Abstract
Nodular scabies is a less common manifestation of scabies. It is characterized by firm, erythematous, pruritic nodules, often involving the genitalia. Diagnosis can be made clinically, and first-line treatment is topical permethrin or oral ivermectin.
Keywords: Scabies, Sexually transmitted infection, Genital nodule
Scabies is a skin disease caused by infestation with a parasitic mite, Sarcoptes scabiei. In developed countries, outbreaks can occur in nursing homes or homeless populations. An increasingly recognized high-risk group for scabies infestation is young males, particularly men who have sex with men [1].
Depicted in Fig. 1 are thin, pink-red, edemotous papules and small nodules on the glans penis, penile shaft, and scrotum of a 22-year-old healthy male on pre-exposure prophylaxis for HIV. The symptom duration is two weeks including pruritic papules on the volar wrists. He noted being sexually active with both men and women with inconsistent use of condoms.
Fig. 1.
Discrete nodules on glans penis and penile shaft.
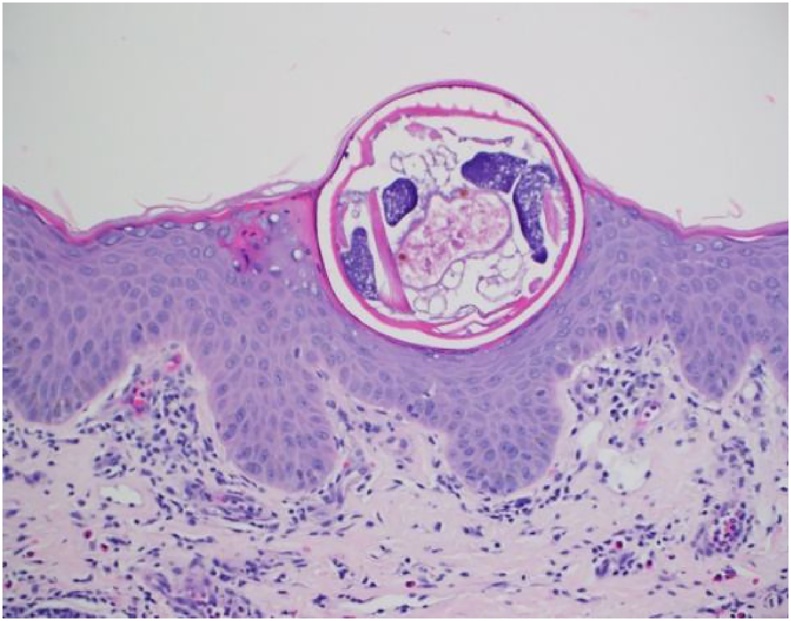
Shave biopsy and histopathology of the lesion from the glans penis showed intracorneal scabies mite and dense mixed dermal lymphocytic inflammation with eosinophils (Fig. 2).
Fig. 2.
Intracorneal scabies mite.
The hallmark presentation of scabies is pruritic cutaneous eruption that is worse at night. Although nearly any area of the body may be involved, scabies infestation often involves finger webspaces, wrists, axilla, and genitals. Papules or nodules on the penis and/or scrotum may also be a presenting sign [2]. Nodular scabies is a less common manifestation of classic scabies, characterized by persistent, firm, erythematous, extremely pruritic nodules, often involving the genitalia. It is thought to represent a hypersensitivity reaction which may persist despite administration of antiparasitic therapy [3].
Diagnosis of scabies is confirmed through visualization of mites, eggs, or fecal pellets through microscopy. It can also be diagnosed clinically through compatible history, clinical examination, and close contact with an individual with similar signs or symptoms or known scabies [4].
Topical and oral treatments are effective. Treatment of close contacts and measures to ensure textiles have been appropriately decontaminated are important. Topical treatment with permethrin 5% cream is first-line agent in management of scabies. It should be applied to the entire skin, only avoiding the eyes, nose, and mouth. It is left overnight and rinsed off in the morning. Ivermectin is an oral antiparasitic that can be given for as a single dose. Both treatments are typically repeated after 7–14 days to ensure clearance, and have cure rates above 90 % [2].
Sources of funding
No funding.
Consent
Mayo Clinic is allowed by Minnesota state law to use medical records for research unless patient has opted out. Patient did not opt out.
Author contribution
All authors contributed significantly to writing the manuscript.
Declaration of Competing Interest
The authors report no declarations of interest.
References
- 1.Otero L., Varela J., Espinosa E., Sanchez C., Junquera M.L., del Valle A. Sarcoptes scabiei in a Sexually Transmitted Infections Unit: A 15-Year Study. Sex Transm Dis. 2004;31(12):761–765. doi: 10.1097/01.olq.0000145853.35574.18. [DOI] [PubMed] [Google Scholar]
- 2.Thomas C., Coates S., Engelman D., Chosidow O., Chang A. Ectoparasites. J Am Acad Dermatol. 2020;82(3):533–548. doi: 10.1016/j.jaad.2019.05.109. [DOI] [PubMed] [Google Scholar]
- 3.Cohen P. Classic and non-classic (Surrepticius) scabies: diagnostic and treatment considerations. Cureus. 2020 doi: 10.7759/cureus.c30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Engelman D., Yoshizumi J., Hay R., Osti M., Micali G., Norton S. The 2020 IACS consensus criteria for the diagnosis of Scabies. Br J Dermatol. 2020 doi: 10.1111/bjd.18943. [DOI] [PMC free article] [PubMed] [Google Scholar]