Abstract
Rhabdomyolysis is characterized by rapid muscle breakdown and release of intracellular muscle components into the circulation. Acute renal injury is the most common and fatal complication of rhabdomyolysis. The current literature emphasizes the importance of preventing rhabdomyolysis and finding the benefits of sodium bicarbonates and mannitol in its prevention. A PubMed database search for the keywords "Rhabdomyolysis," "Sodium bicarbonate use in rhabdomyolysis," "Mannitol use in rhabdomyolysis," and a Medical Subject Headings (MeSH) search using the keyword "Rhabdomyolysis; Acute Kidney Injury (Subheading-Prevention and control)" generated 10,005 articles overall. After a thorough application of inclusion/exclusion criteria, 37 relevant studies were selected for this literature study. This analysis demonstrates that aggressive early volume resuscitation with normal saline should continue being the principal focus of therapy, and the use of sodium bicarbonate and mannitol in practical situations is not entirely justified. This article also emphasizes the need for future research on this topic and provides recommendations for future research.
Keywords: rhabdomyolysis, bicarbonates, mannitol, crush injury, : acute kidney injury, acute renal injury
Introduction and background
Rhabdomyolysis is a syndrome characterized by muscle necrosis and the release of intracellular muscle constituents into the circulation [1]. Bywaters and Beall first reported it in four crush injury victims after excavating them from the rubble during the London bombing in 1941 [2]. They noticed that dark urine and brown pigmented casts similar to hemoglobin were deposited in the distal tubules of the victims, leading to significant renal impairment. The causes of rhabdomyolysis are multifactorial. The most common causes in adults are illicit drugs/toxins, alcohol abuse, medical drugs, trauma (crush injury), genetic defects, seizures, and metabolic disorders [3]. Acute kidney injury (AKI) is the most severe complication of rhabdomyolysis regardless of the etiology. The incidence ranges from 13% to 50%, depending on the clinical setting and diagnosing criteria [4]. In the Meijer et al. study, the mortality of patients who developed AKI was 59% vs. 22% in patients who did not develop AKI [5]. As exemplified by this study, early recognition of rhabdomyolysis and prevention of AKI should be the cornerstone of treatment.
Many studies have shown that progression to significant renal failure can be avoided via early and aggressive saline infusion [6]. The use of sodium bicarbonate and mannitol to deter the development of AKI in rhabdomyolysis is currently controversial. Some studies propose that patients benefit from sodium bicarbonate and mannitol infusions [7]. However, other recent studies suggest against their use to prevent myoglobinuric renal failure as there is little evidence other than from animal studies, retrospective observational studies, and case series to support their routine use [8,9].
This study's objective is to determine the optimal management and review the effectiveness of sodium bicarbonate and mannitol in the prevention of AKI following rhabdomyolysis. This study also aims to summarise the available evidence on this topic and provide recommendations according to current standards for practical guidelines.
Review
Methods
Literature was searched in PubMed with parallel strategies based on Medical Subject Headings (MeSH) subheadings and regular keywords for data collection. Table 1 shows regular and MeSH keywords used for the literature search.
Table 1. Regular and MeSH keywords search for literature review.
MeSH: Medical Subject Headings
| Regular keyword- Rhabdomyolysis | |
| Total results | 9692 |
| Results selected | 1241 |
| Regular keyword- Sodium bicarbonate use in rhabdomyolysis | |
| Total results | 102 |
| Results selected | 23 |
| Regular keyword: Mannitol use in rhabdomyolysis | |
| Total results | 91 |
| Results selected | 19 |
| MeSH keyword: Rhabdomyolysis; Acute Kidney Injury (Subheading-Prevention and control) | |
| Total results | 120 |
| Results selected | 28 |
Studies were selected after applying the following inclusion/exclusion criteria.
Inclusion Criteria:
1. Human subjects of all age groups
2. Diagnosis of AKI following rhabdomyolysis
3. Paper published in English with no year restriction
4. The study types were observational studies, systematic review, literature review, and case-series
5. Full-text papers
Exclusion Criteria:
1. Animal studies
2. Non-English literature
3. Clinical trials, single case reports
Results
Table 2 shows the total number of articles after applying inclusion/exclusion criteria in the following order.
Table 2. Total number of articles after applying inclusion/exclusion criteria.
MeSH: Medical Subject Headings
| Regular keyword- Rhabdomyolysis | |
| Total records | 9692 |
| Human | 8026 |
| English | 6456 |
| Full text | 5423 |
| Type of studies | 1241 |
| Regular keyword: Sodium bicarbonate use in rhabdomyolysis | |
| Total results | 102 |
| Humans | 83 |
| English | 72 |
| Full text | 59 |
| Study designs | 23 |
| Regular keyword: Mannitol use in rhabdomyolysis | |
| Total results | 91 |
| Humans | 81 |
| English | 67 |
| Full text | 50 |
| Study designs | 19 |
| MeSH keyword: Rhabdomyolysis; Acute Kidney Injury (Subheading-Prevention and control) | |
| Total results | 120 |
| Humans | 78 |
| English | 58 |
| Full text | 52 |
| Study designs | 28 |
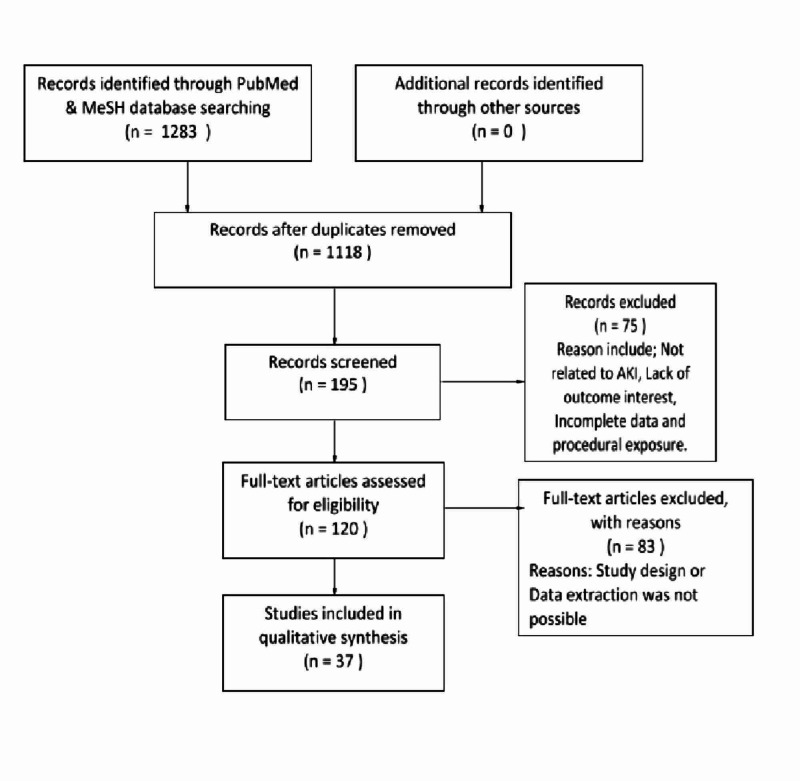
A single PubMed database search generated 10,005 articles overall. After applying the inclusion-exclusion criteria, only 1283 potentially relevant articles remained. After screening the abstracts of these articles, 120 studies were included in the final analyses as they met our study's title and objectives. Out of these, 37 studies were used as they provided full text and pertinent information for this review.
Figure 1 below shows the flowchart with the process of the current literature review.
Figure 1. Flow chart explaining the process of current literature review.
AKI: Acute Kidney Injury, MeSH: Medical Subject Headings
Discussion
Etiology
The risk factors for rhabdomyolysis are very diverse. They can be broadly classified into acquired causes and inherited causes. Acquired causes include trauma (crush injury), ischemia, illicit drugs (cocaine, methadone, heroin), alcohol, drugs (statins, fibrates), infections (Epstein-Barr virus, influenza, HIV), extreme temperatures (heatstroke, malignant hyperthermia, malignant neuroleptic syndrome), and toxins (spider bites, wasp stings, snake venom) [10-17]. Some inherited causes such as metabolic disorders (electrolyte changes, diabetic ketoacidosis, thyroid abnormalities) and genetic disorders (disorders of glycolysis or glycogenolysis, lipid metabolism, mitochondrial diseases) are a few of the most common risk factors for rhabdomyolysis [10-17].
Table 3 below summarizes the common causes of rhabdomyolysis.
Table 3. Common causes of rhabdomyolysis.
| Common causes of rhabdomyolysis |
| Direct muscular injuries |
| Excessive exercise |
| Muscle hypoxia |
| Ischemic causes |
| Genetic defects |
| Metabolic disorders |
| Endocrine disorders |
| Electrolyte disorders |
| Drugs and toxins |
| Infections and Idiopathic |
Complications
Cell destruction promotes leakage of intracellular components causing fatal complications. Immoderate potassium leakage leads to cardiac arrhythmias or cardiac arrest, whereas hypocalcemia is a result of calcium phosphate precipitation with calcification in the necrotic muscle [10-17]. The release of proteases and coagulating cascade from the damaged cell causes hepatic dysfunction and disseminated intravascular coagulation (DIC), respectively. Intracellular fluid accumulation and ischemic changes potentiate the rise in the intra-compartmental pressure and cause compartment syndrome to be an early or late complication [11,14].
Table 4 shows complications of rhabdomyolysis.
Table 4. Complications of rhabdomyolysis.
| Early complications (<12 hrs) | Early or late complications (12-24hrs) | Late complications (>24 hrs) |
| Hyperkalemia | Compartment syndrome | Acute renal failure |
| Hypocalcemia | Disseminated Intravascular Coagulation (DIC) | |
| Cardiac arrhythmias | ||
| Cardiac arrest |
Pathogenesis of Myoglobin-Induced Acute Kidney Injury
The exact mechanism of AKI in rhabdomyolysis is complex and debatable with the growing evidence. Although the deposition of myoglobin in the renal tubules remains the main insult, the mechanism by which it occurs remains controversial [18].
Myoglobin appears in the urine only when the renal threshold of 0.5 to 1.5 mg of myoglobin per deciliter is exceeded and is grossly visible as reddish-brown (commonly referred to as “tea-colored”) urine when serum myoglobin levels reach 100 mg per deciliter [4]. Acidic urine and incremented uric acid in the urine can further complicate this effect by precipitating myoglobin upon interacting with Tamm-Horsfall protein, resulting in tubular casts formation and obstruction to urine flow [10]. Intratubular myoglobin, when degraded, releases reactive oxygen species and free radicals, causing direct ischemic tubular damage [10].
Recent studies demonstrate that in pathological conditions, myoglobin oxidized to ferryl state (Fe) exhibits peroxidase properties and leads to lipid peroxidation. Products of lipid peroxidation contribute to AKI by causing renal vasoconstriction, oxidative injury, and tissue damage [18,19]. The current evidence affirms that kidney failure is due to the collective effects of hypovolemia, aciduria, and direct cytotoxicity due to the accumulation of myoglobin [14,18-20]. Many clinical factors like serum creatine kinase (CK), creatinine, potassium, Ca2+, and urine myoglobin level are valued to foretell the risk of acute renal failure (ARF), but there is no consensus on a single factor [14].
Sodium Bicarbonate
An acidic urine environment potentiates myoglobin-induced renal toxicity [10-14]. The basis behind the use of sodium bicarbonate is that it promotes alkalization of the urine and counteracts the process of heme pigment precipitation, thereby decreasing the direct pigment injury [13-16]. Urine alkalization is also useful in diminishing redox cycling and lipid peroxidation, thus preventing oxidative stress, tubular damage, and renal vasoconstriction [10,17]. Hence, it is believed that urine alkalization, optimizing the pH higher than 6.5, can prevent renal impairment [4]. On the contrary, the evidence is scarce that urine alkalization has a proven clinical benefit over standard saline resuscitation in these patients [6].
A well-observed side effect with bicarbonate therapy in the initial stages of treatment is hypocalcemia. It is also noted that when bicarbonates are used in decompensated respiratory patients or circulatory failure, they can cause hyperosmolar states and paradoxical intracellular acidosis [12,21]. However, no studies have compared it as standard therapy with saline resuscitation alone.
Mannitol
Mannitol is a rapidly acting osmotic diuretic that has many proposed benefits [22]. It works as a renal vasodilator improving glomerular filtration rate. This mechanism leads to diuresis to be beneficial in the excretion of excess myoglobin and the prevention of myoglobin cast formation [22-26]. Mannitol also acts as a free radical scavenger and has an antioxidant effect on renal parenchyma. While some initial studies suggested using mannitol in rhabdomyolysis, most of the evidence presenting mannitol's protective effect comes from animal studies [4]. Further, a few clinical trials and observational studies found no clinical benefit with mannitol [4]. Many studies have observed the paradoxical effect of mannitol as a renal vasoconstrictor when used in higher dosages (>200 g/day), causing osmotic nephrosis [10]. However, many authors support the use of mannitol in rhabdomyolysis-induced renal failure, especially in crush injury victims as mannitol decreases osmotic swelling and edema in the injured muscle cells and helps restore the skeletal muscle function [22,23]. They also recommend that mannitol be administered when saline infusions fail to improve a urine output of more than 300 ml/hr [23], and thus it is practical to initiate treatment with IV fluids and offer mannitol after assessing the urinary response. Frequent monitoring of plasma osmolality and the osmolal gap is needed during mannitol administration, and it should be halted when there is a significant rise in the osmolal gap (>55 mOsm/kg) [10].
Table 5 provides a review of the use of sodium bicarbonates and mannitol as adjuvant therapy in rhabdomyolysis.
Table 5. Comparative studies on preventive and therapeutic regimens in rhabdomyolysis.
CPK: Creatine Phosphokinase, ARF: Acute Renal Failure, RP: Rhabdomyolysis Protocol, RM: Rhabdomyolysis, NS: Normal Saline, B: Bicarbonate, M: Mannitol
| Title/Author | Study design | Sample size | Patient group | Therapeutic strategy | The outcome in AKI patients |
| Eneas et al., 1979 [7] | Retrospective | 20 | Patients with the crush syndrome | Mannitol and sodium bicarbonate | Better in patients with low CPK vs. high CPK |
| Ron et al., 1984 [27] | Prospective | 7 | Crush injuries from the collapsed building | Mannitol and Sodium bicarbonate | All recovered without azotemia or renal failure |
| Knottenbelt et al., 1994 [28] | Retrospective | 200 | Patients with severe beatings | Fluid loads without mannitol and bicarbonate | No difference; Increased ARF with late admissions |
| Shimazu et al., 1994 [29] | Retrospective | 14 | Crush injuries from the earthquake | Early vs Late fluid resuscitation | Better with early and high volume infusions |
| Homsi et al., 1997 [6] | Retrospective | 24 | ICU patients | Normal saline vs. normal saline plus bicarbonate and mannitol | No difference |
| Brown et al., 2004 [30] | Retrospective | 2083 | Traumatic patients | Normal saline vs. bicarbonate plus mannitol | No difference |
| Gunal et al., 2004 [31] | Retrospective | 16 | Patients with crush syndrome | Early vs. late treatment with normal saline followed immediately by bicarbonate | Better with early initiation of treatment. |
| Cho et al., 2007 [32] | Prospective study | 28 | Patients with intoxication from doxylamine | Ringer’s lactate vs. normal saline; bicarbonate if urine pH is <6.5 | Better if therapy initiated early; Better with a high volume of hydration |
| Iraj et al., 2011 [33] | Prospective study | 638 | Earthquake victims with crush injuries. | Early large volume vs Early low volume NS; No sodium bicarb or mannitol associated. | Authors recommend >6 L/day in severe RM and ≥3 L/day IV fluid in moderate RM to decrease the incidence of AKI |
| Tazmini et al., 2017 [34] | Retrospective | 31 | Exercise-induced rhabdomyolysis | Normal saline vs. Urinary alkalinization | No significant difference |
| Nielsen et al., 2017 [35] | Retrospective | 77 | Traumatic rhabdomyolysis, CPK >10,000 u/l | NS vs NS+B+M(RP) | Reduced ARF was noted with RP. ARF developed in 26% of patients with the RP vs. 70% without it (P= .008). |
Many studies have coupled mannitol with bicarbonate to see the synergetic effect, but studies comparing it with saline resuscitation alone are sparse. In 1984, Ron et al. published a study on seven crush victims noticing no visible hemoglobinuria after 48 hrs and no need for hemodialysis in any patients after treating them with sodium bicarbonate and mannitol. A notable impediment of this study was not having a standard control group [27]. According to Scharman et al., sodium bicarbonate and mannitol should be used only to correct metabolic acidosis if present and to achieve a urine output of 300 mL/hr or more, respectively [36]. Brown et al. and Homsi et al. mentioned that the use of bicarbonates and mannitol in patients with rhabdomyolysis seems unrelated or did not improve the clinical outcomes in their study [6,30]. Recently an article published by Michelsen et al. also discouraged the use of bicarbonates and mannitol while categorizing it as a weak recommendation [37].
On the contrary, few studies seem favorable to the use of urinary alkalinization and mannitol therapy. Eneas et al. proposed more favorable results in patients treated with mannitol and bicarbonate with low creatine phosphokinase (CPK) than with higher CPK [7]. Gunal et al. recommends that positive results are striking with early vigorous initiation (<12 hrs of insult) and followed by urine alkalization and mannitol therapy [31]. In 2017, Nielsen et al. recognized a significant decrease in the development of acute renal failure of 26% vs. 70% (P=0.008) in patients with CK>10000 u/l with sodium bicarbonate and mannitol added to normal saline compared to patients with normal saline alone, respectively [35].
Why the Need for Revision?
The recent Neilsen et al. study highlights the importance of reassessment on this topic. There is an emerging need to address these topics forthwith, such as a specific clinical biomarker in categorizing rhabdomyolysis and assessing patients for their risk for AKI. The benefit of these agents catered to case specifics such as anuric patients should be evaluated [35]. Also, the appropriate timing for the initiation of therapy and specific parameters for the use of these agents should be determined. There is a demand and need for more multicenter randomized clinical trials to address these issues and provide more evidence. Future research can help practice an evidence-based approach to attain better outcomes and avoid opting for the use of these agents in regular clinical practice.
Limitations
Nonetheless, the findings of this study have to be seen in light of some limitations. Animal studies and literature published in languages other than English were not used in this review.
Conclusions
Rhabdomyolysis is clinically challenging to manage as many medical, social, and environmental factors can contribute to this condition. Acute kidney injury is a fatal insult following rhabdomyolysis, and early identification of the risk factors and interventions to prevention should be the center of treatment for high-risk patients. Considering the historical evidence and theoretical benefits of bicarbonates and mannitol in AKI, it is assumed that these agents are beneficial, which has led to their routine use in standard practice. However, there is ample evidence that these standards of practice need to be revisited. Aggressive early volume resuscitation with normal saline still should be the primary focus of treatment. The use of these agents as a single standard measure is discouraged as they are not superior to saline therapy, as shown by current evidence.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
Footnotes
The authors have declared that no competing interests exist.
References
- 1.Rhabdomyolysis and myoglobinuria. Knochel JP. Annu Rev Med. 1982;33:435–443. doi: 10.1146/annurev.me.33.020182.002251. [DOI] [PubMed] [Google Scholar]
- 2.Crush injuries with impairment of renal function. Bywaters EG, Beall D. Br Med J. 1941;22:427–432. doi: 10.1136/bmj.1.4185.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rhabdomyolysis: an evaluation of 475 hospitalized patients. Melli G, Chaudhry V, Cornblath DR. Medicine (Baltimore) 2005;84:377–385. doi: 10.1097/01.md.0000188565.48918.41. [DOI] [PubMed] [Google Scholar]
- 4.Rhabdomyolysis and acute kidney injury. Bosch X, Poch E, Grau JM. N Engl J Med. 2009;361:62–72. doi: 10.1056/NEJMra0801327. [DOI] [PubMed] [Google Scholar]
- 5.Serum creatine kinase as predictor of clinical course in rhabdomyolysis: a 5-year intensive care survey. de Meijer, AR AR, Fikkers Fikkers, BG BG. https://doi.org/10.1007/s00134-003-1800-5. Intensive Care Med. 2003;29:1121–1125. doi: 10.1007/s00134-003-1800-5. [DOI] [PubMed] [Google Scholar]
- 6.Prophylaxis of acute renal failure in patients with rhabdomyolysis. Homsi E, Barreiro MF, Orlando JM, Higa EM. Ren Fail. 1997;19:283–288. doi: 10.3109/08860229709026290. [DOI] [PubMed] [Google Scholar]
- 7.The effect of infusion of mannitol-sodium bicarbonate on the clinical course of myoglobinuria. Eneas JF, Schoenfeld PY, Humphreys MH. Arch Intern Med. 1979;139:801–805. [PubMed] [Google Scholar]
- 8.Rhabdomyolysis. Zimmerman JL, Shen MC. Chest. 2013;144:1058–1065. doi: 10.1378/chest.12-2016. [DOI] [PubMed] [Google Scholar]
- 9.Prevention of rhabdomyolysis‐induced acute kidney injury - A DASAIM/DSIT clinical practice guideline. Michelsen J, Cordtz J, Liboriussen L, et al. Acta Anaesthesiol Scand. 2019;63:576–586. doi: 10.1111/aas.13308. [DOI] [PubMed] [Google Scholar]
- 10.Rhabdomyolysis and acute kidney injury. Bosch X, Poch E, Grau JM. N Engl J Med. 2011;1982:62–72. doi: 10.1056/NEJMra0801327. [DOI] [PubMed] [Google Scholar]
- 11.Rhabdomyolysis. Sauret JM, Marinides G, Wang GK. https://pubmed.ncbi.nlm.nih.gov/11898964/ Am Fam Physician. 2002;65:907–912. [PubMed] [Google Scholar]
- 12.Beyond muscle destruction: a systematic review of rhabdomyolysis for clinical practice. Chavez LO, Leon M, Einav S, Varon J. Crit Care. 2016;20:135. doi: 10.1186/s13054-016-1314-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rhabdomyolysis. Vanholder R, Sever MS, Erek E, Lameire N. https://jasn.asnjournals.org/content/11/8/1553. J Am Soc Nephrol. 2000;11:1553–1561. doi: 10.1681/ASN.V1181553. [DOI] [PubMed] [Google Scholar]
- 14.Rhabdomyolysis: a review of the literature. Khan FY. http://pubmed.ncbi.nlm.nih.gov/19841484/ Neth J Med. 2009;67:272–283. [PubMed] [Google Scholar]
- 15.Rhabdomyolysis and myohemoglobinuric acute renal failure. Zager RA. Kidney Int. 1996;49:314–326. doi: 10.1038/ki.1996.48. [DOI] [PubMed] [Google Scholar]
- 16.Rhabdomyolysis: historical background, clinical, diagnostic and therapeutic features. Cervellin G, Comelli I, Lippi G. CCLM;48:749–756. doi: 10.1515/CCLM.2010.151. [DOI] [PubMed] [Google Scholar]
- 17.Acute kidney injury due to rhabdomyolysis. Lima RS, da Silva Junior GB, Liborio AB, Daher Ede F. http://pubmed.ncbi.nlm.nih.gov/18711286/ Saudi J Kidney Dis Transpl. 2008;19:721–729. [PubMed] [Google Scholar]
- 18.Mechanism-based therapeutic approaches to rhabdomyolysis-induced renal failure. Boutaud O, Roberts LJ. Free Radic Biol Med. 2011;51:1062–1067. doi: 10.1016/j.freeradbiomed.2010.10.704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Acetaminophen inhibits hemoprotein-catalyzed lipid peroxidation and attenuates rhabdomyolysis-induced renal failure. Boutaud O, Moore KP, Reeder BJ, et al. Proc Natl Acad Sci. 2010;107:2699–2704. doi: 10.1073/pnas.0910174107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Acute renal failure in the setting of bone marrow transplantation. Zager RA. Kidney Int. 1994;46:1443–1458. doi: 10.1038/ki.1994.417. [DOI] [PubMed] [Google Scholar]
- 21.Rhabdomyolysis: Prevention and treatment. [May;2020 ];Alvaro Bada, MD; Nathan Smith, MD MD, RHABDOMYOLYSIS RHABDOMYOLYSIS. http://www.surgicalcriticalcare.net/Guidelines/Rhabdomyolysis%202018.pdf 2018 http://www.surgicalcriticalcare.net/Guidelines/Rhabdomyolysis%202018.pdf [Google Scholar]
- 22.Mannitol-induced acute renal failure. Visweswaran P, Massin EK, Dubose TD Jr. https://pubmed.ncbi.nlm.nih.gov/9189872/ J Am Soc Nephrol. 1997;8:1028–1033. doi: 10.1681/ASN.V861028. [DOI] [PubMed] [Google Scholar]
- 23.Recommendation for the management of crush victims in mass disasters. Sever MS, Vanholder R, Ashkenazi L, et al. Nephrol Dial Transplant. 2012;27:1. doi: 10.1093/ndt/gfs156. [DOI] [PubMed] [Google Scholar]
- 24.Mannitol increases renal blood flow and maintains filtration fraction and oxygenation in postoperative acute kidney injury: a prospective interventional study. Bragadottir G, Redfors B, Ricksten SE. Crit Care. 2012;16:159. doi: 10.1186/cc11480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mannitol nephrotoxicity syndrome: role of hemodialysis and postulate of mechanisms. Gadallah MF, Lynn M, Work J. Am J Med Sci. 1995;309:219–222. doi: 10.1097/00000441-199504000-00006. [DOI] [PubMed] [Google Scholar]
- 26.Mannitol therapy revisited (1940-1997) Better OS, Rubinstein I, Winaver JM, Knochel JP. Kidney Int. 1997;52:886–894. doi: 10.1038/ki.1997.409. [DOI] [PubMed] [Google Scholar]
- 27.Prevention of acute renal failure in traumatic rhabdomyolysis. Ron D, Taitelman U, Michaelson M, et al. https://pubmed.ncbi.nlm.nih.gov/6696564/ Arch Intern Med. 1984;144:277–280. [PubMed] [Google Scholar]
- 28.Traumatic rhabdomyolysis from severe beating - experience of volume diuresis in 200 patients. Knottenbelt JD. https://pubmed.ncbi.nlm.nih.gov/8064919/ J Trauma. 1994;37:214–219. [PubMed] [Google Scholar]
- 29.Fluid resuscitation and systemic complications in crush syndrome: 14 Hanshin-Awaji earthquake patients. Shimazu T, Yoshioka T, Nakata Y, et al. J Trauma. 1997;42:641–646. doi: 10.1097/00005373-199704000-00010. [DOI] [PubMed] [Google Scholar]
- 30.Preventing renal failure in patients with rhabdomyolysis: do bicarbonate and mannitol make a difference? Brown CV, Rhee P, Chan L, Evans K, Demetriades D, Velmahos GC. J Trauma. 2004;56:1191–1196. doi: 10.1097/01.ta.0000130761.78627.10. [DOI] [PubMed] [Google Scholar]
- 31.Early and vigorous fluid resuscitation prevents acute renal failure in the crush victims of catastrophic earthquakes. Gunal AI, Celiker H, Dogukan A, et al. J Am Soc Nephrol. 2004;15:1862–1867. doi: 10.1097/01.asn.0000129336.09976.73. [DOI] [PubMed] [Google Scholar]
- 32.Comparison of lactated Ringer’s solution and 0.9% saline in the treatment of rhabdomyolysis induced by doxylamine intoxication. Cho YS, Lim H, Kim SH. Emerg Med J. 2007;24:276–280. doi: 10.1136/emj.2006.043265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Prophylactic fluid therapy in crushed victims of Bam earthquake. Iraj N, Saeed S, Mostafa H, et al. J Emerg Med. 2011;29:738–742. doi: 10.1016/j.ajem.2010.02.018. [DOI] [PubMed] [Google Scholar]
- 34.Exercise-induced rhabdomyolysis - a patient series. Tazmini K, Schreiner C, Bruserud S, Raastad T, Solberg EE. Tidsskr Nor Laegeforen. 2017;13:137. doi: 10.4045/tidsskr.16.1103. [DOI] [PubMed] [Google Scholar]
- 35.Bicarbonate and mannitol treatment for traumatic rhabdomyolysis revisited. Neilsen JS, Sally M, Mullins RJ, et al. Am J Surg. 2017;213:73–79. doi: 10.1016/j.amjsurg.2016.03.017. [DOI] [PubMed] [Google Scholar]
- 36.Prevention of kidney injury following rhabdomyolysis: a systematic review. Scharman EJ, Troutman WG. Ann Pharmacother. 2013;47:90–105. doi: 10.1345/aph.1R215. [DOI] [PubMed] [Google Scholar]
- 37.Prevention of rhabdomyolysis‐induced acute kidney injury - A DASAIM/DSIT clinical practice guideline. Michelsen J, Cordtz J, Liboriussen L, et al. Acta Anaesthesiol Scand. 2019;63:576–586. doi: 10.1111/aas.13308. [DOI] [PubMed] [Google Scholar]