Abstract
Comorbidities are common risk factors for rising cardiac troponin in non-acute coronary syndromes conditions. Furthermore, the risk for all-cause mortality appears to be correlated to the troponin levels. Consequently, measurement of cardiac troponin in hospital admission may contribute to predict the mortality risk in elderly patients. Among geriatric patients without acute coronary syndrome, with concomitant diseases, the correct interpretation of elevated cardiac troponin, particularly in emergency conditions poses a diagnostic dilemma. Although in several studies it is suggested that at the presence of comorbidity, there is an increase in cardiac troponin values, the elderly patients have not been included conclusively. In order to assess the diagnostic and prognostic role of cardiac troponin elevation in geriatric patients suffering from chronic diseases, a systematic review was performed. The study included the elderly patients free of acute coronary syndrome admitted to the hospital with concomitant disease, with a report of at least one cardiac troponin measurement. We found that elevated cardiac troponin is an independent prognostic factor, predicting all-cause morbidity and mortality burden in geriatric patients without acute coronary syndromes.
Keywords: Cardiac troponin, Elderly patients without acute coronary syndrome, Chronic diseases
1. Introduction
Cardiac troponin (cTn) is a highly sensitive and specific protein, that can be released during myocardial cell injury, consequently it has been introduced as a preferred biomarker for diagnosis of acute coronary syndrome (ACS) [1]. Two different subtypes of cTn, called high-sensitivity cardiac troponin T (hs-cTnT), and high-sensitivity cardiac troponin I (hs-cTnI), are available in clinical practice and may be used interchangeably [2].
cTn elevation that occurs in elderly patients has been shown not always being related to ACS [3]. Considering that the observation of the unexpected increased concentration of cTn in elderly patients without ACS is a serious challenge for its interpretation, particularly across the emergency ward, it is indispensable to understand the differential diagnosis and clinical role of an elevated cTn value. Accordingly, misdiagnosis could be prevented. Therefore, careful attention should be paid to any condition that can be associated with increased cTn values in this population.
Although elevated cTn values have been addressed as a significant independent risk factor for mortality and morbidity in elderly with diabetes mellitus (DM) [4], hypertension (HTN) [5], renal insufficiency (RI) [6], [7], cardiomyopathy (CM) [8], pulmonary hypertension (PHTN) [9], chronic obstructive pulmonary disease (COPD) [10], stroke [11], [12], [13], obstructive sleep apnea (OSA) [14], and different types of cancer [15], [16], [17], a systematic review to identify the underlying cause of an elevated cTn values for this proportion of elderly patients is scarce.
The aim of current study is to review the published literature regarding the significance of cTn elevations in geriatric patients who do not experience ACS.
2. Research method
2.1. Data source and literature search strategy
An extensive evaluation of original articles and reviews from March 1990 to January 2020, written in English and French, and including participants ≥65 years of age, was systematically used. Embase and PubMed in addition to Scopus were applied by using the following Medical Subject Headings phrase strategy: (‘‘comorbidity’’ OR ‘‘concomitant disease’’) AND (‘‘cardiac troponin’’ OR ‘‘cardiac biomarkers’’). The following mesh terms were used to carefully collect the relevant literature and to identify any potential inconsistencies as well: (“free of acute coronary syndrome”), with a combination of subtitles such as: [non-ACS] OR [without acute myocardial infarction] AND [cardiac biomarkers] OR [cardiac troponin] OR [cTnI] OR [cTnT] OR [troponin assays] OR [hs-cTnT] OR [hs-cTnI] AND [aged patients] OR [older adults] OR [elderly patients] OR [geriatric patients] AND [concomitant diseases] OR [comorbidity].
For this study, the full texts of the potentially related publications were obtained and integrated in order not to miss relevant articles. Titles and abstracts were then reviewed, and the studies were selected based on these full texts.
2.2. Study selection
A standardized data collection form was used to evaluate each article meeting the inclusion criteria by two authors (S.S. and T.F.). Any discrepancies were resolved upon discussion by consensus of all authors. We retrieved first author's surname, publication year, region of study performed, study population information (sample size, age range, cut-off value of cardiac troponin), the cardiac troponin assay (hs-cTnT, hs-cTnI), the reported level for troponin and any type of comorbidity. A concentration of hs-cTn above the assay-specific upper reference limit, more than 14 ng/L, was considered as the cut-off point for increased cardiac troponin in the elderly [18]. The quality items for each study selection are shown in Supplementary Table 1. The response for each item is graded as: Yes, Partly or Not available.
3. Results
3.1. Search results and selected articles
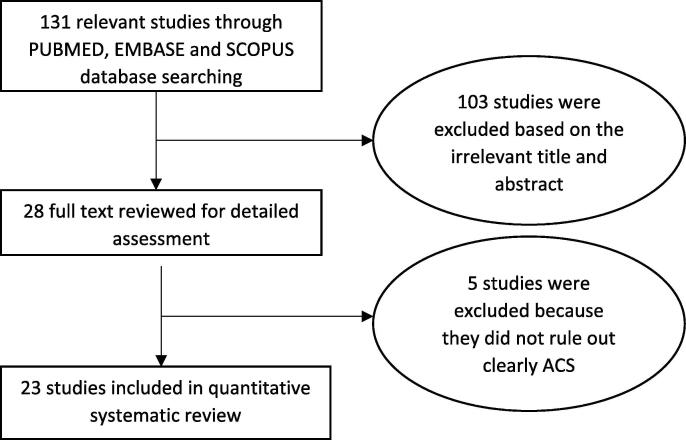
There were 23 relevant articles out of 131 that was initially studied (Fig. 1). The review of the collected articles yields poor outcome, mostly due to inadequate consensus on the definition of elderly, not considering all the causes of high troponin level or comorbidity and not including the geriatric patients without ACS.
Fig. 1.
Flow diagram of the study selection process.
For the assessment of the methodological quality of each study (Supplementary Table 1), and also in order to reduce any possible biases such as the performance bias, detection bias, and attrition bias as much as possible, a maximal 9-star Newcastle–Ottawa Scale (NOS) of cohort studies was used and adopted [19]. According to the NOS score, study awarding 7 or more was considered as good quality (Table 1).
Table 1.
Summary of included studies.
| Source, year | Type of study | Comorbidity | Country | NOS |
|---|---|---|---|---|
| Tang et al., 2020 [4] | retrospective | DM, CKD, HTN, HF, COPD, stroke, frailty, dementia | USA | 9 |
| Sedighi et al., 2020 [23] | retrospective | anemia, hypothyroidism, pneumonia, cancer, CVA, CM, DM, PE, SAH, HTN, PHTN, COPD, RI, ASVD | Canada | 8 |
| Di Micoli et al., 2019 [27] | retrospective | DM, CKD, sepsis + aging | Italy | 7 |
| Crewdson et al., 2019 [21] | retrospective | Post- trauma ICU admission | UK | 7 |
| Sedighi et al., 2019 [22] | retrospective | Ageing, anemia, hypothyroidism, pneumonia, cancer, CVA, CM, DM, PE, SAH, HTN, PHTN, COPD, RI, ASVD + aging | Canada | 7 |
| Árnadóttir et al., 2018 [28] | prospective | stroke, PAD, COPD, DM, HTN along with ESRD | Denmark | 7 |
| Xu et al., 2018 | meta‐analysis | PHTN | China | 7 |
| Fan et al., 2018 [9] | meta‐analysis | Acute ischemic stroke | China | 7 |
| Dziadkowiak et al., 2018 [12] | retrospective | Acute phase of stroke | Poland | 6 |
| VanHouten et al., 2018 [13] | retrospective | Acute Ischemic Stroke | USA | 6 |
| Vestergaard et al., 2016[26] | cross-sectional | HF, LVH, CKD, DM | Denmark | 7 |
| Pavasini et al., 2015 [10] | Systematic review and meta-analysis | AECOPD | Italy | 7 |
| Arshed et al., 2015 [25] | case report with review of literature | AD, arrhythmia, CM, HF, cardiac contusion/manipulation, sepsis, PE, ARDS, stroke, strenuous exercise, cardiac infiltrative disease, toxins | USA | 7 |
| McEvoy et al., 2015 [5] | prospective | HTN | USA | 8 |
| Liu et al., 2015[24] | prospective | sepsis, shock, COPD, ARF, vasopressor medications | USA | 7 |
| Bardají et al., 2015 [29] | retrospective | HTN, DM, HF, PVD, CVD, RI | Spain | 7 |
| Rahman et al., 2014 [30] | review article | sepsis, PE, RI, HF, pericarditis, stroke, arrhythmia, CM, cardiac contusion | Australia | 6 |
| Dubin et al., 2013 [7] | cross-sectional | CKD | USA | 7 |
| Kubo et al., 2013 [8] | retrospective | CM | Japan | 7 |
| Randby et al., 2012 [14] | cross-sectional | OSA | Norway | 7 |
| Røsjø et al., 2011 [20] | prospective | sepsis | Norway | 7 |
| McGill et al., 2010 [6] | prospective | renal disease | Australia | 7 |
| Jeremias et al., 2005 [31] | narrative review | sepsis, hypovolemia, atrial fibrillation, CHF, PE, myocarditis, myocardial contusion, and RI | USA | 7 |
DM (diabetes mellitus), CKD(chronic kidney disease), HTN(hypertension), HF(heart failure), COPD(chronic obstructive pulmonary disease), CVA (cerebrovascular accident), CM(cardiomyopathy), PE (pulmonary embolism), SAH (subarachnoid hemorrhage), PHTN(pulmonary hypertension), RI(renal insufficiency), ASVD(atherosclerotic vascular disease), CRF(chronic renal failure), LVH(left ventricular hypertrophy), ESRD(end-stage renal disease), AECOPD(acute exacerbation of chronic obstructive pulmonary disease), AD (aortic dissection), ARDS(acute respiratory distress syndrome), PVD(peripheral vascular disease), ARF(acute renal failure), OSA(obstructive sleep apnea).
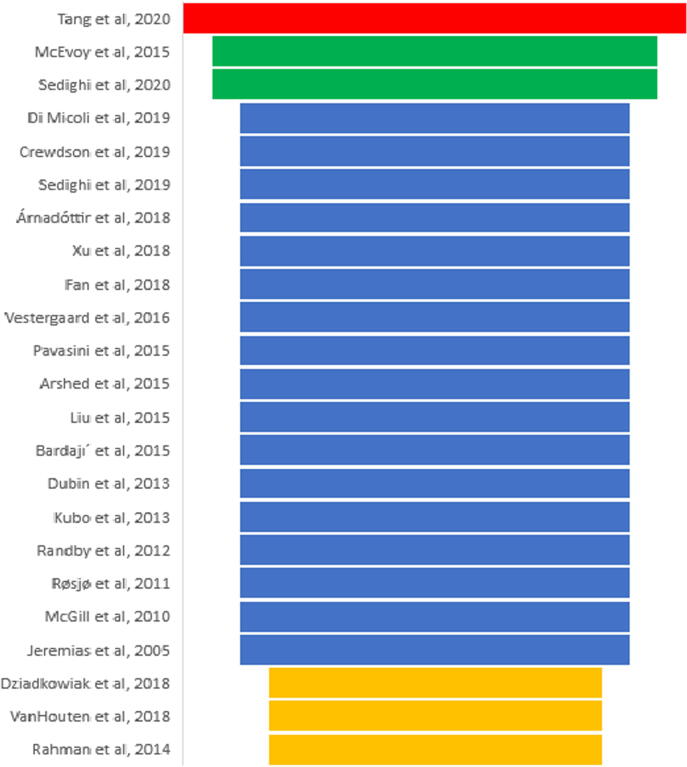
The funnel diagram (Fig. 2) was used to quickly visualize the best qualified studies according to NOS.
Fig. 2.
Funnel diagram according to NOS criteria for each study (red = 9-star, green = 8-star, blue = 7-star, yellow = 6-star). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
In general, all included studies had a moderate-to-good methodological quality. The main finding of this study revealed that there is a comorbidity-induced risk for rising cTn. The table 1 is the conclusion of all provided studies.
3.2. Study populations
Our literature review showed that in numerous studies both the young (<65 years old) and the elderly or geriatric patients (≥65 years) were included in order to explore the data on geriatric patients. Four studies out of 23 have exclusively included the geriatric patients without ACS [4], [22], [23], [27] (Table 2).
Table 2.
The characteristic of studies exclusively related to the geriatric patients.
| Total patients | Objective | Results | |
|---|---|---|---|
| Tang et al. [4] | 1835 | assess the relation between the geriatric syndrome (dementia and frailty) and elevated cTn values, and the use of cTn to stratify mortality risk in DM |
|
| Sedighi et al. [23] | 7062 | determine the relationship between cTn elevation and individual comorbidities, and estimate the impact of each comorbidity on cTn levels |
|
| Sedighi et al. [22] | 6822 | determine the impact of aging on cTn levels in the presence of comorbidities |
|
| Di Micoli et al. [27] | 443 | determine the possibility of correlation between the two different troponin T and I, and age |
|
cTn (cardiac troponin), DM (diabetes mellitus), RI (renal insufficiency), CM (cardiomyopathy), COPD (chronic obstructive pulmonary disease).
In our systematic review, most studies have included patients of all ages [5], [21], [22], [23], [25], [26], nine studies measured cTnT [5], [6], [7], [8], [14], [17], [18], [19], [20] and three studies measured cTnI [13], [24], [25]. Two articles conducted by the same authors, with relatively the same database, compared the influence of age and individual comorbidity of cTn value [22], [23].
3.3. Origin of evaluated studies
Three studies out of the 23 were meta-analysis [9], [10], [11], four systematic and narrative review [25], [30], [31], [32], four prospective [6], [20], [24], [26], whereas twelve studies [4,5,7,8,12–14,21–27,29] were retrospective in nature.
Seven studies were conducted in the United States [5], [7], [13], [24], [25], [31], [33], two in Canada [22], [23], nine in Europe [4], [10], [12], [20], [21], [26], [27], [29], [32], two in Australia [6], [30], and three studies in Asia [8], [9], [11].
3.4. Variables
The interested variables were introduced as the response variable (at least one documented measurement of cTn) and the categorical variables (comorbidities).
There were seventeen categorial variables: anemia, cerebrovascular accident (CVA), cancer, cardiomyopathy (CM), DM, pulmonary embolism (PE), subarachnoid hemorrhage (SAH), HTN, PHTN, hypothyroidism, pneumonia, COPD, RI, end stage renal disease (ESRD), septicemia, peripheral arterial/vascular disease, and arteriosclerotic vascular disease (ASVD). In the collected studies, each comorbidity has been weighted along with the physician's diagnosis.
3.5. Analytical outcomes
At first glance on the collected data, it is found that the cTn value is raised in comorbidity, regardless of age and ACS. Moreover, the mortality profile reveals a linear correlation with elevated cTn in the collected studies. The existence of both publication and selection bias were observed in the general analysis of all-cause mortality.
Considering having age heterogeneity to the large extent of the collected studies versus few numbers of relevant studies, employing a meta-analysis was not appropriate in a practical sense. Table 1 refers to the characteristic of included study.
The prognostic role of cTn was explored individually for COPD [10], acute stroke [11], critically care patients [21], [24], HTN [5] and for RF, PAD, arrhythmia, HF and DM as well [28]. Therefore, the prognostic implications of elevated cTn seem to be correlated with all-cause mortality in geriatric patients without ACS.
A meta-analysis study on circulating cTn level summarized that an increase in cTn levels was more common among older patients with acute ischemic stroke and associated with poor outcome and mortality as well [11].
Although an exclusive retrospective study suggested that aging could be considered mostly an independent factor for rising cTn in the elderly potentially without ACS [22], the significance of each comorbidity was not included.
According to a recent study that has evaluated fourteen comorbidities in roughly 7000 elderly patients who were free of ACS, elevated hs-cTnT levels were observed statistically significant for RI, cardiomyopathy, COPD, DM, and anemia (p < 0.0001) [23]. Moreover, regardless of age, the influence of HTN, HF, PVD (peripheral vascular disease), CVD (cerebrovascular disease), and renal disease on cTn has been significantly shown [28], [29].
One study presented that the elevated cTn implications could be along with severity of sepsis [20], thus, it could be introduced as an early biomarker in septic shock. Interestingly, after excluding sepsis or other confounding comorbidities, the prognostic performance of rising cTn among CVA patients is equally important [13].
After applying a rigorous approach to all the collected literature, only in one study, the authors significantly adjusted the influence of individual concomitant disease on cTn value as RI, cardiomyopathy, COPD, DM, and anemia in geriatric patients [23].
4. Discussion
The main purpose of the present study was to conduct a systematic review of literature with regards to the significance of rising cTn in elderly patients without ACS.
Interestingly, we have found that there is an unwritten agreement reached on the impact of concomitant disease on troponin value. It is appropriate to use the expression “Troponinemia“ to reflect any condition that is correlated to elevated cTn.
According to our review, the significance of elevated cTn role was to be able to predict independently mortality in geriatric patients with concomitant diseases, individually for COPD, RI, HF, DM, CVD, and sepsis [10], [11], [13], [20], [23], [28]. Therefore, our study clearly determines that cTn may be viewed as a prognostic test. Therefore, cTn has the potential to predict patients' outcomes and it is required to be considered in medical interventions to improve mortality profile. Moreover, troponinemia could provide more accurate prognostic information than comorbidity alone. It is thus essential to consider also cTn level while the physician is treating a chronic pathological process or evaluating pharmacological responses to any related interventions.
Significantly, cTn has evolved from a non-significant tool [34] to a “diagnostic and prognostic indicator in end-stage renal disease (ESRD) [35]. As reviewed, the ESRD elderly patients with troponinemia- preferably measuring cTnT- above optimal cut-off point presented with worsening mortality profile [6], [7]. It is still unclear how to exactly explain this result in ESRD elderly patients with acute troponinemia, without ACS as well as in case of the other co-morbidities from the studies included in this systematic review.
With regards to troponinemia in geriatric patients experiencing sepsis and CVA [13], [20], it is suggested to consider the prognostic performance of elevated cardiac troponin. It is suggested that physicians should offer a judicious strategy to pursue additional cardiovascular evaluation in a patient with CVA and troponinemia.
Although the correlation between cTn and comorbidity has been individually studied [4], [5], [6], [8], [10], [11], [12], [13], [14], [20], [35], the possibility of simultaneous comorbidities is not clarified. Therefore, there is higher probability of selection bias.
In an exclusive study, the cumulative effects of comorbidities are more prominent than those produced by individual chronic disease alone [22]. However, the degree of severity of each comorbidity has not been determined. It is reasonable to assume that any changes in the severity of individual diseases, causes a change in the level of troponinemia.
A few studies have reported that cardiac biomarkers including troponin could be considered as a prognostic value to predict mortality and cardiovascular health in patients suffering from various cancer stages independently of the cancer type, age and even treatment [15], [16], [17]. Consequently, it would be judicious to measure the troponin level serially which is a specific biomarker of cardiac damage in all cancer patients to determine either the presence of previous CVD or the dynamic of its changes during the cancer treatment to intervene as adequately as possible.
Although in literature, it is generally proposed that the cTn concentrations progressively increase with age [27], [36], [37], two studies have proposed to consider troponinemia independent from age [22], [23]. To justify the above proposed contention, it is not simply referring to aging at large, but specifically to healthy aged people where the cTn level was found below the defined normal range. In other words, even if aging is a risk factor for cardiovascular disease, it did not correlate with troponin levels. Although false-positive elevation of cTn could be rarely observed in the absence of cardiac or non-cardiac diseases [32], it is even more crucial to exclude all likelihood of ACS in elderly patients. This corroborate all the studies showing the role of troponinemia in elderly with comorbidities after exclusion of ACS.
5. Conclusion
Elevated cardiac troponin is an independent prognostic factor, beyond traditional cardiovascular risk factors, predicting all-cause morbidity and mortality burden in geriatric patients free of ACS.
Given that there is a higher cardiac troponin level in geriatric patients at the presence of any comorbidity it is essential for physicians to care and follow for these elevated troponin levels. This is absolutely essential by further studies to understand the cause(s) underlying the prognostic role of the cTn increased level.
6. Ethics
The present study was done according to previously published studies. Consequently, ethical approval and informed consent were not required.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijcha.2020.100629.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Thygesen K., Alpert J.S., Jaffe A.S., Chaitman B.R., Bax J.J., Morrow D.A., White H.D., Executive Group on behalf of the Joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF) Task Force for the Universal Definition of Myocardial Infarction Fourth Universal Definition of Myocardial Infarction (2018) J. Am. College Cardiol. 2018;72(18):2231–2264. doi: 10.1016/j.jacc.2018.08.1038. [DOI] [PubMed] [Google Scholar]
- 2.Thygesen K., Alpert J.S., Jaffe A.S., Simoons M.L., Chaitman B.R., White H.D., Joint ESC/ACCF/AHA/WHF Task Force for Universal Definition of Myocardial Infarction, Authors/Task Force Members Chairpersons, Thygesen K., Alpert J.S., White H.D., Biomarker Subcommittee, Jaffe A.S., Katus H.A., Apple F.S., Lindahl B., Morrow D.A., ECG Subcommittee, Chaitman B.R., Clemmensen P.M. Third universal definition of myocardial infarction. J. Am. College Cardiol. 2012;60(16):1581–1598. doi: 10.1016/j.jacc.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 3.Alcalai R. Acute coronary syndrome vs Nonspecific troponin elevation. Arch. Int. Med. 2007;167(3):276. doi: 10.1001/archinte.167.3.276. [DOI] [PubMed] [Google Scholar]
- 4.Tang O., Daya N., Matsushita K., Coresh J., Sharrett A.R., Hoogeveen R., Jia X., Windham B.G., Ballantyne C., Selvin E. Performance of high-sensitivity cardiac troponin assays to reflect comorbidity burden and improve mortality risk stratification in older adults with diabetes. Diabetes Care. 2020:dc192043. doi: 10.2337/dc19-2043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McEvoy J.W., Chen Y., Nambi V., Ballantyne C.M., Sharrett A.R., Appel L.J., Post W.S., Blumenthal R.S., Matsushita K., Selvin E. High-sensitivity cardiac troponin T and risk of hypertension. Circulation. 2015;132(9):825–833. doi: 10.1161/circulationaha.114.014364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McGill D., Talaulikar G., Potter J.M., Koerbin G., Hickman P.E. Over time, high-sensitivity TnT replaces NT-proBNP as the most powerful predictor of death in patients with dialysis-dependent chronic renal failure. Clin. Chim. Acta; Int. J. Clin. Chem. 2010;411(13–14):936–939. doi: 10.1016/j.cca.2010.03.004. [DOI] [PubMed] [Google Scholar]
- 7.Dubin R.F., Li Y., He J., Jaar B.G., Kallem R., Lash J.P., Makos G., Rosas S.E., Soliman E.Z., Townsend R.R., Yang W., Go A.S., Keane M., Defilippi C., Mishra R., Wolf M., Shlipak M.G., CRIC Study Investigators Predictors of high sensitivity cardiac troponin T in chronic kidney disease patients: a cross-sectional study in the chronic renal insufficiency cohort (CRIC) BMC Nephrol. 2013;14:229. doi: 10.1186/1471-2369-14-229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kubo T., Kitaoka H., Yamanaka S., Hirota T., Baba Y., Hayashi K., Iiyama T., Kumagai N., Tanioka K., Yamasaki N., Matsumura Y., Furuno T., Sugiura T., Doi Y.L. Significance of high-sensitivity cardiac troponin T in hypertrophic cardiomyopathy. J. Am. College Cardiol. 2013;62(14):1252–1259. doi: 10.1016/j.jacc.2013.03.055. [DOI] [PubMed] [Google Scholar]
- 9.Xu S.L., Yang J., Zhang C.F., Xu S.Y., Zhao F.Y., Liu L.Q., Xie C.L., Xing X.Q., Zhu Y. Serum cardiac troponin elevation predicts mortality in patients with pulmonary hypertension: a meta-analysis of eight cohort studies. Clin. Resp. J. 2019;13(2):82–91. doi: 10.1111/crj.12991. [DOI] [PubMed] [Google Scholar]
- 10.Pavasini R., D'Ascenzo F., Campo G., Biscaglia S., Ferri A., Contoli M., Papi A., Ceconi C., Ferrari R. Cardiac troponin elevation predicts all-cause mortality in patients with acute exacerbation of chronic obstructive pulmonary disease: Systematic review and meta-analysis. Int. J. Cardiol. 2015;191:187–193. doi: 10.1016/j.ijcard.2015.05.006. [DOI] [PubMed] [Google Scholar]
- 11.Fan Y., Jiang M., Gong D., Man C., Chen Y. Cardiac troponin for predicting all-cause mortality in patients with acute ischemic stroke: a meta-analysis. Biosci. Reports. 2018;38(2) doi: 10.1042/BSR20171178. BSR20171178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dziadkowiak E., Chojdak J., Guziński M., Lewczuk K., Noga L. Troponin levels in patients in acute phase of stroke. J. Cardiovasc. Med. Cardiol. 2018;5(4):053–058. doi: 10.17352/2455-2976.000072. [DOI] [Google Scholar]
- 13.VanHouten J., Fricker G., Collins B., Bhatia R., Ellis C., Schrag M. Circulating Troponin I level in patients with acute ischemic stroke. Curr. Neurol. Neurosci. Rep. 2018;18(6):32. doi: 10.1007/s11910-018-0842-6. [DOI] [PubMed] [Google Scholar]
- 14.Randby A., Namtvedt S.K., Einvik G., Hrubos-Strøm H., Hagve T.A., Somers V.K., Omland T. Obstructive sleep apnea is associated with increased high-sensitivity cardiac troponin T levels. Chest. 2012;142(3):639–646. doi: 10.1378/chest.11-1779. [DOI] [PubMed] [Google Scholar]
- 15.Pavo N., Raderer M., Hülsmann M., Neuhold S., Adlbrecht C., Strunk G., Goliasch G., Gisslinger H., Steger G.G., Hejna M., Köstler W., Zöchbauer-Müller S., Marosi C., Kornek G., Auerbach L., Schneider S., Parschalk B., Scheithauer W., Pirker R., Drach J., Pacher R. Cardiovascular biomarkers in patients with cancer and their association with all-cause mortality. Heart (British Cardiac Society) 2015;101(23):1874–1880. doi: 10.1136/heartjnl-2015-307848. [DOI] [PubMed] [Google Scholar]
- 16.Zheng P.P., Li J., Kros J.M. Breakthroughs in modern cancer therapy and elusive cardiotoxicity: critical research-practice gaps, challenges, and insights. Med. Res. Rev. 2018;38(1):325–376. doi: 10.1002/med.21463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cardinale D., Sandri M.T., Colombo A., Colombo N., Boeri M., Lamantia G., Civelli M., Peccatori F., Martinelli G., Fiorentini C., Cipolla C.M. Prognostic value of troponin I in cardiac risk stratification of cancer patients undergoing high-dose chemotherapy. Circulation. 2004;109(22):2749–2754. doi: 10.1161/01.CIR.0000130926.51766.CC. [DOI] [PubMed] [Google Scholar]
- 18.Reiter M., Twerenbold R., Reichlin T., Haaf P., Peter F., Meissner J., Hochholzer W., Stelzig C., Freese M., Heinisch C., Breidthardt T., Freidank H., Winkler K., Campodarve I., Gea J., Mueller C. Early diagnosis of acute myocardial infarction in the elderly using more sensitive cardiac troponin assays. Eur. Heart J. 2011;32(11):1379–1389. doi: 10.1093/eurheartj/ehr033. [DOI] [PubMed] [Google Scholar]
- 19.G. Wells, B. Shea, D. O’Connell, J. Peterson, V. Welch, M. Losos, et al., The Newcastle-Ottawa Scale (NOS) for assessing the quality if nonrandomized studies in meta-analyses. Available at: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
- 20.Røsjø H., Varpula M., Hagve T.A., Karlsson S., Ruokonen E., Pettilä V., Omland T., FINNSEPSIS Study Group Circulating high sensitivity troponin T in severe sepsis and septic shock: distribution, associated factors, and relation to outcome. Intensive Care Med. 2011;37(1):77–85. doi: 10.1007/s00134-010-2051-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Crewdson K., Thompson J., Thomas M. Cardiac troponin T is associated with mortality in patients admitted to critical care in a UK major trauma centre: a retrospective database analysis. J. Intensive Care Soc. 2019;20(2):132–137. doi: 10.1177/1751143718767782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sedighi S.M., Prud'Homme P., Ghachem A., Lepage S., Nguyen M., Fulop T., Khalil A. Increased level of high-sensitivity cardiac Troponin T in a geriatric population is determined by comorbidities compared to age. International journal of cardiology. Heart Vasc. 2019;22:187–191. doi: 10.1016/j.ijcha.2019.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.S.M. Sedighi, T. Fulop, A. Mohammadpour, M. Nguyen, P. Prud’Homme, A. Khalil, Elevated cardiac troponin levels in geriatric patients without ACS: role of comorbidities, CJC Open (2020), https://doi.org/10.1016/j.cjco.2020.07.017. [DOI] [PMC free article] [PubMed]
- 24.Liu M., Shehu M., Herrold E., Cohen H. Prognostic value of initial elevation in cardiac troponin I level in critically ill patients without acute coronary syndrome. Critical Care Nurse. 2015;35(2):e1–e10. doi: 10.4037/ccn2015300. [DOI] [PubMed] [Google Scholar]
- 25.Arshed S., Luo H.X., Zafar S., Regeti K., Malik N., Alam M., Yousif A. Elevated Troponin I in the absence of coronary artery disease: a case report with review of literature. J. Clin. Med. Res. 2015;7(10):820–824. doi: 10.14740/jocmr2280w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vestergaard K.R., Jespersen C.B., Arnadottir A., Sölétormos G., Schou M., Steffensen R., Goetze J.P., Kjøller E., Iversen K.K. Prevalence and significance of troponin elevations in patients without acute coronary disease. Int. J. Cardiol. 2016;222:819–825. doi: 10.1016/j.ijcard.2016.07.166. [DOI] [PubMed] [Google Scholar]
- 27.Di Micoli A., Scarciello C., De Notariis S., Cavazza M., Muscari A. Determinants of troponin T and I elevation in old patients without acute coronary syndrome. Emergency Care J. 2019;15(1) doi: 10.4081/ecj.2019.7798. [DOI] [Google Scholar]
- 28.Árnadóttir Á., Vestergaard K.R., Pallisgaard J., Sölétormos G., Steffensen R., Goetze J.P., Iversen K. High-sensitivity cardiac troponin T is superior to troponin I in the prediction of mortality in patients without acute coronary syndrome. Int. J. Cardiol. 2018;259:186–191. doi: 10.1016/j.ijcard.2018.01.131. [DOI] [PubMed] [Google Scholar]
- 29.Bardají A., Cediel G., Carrasquer A., De Castro R., Sánchez R., Boqué C. Troponin elevation in patients without acute coronary syndrome. Revista Española de Cardiología (English Edition) 2015;68(6):469–476. doi: 10.1016/j.rec.2014.10.018. [DOI] [PubMed] [Google Scholar]
- 30.Rahman A., Broadley S.A. Review article: elevated troponin: diagnostic gold or fool's gold? Emergency Med. Austral.: EMA. 2014;26(2):125–130. doi: 10.1111/1742-6723.12203. [DOI] [PubMed] [Google Scholar]
- 31.Jeremias A., Gibson C.M. Narrative review: alternative causes for elevated cardiac troponin levels when acute coronary syndromes are excluded. Ann. Internal Med. 2005;142(9):786–791. doi: 10.7326/0003-4819-142-9-200505030-00015. [DOI] [PubMed] [Google Scholar]
- 32.Tanindi A., Cemri M. Troponin elevation in conditions other than acute coronary syndromes. Vascular Health Risk Manage. 2011;7:597–603. doi: 10.2147/VHRM.S24509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mantzouris T., Gauer R., Mackler L. Clinical Inquiry: elevated troponin but no CVD: what's the prognosis? J. Family Practice. 2013;62(10):585–598. [PubMed] [Google Scholar]
- 34.Van Lente F., McErlean E.S., DeLuca S.A., Peacock W.F., Rao J.S., Nissen S.E. Ability of troponins to predict adverse outcomes in patients with renal insufficiency and suspected acute coronary syndromes: a case-matched study. J. Am. College Cardiol. 1999;33(2):471–478. doi: 10.1016/s0735-1097(98)00592-0. [DOI] [PubMed] [Google Scholar]
- 35.Khan N.A., Hemmelgarn B.R., Tonelli M., Thompson C.R., Levin A. Prognostic value of troponin T and I among asymptomatic patients with end-stage renal disease: a meta-analysis. Circulation. 2005;112(20):3088–3096. doi: 10.1161/CIRCULATIONAHA.105.560128. [DOI] [PubMed] [Google Scholar]
- 36.Eggers K.M., Jaffe A.S., Lind L., Venge P., Lindahl B. Value of cardiac troponin I cutoff concentrations below the 99th percentile for clinical decision-making. Clin. Chem. 2009;55(1):85–92. doi: 10.1373/clinchem.2007.101683. [DOI] [PubMed] [Google Scholar]
- 37.D.L. Kasper, A.S. Fauci, S.L. Hauser, D.L. Longo, J.L. Jameson, J. Loscalzo, Harrison's principles of internal medicine 19/E, vols.1 & 2, (ebook), McGraw Hill Professional, 2015.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.