Abstract
Objective
To describe nurse hand hygiene practices in the home health care (HHC) setting, nurse adherence to hand hygiene guidelines, and factors associated with hand hygiene opportunities during home care visits.
Design
Observational study of nurse hand hygiene practices.
Setting
and Participants: Licensed practical/vocational and registered nurses were observed in the homes of patients being served by a large nonprofit HHC agency.
Methods
Two researchers observed 400 home care visits conducted by 50 nurses. The World Health Organization's “5 Moments for Hand Hygiene” validated observation tool was used to record opportunities and actual practices of hand hygiene, with 3 additional opportunities specific to the HHC setting. Patient assessment data available in the agency electronic health record and a nurse demographic questionnaire were also collected to describe patients and nurse participants.
Results
A total of 2014 opportunities were observed. On arrival in the home was the most frequent opportunity (n = 384), the least frequent was after touching a patient's surroundings (n = 43). The average hand hygiene adherence rate was 45.6% after adjusting for clustering at the nurse level. Adherence was highest after contact with body fluid (65.1%) and lowest after touching a patient (29.5%). The number of hand hygiene opportunities was higher when patients being served were at increased risk of an infection-related emergency department visit or hospitalization and when the home environment was observed to be “dirty.” No nurse or patient demographic characteristics were associated with the rate of nurse hand hygiene adherence.
Conclusions and Implications
Hand hygiene adherence in HHC is suboptimal, with rates mirroring those reported in hospital and outpatient settings. The connection between poor hand hygiene and infection transmission has been well studied, and it has received widespread attention with the outbreak of SARS-CoV-2. Agencies can use results found in this study to better inform quality improvement initiatives.
Keywords: Infection control, hand hygiene, home care services, home health nursing
Infection is a significant cause of morbidity and preventable deaths, can have emotional consequences for patients and their family, and is associated with high health care costs.1 Infection prevention and control is a top priority across health care settings to ensure high quality of care and patient safety.2 Hand hygiene to reduce pathogen transmission and prevent infections is one foundational approach for effective infection prevention and control.3 The Centers for Disease Control and Prevention (CDC) and World Health Organization (WHO) have published guidelines for hand hygiene in health care settings.1 , 4 Improving adherence to hand hygiene recommendations has become an important goal for health care organizations5 and received significant additional attention with the outbreak of SARS-CoV-2.6 , 7
Most hand hygiene studies to date have been conducted in the inpatient and emergency department settings, with limited evidence in post-acute care settings such as nursing homes.8 Only 1 study, an observation study of practices, has been conducted in an Australia home health care (HHC) setting.9 Findings indicated a 59.2% hand hygiene adherence rate, but this study was limited by a small sample size (8 nurses, 40 HHC visits).
HHC includes skilled, largely post-acute care provided in the patient's home environment. Use of HHC has increased over the past decade to meet the health care needs of the growing aging population and as a result of incentives to discharge patients from the hospital sooner.10 , 11 US HHC spending reached $102.2 billion in 2018,12 which is up 30% compared with home health spending 5 years ago. The Centers for Medicare & Medicaid Services projects home health spending rate to surpass all other care categories in the next 10 years.11 Compared with hospital and nursing home settings, nurses in HHC work under less direct supervision, changing environments, and with limited space and resources. To address the gap in our understanding of HHC practices, we observed HHC nurses' hand hygiene adherence over a large number of nurses and patient visits and examined factors associated with hand hygiene adherence.
Methods
Sample and Settings
This study was conducted in a large, US nonprofit certified home health agency serving both urban and suburban neighborhoods, with approximately 100,000 new patient cases and more than 1 million home visits per year. Observations were conducted in the homes of patients who were admitted to the adult acute care program. The Joint Commission suggests a minimum of 200 opportunities for hand hygiene as appropriate for meaningful comparisons.13 A targeted sample size of 50 nurses (licensed practical or vocational and registered nurses) and 400 observations (8 patient visits per nurse) was selected to provide adequate statistical power to estimate nurse adherence rates and associated characteristics.
Nurses were recruited with purposive sampling to ensure variation in geographic location and level of experience in HHC. Nurses were informed that the study team was interested in infection control and prevention in HHC but were not told specifically what infection control and prevention activities were going to be recorded. Patients were alerted that a researcher would be accompanying the nurse on the visit and gave verbal agreement in advance. Observers confirmed patient agreement on arrival to the home. The institutional review boards at the study agency and collaborating academic partner reviewed and approved the study protocol.
Observations Tools
The research team used 2 observation checklists. The hand hygiene observation checklist includes 8 moments that trigger an opportunity for transmission of pathogens (or microorganisms that may cause infection) and the need for hand hygiene. Five of the 8 opportunities for hand hygiene were taken directly from the WHO “5 Moments of Hand Hygiene” checklist14 , 15—these include “Before patient contact,” “Before aseptic task,” “After body fluid exposure risk,” “After patient contact,” and “After contact with patient surroundings.” The WHO 5 Moments have been validated and implemented globally and are considered the minimal essential moments. Instructions on the checklist suggest observing other moments important to protecting the “patient zone.”16 The 3 additional opportunities are home care–specific and based on home health industry guidelines.17 , 18 They are “Upon arrival in home,” “Before leaving patient's home,” and “Before accessing clean compartment of nursing bag.” Observers used the checklists to record when they witnessed one of these moments and hand hygiene adherence related to that moment. Hand hygiene adherence was noted if the nurse either completed handwashing with soap and water or used an alcohol-based hand rub. An 8-item home environment checklist was also developed based on a review of the literature to identify barriers that could hinder a clinician's ability to practice hand hygiene or distract them from achieving best practices when providing care in the home setting.19, 20, 21, 22 The barriers include poor lighting, clutter, infestations, pets, no running water, unruly children, dirty environment, and poor patient hygiene as assessed by the visiting observer.
Other Data Collected
Observation data were supplemented by a nurse demographic and work history survey along with data from the Outcomes Assessment and Information Set (OASIS), a standardized patient assessment required for all Medicare-certified HHC agencies nationwide by Centers for Medicare & Medicaid Services. The OASIS measures several domains of HHC patient characteristics including sociodemographic, medical history, health status, environmental, support system, and functional status.
A patient-level propensity for 4 types of infection (respiratory, urinary tract, wound, and intravenous catheter–related) that could lead to an emergency department visit or hospitalization during the HHC admission was obtained by extrapolating a predictive model onto the OASIS data for patients served by nurses in this observation study; here on termed “propensity of infection.” The methodology for the predictive model and risk stratification have been described by this team elsewhere.23
Training of Observers
Two researchers were trained by the investigators and the agency educators to observe hand hygiene and other infection prevention and control practices. Training included orientation to the WHO “Moments for Hand Hygiene” observation tool, reviewing WHO- and agency-produced training videos14 , 15 and attending agency skills laboratory classes. The videos cover topics including basic hand hygiene, bag technique, wound care, and urinary catheter insertion. Interrater reliability was tested and achieved firstly through using the observation tool to rate videos of HHC visits, followed by 2 joint field visits (Kappa = 1; 100% agreement). The observers completed an additional tandem visit halfway through data collection to confirm consistency.
Analyses
The number of times hand hygiene was completed and the number of hand hygiene opportunities was tallied for each observation visit. Adherence rates were estimated from intercept-only regression models that controlled the nested structure of visits observed for the same nurse by specifying nurse-level random intercept. A Poisson model was used for most opportunity types model to account for the nature of count data by specifying the number of adherent opportunities as the dependent variable and the log number of opportunities as the offset. Logistic regression was used for opportunity types, where a maximum of 1 opportunity was observed across all visits. Eight patients did not have clinical record data available. We imputed the propensity of infection for these patients based on mean and model values from the remaining patient sample.
Multivariate regression analyses were used to explore the nurse- and patient-level characteristics associated with number of hand hygiene opportunities per visit and rate of adherence to these opportunities. Nurse education, patient's propensity for infection, and environmental variables were considered for these analyses. We excluded variables that had bivariate relationships with P value > .2 from likelihood ratio tests from the regression specifications described below for each dependent variable (not shown here). Several environmental variables met the bivariate criteria, but because of high multicollinearity among environmental variables, only dirty environment and patient hygiene were included because they had the highest F test associated with the opportunity and adherence analysis, respectively. We compared the effect of the midpoints of each propensity of infection risk stratification over this nonlinear relationship and conducted multiple comparison analysis with Bonferroni corrections. The patients' propensity of infection was forced into the adherence rate model to control for any patient-level characteristics that are associated with infection and increased opportunities.
The multivariate adherence rate model is an extension of the intercept-only models described earlier. We specified a quasi-Poisson regression to control for the underdispersion observed in this analysis for both opportunities and adherence rate. The analysis of both models were conducted using generalized additive models to explore the nonlinear relationships of the continuous variables in the study.24 , 25
Results
Fifty nurses were enrolled in the study, most of whom (n = 48) were observed for 8 visits. One nurse was observed for 7 visits and another for 9 visits. Together, a total of 400 observations of nurse visits to patients were completed. Nurse and patient characteristics are presented in Table 1 . The majority of nurses (90%) were female, with an average age of 47 years, and employed on a full-time, salaried basis. Eighty-eight percent of nurses had a bachelor's degree in nursing or higher. Four hundred patient visits were observed across 397 unique patients; 3 individual patients were cared for by 2 different nurses on separate visits. Table 2 presents demographic and clinical characteristics for 389 patients (excluding 8 patients without clinical data). The majority (60%) were female with an average age of 74 years. Forty percent of the patients were white non-Hispanic, 27% black non-Hispanic, 25% Hispanic, and 8% other race non-Hispanic. Forty percent (n = 157) of patients were found to have a high or very high risk of developing an infection that would lead to a hospitalization or emergent care event, according to the propensity of infection risk prediction model. Some of the specific characteristics contributing to the risk level are also presented in Table 2.
Table 1.
Nurse Participant Characteristics (N = 50)
| Age, mean (SD) | 47.4 (10.6) |
| Female, n (%) | 45 (90) |
| Race/ethnicity, n (%) | |
| White, Non-Hispanic | 13 (26) |
| Black or African American, Non-Hispanic | 22 (44) |
| Hispanic | 5 (10) |
| Other, Non-Hispanic | 10 (20) |
| Highest level of professional training, n (%) | |
| Licensed practical nurse (LPN)/licensed vocational nurse (LVN) | 4 (8) |
| Associate's degree in nursing | 7 (14) |
| Bachelor's degree in nursing | 33 (66) |
| Master's degree in nursing | 6 (12) |
| Years of experience, n (%) | |
| Years as a nurse, mean (SD) | 19.3 (11.7) |
| Years at study agency, mean (SD) | 10.6 (7.8) |
| Employment status, n (%) | |
| Full-time, salaried | 44 (88) |
| Per diem | 6 (12) |
Table 2.
Selected Patient Characteristics
| Patient Characteristics (N = 389) | n (%) |
|---|---|
| Demographics | |
| Age (mean, SD) | 73.58 (15.7) |
| Female | 233 (59.9) |
| Race/ethnicity | |
| White, Non-Hispanic | 157 (40.4) |
| Black or African American, Non-Hispanic | 103 (26.5) |
| Hispanic | 98 (25.2) |
| Other, Non-Hispanic | 31 (8.0) |
| Payer | |
| Medicare only | 236 (60.7) |
| Medicaid only | 40 (10.3) |
| Dual eligible | 51 (12.8) |
| Other | 62 (16.2) |
| Home environmental factors that could interfere with good infection control practice: 3 most prevalent conditions | |
| Clutter | 158 (39.5) |
| Poor lighting | 155 (38.8) |
| Dirty | 114 (28.5) |
| Propensity for and Infection-related emergent care event | |
| Low | 139 (35.7) |
| Moderate | 93 (23.9) |
| High | 57 (14.7) |
| Very high | 100 (25.7) |
| Selected infection risk contributors | |
| Lives with others | 238 (61.2) |
| Multiple hospitalizations in past 12 months | 123 (31.6) |
| Presence of one or more wounds | 196 (50.4) |
| No. of ADL and instrumental ADL dependencies requiring human assistance, mean (SD) | 6.8 (3.3) |
| Memory deficit | 35 (9.0) |
| Respiratory treatments at home | 32 (8.2) |
| Presence of a urinary catheter | 29 (7.5) |
| Urinary incontinence | 110 (28.5) |
| No caregiver or caregiver unlikely to provide assistance with medical procedures or treatments (eg, changing wound dressing) | 61 (15.7) |
ADL, activities of daily living.
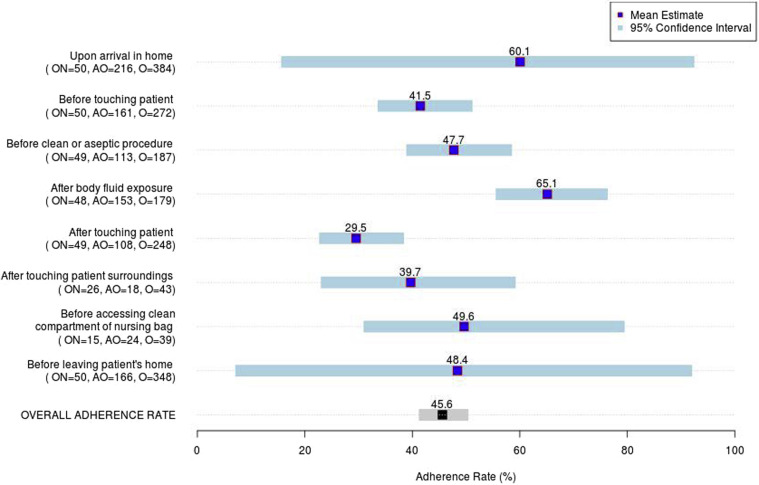
A total of 2,014 hand hygiene opportunities were observed across the 400 visits, an average of 5 (variance = 2.2) opportunities per visit. The unadjusted average opportunity-level hand hygiene adherence rate was 47.6% [95% confidence interval (CI) = 45.4, 49.8]. After adjusting for clustering at the nurse level, the average adherence rate was 45.6% (95% CI = 41.3, 50.4) (see Figure 1 ). The most frequently observed opportunities for hand hygiene were on arrival to the patient's home (n = 384), before patient contact (n = 372), after touching a patient (n = 349), and before leaving the patient's home (n = 348). Adherence was highest (65.1%) after removing gloves when the procedure included contact with body fluid and lowest after touching a patient (29.5%). Adherence to the home care–specific moments were 60.1% on arrival, 49.6% before accessing clean compartment of nursing bag, and 48.4% before leaving. The wide CIs for on arrival and before leaving the patient's home suggest there is wide variability in the nurses' hand hygiene practice in this study.
Fig. 1.
Nurse-level hand hygiene rate by opportunity. Estimates are obtained from the intercept in either a Poisson or logistic specification in the generalized linear model where nurses are defined as a random intercept. All adherence types are specified as Poisson; except logistic regression was used for on arrival in home, after touching surroundings, and before leaving surroundings opportunity types because a maximum of 1 opportunity was observed across all visits. Each estimate of adherence rate shown above is translated back from the link function to a probability. In parentheses, the following notation is used: ON, the number of nurses with at least one hand hygiene opportunity present at a visit; AO, number of hand hygiene adherent opportunities; O, number of opportunities observed.
Drivers of Hand Hygiene Opportunities and Nurse Adherence
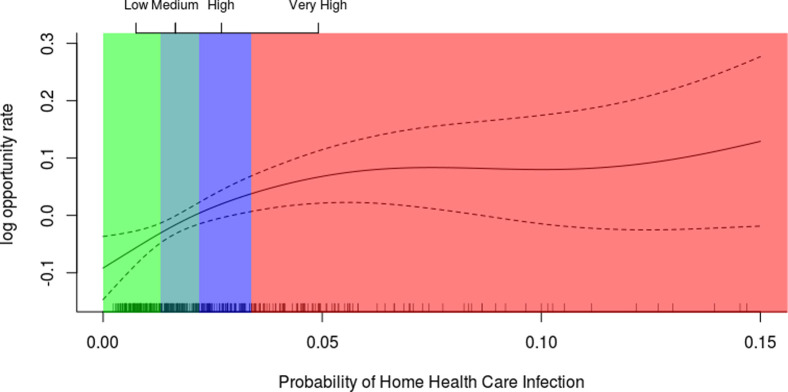
Regression analyses (Table 3 , left side of panel) indicated that the average number of hand hygiene opportunities increased by 1.08 (P < .01) when a patient was observed to live in a dirty environment compared with those who did not live in a dirty environment after controlling for the patient's propensity for infection. Further, the patient-level propensity for infection was strongly positively associated (P < .01) with the hand hygiene opportunity rate after controlling for dirty environment. Figure 2 demonstrates that as the propensity for infection increases (x-axis), the log opportunity rate (y-axis) also increases, leveling off through very high risk. The shading is provided for reference to describe the level of propensity for infection risk. Although the very high risk makes up only 25% of this population, it has the most variability, indicated by each hash on the axis representing one patient's propensity for infection. A patient identified as having a high risk of an infection-related outcome had on average 0.38 more hand hygiene opportunities per visit than a patient at low risk (P < .01). Similarly, a patient identified as having a very high risk of an infection-related outcome had an average of 0.63 (P < .05) more hand hygiene opportunities on average than a patient who was identified as low risk.
Table 3.
Drivers of Hand Hygiene Opportunities During Home Care Visits and Nurse Hand Hygiene Adherence
| Regression of Hand Hygiene Opportunities∗ |
Regression of Hand Hygiene Adherence† |
|
|---|---|---|
| IR (95% CI) | IR (95% CI) | |
| Intercept | 4.88 | 0.392 |
| Education (BSN/MSN vs associate/LPN) | N/A | 1.145 (0.897, 1.462) |
| Dirty environment (vs not dirty) | 1.08‡ (1.023, 1.148) | N/A |
| Poor patient hygiene (vs not poor) | N/A | 1.129 (0.995, 1.282) |
| Propensity for infection§ | —|| | 1.009 (0.998, 1.021) |
BSN, bachelor's in science nursing; IR, incidence rate; LPN, licensed practical nurse; MSN, master's in science nursing; N/A, not applicable.
R2 (adjusted) = 0.269, deviance explained = 34.5%, scale estimate = 0.3092.
R2 (adjusted) = 0.613, deviance explained = 48.0%, scale estimate = 0.3628; controls for the total number of opportunities as an offset parameter.
P < .01.
Propensity for infection is treated as a nonlinear spline in the regression analysis of opportunities using generalized additive models, in which 3.594 estimated degrees for freedom were used to describe the relationship. This relationship is displayed in Figure 2. In contrast, the propensity for infection is controlled for only as a linear term in the regression analysis of adherence; P < .01.
Nonlinear specification, see Figure 2.
Fig. 2.
Relationship between number of hand hygiene opportunities and probability of an infection-related emergent care event.
Although higher levels of nurse professional training and propensity for infection risk were associated with higher rates of hand hygiene adherence in bivariate analysis, these findings did not hold in the multivariate analysis (Table 3, right side of panel). The association between poor patient hygiene and nurses’ hand hygiene adherence did not reach our threshold for statistical significance (P = .06; incidence rate = 1.13, 95% CI = 0.995, 1.282).
Discussion
This is the first large-scale study of hand hygiene opportunities and practices of clinicians in the HHC setting. In this study, we supplemented the observation of the opportunities indicated on the basic WHO tool with 3 hand hygiene opportunities for infection transmission that are stressed in home health practice guidelines.17 , 18 Two of these—on arrival and before departure of the patient's home—are critical opportunities for HHC clinicians to introduce or leave behind contaminants. Bakunas-Kenneley and Madigan reported that 48.4% of the inside of nursing bags were positive for human pathogens, with 6.3% of these being multiply antibiotic resistant. Hence, the bags can serve as an infection-transmitting vehicle between patients.26
The connection between poor hand hygiene and infection transmission has been well studied.1 , 3 Many guidelines and quality improvement initiatives have focused on hand hygiene practices and it has received wide attention with the outbreak of SARS-CoV-2,27 , 28 yet deficiencies continue to be reported across different care settings. The overall adherence rate in this study was lower than the one previously published study in an HHC setting9 (45.6% vs 59.2%) and notably lower than nurse self-report estimates,29 but comparable to many observation studies conducted in other health care facilities. In a systematic review of 96 studies examining adherence with hand hygiene guidelines among hospital staff, Erasmus and colleagues reported an overall median adherence rate of 40%.5 Hand hygiene rates among emergency department clinicians reportedly ranged from ≤10% to more than 89%,30 rates of service providers in nursing homes 11% to 53%,8 , 31 and in other ambulatory settings from 14% to 90%.32 , 33
Full examination of the causes for nonadherence was out of the scope of this study, but we were able to examine whether selected patient or nurse factors were related to hand hygiene care practices. We found that although no factors were directly related to hand hygiene adherence, the relationship between the number of opportunities and adherence, as well as factors identified as being related to the number of opportunities, provides us with useful information to inform the potential development of interventions. Holding adherence rate constant, the number of nonadherent opportunities increases with the total number of opportunities. We observed a greater number of opportunities for hand hygiene among patients with higher levels of infection risk and among patients who were reported to be living in a dirty environment. These findings could inform and influence how HHC agencies think about how they deploy their resources. HHC agencies could use statistical models to predict which patients are at the highest risk of infection early in care and assign advanced nurses who specialize in infection control practices in HHC (eg, wound, ostomy, and continence nurses). The finding that a dirty home environment is associated with a higher number of hand hygiene opportunities is unique to home care service delivery. Further, this finding adds empirical evidence to a result previously noted in the infection control literature.9 Mitigation of risk will involve patient and caregiver education about the relationship of the environment and infection risk and/or the deployment of additional resources, such as home attendant services.
The study agency, like most health care providers, conducts annual infection control training. Nonadherence rates reported here as well as those reported from other health care settings suggest that there are shortcomings of traditional training programs, which are largely the simple distribution and review of written guidelines.34 , 35 More effective approaches, such as the integration of simulations, role-play, along with review of case studies, may be beneficial. Training should be focused on recommended practices for following hand hygiene opportunities on arrival to a patient's home, touching patients, and moving between touching patients and the nurse bag or other reusable equipment. Simulations can help demonstrate more thoughtful placement and handling of equipment and supplies between care processes to reduce the number of opportunities for contamination.36
Limitations
This study examined data from direct observation of hand hygiene practices, which is regarded as the gold standard for assessment but has known biases,37 including sampling bias arising from recruitment of nurse volunteers willing to be observed in the field as well as the days they agree to be observed, the Hawthorne effect that may influence nurse practice while they are being observed, and potential observer bias. To minimize these biases, nurses were observed over a period of several visits and were not specifically informed that hand hygiene practices were being observed, data collectors received formal training to ensure consistency in observational methods, and inter-rater reliability testing was conducted, but it is likely that not all bias was eliminated. Despite potential shortcomings, direct observations provide useful information on what is happening in practice and a meaningful way to inform practice improvement initiatives.
Although the single-agency setting for this study represented a study limitation, nurse participants were recruited from different practice teams in 5 geographically and demographically different counties that serves patients across a wide range of socioeconomic levels and housing situations that would have context for most agencies. Further, hand hygiene adherence rates were consistent with those found in other clinical settings. Nevertheless, additional examination of hand hygiene practices in HHC agencies in other geographical and organizational settings would improve our understanding of the scope of the issue and enhance the generalizability of our findings.
Conclusions and Implications
Home care environments pose unique operational and environmental challenges to hand hygiene adherence compared to acute care settings. Clinicians in home care are decentralized and practice autonomously, serving a largely chronically ill, high–service utilization population. This study provides important data on observed infection control practices during nursing visits to home care patients, a setting that exists outside of traditional acute care facility settings. Although hand hygiene practices in the home care setting were comparable to those in facility settings, there is clearly room for improvement. More innovative teaching strategies may offer an opportunity to improve care practices and reduce infection transmission risk.
Acknowledgments
We like to thank all the nurse volunteers who participated in this study along with all the patients who allowed their visits to be observed. We would also like to thank Yolanda Barrón for her critical review of the methods and manuscript.
Footnotes
This project was supported by the Agency for Healthcare Research and Quality (grant no. R01HS024723). The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
The authors declare no conflicts of interest.
References
- 1.Scott R.D., II . Division of Healthcare Quality Promotion, National Center for Preparedness, Detection, and Control of Infectious Diseases, Coordinating Center for Infectious Disease, Centers for Disease Control and Prevention; Atlanta, GA: 2009. The direct medical costs of healthcare-associated infections in U.S. hospitals and the benefits of prevention. [Google Scholar]
- 2.The Joint Commission . The Joint Commission on Accreditation of Healthcare Organizations; Oakbrook Terrace, IL: 2020. Home Care National Patient Safety Goals. [Google Scholar]
- 3.World Health Organization . WHO Press; Geneva, Switzerland: 2009. WHO Guidelines on Hand Hygiene in Health Care: A Summary. [Google Scholar]
- 4.World Health Organization . WHO Press; Geneva, Switzerland: 2009. Hand Hygiene Technical Reference Manual. [Google Scholar]
- 5.Erasmus V., Daha T.J., Brug H. Systematic review of studies on compliance with hand hygiene guidelines in hospital care. Infect Control Hosp Epidemiol. 2010;31:283–294. doi: 10.1086/650451. [DOI] [PubMed] [Google Scholar]
- 6.Center for Clinical Standards and Quality/Quality SOGS, Centers for Medicare & Medicaid Services . 2020. Guidance for infection control and prevention concerning coronavirus disease 2019 (COVID-19) in home health agencies (HHAs), QSO-20-18; pp. 1–7. [Google Scholar]
- 7.Centers for Disease Control and Prevention Hand hygiene recommendations: Guidance for healthcare providers about hand hygiene and COVID-19. Available at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/hand-hygiene.html
- 8.Liu W.I., Liang S.Y., Wu S.F., Chuang Y.H. Hand hygiene compliance among the nursing staff in freestanding nursing homes in Taiwan: A preliminary study. Int J Nurs Pract. 2014;20:46–52. doi: 10.1111/ijn.12120. [DOI] [PubMed] [Google Scholar]
- 9.Felembam O., John W.S., Shaban R.Z. Hand hygiene practices of home visiting community nurses: Perceptions, compliance, techniques, and contextual factors of practice using the World Health Organization's "five moments for hand hygiene". Home Healthc Nurse. 2012;30:152–160. doi: 10.1097/NHH.0b013e318246d5f4. [DOI] [PubMed] [Google Scholar]
- 10.Rosenfeld P., Russell D. A review of factors influencing utilization of home and community-based long-term care: Trends and implications to the nursing workforce. Policy Polit Nurs Pract. 2012;13:72–80. doi: 10.1177/1527154412449747. [DOI] [PubMed] [Google Scholar]
- 11.Sisko A.M., Keehan S.P., Poisal J.A. National health expenditure projections, 2018-27: Economic and demographic trends drive spending and enrollment growth. Health Aff (Millwood) 2019;38:491–501. doi: 10.1377/hlthaff.2018.05499. [DOI] [PubMed] [Google Scholar]
- 12.Hartman M., Martin A.B., Benson J., Catlin A. National Health Expenditure Accounts T. National health care spending in 2018: Growth driven by accelerations in Medicare and private insurance spending. Health Aff (Millwood) 2020;39:8–17. doi: 10.1377/hlthaff.2019.01451. [DOI] [PubMed] [Google Scholar]
- 13.Consensus Measurement in Hand Hygiene Project Expert Advisory Panel . The Joint Commission; Oakbrook Terrace, IL: 2009. Measuring Hand Hygiene Adherence: Overcoming the Challenges. [Google Scholar]
- 14.Sax H., Allegranzi B., Chraiti M.N. The World Health Organization hand hygiene observation method. Am J Infect Control. 2009;37:827–834. doi: 10.1016/j.ajic.2009.07.003. [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization Five moments for hand hygiene. https://www.who.int/gpsc/tools/Five_moments/en/ Available at:
- 16.World Health Organization . WHO Press; Geneva, Switzerland: 2012. Hand Hygiene in Outpatient and Home-Based Care and Long-Term Care Facilities: A Guide to the Application of the WHO Multimodal Hand Hygiene Improvement Strategy and the "My Five Moments" Approach. [Google Scholar]
- 17.Visiting Nurse Association of America . The Visiting Nurse Association of America; Washington, DC: 2017. Clinical Procedure Manual, 20th ed. [Google Scholar]
- 18.McGoldrick M. Best practices for home care "bag technique" and the use of surface barriers. Home Healthc Now. 2017;35:478–484. doi: 10.1097/NHH.0000000000000611. [DOI] [PubMed] [Google Scholar]
- 19.Markkanen P., Quinn M., Galligan C. There's no place like home: A qualitative study of the working conditions of home health care providers. J Occup Environ Med. 2007;49:327–337. doi: 10.1097/JOM.0b013e3180326552. [DOI] [PubMed] [Google Scholar]
- 20.Sitzman K.L., Leiss J.K. Documentation of incidental factors affecting the home healthcare work environment. Home Healthc Nurse. 2009;27:516–521. doi: 10.1097/01.NHH.0000361921.20388.5b. [DOI] [PubMed] [Google Scholar]
- 21.Polivka B.J., Wills C.E., Darragh A. Environmental health and safety hazards experienced by home health care providers: A room-by-room analysis. Workplace Health Saf. 2015;63:512–522. doi: 10.1177/2165079915595925. quiz 523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wills C.E., Polivka B.J., Darragh A. Making do" decisions: How home healthcare personnel manage their exposure to home hazards. West J Nurs Res. 2016;38:411–426. doi: 10.1177/0193945915618950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shang J., Russell D., Dowding D. A predictive risk model for infection-related hospitalization among home healthcare patients. J Healthc Qual. 2020;43:136–147. doi: 10.1097/JHQ.0000000000000214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wood S.N. Fast stable restricted maximum likelihood estimation of semiparametric generalized linear models. J R Stat Soc. 2011;73:3–36. [Google Scholar]
- 25.Wood S.N. Stable and efficient multiple smoothing parameter estimation for generalized additive models. J Am Stat Assoc. 2004;99:673–686. [Google Scholar]
- 26.Bakunas-Kenneley I., Madigan E.A. Infection prevention and control in home health care: The nurse's bag. Am J Infect Control. 2009;37:687–688. doi: 10.1016/j.ajic.2009.03.004. [DOI] [PubMed] [Google Scholar]
- 27.Cawthorne K.R., Cooke R.P.D. Innovative technologies for hand hygiene monitoring are urgently needed in the fight against COVID-19. J Hosp Infect. 2020;105:362–363. doi: 10.1016/j.jhin.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Peters A., Lotfinejad N., Simniceanu A., Pittet D. The economics of infection prevention: Why it is crucial to invest in hand hygiene and nurses during the novel coronavirus pandemic. J Infect. 2020;81:318–356. doi: 10.1016/j.jinf.2020.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Russell D., Dowding D.W., McDonald M.V. Factors for compliance with infection control practices in home healthcare: Findings from a survey of nurses' knowledge and attitudes toward infection control. Am J Infect Control. 2018;46:1211–1217. doi: 10.1016/j.ajic.2018.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liang S.Y., Riethman M., Fox J. Infection prevention for the emergency department: Out of reach or standard of care? Emerg Med Clin North Am. 2018;36:873–887. doi: 10.1016/j.emc.2018.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Castle N., Handler S., Wagner L. Hand hygiene practices reported by nurse aides in nursing homes. J Appl Gerontol. 2016;35:267–285. doi: 10.1177/0733464813514133. [DOI] [PubMed] [Google Scholar]
- 32.Arenas M.D., Sanchez-Paya J., Barril G. A multicentric survey of the practice of hand hygiene in haemodialysis units: Factors affecting compliance. Nephrol Dial Transplant. 2005;20:1164–1171. doi: 10.1093/ndt/gfh759. [DOI] [PubMed] [Google Scholar]
- 33.Schaefer M.K., Jhung M., Dahl M. Infection control assessment of ambulatory surgical centers. JAMA. 2010;303:2273–2279. doi: 10.1001/jama.2010.744. [DOI] [PubMed] [Google Scholar]
- 34.Gould D.J., Moralejo D., Drey N. Interventions to improve hand hygiene compliance in patient care. Cochrane Database Syst Rev. 2017;9:CD005186. doi: 10.1002/14651858.CD005186.pub2. [DOI] [PubMed] [Google Scholar]
- 35.Lydon S., Power M., McSharry J. Interventions to improve hand hygiene compliance in the ICU: A systematic review. Crit Care Med. 2017;45:e1165–e1172. doi: 10.1097/CCM.0000000000002691. [DOI] [PubMed] [Google Scholar]
- 36.Scheithauer S., Kamerseder V., Petersen P. Improving hand hygiene compliance in the emergency department: Getting to the point. BMC Infect Dis. 2013;13:367. doi: 10.1186/1471-2334-13-367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jeanes A., Coen P.G., Gould D.J., Drey N.S. Validity of hand hygiene compliance measurement by observation: A systematic review. Am J Infect Control. 2019;47:313–322. doi: 10.1016/j.ajic.2018.08.004. [DOI] [PubMed] [Google Scholar]