVID-19 and also a better prognosis than adults.
Studies have shown that people have postponed medical treatments due to the fear of contracting COVID-19, which may increase the risk of serious health issues in the near future (Karacin et al., 2020, Omarini et al., 2020, Teoh et al., 2020). A similar trend was observed in the present study regarding oral health. About 56% of respondents said they are not leaving their houses to attend to medical or dental appointments, and 86% of those who reported that their children were victims of dental trauma during the pandemic did not seek dental care. Besides that, 24.4% of the children had their dental treatment temporarily suspended. The lack of preventive and curative care may negatively impact the oral health of children all over the country and trigger the need for future public actions to address those impacts.
The new routine, work-at-home for parents, remote classes for children and economic instability have contributed to changes in dietary habits (Di Renzo et al., 2020). About 77% of respondents said they increased the intake of high-carb foods. Pietrobelli et al. (2020) correlated the social distancing period to the summer vacation, when children’s carbohydrate intake considerably increases, with a direct impact on childhood obesity. Families with drastic or total income loss reported eating less or choosing cheaper foods during the pandemic. More affordable foods may include pasta, sandwiches, snacks, and other foods with low nutritional value and high sugar content. Those diet changes not only affect general health but also increases the risk of caries development. In addition to the damage caused by the change in dietary pattern to oral health, this change can cause an increase in obesity, nutritional deficiencies, among others. At the same time, there are the psychological effects of the pandemic on children (Spinelli, Lionetti, Pastore, & Fasolo, 2020), which are somehow linked to the changes in food intake patterns and oral hygiene routine. Although this study found no association between parents’ perception of caries lesions, food intake and oral hygiene, one has to consider that the questionnaire was filled in a relatively early stage of the pandemic in Brazil. The effects of dietary habits and decreased care with oral hygiene may become more evident in the next months.
The present study concluded that the COVID-19 pandemic has negatively impacted the eating habits and dental care of children in Brazil. Furthermore, it has trigged moderate and high levels of fear among parents/caregivers. As an alternative to offer dental assistance during these unusual times, future studies should evaluate the effectiveness of ‘Teledentistry’. It has been approved in Brazil by the Council (2020) and allows parents and children to have video or phone appointments, with dentists providing a safe triage, sharing information on oral hygiene and health (Aziz & Ziccardi, 2009).
Funding
There are no fundings to declare.
Data availability
The data are available from the authors upon request.
Author contributions
Conceptualization: M.L.C.F., J.P.S.L.S., D.L.S.S., K.M.S.F. and G.C.S.; Data curation: G.O.C., R.C. and M.P.A.; Formal analysis: K.M.S.F. and G.C.S.; Methodology: M.P.A., J.P.S.L.S., D.L.S.S., K.M.S.F. and G.C.S.; Writing - original draft. G.O.C., D.L.S.S., J.P.S.L.S., K.M.S.F. and G.C.S.; Writing - review & editing: R.C., M.P.A, M.L.C.F., D.L.S.S., K.M.S.F. and G.C.S. All authors read and approved the final version of the manuscript.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.childyouth.2020.105469.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- Aziz S.R., Ziccardi V.B. Telemedicine using smartphones for oral and maxillofacial surgery consultation, communication, and treatment planning. Journal of Oral and Maxillofacial Surgery. 2009;67(11):2505–2509. doi: 10.1016/j.joms.2009.03.015. [DOI] [PubMed] [Google Scholar]
- Balan O., Moise G., Moldoveanu A., Leordeanu M., Moldoveanu F. Fear level classification based on emotional dimensions and machine learning techniques. Sensors (Basel) 2019;19(7) doi: 10.3390/s19071738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burnham J.J., Gullone E. The fear survey schedule for children–II: A psychometric investigation with American data. Behavioral Research and Therapy. 1997;35(2):165–173. doi: 10.1016/s0005-7967(96)00089-7. [DOI] [PubMed] [Google Scholar]
- Candido D.S., Claro I.M., De Jesus J.G., Souza W.M., Moreira F.R.R., Dellicour S.…Faria N.R. Evolution and epidemic spread of SARS-CoV-2 in Brazil. Science. 2020 doi: 10.1126/science.abd2161. eabd2161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi J.W. Can we get a clue for the etiology of Kawasaki disease in the COVID-19 pandemic? Clinical and Experimental Pediatrics. 2020 doi: 10.3345/cep.2020.00955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colombo A.P.V., Tanner A.C.R. The role of bacterial biofilms in dental caries and periodontal and peri-implant diseases: A historical perspective. Journal of Dental Research. 2019;98(4):373–385. doi: 10.1177/0022034519830686. [DOI] [PubMed] [Google Scholar]
- Cotrin P., Peloso R.M., Pini N.I.P., Oliveira R.C., de Oliveira R.C.G., Valarelli F.P., Freitas K.M.S. Urgencies and emergencies in orthodontics during the coronavirus disease 2019 pandemic: Brazilian orthodontists' experience. American Journal of Orthodontics and Dentofacial Orthopedics. 2020 doi: 10.1016/j.ajodo.2020.06.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cotrin P., Peloso R.M., Oliveira R.C., de Oliveira R.C.G., Pini N.I.P., Valarelli F.P., Freitas K.M.S. Impact of coronavirus pandemic in appointments and anxiety/concerns of patients regarding orthodontic treatment. Orthodontics and Craniofacial Research. 2020 doi: 10.1111/ocr.12395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coulthard P. Dentistry and coronavirus (COVID-19) – Moral decision-making. Brazilian Dent Journal. 2020;228(7):503–505. doi: 10.1038/s41415-020-1482-1. [DOI] [PubMed] [Google Scholar]
- Creswell C., Nauta M.H., Hudson J.L., March S., Reardon T., Arendt K.…Kendall P.C. Research review: Recommendations for reporting on treatment trials for child and adolescent anxiety disorders – an international consensus statement. Journal of Child Psychology and Psychiatry. 2020 doi: 10.1111/jcpp.13283. [DOI] [PubMed] [Google Scholar]
- Di Renzo L., Gualtieri P., Pivari F., Soldati L., Attina A., Cinelli G.…De Lorenzo A. Eating habits and lifestyle changes during COVID-19 lockdown: An Italian survey. Journal of Translational Medicine. 2020;18(1):229. doi: 10.1186/s12967-020-02399-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- European Centre for Disease Prevention and Control (2020). COVID-19 situation update worldwide. Retrieved 7 September from https://www.ecdc.europa.eu/en/geographical-distribution-2019-ncov-cases.
- Eysenbach G. Improving the quality of Web surveys: The checklist for reporting results of internet E-surveys (CHERRIES) Journal of Medical Internet Research. 2004;6(3):e34. doi: 10.2196/jmir.6.3.e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faccini M., Ferruzzi F., Mori A.A., Santin G.C., Oliveira R.C., Oliveira R.C.G.d.…Freitas K.M.S. Dental Care during COVID-19 outbreak: A web-based survey. European Journal of Dentistry (EFirst) 2020 doi: 10.1055/s-0040-1715990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Federal Council of Dentistry (2020). Resolution CFO 226-2020 (http://sistemas.cfo.org.br/visualizar/atos/RESOLU%c3%87%c3%83O/SEC/2020/226).
- IBGE (2018). Continuous national household sample survey (PNAD) 2018. Retrieved 15 April from https://biblioteca.ibge.gov.br/visualizacao/livros/liv101548_notas_tecnicas.pdf.
- Karacin, C., Bilgetekin, I., B Basal, F., & Oksuzoglu, O. B. (2020). How does COVID-19 fear and anxiety affect chemotherapy adherence in patients with cancer. Future Oncology (London, England), 10.2217/fon-2020-0592. Advance online publication. 10.2217/fon-2020-0592. [DOI] [PMC free article] [PubMed]
- Knipe D., Evans H., Marchant A., Gunnell D., John A. Mapping population mental health concerns related to COVID-19 and the consequences of physical distancing: A Google trends analysis. Wellcome Open Research. 2020;5:82. doi: 10.12688/wellcomeopenres.15870.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ludvigsson J.F. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatrica. 2020;109(6):1088–1095. doi: 10.1111/apa.15270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mallineni S.K., Innes N.P., Raggio D.P., Araujo M.P., Robertson M.D., Jayaraman J. Coronavirus disease (COVID-19): Characteristics in children and considerations for dentists providing their care. International Journal of Paediatric Dentistry. 2020;30(3):245–250. doi: 10.1111/ipd.12653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministry of Economics (2020). Brazil’s Policy responses to COVID-19. Retrieved 3 June from https://www.gov.br/economia/pt-br/centrais-de-conteudo/publicacoes/publicacoes-em-outros-idiomas/covid-19/covid-19-2020-04-14-brazil-policy-measures-1.pdf/view.
- Omarini C., Maur M., Luppi G., Narni F., Luppi M., Dominici M.…Piacentini F. Cancer treatment during the coronavirus disease 2019 pandemic: Do not postpone, do it! European Journal of Cancer. 2020;133:29–32. doi: 10.1016/j.ejca.2020.04.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ornell F., Schuch J.B., Sordi A.O., Kessler F.H.P. “Pandemic fear” and COVID-19: Mental health burden and strategies. Brazilian Journal of Psychiatry. 2020;42(3):232–235. doi: 10.1590/1516-4446-2020-0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papalia, D. E., & Feldman, R. D. (2013). Psychosocial development in second childhood in human development. Artmed.
- Parsons J. COVID-19, children and anxiety in 2020. Australian Journal of General Practice. 2020;49 doi: 10.31128/AJGP-COVID-27. [DOI] [PubMed] [Google Scholar]
- Peloso R.M., Ferruzzi F., Mori A.A., Camacho D.P., Franzin L., Margioto Teston A.P., Freitas K.M.S. Notes from the field: Concerns of health-related higher education students in brazil pertaining to distance learning during the coronavirus pandemic. Evaluation and the Health Professions. 2020;43(3):201–203. doi: 10.1177/0163278720939302. [DOI] [PubMed] [Google Scholar]
- Peloso R.M., Pini N.I.P., Sundfeld Neto D., Mori A.A., Oliveira R.C.G., Valarelli F.P., Freitas K.M.S. How does the quarantine resulting from COVID-19 impact dental appointments and patient anxiety levels? Brazilian Oral Research. 2020;34:e84. doi: 10.1590/1807-3107bor-2020.vol34.0084. [DOI] [PubMed] [Google Scholar]
- Pereira L.J., Pereira C.V., Murata R.M., Pardi V., Pereira-Dourado S.M. Biological and social aspects of Coronavirus Disease 2019 (COVID-19) related to oral health. Brazilian Oral Research. 2020;34:e041. doi: 10.1590/1807-3107bor-2020.vol34.0041. [DOI] [PubMed] [Google Scholar]
- Pietrobelli A., Pecoraro L., Ferruzzi A., Heo M., Faith M., Zoller T.…Heymsfield S.B. Effects of COVID-19 lockdown on lifestyle behaviors in children with obesity living in Verona, Italy: A longitudinal study. Obesity (Silver Spring) 2020 doi: 10.1002/oby.22861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanche S., Lin Y.T., Xu C., Romero-Severson E., Hengartner N., Ke R. High contagiousness and rapid spread of severe acute respiratory syndrome coronavirus 2. Emerging Infectious Diseases. 2020;26(7):1470–1477. doi: 10.3201/eid2607.200282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spinelli M., Lionetti F., Pastore M., Fasolo M. Parents' stress and children's psychological problems in families facing the COVID-19 outbreak in Italy. Frontiers in Psychology. 2020;11:1713. doi: 10.3389/fpsyg.2020.01713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teoh J.Y., Ong W., Gonzalez-Padilla D., Castellani D., Dubin J.M., Esperto F.…UroSoMe Working Group A global survey on the impact of COVID-19 on urological services. European Urology. 2020;78(2):265–275. doi: 10.1016/j.eururo.2020.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (2003). Summary of probable SARS cases with onset of illness from 1 November 2002 to 31 July 2003. Retrieved 2020 from https://www.who.int/csr/sars/country/table2004_04_21/en/.
- World Health Organization (2020a). MERS situation update. Retrieved 3 June from https://applications.emro.who.int/docs/EMCSR254E.pdf?ua=1&ua=1.
- World Health Organization (2020b). Q&A on coronaviruses (COVID-19). Retrieved 3 June from https://www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and-answers-hub/q-a-detail/q-a-coronaviruses#:~:text=symptoms.
- World Health Organization (2020c). Rolling updates on coronavirus disease (COVID-19). Retrieved 3 June from https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data are available from the authors upon request.