Abstract
This cohort study examines sleep and demographic data from wearable activity tracking devices to assess for an association of sleep duration and variability with body mass index.
Inadequate sleep has been linked to negative health outcomes, including obesity, coronary artery disease, hypertension, type 2 diabetes, and even incident pneumonia.1 Most population-level sleep data are limited by recall bias, cross-sectional nature, and lack of detail regarding sleep habits over months to years. The recent increased uptake of wearable sensors (also known as activity trackers) has made such longitudinal data increasingly obtainable with digital devices that offer unobtrusive monitoring of multiple health parameters, including sleep. Here we describe longitudinal sleep characteristics in more than 120 000 individuals with up to 2 years of monitored sleep duration data. We examined the hypothesis that shorter sleep duration (hours slept at night) and greater day-to-day variability of sleep duration (standard deviation of hours slept at night) are associated with increased body mass index (BMI).1,2
Methods
This retrospective cohort study was deemed exempt from human subjects research oversight by the Scripps Institutional Review Board owing to the use of deidentified data. Sleep data from 200 000 deidentified individuals consistently using a commercially available wearable device (Fitbit Inc) from March 2016 to March 2018 were included. Device users provided basic demographic information and agreed to the use of their deidentified data for research purposes. These data included the longest, or “main,” sleep period for all participants. Individuals without sex or BMI information were excluded, as were those with less than 100 days of data. Only data from days with 22 hours or more of “on-wrist,” or wear, time were included (eFigure in the Supplement). Data were assessed for (1) sleep duration and (2) sleep variability using standard deviation of sleep duration. These metrics were calculated for each user separately, averaged, and then examined according to self-reported baseline BMI. Using an unpaired t test for samples from independent means, we tested the hypothesis that there was an association of shorter sleep duration and greater sleep variability with BMI (dichotomized at 30 based on the threshold for obesity) (eMethods in the Supplement). Data analysis was conducted using Python, version 3.6 (Python Software Foundation).
Results
Sleep Duration and Longitudinal Sleep Patterns
Data from 120 522 individuals (median [interquartile range], 256 [156-342] nights) showed a mean sleep duration of 6 hours 47 minutes (SD, 48 minutes) (Figure 1A). Even when individuals had similar mean sleep durations, their patterns of sleep—or sleep variability—often differed substantially (see examples in Figure 1B, C, and D).
Figure 1. Sleep Duration in the Study Cohort.
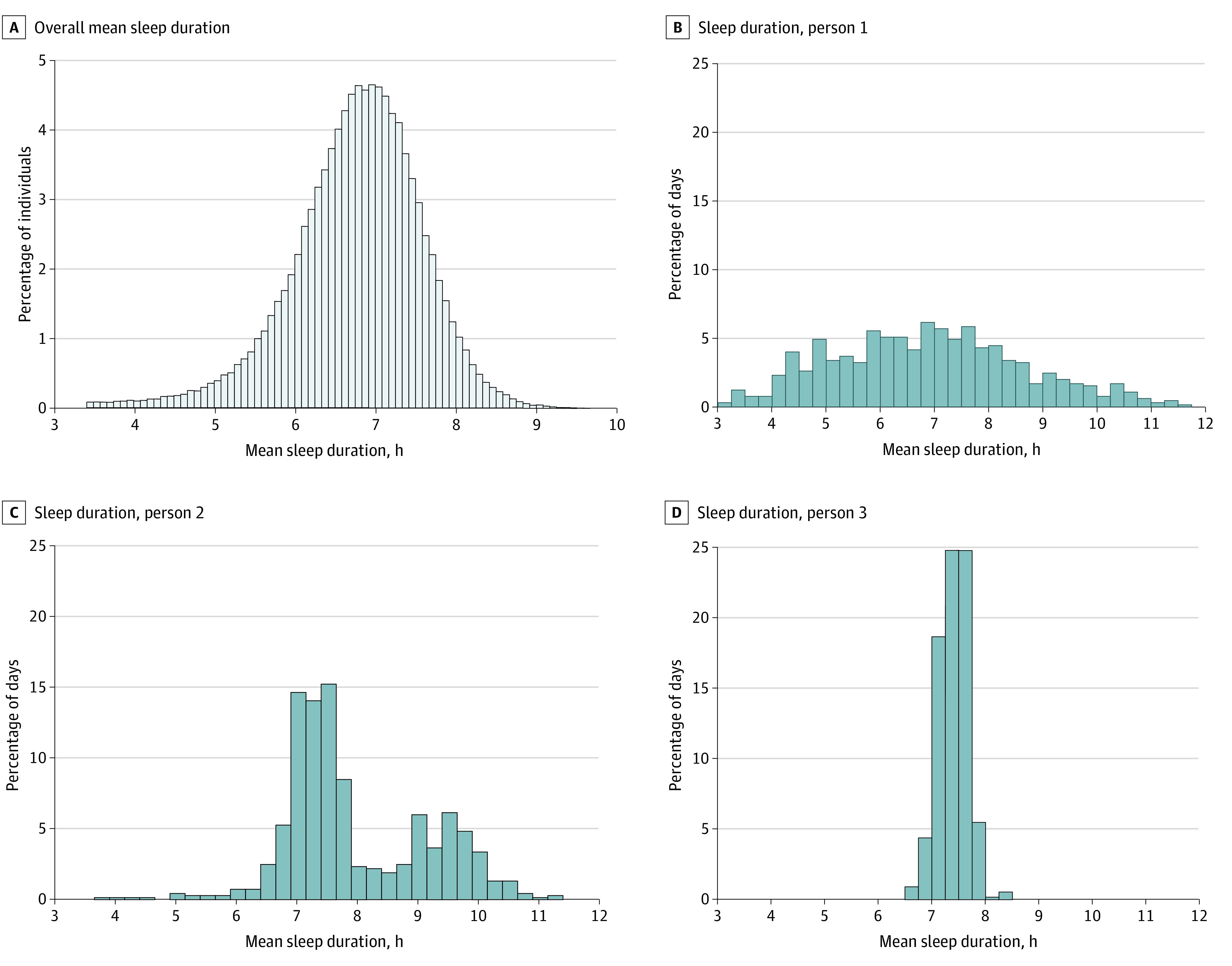
A, Distribution of the mean sleep duration of all 120 522 individuals in the data set. Individuals had to have at least 100 days of sleep data with at least 22 hours of wear time to be included. B, C, and D, The distribution sleep duration for 3 individuals with similar mean sleep duration (6.7-7.3 hours). Their body mass indexes ranged from 27 to 28 and ages ranged from 43 to 79 years. Body mass index is calculated as weight in kilograms divided by height in meters squared.
Association of Sleep With BMI
Shorter sleep duration and greater sleep variability were each associated with higher BMI (Figure 2). Using a BMI threshold of 30, we found that participants with BMIs over the threshold had slightly shorter mean (SD) sleep durations (6.62 [0.85] vs 6.87 [0.76] hours; P < .001; approximately 15 minutes less) and more variable sleep (1.46 [0.38] vs 1.38 [0.37] hours; P < .001).
Figure 2. Sleep and Obesity.
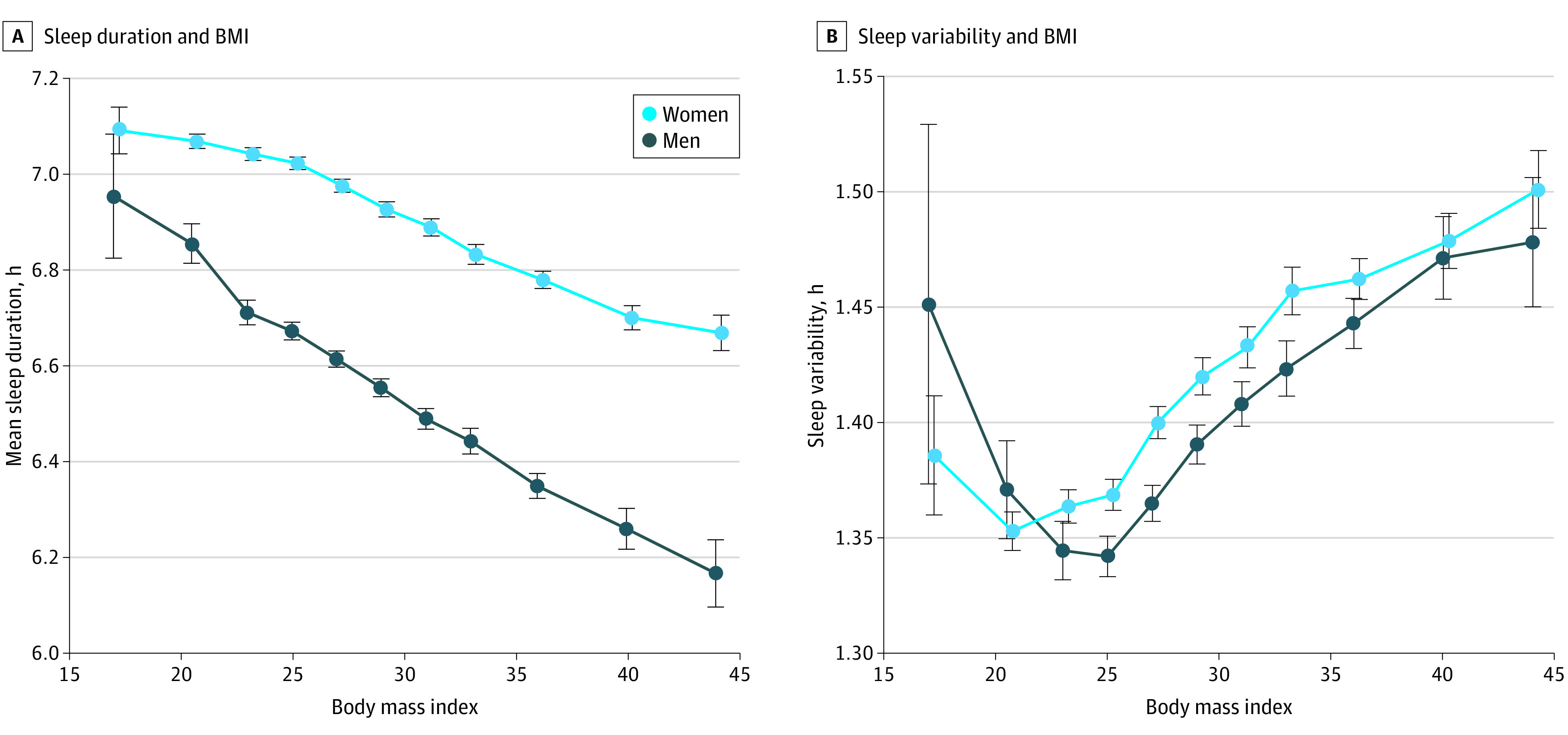
A, Mean sleep duration is associated with body mass index (BMI). B, Sleep variability is associated with BMI. BMI is calculated as weight in kilograms divided by height in meters squared. Error bars represent standard error of the mean.
Discussion
We analyzed objective sleep measurements for a large longitudinal cohort of adults wearing activity monitoring devices. By comparison, while the Centers for Disease Control and Prevention biannually surveys approximately 500 000 people in the US about their sleep duration, this consists of a single question based on subjective recall. Research studies may track sleep using actigraphy, but typically for less than 1 week and include at most several thousand participants. Our work suggests the feasibility of large-scale, ongoing objective sleep measurements.
Major findings of our study include that (1) individual sleep durations and patterns are highly variable, and (2) shorter sleep duration and greater sleep variability were both associated with higher BMI. While we cannot determine the direction of association from our study result, these findings provide further support to the notion that sleep patterns are associated with weight management and overall health. The findings also support the potential value of including both sleep duration and individual sleep patterns when studying sleep-related health outcomes.
Several limitations of our study should be noted. Our sleep measures were estimated from accelerometers/optical sensors rather than criterion-standard polysomnography, although we note validation studies that suggest reasonable accuracy for total sleep time.3,4 Individuals likely to use wearables are generally of higher socioeconomic status, younger, and healthier, and thus our results might not generalize to other populations.5,6 In addition, we excluded nap data, relied on self-reported height and weight, and could not ascertain comorbidities.
eMethods.
eFigure. Device users in data set based on device usage.
eReferences.
References
- 1.Grandner MA, Chakravorty S, Perlis ML, Oliver L, Gurubhagavatula I. Habitual sleep duration associated with self-reported and objectively determined cardiometabolic risk factors. Sleep Med. 2014;15(1):42-50. doi: 10.1016/j.sleep.2013.09.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kobayashi D, Takahashi O, Shimbo T, Okubo T, Arioka H, Fukui T. High sleep duration variability is an independent risk factor for weight gain. Sleep Breath. 2013;17(1):167-172. doi: 10.1007/s11325-012-0665-7 [DOI] [PubMed] [Google Scholar]
- 3.de Zambotti M, Goldstone A, Claudatos S, Colrain IM, Baker FC. A validation study of Fitbit Charge 2 compared with polysomnography in adults. Chronobiol Int. 2018;35(4):465-476. doi: 10.1080/07420528.2017.1413578 [DOI] [PubMed] [Google Scholar]
- 4.Haghayegh S, Khoshnevis S, Smolensky MH, Diller KR, Castriotta RJ. Performance assessment of new-generation Fitbit technology in deriving sleep parameters and stages. Chronobiol Int. 2020;37(1):47-59. doi: 10.1080/07420528.2019.1682006 [DOI] [PubMed] [Google Scholar]
- 5.Macridis S, Johnston N, Johnson S, Vallance JK. Consumer physical activity tracking device ownership and use among a population-based sample of adults. PLoS One. 2018;13(1):e0189298. doi: 10.1371/journal.pone.0189298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Patel NP, Grandner MA, Xie D, Branas CC, Gooneratne N. “Sleep disparity” in the population: poor sleep quality is strongly associated with poverty and ethnicity. BMC Public Health. 2010;10:475. doi: 10.1186/1471-2458-10-475 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods.
eFigure. Device users in data set based on device usage.
eReferences.


