Abstract
Introduction
The WHO declared 2019 severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) a public health emergency of international concern. The National and Regional Health System has been reorganized, and many oncological patients died during this period or had to interrupt their therapies. This study summarizes a single-centre experience, during the COVID-19 period in Italy, in the treatment of brain metastases with Gamma Knife stereotactic radiosurgery (GKRS).
Methods
We retrospectively analysed our series of patients with brain metastases who underwent GKRS at the Niguarda Hospital from February 24 to April 24, 2020.
Results
We treated 30 patients with 66 brain metastases. A total of 22 patients came from home and 8 patients were admitted to the emergency room for urgent neurological symptoms. Duration of stay was limited to 0–1 day in 17 patients. We chose to treat a cluster of 9 patients, whose greater lesion exceeded 10 cm3, with 2-stage modality GKRS to minimize tumour recurrence and radiation necrosis.
Conclusion
Due to the COVID-19 pandemic, the whole world is at a critical crossroads about the use of health care resources. During the COVID-19 outbreak, the deferral of diagnostic and therapeutic procedures and a work backlog in every medical specialty are the natural consequences of reservation of resources for COVID-19 patients. GKRS improved symptoms and reduced the need for open surgeries, allowing many patients to continue their therapeutic path and sparing beds in ICUs. Neurosurgeons have to take into account the availability of stereotactic radiosurgery to reduce hospital stay, conciliating safety for patients and operators with the request for health care coming from the oncological patients and their families.
Keywords: COVID-19, Gamma Knife, Radiosurgery, Brain metastases
Introduction
In January 30, 2020, the WHO declared 2019 coronavirus disease (COVID-19), caused by a novel beta coronavirus known as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), a public health emergency of international concern [1]. Italy, first of the rest of Europe, has experienced the outbreak of COVID-19. In a population of 195,351 confirmed cases at the date of April 25, 26,384 deaths from COVID-19 [2] have been caused by multiple organ dysfunction syndrome or respiratory failure, especially in patients with comorbidities and older than 60 years, with greater epidemic diffusion in Lombardy, the most populated Italian region (over 10 million of inhabitants) [3].
Since the severe respiratory failure due to COVID-19 needs ICU beds and generally an increase of hospital capabilities including personnel, the National Health System and its related regional system have been converted to sustain the epidemic. The goal was to shift every specialty assistance only to the care of COVID-19 patients. In March 8, 2020, the Lombardy Governor (decree No. XI/2906) [4] suspended elective surgical activities in the hospital (nonurgent inpatient and outpatient). The regional medical system has been completely reorganized, with a large number of physicians and nurses from different specialties converted to the COVID-19 patients care.
Patients with cancer are more susceptible to infections than individuals without cancer because of their organic frailty and systemic immunosuppression caused by the disease and anticancer treatments. Therefore, these patients carry an increased risk of COVID-19 infection and have a poorer prognosis, and many oncological patients died during this period or had to interrupt their therapies; the consequences were relevant for physicians and researchers in the oncology field [5].
From 24 February, 2020, since our hospital has been alerted to the epidemic, to avoid that patients with brain metastases deferred adequate radiosurgical treatment, we started to modify our routine and, according to the existing directives on the management of these patients, we put in place a modification of hospitalization procedures [6].
This paper briefly summarizes a single-centre experience in the treatment of a specific population of patients with cancer and brain metastases treated with Gamma Knife Perfexion® (Elekta AB, Stockholm, Sweden) stereotactic radiosurgery (GKRS), during a 2-month period, from 24 February to 24 April, 2020. In our institution, GKRS is carried out by a multidisciplinary workgroup involving neurosurgeons, radiation oncologists, physicists, and a staff of nurses, and radiographers. It is an elective therapeutic activity, however, for its features (non-invasive procedure, a brief hospital stay, and no need for intensive care), it may play a role in this dramatic period [7, 8, 9].
Methods
We retrospectively analysed our series of patients with brain metastases who underwent GKRS in our institution from 24 February to 24 April, during the COVID-19 pandemic. Demographical data and information about primary disease and radiosurgical plans were collected. We describe the whole process of selection of patients suitable for GKRS, their admission to the hospital, and the radiosurgical procedure from positioning of stereotactic frame to its removal, with particular attention to safety and hygienic procedures.
Results
We treated 30 patients (M:F ratio 1.14:1, mean age 68.7 ± 8.97 years) with 66 brain metastases (mean 2.2, range 1–7). The primary tumour site was the lung in 14 patients (46.6%), colon in 5 patients (16.6%), breast in 4 patients (13.3%), melanoma in 2 patients (6.6%), SCLC in 2 patients (6.6%), kidney in 2 patients (6.6%), salivary in 1 patient (3.3%). Demographical data and disease information are shown in Table 1.
Table 1.
Summary of patient characteristics
| Patient | Sex (M/F) | Age (years) | Metastases | Primary tumour | Mass effect (yes/no) | GK (single/2-stage) | Length of stay (days) | Provenance (scheduled/urgent) | Notes |
|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 80 | 3 | colon | no | 2-stage | 1 | Scheduled | |
| 2 | F | 71 | 7 | lung | no | single | 1 | Scheduled | |
| 3 | F | 81 | 1 | melanoma | no | single | 21 | Urgent | |
| 4 | M | 71 | 1 | lung | yes | 2-stage | 9 | Urgent | |
| 5 | M | 80 | 3 | lung | no | single | 0 | Scheduled | |
| 6 | F | 73 | 6 | breast | no | single | 0 | Scheduled | |
| 7 | F | 77 | 1 | melanoma | no | single | 0 | Scheduled | |
| 8 | F | 57 | 2 | lung | no | single | 0 | Scheduled | |
| 9 | F | 66 | 3 | lung | no | single | 0 | Scheduled | |
| 10 | F | 71 | 2 | lung | no | single | 0 | Scheduled | |
| 11 | F | 73 | 1 | lung | yes | 2-stage | 12 | Urgent | |
| 12 | M | 69 | 2 | lung | no | single | 0 | Scheduled | |
| 13 | M | 61 | 1 | SCLC | no | single | 0 | Scheduled | |
| 14 | M | 61 | 4 | lung | yes | 2-stage | 18 | Urgent | Cyst drainage and biopsy |
| 15 | F | 54 | 1 | breast | no | single | 0 | Scheduled | |
| 16 | F | 67 | 1 | breast | no | 2-stage | 0 | Scheduled | |
| 17 | M | 76 | 5 | salivary | no | single | 0 | Scheduled | |
| 18 | M | 79 | 2 | lung | no | 2-stage | 14 | Urgent | |
| 19 | F | 50 | 1 | colon | yes | 2-stage | 10 | Urgent | |
| 20 | M | 68 | 1 | colon | yes | 2-stage | 14 | Urgent | EVD |
| 21 | F | 84 | 3 | lung | no | single | 18 | Urgent | |
| 22 | M | 60 | 2 | colon | no | single | 4 | Scheduled | |
| 23 | F | 55 | 1 | breast | no | single | 1 | Scheduled | |
| 24 | M | 62 | 1 | SCLC | no | 2-stage | 11 | Urgent | |
| 25 | M | 70 | 2 | kidney | no | single | 0 | Scheduled | |
| 26 | M | 61 | 1 | kidney | no | single | 8 | URGENT | |
| 27 | M | 80 | 1 | colon | no | single | 0 | Scheduled | |
| 28 | M | 71 | 1 | lung | no | single | 0 | Scheduled | |
| 29 | F | 73 | 1 | lung | no | single | 4 | Scheduled | |
| 30 | M | 61 | 5 | lung | no | single | 3 | Scheduled |
All treated patients were COVID-19-free confirmed cases. Twenty-two patients coming from home were selected by phone or video calling by our telenursing service usually adopted for follow-up to exclude the existence of clinical signs of infectious disease. No patient developed symptoms of COVID-19 infection during hospitalization.
At the hospital triage, fever scan and clinical examination to assess the absence of signs were performed, and, starting from April 4, 2020, nasopharyngeal swab for COVID-19 testing was done 48 h before treatment in an outpatient setting.
Eight patients were admitted to the emergency room for urgent neurological symptoms. An urgent brain CT scan was performed in all these cases and revealed lesions suspected for brain metastases; therefore, a lung and abdomen CT scan was performed to search for systemic disease as well as to exclude interstitial pneumonia, the COVID-19 test result made at emergency room entry not yet being available.
Out of these 30 patients, 8 patients were admitted in departments (Oncology and Medicine COVID-free) different than Neurosurgery, which was particularly overloaded by being one of three regional hubs for neurosurgical emergencies [10]. In several cases, we exploited simultaneous hospital access for scheduled administration of systemic therapy. All patients wore a surgical mask from admission to discharge, as well as during the whole radiosurgical procedure (from stereotactic frame fixation to its removal); they performed hand hygiene and hair washing before treatment. During frame manoeuvres, neurosurgeons and nurses were provided with adequate individual protective equipment (surgical mask, gown, gloves, and face shield) due to the brief distance from the nose and mouth of the patient, even though they took direct care to non-COVID-19 patients. In the other steps of GKRS workflow (imaging, planning, and positioning in the couch for treatment), the entire staff worked with the medical mask [11].
After the procedure, the frame was decontaminated with Antisapril® (active chlorine from sodium hypochlorite) then sterilized by autoclave. Finally, we observed to look after the patient by ensuring general safety. Visitors to inpatients were forbidden, but in the phase of radiosurgical planning, the patient in rest waiting for the treatment could talk with familiars by phone. The length of stay in the hospital was limited to 0–1 day in 17 out of 22 (77.2%) scheduled patients. In all other cases, the mean length of stay was 11.23 ± 5.71 days.
All patients were excluded for resection surgery after multidisciplinary oncologic evaluation, even though in five cases an evident mass effect was present. Three patients were affected from known oncologic disease with prognosis quoad vitam greater than 6 months. Two patients had unknown primitive disease: the first had a frontal cystic lesion that was stereotactically drained (with insertion of Ommaya reservoir) to reduce mass effect and to make the diagnosis (lung adenocarcinoma); then, he was treated with GKRS in two stages; the second patient had a posterior fossa tumour causing hydrocephalus, he was treated immediately after admission with external ventricular drainage, and was then submitted to GKRS in 2-stage modality. Between the two stages, a biopsy of the cecal lesion, detected by abdomen CT scan, was performed and histopathologic diagnosis of colon adenocarcinoma was made. We chose to treat a cluster of 9 patients, whose greater lesion exceeded 10 cm3, with 2-stage modality GKRS (12 Gy to total volume in two sessions, 4 weeks apart) rather than palliative GKRS to minimize tumour recurrence and radiation necrosis [12].
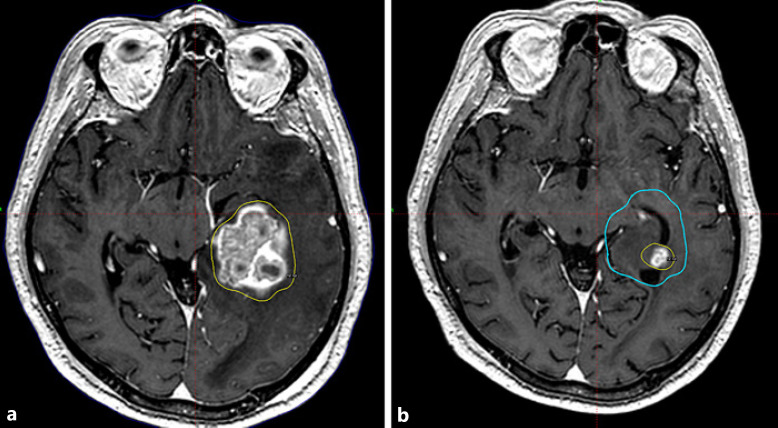
Five of these patients underwent the second stage of their treatment in the time span described in this article (see Fig. 1).
Fig. 1.
Case of a 50-year-old female with a large single brain metastasis from colon cancer treated with 2-stage GKRS. a First stage. Yellow line: prescription isodose 12 Gy at 50%. b Second stage. Blue line: overlapped prescription isodose of first stage. Yellow line: prescription isodose 12 Gy at 50%.
Discussion
Patients with cancer are more susceptible to infections than individuals without cancer because of their organic frailty and systemic immunosuppression caused by the disease and anticancer treatments. 2019 coronavirus disease (COVID-19) caused by a novel beta coronavirus known as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a public health emergency of international concern. Due to the COVID-19 pandemic, the whole world is at a critical crossroads about the use of health care resources. This issue is strengthened in the Italian National Health System because it is based on universality, solidarity, and uniformity, and the Italian Constitutional Law recognises the right of every individual to receive all necessary health care [13].
Wide use of telemedicine is the very innovation in this horrible period. It was useful for the management of patients to reduce travelling, hospital access, and risk of contracting coronavirus, for the screening of candidates to treat and to effectively share knowledge with other specialist of our staff.
During the COVID-19 outbreak, which will have probably a long period of diffusion with a high risk of recrudescence, efforts and resources (personnel, hospital beds, ventilators, etc.) shall be reserved for COVID-19 patients with the natural consequence of the deferral of diagnostic and therapeutic procedures and a work backlog in every medical specialty [14].
Conclusion
In our experience, the use of GKRS improved symptoms and reduced the need for open surgical operations, allowing many patients to continue their targeted or immunologic therapies or to start primary systemic treatments, and moreover to spare beds and intensive care. In order to improve patient selection, optimizing risk reduction for health care workers and patients, we suggest performing a pre-hospitalization triage through phone calling and questionnaire. All patients with no symptoms of COVID-19 infection and no recent contacts with COVID-19-positive patients, after a negative nasopharyngeal swab test for COVID-19 performed 48 h before admission, should be treated. In order to rationalize resources, neurosurgeons have to take into account the availability of stereotactic radiosurgery (both Gamma and X rays-based apparatus) to reduce hospital inpatient stay and conciliating safety for patients and operators with the request for health care coming from the patients with cancer and their families.
Statement of Ethics
The paper is exempt from ethical committee approval, since it is a retrospective, anonymized analysis. All patients signed an informed consent to treatment which included a consent to use anonymized data for scientific purposes.
Disclosure Statement
The authors have no conflicts of interest to declare.
Funding Sources
No funding was received.
Authors Contributions
Francesco Maria Crisaà designed the study and wrote and edited the paper. Filippo Leocata collected the data. Virginia Maria Arienti collected the data. Marco Picano collected the data and edited the paper. Luca Berta collected the data. Hae Song Mainardi collected the data. Angelo Filippo Monti collected the data. Francesco Musca collected the data. Silvia Colombo collected the data. Mauro Palazzi collected the data. Alessandro La Camera designed the study and wrote the paper.
Acknowledgements
A special tribute to all colleagues who fight against the coronavirus, even at cost of their life, allowing us to continue our work.
References
- 1.WHO Director-General's statement on IHR Emergency Committee on Novel Coronavirus (2019-nCoV) https://www.who.int/dg/speeches/detail/who-director-general-s-statement-on-ihr-emergency-committee-on-novel-coronavirus-(2019-ncov)[last accessed: May, 5th 2020]
- 2.National COVID-19 Trends. https://github.com/pcm-dpc/COVID-19/blob/master/dati-andamento-nazionale/dpc-covid19-ita-andamento-nazionale-20200425.csv [last accessed: May, 7th 2020]
- 3.Lombardy Population. http://dati.istat.it/Index.aspx?QueryId=18548#[last accessed: May, 7th 2020]
- 4.Deliberazione Xi/2906. www.regione.lombardia.it > connect > DGR+2906+8+marzo+2020 [last accessed: May, 5th 2020]
- 5.The Lancet Oncology COVID-19: global consequences for oncology. Lancet Oncol. 2020 Apr;21((4)):467. doi: 10.1016/S1470-2045(20)30175-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Recommendations for the management of oncological and onco-hematological patients during COVID-19 emergency. http://www.trovanorme.salute.gov.it/norme/renderNormsanPdf?anno=2020&codLeg=73635&parte=1%20&serie=null [last accessed: May, 5th 2020]
- 7.Guidance for Stereotactic Radiosurgery during COVID-19 pandemic. https://www.rcr.ac.uk/sites/default/files/stereotactic-radiosurgery-srs-covid19.pdf [last accessed: May, 5th 2020]
- 8.Pannullo SC, Chidambaram S, Brandmaier A, Knisely J, Adler JR., Jr Clinical Considerations in Neurosurgical Radiosurgery in the Time of COVID-19. Cureus. 2020 Apr;12((4)):e7671. doi: 10.7759/cureus.7671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Muhammad S, Tanikawa R, Lawton MT, et al. Letter: Safety Instructions for Neurosurgeons During COVID-19 Pandemic Based on Recent Knowledge and Experience. Neurosurgery. 2020 Aug;87((2)):E220–1. doi: 10.1093/neuros/nyaa184. https://doi.org/ https://doi.org/10.1093/neuros/nyaa184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zoia C, Bongetta D, Veiceschi P, Cenzato M, Di Meco F, Locatelli D, et al. Neurosurgery during the COVID-19 pandemic: update from Lombardy, northern Italy [published online ahead of print, 2020 Mar 28] Acta Neurochir (Wien) 2020 Jun;162((6)):1221–2. doi: 10.1007/s00701-020-04305-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.WHO Rational use of personal protective equipment for coronavirus disease (COVID-19) and considerations during severe shortages. https://apps.who.int/iris/bitstream/handle/10665/331695/WHO-2019-nCov-IPC_PPE_use-2020.3-eng.pdf [last accessed: May, 5th 2020]
- 12.Serizawa T, Higuchi Y, Yamamoto M, Matsunaga S, Nagano O, Sato Y, et al. Comparison of treatment results between 3- and 2-stage Gamma Knife radiosurgery for large brain metastases: a retrospective multi-institutional study. J Neurosurg. 2018 Sep;131((1)):227–37. doi: 10.3171/2018.4.JNS172596. [DOI] [PubMed] [Google Scholar]
- 13.Remuzzi A, Remuzzi G. COVID-19 and Italy: what next? Lancet. 2020 Apr;395((10231)):1225–8. doi: 10.1016/S0140-6736(20)30627-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ramakrishna R, Zadeh G, Sheehan JP, Aghi MK. Inpatient and outpatient case prioritization for patients with neuro-oncologic disease amid the COVID-19 pandemic: general guidance for neuro-oncology practitioners from the AANS/CNS Tumor Section and Society for Neuro-Oncology [published online ahead of print, 2020 Apr 9] J Neurooncol. 2020 May;147((3)):525–9. doi: 10.1007/s11060-020-03488-7. [DOI] [PMC free article] [PubMed] [Google Scholar]