Structured Abstract
Introduction
The recognition of anteromedial knee arthritis as a distinct early clinicopathological entity has led to a resurgence in medial unicompartment knee arthroplasty (UKA). Symptomatic knee pain caused by 180° rotational spin of the mobile bearing of the Oxford Knee is an unrecognized and therefore under-reported complication of UKA. Whilst the post-operative radiographic criteria for optimal positioning of UKA is well described in the available literature, this isn't the case for assessing antero-posterior (AP) orientation of the mobile-bearing.
Methods
Following a literature review, we describe a novel radiographic technique that can consistently assess AP orientation, and as a result, diagnose 180° rotational spin of the mobile-bearing. This technique overcomes the radiological challenge of superimposition of the radiopaque markers with the lateral edge of the tibial tray.
Results
The modified oblique view results in clear visualization of the metallic rod embedded in the polyethylene, away from the lateral edge of the tibial tray. An anteriorly viewed metallic rod would indicate a well oriented mobile bearing. However, if the metallic beads are visualized anteriorly without dislocation, the component would have spun 180°
Conclusion
Clinicians should have a high index of suspicion for 180° spin to have occurred in patients with posterior dislocation with or without spontaneous reduction. We recommend bearing exchange ± revision arthroplasty for symptomatic patients. The modified oblique view is now part of our immediate post-operative XR protocol and repeated for any patient who re-presents symptomatically at any stage following the index procedure.
Keywords: Unicompartment knee arthroplasty, Mobile-bearing, 180° rotational spin, Modified oblique view
Symptomatic knee pain caused by 180° rotational spin of the mobile bearing of the Oxford Knee is an unrecognized and therefore under-reported complication of UKA. We describe a novel radiographic technique that can consistently assess antero-posterior orientation, and as a result, diagnose 180° rotational spin of the mobile-bearing. This technique overcomes the radiological challenge of superimposition of the radiopaque markers embedded in the polyethylene, with the lateral edge of the tibial tray. The modified oblique view is now part of our immediate post-operative XR protocol and repeated for any patient who re-presents symptomatically at any stage following the index procedure.
Abbreviations
- UKA
Unicompartment Knee Arthroplasty
- TKA
Total Knee Arthroplasty
- AP
Antero-posterior
- XR
X-Rays
- MCL
Medial Collateral Ligament
1. Introduction
Unicompartment knee arthroplasty (UKA) is a well-recognized treatment modality for severe arthritis confined to a single compartment, providing faster recovery, fewer complications and better function than total knee arthroplasty (TKA).1, 2, 3 Despite higher revision rates in national registries,4,5 there is a growing evidence base supporting long-term survivorship6, 7, 8 of the prosthesis. This has led to a resurgence in medial UKA over the past 2 decades; its gaining popularity in part due to upgraded anatomic implants, minimally invasive surgical techniques, shorter hospital stays and better preservation of knee kinematics. It has therefore resulted in a paradigm shift in surgical practice, challenging the notion that TKA should be the gold-standard treatment for all knee arthrosis.9
Since its introduction in 1982, the Oxford Mobile Bearing UKA has now achieved worldwide usage and is currently the most commonly implanted UKA design.10 It is the implant of choice in our department for patients with symptomatic anteromedial osteoarthritis of the knee. Our experience with the Oxford Knee has shown that despite modifications and evolutions in the bearing implant design, in situ 180° rotational spin (without dislocation) of the mobile bearing does occur. Whilst the post-operative radiographic criteria for optimal positioning of the Oxford UKA is well described in the available literature,11 this isn't the case for assessing antero-posterior (AP) orientation of the mobile bearing. We therefore developed a novel, reproducible radiographic technique to assess AP orientation of the mobile bearing of the Oxford Medial UKA.
2. Case study
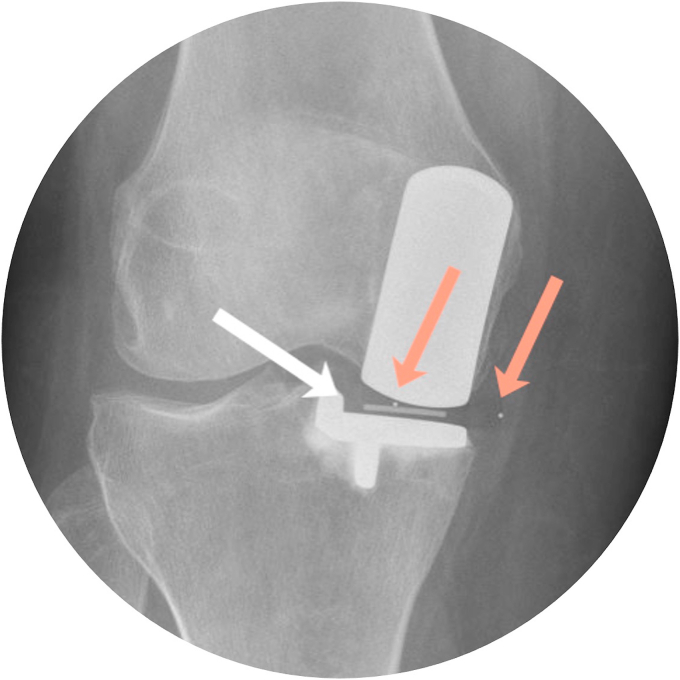
A 51-year old female underwent a right knee medial UKA in June 2017 with an unremarkable post-operative period. At follow-up appointments, she was noted to be managing well and had returned to her normal level of activity. 2 years following her index procedure, she presented to the Emergency Department complaining of atraumatic right knee pain - predominantly on the medial side and reduced range of motion in the knee. Unfortunately, the posterior dislocation of the mobile bearing was missed on initial radiographs (Fig. 1). She was subsequently referred to the elective Orthopaedic clinic, where repeat AP radiographs showed that the bearing had reduced spontaneously but remained rotated at 90° (Fig. 2). A clinical decision was made at the time to perform revision surgery. On the day of her planned surgery date, the patient reported less discomfort in the knee, but was not pain-free. We therefore repeated X-rays (XRs) pre-operatively (Fig. 3) which showed a well-positioned, reduced mobile bearing on AP view. As the patient was still symptomatic, we proceeded with the planned surgery.
Fig. 1.
Lateral radiograph depicting a posteriorly dislocated mobile bearing.
Fig. 2.
AP radiograph depicting 90° rotated mobile bearing.
Fig. 3.
AP radiograph depicting well positioned mobile bearing.
Intraoperatively, the bearing was noted to have spun 180°. The femoral and tibial implants were well fixed with no macroscopic surface damage. The flexion and extension gaps were well balanced, the ACL was present and there was no varus-valgus instability. There was no impingement and no lift-off of a trial mobile bearing of the same thickness throughout the range of movement of the knee. Mobile bearing exchange was subsequently performed instead of revision arthroplasty. The patient had an unremarkable postoperative period, and remained asymptomatic at 6-week, 1 year and 2-year follow up appointments. She was subsequently discharge from routine follow-up.
On retrospective review, we recognize that 180° rotational spin of the mobile bearing did occur but was not highlighted on radiographic assessment. The pre-operative AP radiographs depicted a well-seated polyethylene mobile bearing. Lateral XR assessment did not highlight obvious rotational spin due to overlap of the mobile bearing markers with the lateral edge of the tibial tray. Therefore, given the unusual nature and radiographic challenges posed when assessing for this complication, we reviewed the pre-existing literature for technical tips and subsequently describe our novel radiographic technique that can consistently assess AP orientation and as a result, diagnose 180° rotational spin of the mobile bearing.
3. Methods & results
We performed a literature search using the Ovid Medline, EMBASE and PubMed databases to identify any other relevant articles or case reports sharing similar experiences to our department of the mobile bearing spinning 180° as an isolated complication of UKA.
The search criteria were restricted to ‘unicompartment knee arthroplasty’ or ‘unicondylar knee arthroplasty’. For the Medical Subject Heading (MeSH) term “spin” and “dislocation” were used with “complication” as the subheading. Articles were restricted to the English language and limited to the most recent articles published between 1st January 2000 up to the 1st of January 2020. Individual studies highlighting generic complications were further assessed for complications of unexplained knee pain without radiological abnormalities. Non-clinical studies and those not available with English translation were excluded.
Our search revealed only one other case report, specifically highlighting asymptomatic 180° rotational spin as a specific complication of mobile-bearing UKA.12 Several studies highlight unexplained knee pain without obvious radiological abnormalities,13, 14, 15, 16, 17 with many cases progressing to revision arthroplasty with successful outcomes. However, given the difficulty in recognizing a spun component radiologically, we suspect this is an unrecognized and therefore under-reported complication with a higher probable incidence.
Of note, no study endorsed any additional post-operative radiographic views other than the standard AP and lateral XRs to assess implant position or evidence of dislocation of the mobile-bearing.
4. The modified oblique view
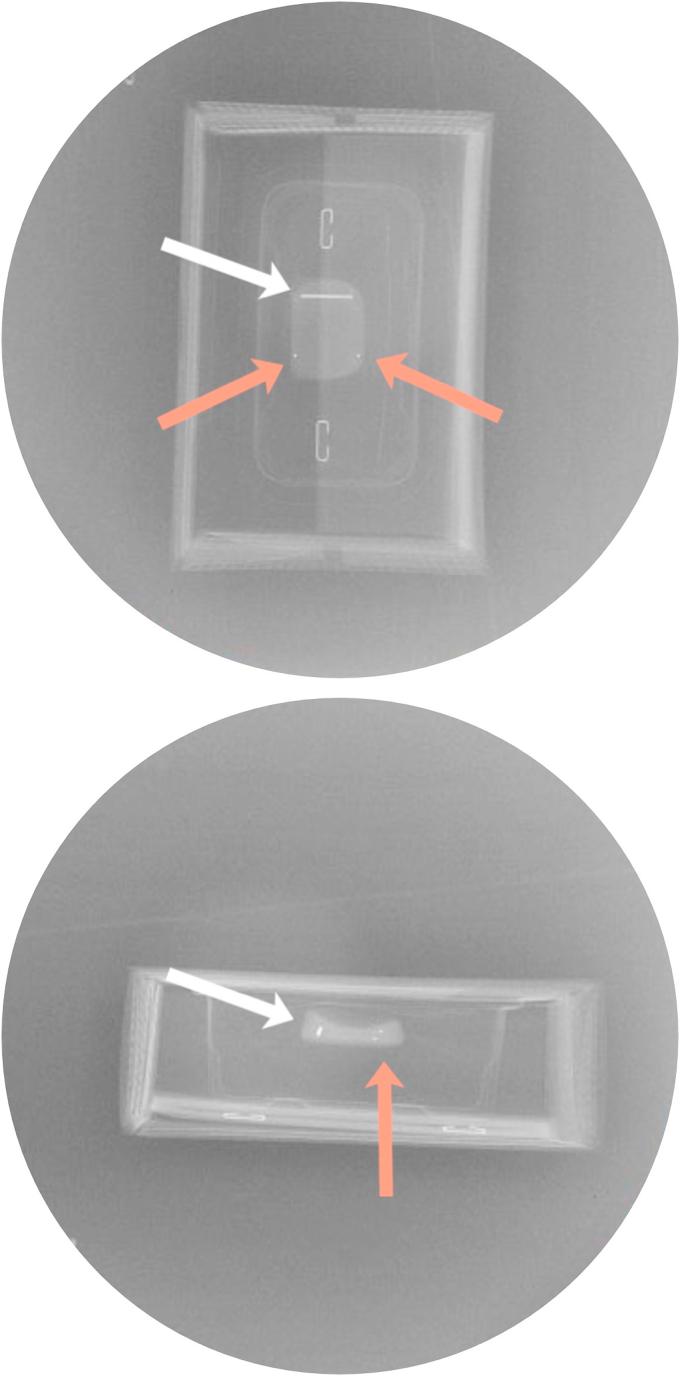
The mobile-bearing has three radiopaque markers embedded within the polyethylene – a metallic rod anteriorly and 2 metallic beads posteriorly, highlighted by white and orange arrows respectively (Fig. 4a & b). The images depict an un-implanted mobile bearing in AP and lateral views, without metal interference from the tibial tray. The traditionally recommended and accepted postoperative imaging consists of a standing AP view and a lateral view.18
Fig. 4.
a & 1b: AP and Lateral XRs of an un-implanted polyethylene mobile-bearing (Key: white arrow – metallic rod, orange arrow(s) – metallic beads). (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
The metallic markers are clearly visible on AP and could still be used to identify medial or lateral displacement of the mobile-bearing (Fig. 5). On the lateral view, all three radiopaque markers are superimposed onto the lateral wall of the tibial tray (Fig. 6). Whilst partial or complete dislocations would be easily identified on a lateral view, it would be virtually impossible assess for 180° rotational spin of the mobile-bearing on the conventional lateral view with all markers getting obscured.
Fig. 5.
AP view highlighting metallic rod and beads.
Fig. 6.
Lateral view, with no clear distinction of metallic rod and beads from the tibial tray.
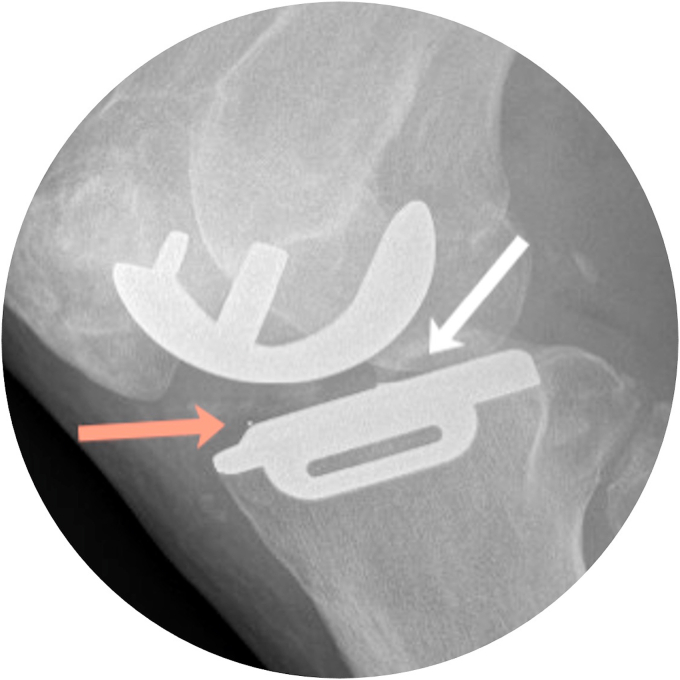
We subsequently asked our radiology colleagues to screen the Oxford Mobile Bearing on the tibial tray under XR guidance to determine an optimum view to clearly visualize the radiopaque markers. The best images were obtained with the XR source parallel to the tibial tray but angulated 10° degrees in the axial plane, projecting anteriorly. The patient is positioned in the lateral decubitus position with the operated leg under. The beam therefore projects anteriorly but remains parallel to the joint line. This modified oblique view results in clear visualization of the metallic rod, away from the lateral all of the tibial tray. An anteriorly viewed metallic rod would indicate a well oriented mobile bearing. However, if the metallic beads are visualized anteriorly without dislocation, the component would have spun 180° (Fig. 7).
Fig. 7.
Modified oblique view (Radiopaque metallic rod (white arrow) clearly visualized anteriorly, highlighting correct position of mobile-bearing).
Fig. 8, Fig. 9 highlight XRs from the same patient, depicting a conventional lateral view with complete obscuring of the metallic components. Using the modified oblique view, the component is clearly shown to have spun 180°, accounting for the patient's symptoms.
Fig. 8.
Conventional lateral view resulting in obscuring of radiopaque markers.
Fig. 9.
Modified oblique view highlighting 180° rotational spin of mobile bearing with anterior visualization of metallic beads.
5. Discussion
The UKA is an anatomic design, based on preservation of the cruciate ligaments and no manipulation of collateral tension. It therefore does not alter normal kinetic knee motion allowing the lateral compartment and intact soft tissue envelop to guide knee motion. With the fixed-bearing design, a curved femoral component sits on a flat polyethylene surface. Therefore, forces get focused on a small contact area and historically, one of the main causes of failure in both TKR and UKA was oxidation and fatigue failure of the polyethylene, with delamination of the inserts.19, 20, 21 This focused contact area was addressed in the mobile-bearing design.
The Oxford Knee was initially introduced as a bi-compartmental procedure. However, the recognition of anteromedial arthritis as a distinct early clinicopathological entity in joints with intact anterior cruciate ligaments,22 has led to medial compartment OA being the predominant pattern of arthritis being treated with UKA.23 Whilst some national joint registries do show evidence increased revision rates,4,5 many of the same registries do show better clinical results and patient reported outcomes from UKA compared to TKA.4 There is now good evidence of long-term survivorship across the globe with the Oxford Knee prosthesis.6, 7, 8,24,25
Polyethylene wear remains a major concern affecting survival of UKA in fixed-bearing implants.26, 27, 28 This has resulted in a change in practice, with increasing use of congruous mobile-bearing implants.29 However, despite numerous advantages, polyethylene bearing dislocation remains a specific complication of mobile-bearing UKA. The reported incidence varies between 0.5% and 5% in the available literature.17,24,30,31 For dislocation to occur, there has to be both distraction of the joint surface and displacement of the bearing. Displacement usually occurs due to impingement of the bearing against retained osteophytes.32,33 Joint distraction may occur as a consequence of traumatic/iatrogenic injury i.e. medical collateral ligament (MCL) injury or unequal flexion-extension gaps. Therefore, to minimize the risk of dislocation, Phase 2 and Phase 3 designs of the Oxford mobile-bearing knee introduced instrumentation to accurately balance and tension the knee intraoperatively. Additionally, asymmetrical mobile-bearing designs were introduced to counter spin. These designs had a raised, flat lateral surface to abut the tibial tray laterally and the front of the mobile bearing was about 5 mm higher than the deepest part of the bearing.33 Theoretically, this would prevent posterior dislocation by the femoral component buttressing the raised portion of the bearing. Therefore, a posterior dislocation is unlikely to occur unless to occur unless the bearing has already spun 180°.
Treatment for a mobile-bearing dislocation is adapted on a case-to-case basis and the direction of the displacement. Anterior dislocation may be treated with closed repositioning or bearing exchange, whilst posterior and medial dislocations usually require surgical intervention in the form of bearing exchange or revision arthroplasty. Rare cases of asymptomatic lateral dislocations in patients have also been described in the literature.34
180° rotational spin of the mobile bearing component is an usual complication of UKA that is difficult to recognize on traditional radiographs. Lee et al.12 in 2017 highlight 180° rotational spin as an entity in itself, and to date, this remains the sole study in the available literature. However, given the fact that ‘unexplained’ knee pain with no radiological abnormality does occur following UKA,13, 14, 15, 16, 17 we suspect the incidence of this complication may be higher, and often unaccounted for, due to the diagnostic challenges posed. Our study highlights a simple, reproducible radiological technique that consistently differentiates the radiopaque markers from the tibial tray thus allowing accurate assessment of AP orientation of the mobile bearing.
The sequence of events that results in 180° rotational spin remains a conundrum. We therefore hypothesize a possible mechanism: the pre-existing factors that inherently result in an unstable mobile bearing i.e. joint distraction with bearing displacement may result in the bearing displacing to 90° first. This non-anatomic position undoubtedly triggers pain, puts tension on the medial collateral ligament and results in restricted range of motion in the knee. In the first instance, patients would inevitably attempt to self-manipulate. If the knee is placed in valgus at any point whilst attempting to self-manipulate, the medial joint space opens up, providing enough space to fully spin 180°. Similarly, we suspect that if complete anterior or posterior dislocation has occurred, there is adequate space for the bearing to fully spin 180° prior to spontaneous relocation within the range of motion process.
Therefore, in cases where spontaneous bearing reduction has occurred following posterior dislocation, clinician should have a high index of suspicion for the mobile bearing to have rotated 180°. We therefore recommend that surgical exploration and mobile bearing exchange or revision arthroplasty should be considered in all cases to address the underlying cause for the 180° rotational spin and protect them from subsequent dislocation.
6. Conclusion
Symptomatic knee pain caused by 180° rotational spin of the mobile bearing is likely an unrecognized and therefore under-reported complication of UKA. It is therefore likely to have a higher probable incidence. Whilst traditional lateral views result in superimposition of the metallic radiopaque mobile bearing markers on the lateral wall of the tibial tray, our novel, modified radiological technique allows consistent assessment of AP orientation and as a result enable accurate diagnosis of 180° rotational spin of the mobile bearing. Clinicians should have a high index of suspicion for 180° rotational spin to have occurred in patients with posterior dislocation with or without spontaneous reduction. We therefore recommend bearing exchange ± revision arthroplasty for symptomatic patients.
The modified oblique view is now part of our immediate post-operative XR protocol. It is additionally performed on any patient who re-presents symptomatically at any stage following the index procedure.
Funding
No funding was received for this study.
CRediT author statement
All authors contributed equally and were involved in the study conceptualization, methodology and preparation, wiring and reviewing of the manuscript.
Declaration of competing interest
The authors declare no conflicts of interest.
References
- 1.Murray D.W., Parkinson R.W. Usage of unicompartmental knee arthroplasty. Bone Joint Lett J. 2018;100-B(4):432–435. doi: 10.1302/0301-620X.100B4.BJJ-2017-0716.R1. [DOI] [PubMed] [Google Scholar]
- 2.Emerson R.H., Higgins L.L. Unicompartmental knee arthroplasty with the oxford prosthesis in patients with medial compartment arthritis. J Bone Joint Surg Am. 2008;90(1):118–122. doi: 10.2106/JBJS.F.00739. [DOI] [PubMed] [Google Scholar]
- 3.Jones G.G., Kotti M., Wiik A.V. Gait comparison of unicompartmental and total knee arthroplasties with healthy controls. Bone Joint Lett J. 2016;98-B(10 Supple B):16–21. doi: 10.1302/0301-620X.98B10.BJJ.2016.0473.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liddle A.D., Pandit H., Judge A., Murray D.W. Patient-reported outcomes after total and unicompartmental knee arthroplasty: a study of 14,076 matched patients from the National Joint Registry for England and Wales. Bone Joint Lett J. 2015;97-B(6):793–801. doi: 10.1302/0301-620X.97B6.35155. [DOI] [PubMed] [Google Scholar]
- 5.Liddle A.D., Judge A., Pandit H., Murray D.W. Adverse outcomes after total and unicompartmental knee replacement in 101,330 matched patients: a study of data from the National Joint Registry for England and Wales. Lancet. 2014;384(9952):1437–1445. doi: 10.1016/S0140-6736(14)60419-0. [DOI] [PubMed] [Google Scholar]
- 6.Khanna G., Levy B.A. Oxford unicompartmental knee replacement: literature review. Orthopedics. 2007;30(5 Suppl):11–14. [PubMed] [Google Scholar]
- 7.Price A.J., Svard U. A second decade lifetable survival analysis of the Oxford unicompartmental knee arthroplasty. Clin Orthop Relat Res. 2011;469(1):174–179. doi: 10.1007/s11999-010-1506-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Svärd U.C., Price A.J. Oxford medial unicompartmental knee arthroplasty. A survival analysis of an independent series. J Bone Joint Surg Br. 2001;83(2):191–194. doi: 10.1302/0301-620x.83b2.10966. [DOI] [PubMed] [Google Scholar]
- 9.Hurst J.M., Berend K.R. Mobile-bearing unicondylar knee arthroplasty: the Oxford experience. Orthop Clin North Am. 2015;46(1):113–124. doi: 10.1016/j.ocl.2014.09.007. [DOI] [PubMed] [Google Scholar]
- 10.Schroer W.C., Barnes C.L., Diesfeld P. The Oxford unicompartmental knee fails at a high rate in a high-volume knee practice. Clin Orthop Relat Res. 2013;471(11):3533–3539. doi: 10.1007/s11999-013-3174-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Edmondson M.C., Isaac D., Wijeratna M., Brink S., Gibb P., Skinner P. Oxford unicompartmental knee arthroplasty: medial pain and functional outcome in the medium term. J Orthop Surg Res. 2011;6:52. doi: 10.1186/1749-799X-6-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee S.C., Hwang S.H., Nam C.H., Ryu S.R., Ahn H.S. The 180° spin of meniscal bearing in unicompartmental knee arthroplasty. J Orthop Surg (Hong Kong) 2017;25(3) doi: 10.1177/2309499017731630. 2309499017731630. [DOI] [PubMed] [Google Scholar]
- 13.Clement N.D., Duckworth A.D., MacKenzie S.P., Nie Y.X., Tiemessen C.H. Medium-term results of Oxford phase-3 medial unicompartmental knee arthroplasty. J Orthop Surg (Hong Kong) 2012;20(2):157–161. doi: 10.1177/230949901202000204. [DOI] [PubMed] [Google Scholar]
- 14.Epinette J.A., Brunschweiler B., Mertl P., Mole D., Cazenave A. Unicompartmental knee arthroplasty modes of failure: wear is not the main reason for failure: a multicentre study of 418 failed knees. Orthop Traumatol Surg Res. 2012;98(6 Suppl):S124–S130. doi: 10.1016/j.otsr.2012.07.002. Knee FSfHa. [DOI] [PubMed] [Google Scholar]
- 15.Baker P.N., Petheram T., Avery P.J., Gregg P.J., Deehan D.J. Revision for unexplained pain following unicompartmental and total knee replacement. J Bone Joint Surg Am. 2012;94(17):e126. doi: 10.2106/JBJS.K.00791. [DOI] [PubMed] [Google Scholar]
- 16.Hama S., Hamada D., Goto T. Revision total knee arthroplasty for unexplained pain after unicompartmental knee arthroplasty: a case report. J Med Invest. 2015;62(3-4):261–263. doi: 10.2152/jmi.62.261. [DOI] [PubMed] [Google Scholar]
- 17.Pandit H., Hamilton T.W., Jenkins C., Mellon S.J., Dodd C.A., Murray D.W. The clinical outcome of minimally invasive Phase 3 Oxford unicompartmental knee arthroplasty: a 15-year follow-up of 1000 UKAs. Bone Joint Lett J. 2015;97-B(11):1493–1500. doi: 10.1302/0301-620X.97B11.35634. [DOI] [PubMed] [Google Scholar]
- 18.Sarmah S.S., Patel S., Hossain F.S., Haddad F.S. The radiological assessment of total and unicompartmental knee replacements. J Bone Joint Surg Br. 2012;94(10):1321–1329. doi: 10.1302/0301-620X.94B10.29411. [DOI] [PubMed] [Google Scholar]
- 19.Blunn G.W., Joshi A.B., Minns R.J. Wear in retrieved condylar knee arthroplasties. A comparison of wear in different designs of 280 retrieved condylar knee prostheses. J Arthroplasty. 1997;12(3):281–290. doi: 10.1016/s0883-5403(97)90024-3. [DOI] [PubMed] [Google Scholar]
- 20.Brockett C.L., Jennings L.M., Fisher J. The wear of fixed and mobile bearing unicompartmental knee replacements. Proc Inst Mech Eng H. 2011;225(5):511–519. doi: 10.1177/2041303310393824. [DOI] [PubMed] [Google Scholar]
- 21.Reeves E.A., Barton D.C., FitzPatrick D.P., Fisher J. Comparison of gas plasma and gamma irradiation in air sterilization on the delamination wear of the ultra-high molecular weight polyethylene used in knee replacements. Proc Inst Mech Eng H. 2000;214(3):249–255. doi: 10.1243/0954411001535741. [DOI] [PubMed] [Google Scholar]
- 22.White S.H., Ludkowski P.F., Goodfellow J.W. Anteromedial osteoarthritis of the knee. J Bone Joint Surg Br. 1991;73(4):582–586. doi: 10.1302/0301-620X.73B4.2071640. [DOI] [PubMed] [Google Scholar]
- 23.Jackson W.F., Berend K.R., Spruijt S. 40 years of the oxford knee. Bone Joint Lett J. 2016;98-B(10 Supple B):1–2. doi: 10.1302/0301-620X.98B10.38076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Emerson R.H., Alnachoukati O., Barrington J., Ennin K. The results of Oxford unicompartmental knee arthroplasty in the United States: a mean ten-year survival analysis. Bone Joint Lett J. 2016;98-B(10 Supple B):34–40. doi: 10.1302/0301-620X.98B10.BJJ-2016-0480.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lisowski L.A., Meijer L.I., van den Bekerom M.P., Pilot P., Lisowski A.E. Ten- to 15-year results of the Oxford Phase III mobile unicompartmental knee arthroplasty: a prospective study from a non-designer group. Bone Joint Lett J. 2016;98 B(10 Supple B):41–47. doi: 10.1302/0301-620X.98B10.BJJ-2016-0474.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ashraf T., Newman J.H., Desai V.V., Beard D., Nevelos J.E. Polyethylene wear in a non-congruous unicompartmental knee replacement: a retrieval analysis. Knee. 2004;11(3):177–181. doi: 10.1016/j.knee.2004.03.004. [DOI] [PubMed] [Google Scholar]
- 27.Parratte S., Argenson J.N., Pearce O., Pauly V., Auquier P., Aubaniac J.M. Medial unicompartmental knee replacement in the under-50s. J Bone Joint Surg Br. 2009;91(3):351–356. doi: 10.1302/0301-620X.91B3.21588. [DOI] [PubMed] [Google Scholar]
- 28.Argenson J.N., Parratte S. The unicompartmental knee: design and technical considerations in minimizing wear. Clin Orthop Relat Res. 2006;452:137–142. doi: 10.1097/01.blo.0000229358.19867.60. [DOI] [PubMed] [Google Scholar]
- 29.Erdem Y., Neyisci C., Yıldız C. Mid-term clinical and radiological results of oxford phase 3 medial unicompartmental knee arthroplasty. Cureus. 2019;11(9) doi: 10.7759/cureus.5674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lee S.Y., Bae J.H., Kim J.G. The influence of surgical factors on dislocation of the meniscal bearing after Oxford medial unicompartmental knee replacement: a case-control study. Bone Joint Lett J. 2014;96-B(7):914–922. doi: 10.1302/0301-620X.96B7.33352. [DOI] [PubMed] [Google Scholar]
- 31.Choy W.S., Kim K.J., Lee S.K., Yang D.S., Lee N.K. Mid-term results of oxford medial unicompartmental knee arthroplasty. Clin Orthop Surg. 2011;3(3):178–183. doi: 10.4055/cios.2011.3.3.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.van Tienen T.G., Taylor S.J., Brink R.B. Successful salvage of a recurrently dislocating Oxford medial unicompartmental bearing. J Arthroplasty. 2010;25(3) doi: 10.1016/j.arth.2009.02.010. 497.e17-9. [DOI] [PubMed] [Google Scholar]
- 33.Tibrewal S., Pandit H., McLardy-Smith P., Tibrewal S.B., Murray D.W. Posterior dislocation of the Oxford knee meniscal bearing: a treatment option. J Orthop Traumatol. 2014;15(1):59–62. doi: 10.1007/s10195-013-0250-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fujii T., Matsui Y., Noboru M., Inagaki Y., Kadoya Y., Tanaka Y. Meniscal bearing dislocation of unicompartmental knee arthroplasty with faint symptom. Case Rep Orthop. 2015;2015:217842. doi: 10.1155/2015/217842. [DOI] [PMC free article] [PubMed] [Google Scholar]