Abstract
Background
Total hip arthroplasty (THA) is an effective operation for patients with hip osteoarthritis; however, patients with hip dysplasia present a particular challenge. Our novel study examined the effect of robot-assisted THA in patients with hip dysplasia.
Methods
We retrospectively reviewed patients with developmental dysplasia of the hip undergoing primary THA using robotic arm assistance at 2 institutions from January 2010 to January 2017. Patients undergoing revision arthroplasty were excluded. Preoperatively, all patients underwent a computed tomography scan so that 3-dimensional templating could be performed. Hip range of motion (ROM) and clinical leg length discrepancy were recorded preoperatively. Two independent observers calculated Crowe and Hartofilakidis grades for each operative hip. At the final follow-up, hip ROM, postoperative complications, and modified Harris Hip scores were obtained.
Results
Seventy-nine patients underwent THA because of degenerative joint disease in the setting of developmental dysplasia of the hip. There were 56 females and 23 males with a mean age of 45 years (range: 26-64 years). We found that components were placed according to the preoperative plan, that there was an improvement in the modified Harris hip score from 29 to 86 (P < .001), an improvement in the hip ROM (flexion improvement from 66° to 91°, P < .0001), and a correction of leg length discrepancy (17.1 vs 4 mm, P < .0002). There were no complications during the short-term interim follow-up (mean: 3.1 years).
Conclusions
Robot-assisted THA can be a useful method to ensure adequate component positioning and excellent outcomes in patients with hip dysplasia.
Level of Evidence
Level III, Retrospective
Keywords: Robot assisted, Total hip arthroplasty, Dysplasia, Component positioning
Introduction
Total hip arthroplasty (THA) is considered one of the most successful surgeries with regard to postoperative patient satisfaction and function. The outcome after THA depends greatly on the accuracy of component positioning, particularly on the placement of the acetabular cup. Failure to achieve appropriate cup inclination, anteversion, and restoration of the hip center can lead to early and late complications after THA including dislocation, impingement, reduced postoperative range of motion (ROM), and increased edge loading leading to accelerated wear [[1], [2], [3], [5], [6], [4]]. Dysplasia of the hip is recognized as the cause for joint degeneration and is thus often eventually considered an indication for THA. However, THA in this patient population has been associated with a higher risk of complications including cup malposition, hip instability, wound issues, and infection because of increased surgical time, leg length inequality, and nerve palsies [[7], [8], [9], [10], [11], [12], [13]].
THA in patients with dysplasia can be technically demanding because of various anatomical variations of the acetabulum and the femur. In patients with dysplasia, the acetabula are hypoplastic and deficient in various planes and dimensions, thus increasing the difficulty of placing the acetabular cup [14]. In addition, patients with dysplasia often have narrow femoral canals and increased anteversion in addition to bone stock deficiency [13,15,16]. These and other anatomical aberrations make the surgery more challenging and increase the risk of complications [[17], [18], [19]]. In addition to anatomical difficulties, surgeons also must consider that this patient population may present at an early age and thus may eventually require revision surgery [[17], [18], [19]]. Therefore, component selection and placement become paramount in the primary procedure to ensure implant survival for as long as possible.
Studies have shown that THA is a very effective operation even in patients with varying levels of dysplasia of the hip [[20], [21], [22]]. Preoperative digital planning via computed tomography (CT) scans and additional computer software has shown to lead to satisfactory results of prosthesis positioning [21,23,24]. Nonetheless, human error is still a major variable in acetabular cup positioning, and to ensure accurate execution of the preoperative surgical plan in the setting of anatomic distortion, many surgeons have begun to use robot-assisted techniques during THA with good to excellent results [25,26].
The rise of robot-assisted technology in THA is due in large part to the accuracy of implant placement as demonstrated in studies by Nodzo et al. [27] and Domb et al. [28]. Nodzo et al. [27] validated the use of robot-assisted THA in achieving accurate component positioning when assessed using CT-based three-dimensional (3D) modeling, and Domb et al. [28] reported on the improvement in cup placement using a robotic navigation relative to manual techniques. Precision in achieving the preoperative plan is especially important in patients with developmental dysplasia of the hip (DDH) with challenging anatomy, as they may eventually require revision surgery. Determining and achieving appropriate acetabular cup position has implications on hip biomechanics, leg length, implant longevity and wear, component stability, and gait [16].
Therefore, given the promising results of robotics in primary THAs, we sought to determine whether similarly positive outcomes would be observed in patients with DDH undergoing THA. No study to our knowledge has evaluated the use of haptically guided robot-assisted THA in patients with hip dysplasia. We sought to determine whether the use of MAKOplasty (Stryker Corp, Mako Surgical Corp, Fort Lauderdale, FL) during THA in patients with DDH affects postoperative radiographic parameters, complications, need for revision surgery, and functional outcomes.
Material and methods
Using institutional electronic medical records, we retrospectively reviewed all patients with DDH undergoing primary THA using MAKOplasty at 2 institutions from January 2010 to January 2015. Institutional review board approval was obtained at each institution before the initiation of the study. Patients undergoing revision arthroplasty were excluded.
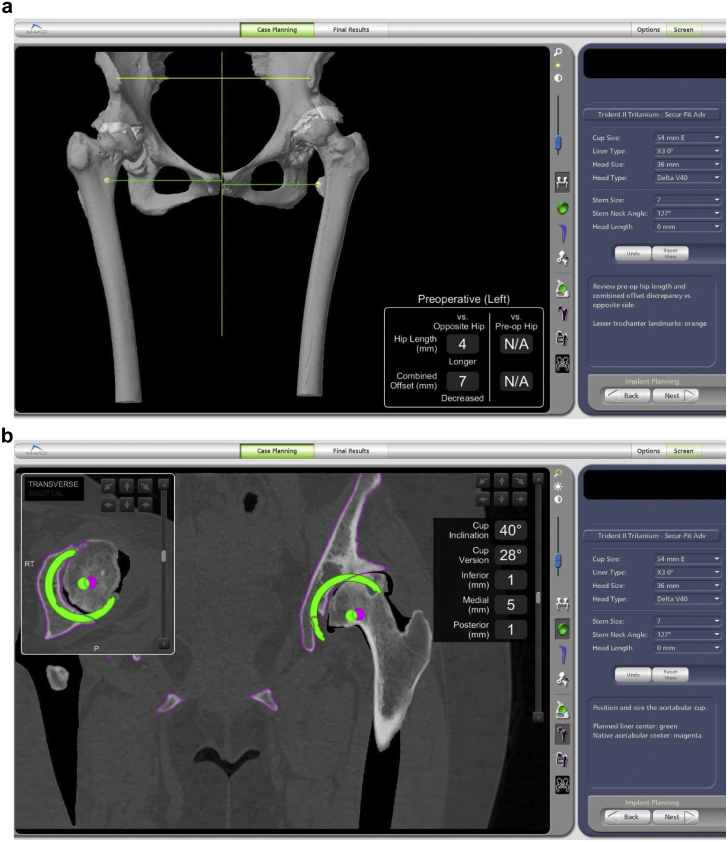
Preoperatively, all patients underwent a CT scan so that 3D templating could be performed. Surgeons then used the 3D model to preoperatively template patient-specific plans for cup position, stem position and anteversion, head diameter, head length and liner type, and leg length (Fig. 1a-d). The goal acetabular inclination was between 40° and 45°, and the goal anteversion was between 20° and 25°. In general, the hip center was attempted to be restored to the native hip center, allowing up to 1 centimeter of hip center elevation in the most complex cases as measured on the CT templating. In only one of the cases, a femoral head allograft was required, specifically for acetabular deficiency and in a patient aged 23 years. All implants used on the femoral side were the S-ROM (DePuy Synthes, Warsaw, IN), which accommodates for torsional abnormalities of the femur and small diameter canal sizes down to 6 millimeters.
Figure 1.
Three-dimensional (3D) templating of (a) patient-specific anatomical models using robot-assisted navigation software derived from preoperative CT scanning. The 3D model is used to template patient-specific plans for (b, c, and d) the cup position, stem position and anteversion, head diameter, head length and liner type, and leg length.
All patients received spinal or general anesthesia and were operated on in the lateral decubitus position using a standard lateral positioner, level bed, and posterior approach. Three fellowship-trained hip arthroplasty surgeons performed all robot-assisted procedures. Preoperative assessment of the hips was performed using chart review of electronic medical records, radiographs, and CT scans. Patient ROM and clinical leg length discrepancy (LLD) were recorded preoperatively. LLD was calculated using measurements from the anterior superior iliac spine to the medial malleolus with the patient lying supine and using the Coleman block testing. Two independent observers calculated Crowe and Hartofilakidis grades for each operative hip. Patients with Crowe types III and IV present unique issues, often exhibiting more severe subluxation in the hips and hypoplastic acetabula. In this study, there were 10 patients with Crowe type III and 6 with Crowe type IV, and a minority of the total patients was analyzed, and given that they both exhibited severe dysplasia and were surgically managed in the same way, a subgroup analysis was not performed.
All radiographs assessed were taken at initial postoperative follow-up office visits between one and 3 months after surgery by 2 separate reviewers (Figure 2, Figure 3a and b). All measurements were made using the postoperative AP pelvis radiographs using our institution’s picture archiving and communication system software. Cup anteversion and inclination was measured using previously established techniques [1,29]. To assess the effect of intraoperative robot-assisted surgery on component positioning, postoperative acetabular cup inclination angle, anteversion, hip center elevation, and LLD were compared with planned values. Preoperative and postoperative LLD was measured on standing radiographs using established methods using the teardrop and lesser trochanters and compared with CT measurements from the robotic system. At the final follow-up, the hip ROM, postoperative complications, and modified Harris Hip Scores (HHSs) were obtained.
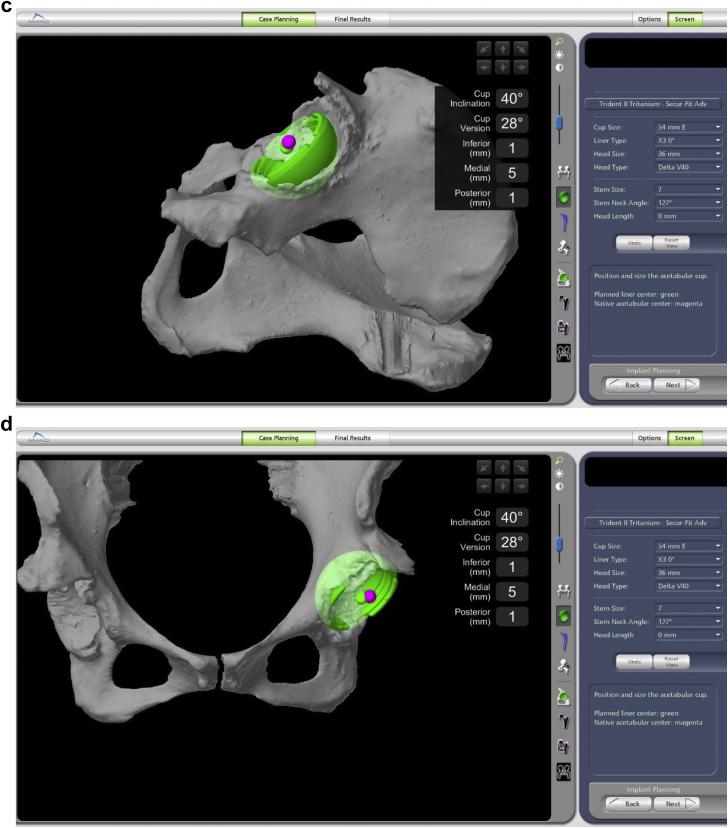
Figure 2.
Preoperative (a) anteroposterior pelvis and (b) Lowenstein view radiographs showing chronic dysplastic changes.
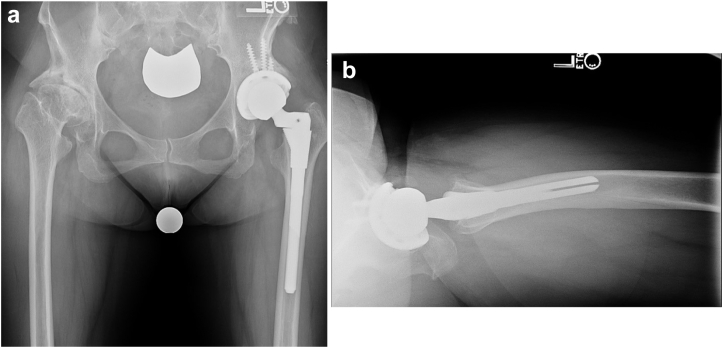
Figure 3.
Postoperative (a) anteroposterior pelvis and (b) cross-table lateral radiographs showing component positioning after robot-assisted total hip arthroplasty.
Statistical analysis
Data were analyzed using quantitative statistical parameters. The student t-test was used for between-group comparisons of parametric continuous variables. Categorical variables were analyzed using chi-squared tests or Fisher’s exact test. Statistical significance was set at 0.05. Descriptive statistical results will be presented as means with the standard deviation.
Results
Overall, there were 79 patients from 2 institutions who underwent primary THA for dysplasia using MAKOplasty robot-assisted navigation that were included in our study. The mean age of these patients was 45 years (range: 26-64 years), and there were 56 (71%) female patients and 23 male patients. Twenty-three patients had Crowe grade I, 40 patients had Crowe grade II, 10 patients had Crowe grade III, and 6 patients had Crowe grade IV dysplasia determined by radiographs. This corresponded to 23 patients with Hartofilakidis class A, 50 patients with class B, and 6 patients with class C dysplasia on the CT scan. One patient did not have sufficient imaging to determine the preoperative Crowe or Hartofilakidis grade. All 79 patients underwent THA because of degenerative joint disease in the setting of DDH.
The modified HHSs showed a significant improvement in patient function/satisfaction from a mean of 29 preoperatively to a mean of 86 postoperatively (P < .001). When comparing patients’ preoperative and postoperative ROM in chart reviews of electronic medical records, there was a clear increase in the mean degree of hip flexion (66° to 91°, P < .0001) and hip extension (5° to 0°, P = .0065), which were both statistically significant. In addition, there was a significant correction of LLD after robot-assisted surgery from a mean of 17.1 mm preoperatively to 4 mm postoperatively (P = .0002).
A comparison was made between the cup position as determined by the intraoperative MAKOplasty navigation and the position measured via postoperative radiographs. The hip center on the postoperative radiograph was found to be in the templated location in all 79 hips. There was no difference between robotic templated acetabular inclination and the postoperative radiograph, 42° vs 40° (P = .1809). There was, however, a difference in the radiographically calculated anteversion from the robotic plan, 28° vs 19°. Because the radiographically calculated anteversion was taken on a cross-table lateral radiograph, this difference is explained by a difference in pelvic tilt or in Murray’s definition of anteversion. The robotic system used CT scans for preoperative planning, and its software performed acetabular cup measurements based on the patient’s coronal plane, as Murray initially used to define the acetabular inclination and anteversion [29]. For postoperative radiographic measurements of cup orientation, cross-table lateral views of the pelvis were used, with measurements made using previously established techniques [28,30,31]. When cup inclination and version was measured on AP pelvis views using the coronal plane of the pelvis, there was no difference observed between the radiographic and robotic calculations [31].
There were no complications or revisions in any of the 79 patients included in the study during the short-term interim follow-up (mean: 3.1 years, range: 2-4.6 years).
Discussion
The importance of the acetabular cup position during THA is especially important in patients with dysplasia of the hip. The normal anatomic landmarks and relationships in the hip are often altered, making freehand placement of the cup quite difficult and somewhat unreliable. The ability to preoperatively plan based on patient-specific anatomy allows the surgeon to accurately place the cup in an optimal position where there is the most bone coverage. In addition, the ability to preoperatively plan using the MAKOplasty software allows the surgeon to adjust the femur to the correct overall leg length. The use of robot-assisted placement of the cup with MAKOplasty can assist with high-accuracy prosthesis placement, which our study shows can ultimately optimize patient outcomes after THA. In our study, all 79 cases resulted in accurate placement of the acetabular component, consistent with the preoperative plan for hip center, inclination and anteversion, and achievement of the most acetabular coverage based on 3D CT templating (Fig. 1a-d). The postoperative hip ROM, leg length inequalities, and patient-reported functional outcomes were all significantly improved from preoperative values with robot-assisted THA in a cohort of patients with DDH.
It is unclear whether THA by itself can lead to improvements in the patient hip ROM postoperatively. This is particularly true for patients with DDH, as there is still no consensus on the overall effects of THA on the hip ROM in this patient population. In a cohort of 52 hips with DDH compared with 73 healthy hips, Nakahara et al. [32] found that while the ROM was either better or similar in patients with DDH, the rates of impingement were significantly higher. Other studies however show higher grades of dysplasia do in fact cause limitations in the ROM at the hip joint [20]. Our study did show a significant improvement in both flexion and extension in patients with DDH undergoing robot-assisted THA using MAKOplasty. Flexion particularly improved from a mean of 65.9° to 90.8° after THA (P < .0001). Our results are similar to findings in the literature that report successful improvements in the hip center of rotation and the overall ROM after THA [20,26,33].
LLD is known to be a significant source of patient litigation after THA [34]. This discrepancy is exaggerated in patients with hip dysplasia, as demonstrated by our study cohort whose mean preoperative LLD was 17.1 mm (range of 0-40 mm) [35]. Zhu et al. [20] examined 27 patients with severe DDH (Crowe types 3 and 4) undergoing freehand primary THA and found their postoperative LLD (1.3 cm ± 0.3 cm) to be significantly improved compared with their preoperative LLD (P < .001). The use of robot-assisted surgery has previously been shown to be highly accurate in predicting postoperative LLD, as reported by El Bitar et al. [25]. Although no study has examined the leg length change in patients with DDH with MAKOplasty, El Bitar et al. reported 100% of their 61-patient cohort who underwent robot-assisted primary THA as having a leg length change within 10 mm of their radiographic measurements. In our study, most patients experienced an equalization of their leg lengths with a mean postoperative LLD measuring just 4 mm radiographically, a statistically significant difference from preoperative measurements (P = .0002). Four millimeter of LLD was deemed to be a safe, acceptable, and reproducible result as the accuracy of leg length with the robotic system has been found to be within 5 mm [36]. In addition, depending on the situation, the surgeon may not have wanted to fully correct LLD because of too much preoperative discrepancy or tight soft tissues.
Controversy still exists around the efficacy of robot-assisted surgery in improving clinical outcomes. Honl et al. reported statistically better HHSs compared with controls; however, Bargar et al. found no significant difference in the modified HHSs or 36-Item Short Form Health Survey scores between the 2 groups [37,38]. While Australian registry data have reported decreased revision rates at 11-year follow-up with the use of robotic assistance, Bach et al. did not find any difference in the functional outcome in the robotic group [39,40]. In addition, the cost for CT imaging is between $750 and $1000 per case and estimates for the robot range from $850,000 to $1,300,000, with a $150,000 yearly cost of maintenance. However, correct component positioning and sizing is important for the success of THA, and when considering that robot-assisted surgery has been associated with more accurate component alignment and has improved reproducibility for primary THA, this may lead to lower 90-day costs because of fewer readmissions and economically beneficial discharge destinations [28,41,42]. Domb et al. [28] reported results of using the MAKOplasty and found it was significantly more likely to obtain correct acetabular cup alignment (P = .001), inclination (P = .004), and anteversion (P = .002) compared with controls. This increased accuracy and precision of component placement could be especially useful in challenging cases such as patients with dysplasia where anatomy can be variable. Furthermore, robot-assisted surgery has been shown to result in shorter postoperative lengths of stay in the hospital, but long-term studies on prosthesis survival are needed to confirm the cost-effectiveness [43].
Our study is among the first and largest to our knowledge to characterize the use of MAKOplasty robot-assisted THA in the specific challenging subset of patients with dysplasia of the hip. Its strengths include the inclusion of several patient outcome measures to gauge the success of robot-assisted THA. These include clinical parameters of the ROM and LLD, the prosthetic position determined from both radiographs and the robot itself, as well as functional scores reported directly from the patients. Historically, the literature has shown that THA in patients with dysplasia has an increased risk of complications; however, in our cohort of patients with DDH undergoing robot-assisted THA, we did not have any complications, including postoperative nerve palsies. Thus, the use of preoperative planning and robot-assisted surgery is one of several factors, such as an appropriate surgical indication, technique, and robust soft-tissue repair, that may decrease the risk of complications in patients with dysplasia, who are typically at a higher risk of postoperative complications. Given that our study has relatively small numbers, further studies would need to be performed to assess the complication rates of robot-assisted surgery compared with standard THA in patients with dysplasia.
The present study has several limitations. The small size of the cohort makes it difficult to draw conclusions about potential confounding variables, as a multivariate analysis would be underpowered. As far as not performing a subgroup analysis for patients with Crowe type III or IV, Yoon et al. [44] report on the use of cementless THA for patients with Crowe type III or IV and, similar to this study, do not evaluate the outcomes of both cohorts based on the Crowe classification, given that they both undergo the same surgical intervention. In addition, we do not have a control group in this study to draw direct specific conclusions on the success of robotic vs freehand THA in patients with similar preoperative demographics and degrees of hip dysplasia.
Conclusions
The current success of THA will continue to evolve with technology-guided techniques for surgery being introduced. Despite the effectiveness of traditional THA, in challenging patients such as those with dysplasia, these novel techniques that include MAKOplasty may play a significant role in optimizing patient outcomes. Further randomized studies will be needed to determine the overall role and cost-effectiveness of robot-assisted surgery in THA for dysplasia.
Conflict of interest
J.M. Vigdorchik reports receiving personal fees from Corin Group and has received research funding from Corin Group. A.K. Sharma declares that he has no conflict of interest. K.M. Carroll reports having stock ownership in OrthAlign. V.K. Aggarwal declares that he has no conflict of interest. S.A. Jerabek reports having stock ownership in Stryker, receiving personal fees from Stryker, and has received research funding from Stryker.
Appendix A. Supplementary data
References
- 1.Lewinnek G.E., Lewis J., Tarr R., Compere C., Zimmerman J. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60(2):217. [PubMed] [Google Scholar]
- 2.D'lima D.D., Urquhart A.G., Buehler K.O., Walker R.H., Colwell C.W. The effect of the orientation of the acetabular and femoral components on the range of motion of the hip at different head-neck ratios. J Bone Joint Surg Am. 2000;82(3):315. doi: 10.2106/00004623-200003000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Del Schutte H., Jr., Lipman A.J., Bannar S.M., Livermore J.T., Ilstrup D., Morrey B.F. Effects of acetabular abduction on cup wear rates in total hip arthroplasty. J Arthroplasty. 1998;13(6):621. doi: 10.1016/s0883-5403(98)80003-x. [DOI] [PubMed] [Google Scholar]
- 4.Carter A.H., Sheehan E.C., Mortazavi S.J., Purtill J.J., Sharkey P.F., Parvizi J. Revision for recurrent instability: what are the predictors of failure? J Arthroplasty. 2011;26(6):46. doi: 10.1016/j.arth.2011.03.021. [DOI] [PubMed] [Google Scholar]
- 5.Little N.J., Busch C.A., Gallagher J.A., Rorabeck C.H., Bourne R.B. Acetabular polyethylene wear and acetabular inclination and femoral offset. Clin Orthop Relat Res. 2009;467(11):2895. doi: 10.1007/s11999-009-0845-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.DeWal H., Su E., DiCesare P.E. Instability following total hip arthroplasty. Am J Orthop (Belle Mead NJ) 2003;32(8):377–382. [PubMed] [Google Scholar]
- 7.Charnley J., Feagin J.A. Low-friction arthroplasty in congenital subluxation of the hip. Clin Orthop Relat Res. 1973;91:98. doi: 10.1097/00003086-197303000-00015. [DOI] [PubMed] [Google Scholar]
- 8.Garvin K.L., Bowen M., Salvati E., Ranawat C. Long-term results of total hip arthroplasty in congenital dislocation and dysplasia of the hip. A follow-up note. J Bone Joint Surg Am. 1991;73(9):1348. [PubMed] [Google Scholar]
- 9.Pagnano M.W., Hanssen A.D., Lewallen D.G., Shaughnessy W.J. The effect of superior placement of the acetabular component on the rate of loosening after total hip arthroplasty. Long-term results in patients who have Crowe type-II congenital dysplasia of the hip. J Bone Joint Surg Am. 1996;78(7):1004. doi: 10.2106/00004623-199607000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Stans A.A., Pagnano M.W., Shaughnessy W.J., Hanssen A.D. Results of total hip arthroplasty for Crowe Type III developmental hip dysplasia. Clin Orthop Relat Res. 1998;(348):149. [PubMed] [Google Scholar]
- 11.Linde F., Jensen J. Socket loosening in arthroplasty for congenital dislocation of the hip. Acta Orthop Scand. 1988;59(3):254. doi: 10.3109/17453678809149356. [DOI] [PubMed] [Google Scholar]
- 12.Okamoto T., Inao S., Gotoh E., Ando M. Primary Charnley total hip arthroplasty for congenital dysplasia: effect of improved techniques of cementing. J Bone Joint Surg Br. 1997;79(1):83. doi: 10.1302/0301-620x.79b1.6771. [DOI] [PubMed] [Google Scholar]
- 13.Crowe J.F., Mani V.J., Ranawat C.S. Total hip replacement in congenital dislocation and dysplasia of the hip. J Bone Joint Surg Am. 1979;61(1):15. [PubMed] [Google Scholar]
- 14.van Bosse H., Wedge J.H., Babyn P. How are dysplastic hips different? A three-dimensional CT study. Clin Orthop Relat Res. 2015;473(5):1712. doi: 10.1007/s11999-014-4103-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Argenson J.-N.A., Flecher X., Parratte S., Aubaniac J.-M. Anatomy of the dysplastic hip and consequences for total hip arthroplasty. Clin Orthop Relat Res. 2007;465:40. doi: 10.1097/BLO.0b013e3181576052. [DOI] [PubMed] [Google Scholar]
- 16.Wang Y. Current concepts in developmental dysplasia of the hip and Total hip arthroplasty. Arthroplasty. 2019;1(1):2. doi: 10.1186/s42836-019-0004-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Greber E.M., Pelt C.E., Gililland J.M., Anderson M.B., Erickson J.A., Peters C.L. Challenges in total hip arthroplasty in the setting of developmental dysplasia of the hip. J Arthroplasty. 2017;32(9):S38. doi: 10.1016/j.arth.2017.02.024. [DOI] [PubMed] [Google Scholar]
- 18.Biant L.C., Bruce W.J., Assini J.B., Walker P.M., Walsh W.R. Primary total hip arthroplasty in severe developmental dysplasia of the hip. Ten-year results using a cementless modular stem. J Arthroplasty. 2009;24(1):27. doi: 10.1016/j.arth.2007.12.016. [DOI] [PubMed] [Google Scholar]
- 19.Faldini C., Nanni M., Leonetti D., Miscione M.T., Acri F., Giannini S. Total hip arthroplasty in developmental hip dysplasia using cementless tapered stem. Results after a minimum 10-year follow-up. Hip Int. 2011;21(4):415. doi: 10.5301/HIP.2011.8588. [DOI] [PubMed] [Google Scholar]
- 20.Zhu J., Wang Y., Pang J. Effectiveness of total hip arthroplasty for severe developmental dysplasia of hip in adults. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2014;28(3):335. [PubMed] [Google Scholar]
- 21.Zhang J., Wang L., Mao Y., Li H., Ding H., Zhu Z. The use of combined anteversion in total hip arthroplasty for patients with developmental dysplasia of the hip. J Arthroplasty. 2014;29(3):621. doi: 10.1016/j.arth.2013.08.004. [DOI] [PubMed] [Google Scholar]
- 22.Bożek M., Bielecki T., Nowak R., Żelawski M. Arthroplasty in patients with congenital hip dysplasia--early evaluation of a treatment method. Ortop Traumatol Rehabil. 2013;15(1):49. doi: 10.5604/15093492.1032794. [DOI] [PubMed] [Google Scholar]
- 23.Inoue D., Kabata T., Maeda T. Value of computed tomography-based three-dimensional surgical preoperative planning software in total hip arthroplasty with developmental dysplasia of the hip. J Orthop Sci. 2015;20(2):340. doi: 10.1007/s00776-014-0683-3. [DOI] [PubMed] [Google Scholar]
- 24.Zeng Y., Lai O.J., Shen B. Three-dimensional computerized preoperative planning of total hip arthroplasty with high-riding dislocation developmental dysplasia of the hip. Orthop Surg. 2014;6(2):95. doi: 10.1111/os.12099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.El Bitar Y.F., Jackson T.J., Lindner D., Botser I.B., Stake C.E., Domb B.G. Predictive value of robotic-assisted total hip arthroplasty. Orthopedics. 2015;38(1):e31. doi: 10.3928/01477447-20150105-57. [DOI] [PubMed] [Google Scholar]
- 26.Kanawade V., Dorr L.D., Banks S.A., Zhang Z., Wan Z. Precision of robotic guided instrumentation for acetabular component positioning. J Arthroplasty. 2015;30(3):392. doi: 10.1016/j.arth.2014.10.021. [DOI] [PubMed] [Google Scholar]
- 27.Nodzo S.R., Chang C.C., Carroll K.M. Intraoperative placement of total hip arthroplasty components with robotic-arm assisted technology correlates with postoperative implant position: a CT-based study. Bone Joint J. 2018;100-B(10):1303. doi: 10.1302/0301-620X.100B10-BJJ-2018-0201.R1. [DOI] [PubMed] [Google Scholar]
- 28.Domb B.G., El Bitar Y.F., Sadik A.Y., Stake C.E., Botser I.B. Comparison of robotic-assisted and conventional acetabular cup placement in THA: a matched-pair controlled study. Clin Orthop Relat Res. 2014;472(1):329. doi: 10.1007/s11999-013-3253-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Murray D.W. The definition and measurement of acetabular orientation. J Bone Joint Surg Br. 1993;75(2):228. doi: 10.1302/0301-620X.75B2.8444942. [DOI] [PubMed] [Google Scholar]
- 30.Woo R.Y., Morrey B.F. Dislocations after total hip arthroplasty. J Bone Joint Surg Am. 1982;64(9):1295. [PubMed] [Google Scholar]
- 31.Wan Z., Malik A., Jaramaz B., Chao L., Dorr L.D. Imaging and navigation measurement of acetabular component position in THA. Clin Orthop Relat Res. 2009;467(1):32. doi: 10.1007/s11999-008-0597-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nakahara I., Takao M., Sakai T., Miki H., Nishii T., Sugano N. Three-dimensional morphology and bony range of movement in hip joints in patients with hip dysplasia. Bone Joint J. 2014;96(5):580. doi: 10.1302/0301-620X.96B5.32503. [DOI] [PubMed] [Google Scholar]
- 33.Sakellariou V.I., Christodoulou M., Sasalos G., Babis G.C. Reconstruction of the acetabulum in developmental dysplasia of the hip in total hip replacement. Arch Bone Joint Surg. 2014;2(3):130. [PMC free article] [PubMed] [Google Scholar]
- 34.Clark C.R., Huddleston H.D., Schoch E.P., III, Thomas B.J. Leg-length discrepancy after total hip arthroplasty. J Am Acad Orthop Surg. 2006;14(1):38. doi: 10.5435/00124635-200601000-00007. [DOI] [PubMed] [Google Scholar]
- 35.Murayama T., Ohnishi H., Mori T., Okazaki Y., Sujita K., Sakai A. A novel non-invasive mechanical technique of cup and stem placement and leg length adjustment in total hip arthroplasty for dysplastic hips. Int Orthop. 2015;39(6):1057. doi: 10.1007/s00264-014-2613-6. [DOI] [PubMed] [Google Scholar]
- 36.El Bitar Y.F., Stone J.C., Jackson T.J., Lindner D., Stake C.E., Domb B.G. Leg-length discrepancy after total hip arthroplasty: comparison of robot-assisted posterior, fluoroscopy-guided anterior, and conventional posterior approaches. Am J Orthop (Belle Mead NJ) 2015;44(6):265. [PubMed] [Google Scholar]
- 37.Honl M., Dierk O., Gauck C. Comparison of robotic-assisted and manual implantation of a primary total hip replacement: a prospective study. J Bone Joint Surg Am. 2003;85(8):1470. doi: 10.2106/00004623-200308000-00007. [DOI] [PubMed] [Google Scholar]
- 38.Bargar W.L., Bauer A., Börner M. Primary and revision total hip replacement using the Robodoc® system. Clin Orthop Relat Res. 1998;354:82. doi: 10.1097/00003086-199809000-00011. [DOI] [PubMed] [Google Scholar]
- 39.Bach C.M., Winter P., Nogler M., Göbel G., Wimmer C., Ogon M. No functional impairment after Robodoc total hip arthroplasty. Acta Orthop Scand. 2002;73(4):386. doi: 10.1080/00016470216316. [DOI] [PubMed] [Google Scholar]
- 40.NJRRA . 2016. Australian National joint registry Annual report 2016.https://aoanjrr.sahmri.com/annual-reports-2016 [Google Scholar]
- 41.Banerjee S., Cherian J., Elmallah R., Pierce T., Jauregui J., Mont M. Robot-assisted total hip arthroplasty. Expert Rev Med Devices. 2015;13:47. doi: 10.1586/17434440.2016.1124018. [DOI] [PubMed] [Google Scholar]
- 42.Nawabi D.H., Conditt M.A., Ranawat A.S. Haptically guided robotic technology in total hip arthroplasty: a cadaveric investigation. Proc Inst Mech Eng H. 2013;227(3):302. doi: 10.1177/0954411912468540. [DOI] [PubMed] [Google Scholar]
- 43.Banchetti R., Dari S., Ricciarini Comparison of conventional versus robotic-assisted total hip arthroplasty using the Mako System: an Italian retrospective study. J Health Soc Sci. 2018;2018:37. [Google Scholar]
- 44.Yoon P.W., Kim J.I., Kim D.O. Cementless total hip arthroplasty for patients with Crowe type III or IV developmental dysplasia of the hip: two-stage total hip arthroplasty following skeletal traction after soft tissue release for irreducible hips. Clin Orthop Surg. 2013;5(3):167. doi: 10.4055/cios.2013.5.3.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.