Abstract
Recognizing that health outcomes are influenced by and occur within multiple social and physical contexts, researchers have used multilevel modeling techniques for decades to analyze hierarchical or nested data. Cross-Classified Multilevel Models (CCMM) are a statistical technique proposed in the 1990s that extend standard multilevel modeling and enable the simultaneous analysis of non-nested multilevel data. Though use of CCMM in empirical health studies has become increasingly popular, there has not yet been a review summarizing how CCMM are used in the health literature. To address this gap, we performed a scoping review of empirical health studies using CCMM to: (a) evaluate the extent to which this statistical approach has been adopted; (b) assess the rationale and procedures for using CCMM; and (c) provide concrete recommendations for the future use of CCMM. We identified 118 CCMM papers published in English-language literature between 1994 and 2018. Our results reveal a steady growth in empirical health studies using CCMM to address a wide variety of health outcomes in clustered non-hierarchical data. Health researchers use CCMM primarily for five reasons: (1) to statistically account for non-independence in clustered data structures; out of substantive interest in the variance explained by (2) concurrent contexts, (3) contexts over time, and (4) age-period-cohort effects; and (5) to apply CCMM alongside other techniques within a joint model. We conclude by proposing a set of recommendations for use of CCMM with the aim of improved clarity and standardization of reporting in future research using this statistical approach.
Keywords: Cross-classified multilevel modeling, Area-level effects, Contextual effects, Age period cohort effects
1. Introduction
There has been substantial interest among researchers in understanding multilevel phenomena, including how features of the physical and psychosocial environment in which individuals live, learn, work, and play are associated with individual health, disease, and behavior (Mair, Diez Roux, & Galea, 2008; Pickett & Pearl, 2001). This interest can be traced partially to theoretical works describing the nesting of individuals in multiple social ecologies (see for example Bronfenbrenner & Morris, 2006; Dunn, Masyn, Yudron, Jones, & Subramanian, 2014; Krieger, 2001; Stokols, 1996) as well as advances in statistical modeling, namely multilevel modeling (MLM) or hierarchical linear modeling (HLM) (Aitkin, Anderson, & Hinde, 1981; Diez Roux, 1998, 2002; Raudenbush & Bryk, 2002; Subramanian, Jones, & Duncan, 2003). The major achievement of these multilevel methods is that they address weaknesses of standard multiple regression by taking into account the hierarchical or nested structures that arise naturally in most kinds of social data (Fielding & Goldstein, 2006). In doing so, multilevel models enable researchers to expand focus beyond individual-level characteristics to investigate the social and geographic contexts or groups to which individuals belong.
Despite these benefits, a major limitation of standard multilevel models is that they require researchers to study contexts configured according to strict hierarchies, for example a clean hierarchical nesting of students in classrooms and classrooms in schools (see Fig. 1). To overcome this limitation, educational researchers Goldstein and Rasbash (Goldstein, 1994; Rasbash & Goldstein, 1994) developed statistical software and approaches known as cross-classified multilevel models (CCMM). CCMM are an extension of standard hierarchical multilevel models and allow researchers to examine more complex data structures to determine, among other things, what proportion of total variance is attributable to multiple contextual (or area level) units of analysis that do not follow a strict hierarchical structure. These types of data structures are common in social, behavioral, and health data and are referred to as cross-classified data. For example, children may be nested simultaneously in schools and neighborhoods of residence where no clear hierarchies exist between schools and neighborhoods (see Fig. 2). The analytical extensions represented by CCMM are important because multilevel studies are vulnerable to ‘omitted context bias’ (Evans, Onnela, Williams, & Subramanian, 2016; Goldstein, 1994; Meyers & Beretvas, 2006) whereby the variance associated with relevant omitted contexts is misattributed, in part, to the context(s) included in the regression model.
Fig. 1.
Hierarchical multilevel data structure.
XFig. 2.
Cross-classified multilevel data structure.
Excellent resources describing the CCMM approach are available to researchers wishing to capitalize upon its capacity to more accurately model the social reality represented in complex data structures (see, e.g., Goldstein, 2011; Leckie & Bell, 2013). Yet the extent to which this versatile approach has been utilized in empirical health research has not been adequately characterized and remains unknown. An improved understanding of this is necessary to identify emerging issues in the literature that could be addressed in future research and to identify areas of the empirical health literature in which the approach has thus far been underutilized. To address this gap in the literature, we conducted a scoping review to characterize when, why, and how CCMM have been applied to multilevel data in empirical health research. Informed by these findings, we additionally conclude with recommendations for best research practices in the use of CCMM for health researchers wishing to employ this innovative statistical approach.
2. Methods
The aim of a scoping review is to map the body of literature pertaining to a broad topic (Levac, Colquhoun, & O'Brien, 2010). As recommended by Levac et al. (2010), the review began with the establishment of a research team consisting of individuals with expertise in applied CCMM and social epidemiology who provided both methodological and substantive expertise. In coordination with a reference librarian trained in library science, the research team then developed the overall study protocol, including identification of search terms and databases.
2.1. Data sources and search strategy
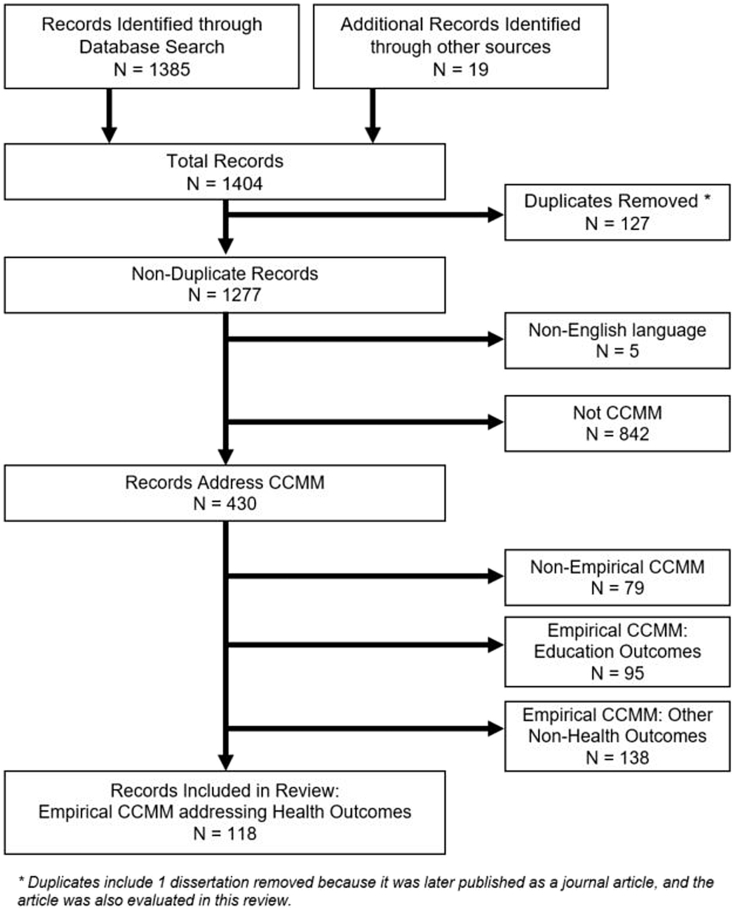
Steps for the review follow those outlined by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) and reflect the synergistic nature of the review process (Moher et al., 2015). Fig. 3 provides a flowchart summarizing the article review and exclusion process. We started with a systematic search of articles published as of February 1, 2018 in the following eight databases: ABI/Inform, Academic Search Premier, Cab Abstract, EconLit, ERIC, PsycINFO, PubMed, and Web of Science. In these databases, we searched for “cross-classified multilevel model.” In addition, searches included instances in which “cross classified” or “cross-classified” was listed eight or fewer words apart from either “multilevel” or “multi-level” in order to identify publications where “cross classified”, with or without the hyphen, was not listed immediately with “multilevel” or “multi-level.” Occasionally authors use CCMM but do not mention it in either the title or abstract; in order to attempt to identify these articles, which would not be captured by the search criteria, we also searched for articles by examining the reference pages of published empirical articles focusing primarily on health. In addition, given that disciplines outside of the health sciences refer to CCMM approaches with different naming protocols, we also searched using the terms “cross-classification” and “cross-classified random effects models,” to be inclusive of studies using this statistical technique under different naming strategies. We acknowledge that despite these attempts, the search terms used here are imperfect and may not have fully captured studies using other disciplinary-specific naming strategies for CCMM. Therefore, we may not have been able to identify all papers using this statistical technique. In addition, in a project of this scope it is always possible (and perhaps even likely) for researchers to misclassify or misunderstand a published piece. We take full responsibility for any misrepresentations of the original study in our synthesis and categorizations.
Fig. 3.
Record Identification and Exclusion.
2.2. Citation management
All citations were imported into the bibliographic manager EndNote, with this software automatically removing duplicate citations. Further duplicates were removed manually when found later in the process.
2.3. Inclusion/exclusion criteria
To be included, studies had to be written in English and use CCMM for at least two levels of analysis. Studies using multiple membership multilevel models were excluded from analysis. Multiple membership multilevel models are closely-related to cross-classified multilevel models in that both can handle non-hierarchical data, however multiple membership models differ methodologically and substantively from CCMM so are not included in this review. From this pool of English-language CCMM studies, we reviewed titles and abstracts to determine whether a study was either a non-empirical or empirical CCMM study. Non-empirical studies (such as theory papers, simulation studies, review articles, and meta-analyses) were excluded. Empirical CCMM studies were further sorted by domain of outcome examined: health, education, and other. For the health studies, we allowed for a range of diverse health and health behavior outcomes, including: mental health, subjective well-being, self-rated health, anthropometric measures, cancer and cardiovascular health, physical activity, and mortality. Included records came from peer-reviewed journal articles, book chapters and dissertations. Abstracts, conference posters, and commentaries were excluded.
2.4. Study selection
Following this initial review process using the abstract and title screening process, we conducted a full-text review of all empirical health studies. Reviewers discussed records throughout this screening process to reach consensus on any uncertainties related to study selection (Levac et al., 2010). After initial full-text review of these publications, it became apparent that some authors examining age, period, and cohort (APC) effects referred to them as hierarchical rather than cross-classified models. To ensure we were not missing literature that referred to CCMM as hierarchical, we conducted a secondary search. The basis of this search was a paper by Yang and Land (2006) that proposed the use of CCMM to examine APC effects. This additional search comprised all citations listed in Google Scholar that cited the original Yang and Land 2006 paper. This resulted in 18 additional empirical health CCMM studies.
2.5. Data extraction
For each study from the empirical health literature, the following information was extracted: author(s), year, publication journal, health outcome, data source, study participants, sample size, reason for use of CCMM, and the multilevel data structure (e.g., student, school, neighborhood). In addition to indexing the studies, the date of publication for each record allowed us to assess growth in the literature over time and the number of studies published by health outcome. For APC studies, the use of CCMM has been highly controversial. We therefore also noted timing of publication for APC studies relative to the publication of the original major critique of this approach (Bell & Jones, 2014) and the extent to which authors addressed this controversy.
2.6. Data summary and synthesis
Data were extracted into a single spreadsheet in Microsoft Excel (2010) for validation and coding for health topic and methodological rationale for use of CCMM. The reporting of this review conforms to recommendations from the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (Moher et al., 2015).
3. Results
3.1. Records identified for review
The search methods yielded 1404 articles (1385 from database searches and 19 from other sources) with 1277 remaining after duplicates were removed. Following title and abstract screening, an additional 847 were subsequently excluded as they were either non-English (n = 5) or did not use CCMM (n = 842). Of 430 publications that did address CCMM, a further 312 were excluded as they focused on topics unrelated to empirical health research: non-empirical CCMM on any domain (n = 79); empirical CCMM studies from education (n = 95) or other non-health outcomes (n = 138). Research areas covered in this latter category included studies from a wide range of disciplines such as economics, political science, sociology, psychology, demography, transportation studies, criminal justice, ecology, forestry, and agriculture. Following the exclusion of these studies, a total of 118 empirical CCMM studies focusing on health outcomes were included in this review. Table 1 provides information on the author, year of publication, journal, health outcome examined, study sample and participants, sample size, data source and structure, and the reason for use of CCMM for non-APC studies. Table 2 provides similar information for studies applying CCMM for APC analysis.
Table 1.
Summary of empirical health studies using cross-classified multilevel models (CCMM) by reason for use of CCMM.
| Authors | Journal | Outcome | Country | Sample Sizea | Data Source | Data Structure |
|---|---|---|---|---|---|---|
| Reason for Use of CCMM: Concurrent Contexts | ||||||
| Aminzadeh et al. (2013) | Social Science & Medicine | Subjective well-being | New Zealand | N = 5567 | Youth 2007 Health Survey | L1: Individuals L2a: Schools L2b: Neighborhoods |
| Bozorgmehr et al. (2015) | Journal of Epidemiology and Community Health | Disease management program enrollment | Germany | N = 1280 | Epidemiological Study for the Prevention, Early Diagnosis and Optimal Treatment of Chronic Diseases in an Elderly Population (ESTHER) | L1: Individuals L2a: Neighborhoods L2b: General Practitioners |
| Cafri and Fan (2018) | Statistical Methods in Medical Research | Hip implant survival | USA | N = 13,920 | Kaiser Permanente Total Joint Replacement Registry | L1: Individuals L2a: Hospitals L2b: Surgeons |
| Carroll-Scott et al. (2015) | American Journal of Public Health | Body mass index (BMI) | USA | N = 811 | Community Interventions for Health Study; School Administrative Records; US Census; School Learning Environment Survey | L1: Individuals L2a: Schools L2b: Neighborhoods |
| Chaix et al. (2012) | PLoS ONE | Body mass index (BMI); Waist circumference | France | N = 7131 | Residential Environment and Coronary Heart Disease | L1: Individuals L2a: Neighborhoods L2b: Supermarket |
| Cheung, Goodman, Leckie, and Jenkins (2011) | Children and Youth Services Review | Externalizing behaviors | Canada | N = 1063 | Ontario Looking after Children (OnLAC) project | L1: Individuals L2a: Foster Families L2b: Foster Care Workers |
| Chum and O'Campo (2013) | Health & Place | Cardiovascular disease risk | Canada | N = 1626 | Neighborhood Effects on Health and Well-being Study | L1: Individuals L2a: Residential Neighborhoods L2b: Workplace Neighborhoods |
| De Clerq et al. (2014) | Social Science & Medicine | Tobacco use | Belgium | N = 8453 | 2005-6 Health Behavior in School-Aged Children Study | L1: Individuals L2a: Communities L2b: Schools |
| Di Martino et al. (2016) | BMJ Open | Adherence to chronic polytherapy after Myocardial Infarction | Italy | N = 9606 | Hospital Information System (patient records) | L1: Individuals L2a: Hospitals of Discharge L2b: Primary Care Providers |
| Di Martino et al. (2017) | Journal of Chronic Obstructive Pulmonary Disease | Adherence to long acting bronchodilators | Italy | N = 13,178 | Hospital Information System (patient records) | L1: Individuals L2a: Hospitals of Discharge L2b: Local Health District |
| Dundas, Leyland, and Macintyre (2014) | American Journal of Epidemiology | Self-rated health and mental health | Scotland | N = 6285 | Aberdeen Children of the 1950s Study | L1: Individuals L2a: Schools L2b: Families L3: Neighborhoods |
| Dunn, Milliren, Evans, Subramanian, and Richmond (2015) | American Journal of Public Health | Depressive symptoms | USA | N = 16,172 | National Longitudinal Study of Adolescent to Adult Health (Add Health) | L1: Individuals L2a: Schools L2b: Neighborhoods |
| Dunn, Milliren, et al. (2015) | Health & Place | Tobacco use | USA | N = 16,070 | National Longitudinal Study of Adolescent to Adult Health (Add Health) | L1: Individuals L2a: Schools L2b: Neighborhoods |
| Ecob et al. (2004) | International Journal of Methods in Psychiatric Research | Ratings of clinical and psychosocial needs of patients (Health of the Nation Outcome Scales (HoNOS)) | UK | N = 384 | Referrals to Secondary Care Psychiatric Services | L1: Individuals L2a: Primary Care Practice L2b: Health Care Professionals in Secondary Site |
| Ecochard and Clayton (1998) | Statistics in Medicine | Conception; pregnancy | France | N = 1901 | Center for the Study and Preservation of Eggs and Sperm | L1: Ovulation Cycles L2a: Women L2b: Sperm Donors |
| Gifford and Foster (2008) | Medical Care | Inpatient length of stay for a given admission | USA | N = 8400 | Tennessee Impact Study | L1: Hospital Admissions L2a: Children L2b: Facility |
| Groenewegen et al. (2018) | Health & Place | All-cause morbidity | Netherlands | N = 1,159,929 |
NIVEL Primary Care Database; Dutch Integral Safety Monitor 2011; Statistics Netherlands | L1: Individuals L2a: General Practitioner Practices L2b: Neighborhoods L3: Municipalities |
| Gross, Herrin, Wong, and Krumholz (2005) | Journal of Clinical Oncology | Likelihood of enrollment in a cancer trial | Australia | N = 36,167 | National Cancer Institute Clinical Trial Evaluation Program Database | L1: Individuals L2a: Protocols L2b: Centers L2c: Counties |
| Hofer et al. (2004) | BMC Health Services Research | Reliability of physician-assessed patient quality of care | USA | N = 496 physician reviews | Veterans' Medical Records | L1: Quality of Care scores L2a: Patient Records L2b: Physician Reviewers |
| Kendler, Ohlsson, Sundquist, and Sundquist (2015) | Social Psychiatry and Psychiatric Epidemiology | Drug abuse | Sweden | N = 1,089,940 |
Primary Health Care Register, the Total Population Register, the Swedish Hospital Discharge Register, and the Multi-Generation Register | L1: Individuals L2a: Households L2b: Districts |
| Langford and Bentham (1996) | Social Science & Medicine | Age standardized mortality ratio (SMR) | England and Wales | Not Reported | Unspecified nationally-representative data (1989–1991) | L1: Districts L2a: Regions L2b: ACORN Sociodemographic Category |
| Milliren, Richmond, Evans, Dunn, and Johnson (2017) | Substance Abuse: Research and Treatment | Marijuana Use | USA | N = 18,329 | Longitudinal Study of Adolescent to Adult Health (Add Health) | L1: Individuals L2a: Schools L2b: Neighborhoods |
| Moore et al. (2013) | Journal of Epidemiology and Community Health | Body mass index (BMI); Waist circumference | USA | N = 1503 | Multi-Ethnic Study of Atherosclerosis | L1: Individuals L2a: Workplace Environments L2b: Neighborhoods |
| Muntaner et al. (2004) | International Journal of Occupational and Environmental Health | Depression | USA | N = 473 | Primary Data Collection | L1: Individuals L2a: Nursing Home Workplaces L2b: County of Residence |
| Muntaner et al., 2006 | Health & Place | Depressive symptoms | USA | N = 241 | Primary Data Collection | L1: Observation Occasion L2a: Nursing Assistants L2b: Nursing Home Workplaces L3: County of Residence |
| Muntaner, Li, Xue, Thompson, Chung, et al. (2006) | Social Science & Medicine | Depressive symptoms | USA | N = 341 | Primary Data Collection | L1: Observation Occasion L2a: Nursing Assistants L2b: Nursing Home Workplaces L3: County of Residence |
| Muntaner, Li, Ng, Benach, and Chung (2011) | International Journal of Health Services | Self-reported health; Activity limitations; Alcohol use; Caffeine consumption | USA | N = 868 | Primary Data Collection | L1: Observation Occasion L2a: Nursing Assistants L2b: County of Residence |
| Pedan, Varasteh, and Schneeweiss (2007) | Journal of Managed Care Pharmacy | Adherence to statins | USA | N = 6436 | Blinded Computerized Pharmacy Prescription Records | L1: Individuals L2a: Physicians L2b: Pharmacies |
| Pedersen (2017) | Journal of Youth and Adolescence | Alcohol use; Heavy episodic drinking | Norway | N = 10,038 | Young in Oslo Study | L1: Individuals L2a: Schools L2b: Neighborhoods |
| Penfold, Deena, Benedict, and Kelleher (2008) | International Journal of Health Geographics | Risk of perforated appendicitis | USA | N = 8086 | Ohio Hospital Association | L1: Individuals L2a: Zip Code of Residence L2b: Hospitals |
| Pilbery, Teare, Goodacre, and Morris (2016) | Emergency Medicine Journal | Correct reading of an ECG | UK | N = 254 | Recognition of STEMI (ST-segment elevation myocardial infarction) by Paramedics and the Effect of Computer Interpretation Feasibility Study | L1: Observation Occasion L2a: Individuals L2b: ECG Machines |
| Pruitt et al. (2014) | Cancer Epidemiology, Biomarkers & Prevention | Colorectal cancer screening | USA | N = 3898 | John Peter Smith Health System | L1: Individuals L2a: Primary Care Physicians L2b: Clinics L2c: Neighborhoods |
| Ratnapradipa et al. (2017) | Diseases of the Colon & Rectum | Laparoscopic colon cancer resection | USA | N = 10,618 | National Cancer Institute's Surveillance, Epidemiology, and End Results database; Medicare claims Data (2008–2011); 2010 US Census; 2008–2012 American Community Survey | L1: Individuals L2a: Hospitals L2b: Counties |
| Richmond, Dunn, Milliren, Evans, and Subramanian (2016) | Obesity | Body mass index (BMI) | USA | N = 18,200 | National Longitudinal Study of Adolescent to Adult Health (Add Health) | L1: Individuals L2a: Schools L2b: Neighborhoods |
| Riva, Gauvin, Apparicio, and Brodeur (2009) | Social Science & Medicine | Physical activity | Canada | N = 2716 | Unnamed larger study in Montreal | L1: Individuals L2a: Census Tracts L2b: Active Living Potential Walkability Zones |
| Schootman et al. (2014) | Annals of Surgical Oncology | Colorectal surgery outcomes | USA | N = 35,946 | 2000–2005 National Cancer Institute's Surveillance, Epidemiology and End Results; 1999–2005 Medicare Claims | L1: Individuals L2a: Hospitals L2b: Census Tracts |
| Teitler and Weiss (2000) | Sociology of Education | Sexual activity | USA | N = 2080 | Philadelphia Teen Survey 1993 Wave | L1: Individuals L2a: Schools L2b: Neighborhoods |
| Thomas, Rahman, Mor, and Intrator (2014) | American Journal of Managed Care | Rehospitalization | USA | N = 1,382,477 |
Medicare Claims and Enrollment Records; Minimum Data Set; Online Survey Certification and Reporting Dataset; Hospital Compare; American Hospital Association Database | L1: Patients L2a: Hospitals L2b: Nursing Home |
| Townsend (2012) | International Journal of Obesity | Body mass index (BMI); Waist circumference | England | N = 788,525 |
National Child Measurement Program | L1: Individuals L2a: Schools L2b: Neighborhoods |
| Tsugawa (2018) | Dissertation | Health care spending | USA | N = 434,616 |
Medicare Beneficiaries | L1: Hospitalizations L2a: Hospitals L2b: Physicians |
| Utter (2011) | American Journal of Public Health | Physical activity | New Zealand | N = 9107 | Youth 2007 Health Survey | L1: Individuals L2a: Schools L2b: Neighborhoods |
| Virtanen et al. (2010) | American Journal of Epidemiology | Long-term sick leave | Finland | N = 3063 | Finnish 10-Town Study | L1: Individuals L2a: Communities L2b: School Workplaces |
| Weich et al. (2017) | The Lancet Psychiatry | Rates of compulsory admission to inpatient psychiatric beds | England | N = 1,238,188 |
2010–11 Mental Health Minimum Data Set (MHMDS) | L1: Patients L2a: Hospitals L2b: Neighborhoods |
| West, Sweeting, and Leyland (2004) | Research Papers in Education | Drinking; Smoking; Illicit drug use; Unhealthy eating | Scotland | N = 2000+ | West of Scotland 11 to 16 Study | L1: Individuals L2a: Schools L2b: Neighborhoods |
| Wilk et al. (2018) | SSM - Population Health | Physical activity | England | N = 1517 | Grade 5 ACT-i-Pass | L1: Individuals L2a: Schools L2b: Neighborhoods |
| Williams et al., 2016 | PLoS ONE | Body mass index (BMI) | USA | N = 16,956 | National Child Measurement Program | L1: Individuals L2a: Residential Neighborhoods L2b: School Neighborhoods |
|
Young (2010) |
International Journal of Health Geographics |
Birth weight |
USA |
N = 1449 |
Cape Cod Family Healthy Study |
L1: Individuals L2a: Communities L2b: Families |
|
Reason for Use of CCMM: Account for Data Structure | ||||||
| Aerenhouts, Clarys, Taeymans, and Cauwenberg (2015) | PLoS ONE | Body fat percentage | Belgium | N = 69 | Primary Data Collection | L1: Observation Occasions L2a: Individuals L2b: Measurement Instruments |
| Ali et al. (2007) | Health & Place | Vaccine uptake | Vietnam | N = 56,076 | Diseases of the Most Impoverished program | L1: Individuals L2a: Schools L2b: Neighborhoods |
| Atkin, Sharp, Harrison, Brage, and Van Sluijs (2016) | Medicine and Science in Sports and Exercise | Physical activity | UK | N = 704 | Millennium Cohort Study | L1: Observation Occasions L2a: Individuals L2b: Seasons |
| Atkin, Sharp, et al. (2016) | PLoS ONE | Sedentary Behavior | UK | N = 264 | Sport, Physical Activity, and Eating Behavior: Environmental Determinants in Young People (SPEEDY study) | L1: Individuals L2a: Primary Schools L2b: Secondary Schools |
| Becker et al. (2016) | Journal of Hand Surgery | Classification of severity of trapeziometacarpal (TMC) arthrosis | Global | N = 92 | Science of Variation Group 8, 2014-5 | L1: Observation Occasion L2a: Patients' Radiographs L2b: Hand Surgeons |
| Block, Christakis, O'Malley, and Subramanian (2011) | Qual Quant | Body mass index (BMI) | USA | N = 3113 | Framingham Heart Study (Offspring Cohort) | L1: Observation Occasion L2a: Individuals L2b: Neighborhoods |
| De Meester, Van Dyck, De Bourdeaudhuij, Deforche, and Cardon (2014) | BMC Public Health | Physical activity | Belgium | N = 736 | Primary Data Collection | L1: Individuals L2a: Primary Schools L2b: Secondary Schools |
| D'Haese, Dyck, Bourdeaudhuij, Deforche, and Cardon (2014) | International Journal of Behavioral Nutrition and Physical Activity | Physical activity | Belgium | N = 606 | Belgian Environmental Physical Activity Study (BEPAS-child) | L1: Individuals L2a: Schools L2b: Neighborhoods |
| D'Haese et al. (2016) | International Journal of Behavioral Nutrition and Physical Activity | Physical activity | Belgium | N = 494 | Belgian Environmental Physical Activity Study (BEPAS-child) | L1: Individuals L2a: Schools L2b: Neighborhoods |
| Doumouras et al. (2017) | British Journal of Surgery | Non-technical skills of surgeons and anesthetists | USA | N = 26 | Primary Data Collection | L1: Individuals L2a: Simulation Raters L2b: Training Simulation |
| Hooiveld et al. (2016) | Environmental Health | Morbidity | Netherlands | N = 197,096 |
Dutch Agricultural Geographic Information System & electronic medical record data registered by Dutch general practitioners | L1: Individuals L2a: General Practitioner Practices L2b: Neighborhoods |
| Kirby (2008) | Social Forces | Access to health care | USA | N = 22,682 | Medical Expenditure Panel Survey (MEPS); U.S. Census; Health Resources and Services Administration | L1: Individuals L2a: Census Block Groups L2b: Primary Care Service Areas |
| Li et al. (2015) | Academic Emergency Medicine | Length of stay in emergency department | Australia | N = 27,656 | Linked Emergency Department-Laboratory Information Systems database | L1: Individuals L2a: Emergency Departments L2b: Years |
| Linton, Jennings, Latkin, Kirk, and Mehta (2014) | Health & Place | Injection drug use | USA | N = 1510 | AIDS Linked to the Intravenous Study (ALIVE) | L1: Individuals L2a: Neighborhoods at Time 1 L2b: Neighborhoods at Time 2 |
| Meunier, Bisceglia, and Jenkins (2012) | Developmental Psychology | Children's oppositional and emotional problems | Canada | N = 809 | Primary Data Collection | Not reported |
| Schofield, Das-Munshi, Mathur, Congdon, and Hull (2016) | Psychological Medicine | Depression | UK | N = 410,541 |
General Practitioner Patient Health Records from four ethnically diverse London boroughs: Lambeth, Hackney, Tower Hamlets and Newham | L1: Individuals L2a: Neighborhoods L2b: General Practitioner Practices |
| Sharp, Denney, and Kimbro (2015) | Social Science & Medicine | Self-rated health | USA | N = 1147 | Los Angeles Family and Neighborhood Survey (LAFANS) | L1: Observation Occasion L2a: Individuals L2b: Neighborhoods |
| Sink, Hope, and Hagadorn (2011) | Archives of Disease in Childhood - Fetal and Neonatal Edition | Oxygen saturation target achievement | USA | N = 1019 | Quality Improvement Oximeter Data and Neonatal Intensive Care Unit Nurse Administrative Data and Bedside Patient Flowsheets | L1: Monitoring Period L2a: Infants L2b: Nurses |
| Vigil et al. (2017) | Pain | Pain intensity & emergency room prioritization | USA | N = 129,991 |
Veterans' Health Administration Corporate Data Warehouse | Not reported |
|
Winpenny et al. (2017) |
Appetite |
Dietary intake |
UK |
N = 351 |
Sport, Physical Activity and Eating behavior: Environmental Determinants in Young People |
L1: Individuals L2a: Primary Schools L2b: Secondary Schools |
|
Reason for Use of CCMM: Contexts Over Time | ||||||
| Gustafsson et al. (2017) | Health & Place | Functional somatic symptoms | Sweden | N = 920 | Northern Swedish Cohort Study | L1: Individuals L2a: Neighborhoods at 1981 L2b: Neighborhoods at 1986 L2c: Neighborhoods at 1995 L2d: Neighborhoods at 2007 |
| Huijts and Kraaykamp (2012) | International Migration Review | Self-rated health | 31 European Countries | N = 19,210 | European Social Surveys (2002–2008) | L1: Individuals L2a: Country of Origin L2b: Country of Destination L2c: Immigrant Community |
| Leyland and Naess (2009) | Journal of the Royal Statistical Society: Series A | Mortality | Norway | N = 49,736 | Oslo Census Information from 1960, 1970, 1980 and 1991 | L1: Individuals L2a: Area in 1960 L2b: Area in 1970 L2c: Area in 1980 L2d: Area in 1990 |
| Morton et al. (2016) | International Journal of Behavioral Nutrition and Physical Activity | Physical activity | England | N = 325 | Sport, Physical Activity, and Eating Behavior: Environmental Determinants in Young People | L1: Individuals L2a: Primary Schools L2b: Secondary Schools |
| Murray et al. (2013) | American Journal of Epidemiology | Physical capability (chair rise, grip strength, balance) | England | N = 2566 | National Survey of Health and Development | L1: Individuals L2a: Residential Area (age 4) L2b: Residential Area (age 26) L2c: Residential Area (age 53) |
| Ohlsson and Merlo (2011) | Social Science & Medicine | All-cause mortality; Ischemic heart disease mortality and morbidity; Cancer mortality and morbidity; Respiratory diseases and related mortality | Sweden | Not reported | National Registers | L1: Individuals L2a: Parish of Residence in 1969 L2b: Parish of Residence in 1979 L2c: Parish of Residence in 1989 L2d: Parish of Residence in 1999 |
| Urquia et al. (2009) | American Journal of Public Health | Birth weight | Canada | N = 22,189 | Canadian Institute for Health Information (1993–2000) | L1: Individuals L2a: Census Tracts L2b: Country of Origin |
| Urquia, Frank, and Glazier (2010) | Social Science & Medicine | Birth weight | Canada | N = 320,398 |
Discharge Abstract Database of the Canadian Institute for Health Information | L1: Infants L2a: Migrant Mother's Country of Birth L2b: Migrant Mother's Country of Last Permanent Residence |
| Urquia, Frank, Moineddin, and Glazier (2011) | Journal of Urban Health | Preterm birth | Canada | N = 397,470 |
Discharge Abstract Database of the Canadian Institute for Health Information | L1: Births L2a: Neighborhoods L2b: Maternal Country of Origin |
|
Zaccarin and Rivellini (2002) |
Statistical Methods & Applications |
Decision to have second child |
Italy |
N = 1092 |
World Fertility Survey Project of the International Statistical Institute and Fertility and Family Survey Project of the European Economic Commission |
L1: Individuals L2a: Birth Place L2b: Current Residence |
|
Reason for Use of CCMM: Innovative Applications | ||||||
| Bell, 2014b | Social Science & Medicine | Mental Health | UK | N = 21,142 | British Household Panel Survey, 1991–2009 | L1: Observation Occasion L2a: Household Year L2b: Period L2c: Individual L3a: Cohorts L3b: Local Authority District |
| Congdon and Best (2000) | Applied Statistics | Emergency in-patient admissions | UK | N = 335 ward-practice catchment zones | Hospital records from Barking and Havering Health Authority (UK); unspecified ward-level data | L1: Hospital Admissions L2a: Ward-Practice Catchment Zones L2b: Primary Care Practices L2c: Hospitals |
| Evans et al. (2016) | Social Science & Medicine | Body mass index (BMI) | USA | N = 14,144 | National Longitudinal Study of Adolescent to Adult Health (Add Health) | L1: Individuals L2a: Social Network Communities L2b: Schools L2c: Neighborhoods |
| Fischbach et al. (2002) | International Journal of Epidemiology | Helicobacter pylori treatment success | Global | N = 618 treatment groups | Meta-analysis of studies examining treatment regimens to eliminate H. pylori from human subjects | L1: Treatment Groups L2a: Studies L2b: Treatment Regimens |
Sample size unit is human respondents, unless otherwise noted.
Bell, 2014 is classified as an Innovative Methods paper and so is included in Table 1. However it is also an APC paper.
Table 2.
Summary of empirical health studies examining Age-Period-Cohort (APC) effects.
| Authors | Journal | Outcome | Country | Data Source | Did the Authors Address the Controversies over APC Models, particularly those raised by Bell and Jones (2014)? |
|---|---|---|---|---|---|
| Ananth, Keyes, and Wapner (2013) | BMJ | Pre-eclampsia | USA | US Centers for Disease Control and Prevention National Hospital Discharge Survey Data | NO: published before Bell and Jones (2014). Did acknowledge the identification problem and used two approaches. CCMM was a robustness check on the first approach. |
| Bardo 2015a | Dissertation | Self-rated health | USA | General Social Survey | NO: published after Bell and Jones (2014) but does not cite them; does discuss the identification problem but claims CCMM addresses the issue. |
| Beck, Finch, Lin, Hummer, and Masters (2014) | Social Science & Medicine | Self-rated health | USA | National Health Interview Survey | NO: published concurrently with the Bell and Jones (2014). |
| Bell and Jones (2018) | Qual Quant | Body mass index (BMI) | USA | National Health Interview Survey | YES: this is a paper in the dialogue between the two factions and uses the approach only to illustrate issues of concern. |
| Chaurasiya (2018) | Asian Journal of Epidemiology | Non-communicable disease | India | National Sample Survey (NSS) in India | NO: published after Bell and Jones (2014) but does not cite them; also does not mention the identification problem. |
| Delaruelle, Buffel, and Bracke (2015) | Social Science & Medicine | 32 European countries | European Social Survey | YES: mentions the identification problem and cites Bell and Jones (2014); attempts to address the issue through theory-informed sensitivity analyses. | |
| Fu and Land (2015) | Population Research and Policy Review | Overweight; Obesity | China | China Health and Nutrition Survey | YES: acknowledges the controversy and cites Bell and Jones (2014); attempts to address the issue through sensitivity analyses. |
| Giordano et al. (2014) | Drug and Alcohol Dependence | Hospitalization for drug abuse | Sweden | National Swedish Hospital Discharge Register | NO: published concurrently with the Bell and Jones (2014). |
| Hidehiro, Ken, Yoko, Shizuko, and Masaya (2016) | Population Health Metrics | Self-rated health | Japan | Comprehensive Survey of Living Conditions | NO: published after Bell and Jones (2014) but does not cite them; does discuss the identification problem but claims CCMM addresses the issue. |
| Keyes, Gary, O'Malley, Hamilton, and Schulenberg (2019) | Social Psychiatry & Psychiatric Epidemiology | Depressive symptoms | USA | Monitoring the Future | NO: published after Bell and Jones (2014) but does not cite them; also does not mention the identification problem. |
| Kraus et al. (2015) | Alcohol and Alcoholism | Alcohol use | Sweden | 1979 Scandinavian Drinking Survey (SDS-79), the 1995 Nordic Survey of Alcohol and Narcotics (NSAN-95), the 2003 Alcohol and Narcotics Survey (ANS-03) and the 2005, 2007, 2009 and 2011 Swedish Alcohol Monitoring Survey (AMS-05/11) | NO: published after Bell and Jones (2014) but does not cite them; does discuss the identification problem but claims CCMM addresses the issue. |
| Krieger et al. (2014) | Epidemiology | Mortality | USA | National Center fro Health Statistics Mortality Data, and US Census Data | NO: published concurrently with the Bell and Jones (2014). |
| Kwon and Schafer (2016) | SSM -Population Health | Self-rated health | China | World Value Survey-China | YES: acknowledges the controversy and cites Bell and Jones (2014); attempts to address the issue through sensitivity analyses. |
| Lin, Beck, and Finch (2014) | Journals of Gerontology, Series B: Psychological Sciences and Social Sciences | Disability | USA | National Health Interview Survey | NO: published concurrently with the Bell and Jones (2014). |
| Lin, Beck, and Finch (2016) | Disability and Health Journal | Disability | USA | National Health and Nutrition Examination Survey (NHANES) | NO: published after Bell and Jones (2014) but does not cite them; does discuss the identification problem but claims CCMM addresses the issue. |
| Livingston et al. (2016) | Addiction | Alcohol use | Australia | Australian National Drug Strategy Household Survey (NDSHS) | YES: cite the Bell and Jones paper; argue that linear effects are less likely to be an issue in this case (based on supplemental analyses). |
| Luo, Pan, Sloan, Feinglos, and Wu (2015) | Preventing Chronic Disease | Tooth loss | USA | National Health and Nutrition Examination Survey (NHANES) | NO: published after Bell and Jones (2014) but does not cite them; does discuss the identification problem but claims CCMM addresses the issue. |
| Masters (2012) | Demography | Mortality | USA | National Health Interview Survey-Linked Mortality Files | NO: published prior to controversy. |
| Masters, Hummer, and Powers (2012) | American Sociological Review | Mortality | USA | National Health Interview Survey-Linked Mortality Files | NO: published prior to controversy. |
| Masters et al. (2013) | American Journal of Public Health | Mortality | USA | National Health Interview Survey-Linked Mortality Files | NO: published prior to controversy. |
| Piontek, Kraus, Müller, and Pabst (2010) | Sucht: Zeitschrift für Wissenschaft und Praxis | Cigarette use prevalence and frequency | Germany | German Epidemiological Survey of Substance Abuse | NO: published prior to controversy. |
| Piontek, Kraus, Pabst, and Legleye (2012) | Journal of Epidemiology & Community Health | Cannabis use prevalence and frequency | Germany | German Epidemiological Survey of Substance Abuse | NO: published prior to controversy. |
| Reither, Hauser, and Yang (2009) | Social Science & Medicine | Body mass index (BMI) | USA | National Health Interview Survey | NO: published prior to controversy. |
| Ryan-Ibarra et al. (2016) | Annals of Epidemiology | Lifetime asthma diagnosis | USA | California Behavioral Risk Factor Surveillance System | NO: published after Bell and Jones (2014) but does not cite them; also does not mention the identification problem. |
| Sugisawa et al. (2016) | International Journal of Nephrology & Renovascular Disease | Dialysis complications and depressive symptoms in dialysis patients | USA | Original Data Collected | NO: published after Bell and Jones (2014) but does not cite them; also does not mention the identification problem. |
| Tang (2014) | Social Indicators Research | Subjective well-being | China | World Values Survey | NO: published concurrently with the Bell and Jones (2014). |
| Teisl, Lando, Levy, and Noblet (2016) | Food Control | In-home food preparation safety | USA | The Food Safety Survey | NO: published after Bell and Jones (2014) but does not cite them; also does not mention the identification problem. |
| Thibodeau (2015) | Population Review | Suicide mortality | Canada | Statistics Canada | YES: acknowledged as a limitation. |
| Thorpe et al. (2016) | Journal of Urban Health | Hypertension; Diabetes; Stroke; Cardiovascular Disease | USA | National Health Interview Survey | NO: published after Bell and Jones (2014) but does not cite them; also does not mention the identification problem. |
| Twenge, Sherman, and Wells (2017) | Archives of Sexual Behavior | Number of sexual partners since age 18 | USA | General Social Survey | NO: published after Bell and Jones (2014) but does not cite them; also does not mention the identification problem. |
| Volken, Wieber, Ruesch, Huber, and Crawford (2017) | Public Health | Self-rated health | Switzerland | Swiss Health Survey (1997, 2002, 2007 and 2012) | YES: acknowledges the controversy and referenced Bell and Jones (2014) book chapter which suggested modifications to the HAPC approach and strong assumptions that would enable the analysis to be conducted. |
| Wilk, Maltby, and Cooke (2017) | Canadian Studies in Population | Body mass index (BMI) | Canada | Canadian Community Health Survey (CCHS) | NO: published after Bell and Jones (2014) but does not cite them; does discuss the identification problem but claims CCMM addresses the issue. |
| Willson and Abbott (2018) | Australian and New Zealand Journal of Public Health | Body mass index (BMI) | New Zealand | New Zealand National Health Surveys | NO: published after Bell and Jones (2014) but does not cite them; also does not mention the identification problem. |
| Yu et al. (2016) | BMJ Open | Disability | Hong Kong | Hong Kong Elderly Health Centers (EHCs) of the Department of Health | NO: published after Bell and Jones (2014) but does not cite them; does discuss the identification problem but claims CCMM addresses the issue. |
| Zhang (2017) | Journal of Religion and Health | Self-rated health | USA | General Social Survey | NO: published after Bell and Jones (2014) but does not cite them; does discuss the identification problem but claims CCMM addresses the issue. |
| Zheng, Yang, and Land (2011) | American Sociological Review | Self-rated health | USA | National Health Interview Survey | NO: published prior to controversy. |
| Zheng et al. 2016b | Population Research and Policy Review | Mortality | Australia, Belgium, Denmark, England and Wales, Finland, France, Iceland, Italy, Japan, Netherlands, New Zealand, Norway, Sweden, Switzerland, and U.S.A. |
Human Mortality Database | NO: published after Bell and Jones (2014) but does not cite them; also does not mention the identification problem. |
Bardo, 2015 is a dissertation that includes a variety of analyses. Bardo examined “domain satisfaction” (which is related to subjective well being but focuses on specific domains, including satisfaction with residence, hobbies, family, friends and health. Because health was examined we included this in our review even though it is not exclusively focused on health). In Chapter 3 these outcomes are treated separately, including a CCMM specifically for the health satisfaction outcome. This is the main model we reviewed.
Zheng, Yang, & Land, 2016 (Popul Res Policy Rev) conduct an atypical APC analysis where level 1 units are mortality rates in groups rather than outcomes for individual respondents.
3.2. Increasing but limited use of CCMM, and patterns in the literature
As shown in Fig. 4, heath researchers have increasingly adopted CCMM in empirical studies. Since the publication of the seminal CCMM paper in 1994 by Goldstein, a total of 118 empirical health articles had been published by the time of our scoping review. Most papers (n = 71; 60%) were published since 2014.
Fig. 4.
CCMM Empirical Health Publications by Year*. The main review was conducted through Feb 1, 2018, however several additional APC papers were identified in the APC secondary literature search after this date, including one study from 2019.
The 118 papers came from 54 different journals and a range of health sub-disciplines: medicine, public health, and the social sciences. A large variety of data sources were used, from large nationally-representative cohort studies to smaller data sets collected to answer specific research questions. The countries in which the data were collected largely represent the global north, especially English-speaking nations, which likely reflects both our inclusion criteria of English-language articles, and data availability within these countries.
Across reviewed studies, the language used to describe data structures was highly non-standardized. For example, some authors would describe the data structure represented in Fig. 2, with children nested in schools and cross-classified by neighborhoods, as a two-level model, while others would describe this as a three-level model. These inconsistencies in description became particularly challenging when data structures were especially complex. There were also considerable inconsistencies in reporting of other vital information, such as sample sizes for each level of analysis.
3.3. CCMM used across multiple health domains
The 118 studies covered topics that fell into 17 health domains, as presented in Table 3. The most-often examined health outcome in CCMM studies is body weight (n = 14), using measures of body mass index (BMI) and waist circumference. The next most-often examined health outcomes were self-rated individual health or subjective wellbeing (‘general health’) (n = 12) and substance use (n = 11). As an example of a general health study, Aminzadeh et al. (2013) used CCMM to examine the relationship between neighborhood social capital and adolescent subjective wellbeing, as measured by questions on general mood, life satisfaction and the WHO-5 Wellbeing Index. Mental health (n = 10) was the next most examined health outcome. These four domains comprised 40% of the total studies included in the review. Other health domains covered by CCMM studies include: physical activity (n = 9); medical services (n = 9); medical care quality (n = 9); mortality (n = 8); morbidity and disease outcomes (n = 8); sexual and reproductive health (n = 5); infant health (n = 5); physical capability (n = 4); pregnancy or other reproductive health (n = 3); adherence to treatment (n = 3); sexual activity (n = 2); diet (n = 1); a combination of these topics (n = 5); and other topics (n = 5).
Table 3.
Type of health outcome evaluated by reviewed studies.
| Outcome Type | Frequency | Percent |
|---|---|---|
| Body Weight | 14 | 11.9 |
| General Health/Self-rated Health | 12 | 10.2 |
| Substance Use | 11 | 9.3 |
| Mental Health | 10 | 8.5 |
| Physical Activity | 9 | 7.6 |
| Medical Services | 9 | 7.6 |
| Medical Care Quality | 9 | 7.6 |
| Mortality | 8 | 6.8 |
| Morbidity & Specific Disease Outcomes | 8 | 6.8 |
| Sexual and Reproductive Health | 5 | 4.2 |
| Infant Health | 5 | 4.2 |
| Other | 5 | 4.2 |
| Combinations of Other Categories | 5 | 4.2 |
| Physical Capability | 4 | 3.4 |
| Adherence to Treatment | 3 | 2.5 |
| Diet |
1 |
0.8 |
| Total | 118 | 100 |
Common levels of analysis included in these studies include individuals (e.g., patients, survey respondents, students), institutions (e.g., schools, hospitals), area (e.g., neighborhood, district), and time (measurement occasion or cohort).
3.4. Five rationales for use of CCMM
Across all 118 studies included in the review, cross-classified multilevel modeling was correctly chosen as an analytic technique to handle clustering or grouping in non-hierarchical data. The research questions asked by investigators using clustered data did, however, vary in five key ways. These reflect different rationales for and uses of CCMM in empirical health research, as outlined below. We note that researchers may have multiple research questions in each study and therefore may use CCMM for multiple reasons. We chose to categorize the studies by their primary reason for use of CCMM, as shown in Table 3.
3.4.1. Examining concurrent contextual effects
Some authors had substantive interest in the clustering within the data, and as such, an examination of contextual effects was a key aim of the study. As shown in Fig. 5, this was the most common reason for use of CCMM (40%) (i.e., to assess the contributions that concurrent contexts (e.g., schools and neighborhoods) have on individual-level health outcomes). For example, Di Martino et al. (2016) used CCMM to assess the extent to which variation in patient treatment adherence (Level 1) after myocardial infarction was attributable to hospitals (Level 2a) or primary care providers (Level 2 b). In studies such as these, results from the random effects, or variance components, of the CCMM are of primary consideration.
Fig. 5.
Uses of CCMM in empirical health literature.
3.4.2. Accounting for non-independence in the data structure
Other authors had no substantive interest in the ways in which observations were related to each other, but used CCMM to account for data structure, namely the non-independence of data values. In these instances, the authors chose CCMM as a way to adjust standard errors to account for clustering. Nearly a fifth (17%) of CCMM studies use the technique to account for clustering in the data structure without a particular focus on the random effect estimates. For instance, Ali et al. (2007) examined vaccine uptake among students in Vietnam. The authors accounted for cross-classification of individuals (Level 1) within both schools (Level 2a) and neighborhoods (Level 2b) to address the data's non-hierarchal structure and to account for the potential variation in vaccine uptake by school and neighborhood. Previous research indicates that ignoring one of these levels does not drastically affect fixed-effect point estimates, but importantly, could cause standard errors to be underestimated (Fielding, 2002; Raudenbush & Bryk, 2002). This impacts the statistical significance inferences associated with the fixed-effect parameter estimates and may lead to increased Type I error (Meyers & Beretvas, 2006). However, as opposed to reporting results from the variance components of the models, many authors included only fixed-effects coefficients from the independent variables included in models. In this sense, authors employing CCMM to account for non-independence in the data structure seek to account for contextual effects rather than to explore them substantively.
3.4.3. Examining contextual effects over time
CCMM are also used to examine longitudinal relationships that vary across time or by measurement occasion, including in studies adopting a life course perspective. We define life course studies as those in which the predictor variable was measured at multiple points in time (e.g., socioeconomic status measured in childhood, adolescence, adulthood). Longitudinal studies are those in which the outcome was measured at multiple occasions. In longitudinal studies with strict hierarchical levels, observation occasions (Level 1) are nested cleanly within individuals (Level 2). However, this strict hierarchical structure is not always present in the data. For example, in a Swedish study by Gustafsson, Bozorgmehr, Hammarstrom, and San Sebastian (2017), individuals were assessed in 1981, 1986, 1995, and 2007, with some respondents residing in different neighborhoods at each time point. Given individuals were not nested in the same neighborhood at each of the four time points, CCMM were necessary to accurately model the cross-classified data structure.
3.4.4. Age-period-cohort models
Age-Period-Cohort analyses are the second-most popular use for CCMM (31%). Generally, APC analyses attempt to disentangle the contributions of the age of individuals, the period of time they are surveyed in, and their birth cohort to explain individual-level outcomes. In CCMM APC models, individuals (Level 1) are nested in periods (Level 2a) cross-classified by cohorts (Level 2 b), and age is treated as a level 1 fixed effect. For instance, in a Chinese age-period-cohort model fit by Tang (2013), respondents were surveyed in four time periods: 1990, 1995, 2001, and 2007. Tang defined seven cohorts: Children of Old China (born 1908–1938), Children of New China (born 1939–1946), the “Lost” Generation (1947–1955), Children of the Early Cultural Revolution (1956–1960), Children of the Late Cultural Revolution (1961–1966), Children of Economic Reform (1967–1976), and Children of Opening-Up (born 1977 and later). Individuals were then cross-classified according to which cohort they belonged to and what time (or period) they were surveyed in. Their age at the time of the survey was included in the model as an individual-level fixed effect.
For decades, a notorious problem in the APC literature has been the “identification problem” (e.g., Fienberg & Mason, 1979; Glenn, 1976), whereby an exact linear dependency exists between the three measures of temporal effects: Period = Age + Cohort. Yang proposed CCMM as a solution to this issue because the model setup would break the dependency between the three factors by treating two as random effects and one as a fixed effect. However, critiques of Yang and Land's (2006) claim soon emerged, beginning notably with a critique by Bell and Jones (2014). A long exchange has now occurred in the literature between proponents and opponents of the CCMM approach (see Bell & Jones, 2018 for a succinct summary). Briefly, opponents of the CCMM approach show that results can vary strongly as an artefact of how the data were collected; when there is a large ratio of cohorts to periods, or vice versa, random effects can vary dramatically in favor of one or the other (Bell & Jones, 2018). Thus, study findings may not be attributable to substantive APC processes, but rather to the way in which the data were collected (Bell & Jones, 2018).
Results from this review indicate that, of 37 CCMM APC studies captured in our review, 24 were published after the 2014 critique by Bell and Jones (see Fig. 6).
Fig. 6.
Age-Period Cohort CCMM Studies in the Empirical Health Literature by Year. * The main review was conducted through Feb 1, 2018, however several additional APC papers were identified in the APC secondary literature search after this date, including one study from 2019.
Of the 24 CCMM studies published after the critique by Bell and Jones, only 7 (29%) acknowledged the controversy, and one of these was a follow-up paper by Bell and Jones (2018). Studies that do acknowledge the controversy often do not do so satisfactorily. We find, for example, that they may reference this substantive methodological debate only within the limitations section of the manuscript rather than meaningfully describing the ways in which findings could be affected within the methods or discussion sections. Of the remaining 17 studies (74%), more than half (n = 9) failed to acknowledge the identification problem and the rest seemed to assume that CCMM would resolve the issue. This is concerning from a methodological perspective because it indicates both that CCMM has become very popular for APC analysis in the empirical health literature, and that most scholars are either unaware of the methodological debate or are not engaging with the debate in a thoughtful manner.
3.4.5. Innovative applications of CCMM
CCMM are often applied to novel research questions and most studies that use this statistical approach could be considered innovative. A small set of studies (3%) did, however, apply the method in unique or unusual ways. These highly innovative applications included combining CCMM with other modeling techniques, as in Congdon and Best (2000) who integrated elements of gravity models to represent flows of patients between area-practice combinations and hospital units into CCMM. Fischbach, Goodman, Feldman, and Aragaki (2002) applied cross-classified modeling in a meta-analysis of clinical trials, in which treatment groups (level 1) were cross-classified by study (Level 2) and treatment regimen (Level 2). Further information about each study that used CCMM in an innovative manner is provided in Table 1.
4. Discussion
Motivated by both theoretical and methodological concerns, health researchers have increasingly employed cross-classified multilevel modeling methods. These advanced statistical methods are highly flexible tools for modeling data with complex structures and are appropriate and advantageous for addressing a wide range of substantive and methodological issues. Additionally, the approach can allay concerns about omitted context bias (Goldstein, 1994; Meyers & Beretvas, 2006). Despite its many advantages and the fact that it has been nearly three decades since the approach was proposed, we found only 118 empirical health studies that used this approach.
The range of topics examined within these empirical CCMM studies is diverse, with some health outcomes examined to a greater extent than others. Of the 118 reviewed studies, the health topics most commonly examined were body weight, self-rated health and wellbeing, substance use, and mental health. Other health outcomes, such as treatment adherence and diet were the least-examined topics. Treatment adherence and diet are widely discussed in the health literature, but our findings highlight a paucity of research designed to understand the multiple and intersecting contexts that influence an individual's ability to adhere to medical treatment and select the foods they consume. The relatively limited use of CCMM in empirical health studies indicates a fruitful avenue for future research, and its increased application is possible in a number of statistical packages including: SAS (proc mixed) (Hox, 2010); SPSS (mixed) (IDRE, 2020); Stata (xtmixed) (Hox, 2010); R (lmer) (Bolker, 2020); and MLwiN (Leckie & Bell, 2013); among others. For researchers wishing to use CCMM, we further provide a number of recommendations and best practices to improve clarity and standardize reporting within CCMM studies.
4.1. Recommendations
4.1.1. Explicitly state rationale for use of CCMM and sample sizes at all levels
Authors should indicate whether their use of CCMM is “out of necessity” (i.e., to account for clustering in the data) or “out of substantive interest” (i.e., to examine variation explained in a health outcome by multiple and intersecting contexts), or both. This is, surprisingly, not always clear in some studies, particularly in brief descriptions provided in abstracts. Clarity on this issue will enable readers to more easily determine the purpose(s) of a study.
Similarly, information should be provided about the sample size at all levels (e.g., number of individuals, number of schools, number of neighborhoods) regardless of the stated rationale for use of CCMM. Sample size information was inconsistently reported, yet this information is vital to the evaluation of potential study limitations in multilevel models and CCMM (Dedrick, Ferron et al., 2009; McNeish & Stapleton, 2016; Milliren, Evans, Richmond, & Dunn, 2018).
4.1.2. Describe cross-classified data structure
Regardless of the rationale for use of CCMM, it is essential to clearly communicate the multilevel structure of the data and the model(s). Three main strategies may be used to communicate the data structure. At minimum, one of these three strategies should be used, however we recommend that authors consider using all three.
First, the use of figures such as unit and classification diagrams (shown in Fig. 1, XFig. 2) is an effective and efficient way to communicate data structures. For more complex data structures, such as three-level models where only two contexts are cross-classified, a diagram is the most appropriate tool for communicating model structure because even carefully worded textual descriptions may be unclear. For example, in the study by Bell (2014) the data structure was highly complex; the visualization used in the study was a clear and effective way to communicate the data structure.
Second, we recommend including a full equation in classification notation (Browne, Goldstein, & Rasbash, 2001; Fielding & Goldstein, 2006). Although CCMM equations can sometimes be quite complex, they accurately reflect the cross-classified nature of the data and efficiently document subtle modeling choices made by researchers. Please see Appendix A for an example for a CCMM equation using classification notation.
Finally, we encourage a clear description of the data and model structure within the text, noting both the clustering units and the level at which each cluster is nested. Variation in this practice exists and we therefore encourage standardization around the description provided by Goldstein (1994) in his original paper on CCMM. Goldstein referred to cross-classified contexts as residing at the same level (e.g., cross-classified at level 2), rather than as being separate levels. This helps to distinguish between strict hierarchical data structures found in traditional multilevel modeling and the less strict cross-classified hierarchies present in data structures used in CCMM. In the strict hierarchical data structure visualized in Fig. 1, three levels are present: students (Level 1) nested in schools (Level 2), which are in turn nested in neighborhoods (Level 3). In the case of cross-classified data structures, as in Fig. 2 where there are three distinct types of units, this should be considered a two-way cross-classification, with two units of analysis (schools and neighborhoods) both existing at Level 2 because they are each a single “step” away from the lowest unit of analysis (Level 1, individuals). In this instance, we would recommend describing the data structure using language similar to the following: individuals (Level 1) are nested within a two-way cross-classification of schools (Level 2a) by neighborhoods (Level 2b). In both the strict hierarchical and less-strict cross-classified data structures, the numeric value for higher levels (or clustering units) corresponds with the number of steps away from the lowest unit of analysis.
Descriptions such as these will greatly clarify for readers of CCMM manuscripts the cross-classified nature of the data used in analysis. We hasten to add that not all statistical software for CCMM analysis uses this naming convention suggested by Goldstein, perhaps due to the software's original development for use in traditional multilevel models with strict hierarchical data structures. Depending on the software used, researchers specifying a cross-classified multilevel model may need to code “Level 2b” of the cross-classified data as “Level 3.” This misalignment between the recommendations in the literature and the practical considerations of coding language is perhaps not surprising from a software development perspective, but may nonetheless have fueled some of the inconsistencies in the ways in which CCMM model descriptions are described in the literature.
4.1.3. Report variance estimates and other relevant summary statistics
All multilevel models, regardless of whether they are hierarchical or non-hierarchical, allow for a decomposition of the total variance across levels and clustering units. These variance components should be reported for all contextual levels when using CCMM, even if the primary reason for use of CCMM is to account for clustering in the data. The Intraclass Correlation Coefficient (ICC) (also termed Variance Partition Coefficients (VPC) in its most general form) measures the proportion of total variance in the outcome that is attributable to the area or contextual-level (i.e., the correlation between two observations within the same cluster) (Merlo, Chaix et al., 2006). For linear CCMM, this is calculated as VPC = VA/(VA + V1), where VA is the area level variance and V1 corresponds to the individual-level variance. As compared to linear models, in CCMM for binary and other discrete responses, there is no single ICC or VPC value as the level 1 variance is a function of the mean (Leckie & Charlton, 2013). A popular solution is to formulate the model in terms of a continuous latent response variable (i.e., the linear threshold model method) which underlies the observed binary response (Leckie & Charlton, 2013; Merlo et al., 2006). In this case, VPC is calculated as: .
In models with more than one area or contextual level unit of analysis, a separate VPC estimate is calculated for each clustering unit (e.g., one for classrooms, one for schools, one for neighborhoods). The VPC estimates for each area level included in a model should be reported in the manuscript, regardless of whether the area level was of substantive research interest to the investigators. In other words, even if CCMM was used only to account for clustering in the data structure, investigators using CCMM should report VPC estimates for each unit of analysis at the higher level(s).
4.1.4. Engage with the APC controversy
As discussed above, a substantial controversy has surrounded APC analysis in general and the use of CCMM for APC analysis in particular. Bell and Jones (2018) have done much to explicate the debate, the ‘identification problem,’ and the methodological concerns. Despite this, the vast majority of researchers continue to employ CCMM for APC analysis without reference to the identification problem, the controversy itself, or any of the latest recommendations for best practices. Those that do refer to the identification problem often note this only within the limitations section of the manuscript. In light of the ongoing debate surrounding these methods, however, we urge substantial caution when conducting APC analysis and recommend a more meaningful engagement with the logic underlying the controversy. If researchers decide to apply the CCMM approach to the “identification problem,” they should—at a minimum—engage seriously with this literature, specify how their data structure may influence their findings, and detail their reasons for believing that the analysis they are conducting yields unbiased estimates. Researchers are also encouraged to stay abreast of the controversy and to consult recently published recommendations that center on this topic (Bell, 2020).
4.2. Conclusion
Health and human behavior are shaped by multiple and intersecting social and physical contexts—contexts that rarely form perfect hierarchies. Cross-classified multilevel modeling allows researchers to model these complex realities. This statistical technique may be and is used to: account for complex data structures, answer research questions related to concurrent geographic and social contexts, and contexts over time, and to incorporate a hybrid of statistical applications within one model. Results from this review indicate that CCMM are used to examine a wide range of health topics and domains and that the use of CCMM in health research has expanded in recent years. Despite its increased use, this flexible approach remains relatively underutilized. This leaves much room for research investigations that employ this technique to more precisely model the complex causal architecture of individual health outcomes. Recommendations proposed in this review can improve clarity and standardization of CCMM studies that seek to comprehensively understand the causes of health and disease in human populations.
Ethics statement
This review article did not involve human subjects research. As such, this research did not require ethical approval from an Institutional Review Board.
Acknowledgements
The authors thank Grace Kennedy, Tatum Williamson, and Samantha Ernst for their assistance in conducting the literature review. We wish to thank the reference librarian Carol Mita of the Harvard University Countway Library of Medicine for her assistance in constructing the search parameters for this review of the literature. Dr. Dunn was supported in part by the National Institute of Mental Health of the National Institutes of Health under Award Numbers K01MH102403 and 1R01MH113930. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Appendix A. Equation in classification notation
The following equation uses notation for cross-classified multilevel models proposed by Fielding and Goldstein (2006). It represents a random intercepts cross-classified model predicting outcome (y) that nests individuals (Level 1, denoted as i) within a three-way cross-classification of context 1 (Level 2a, denoted as j1), by context 2 (Level 2 b, denoted as j2), and bycontext 3 (Level 2c, denoted as j3):
where:
is the outcome of individual i who is nested in cross-classified context at level 2a (j1), context at level 2 b (j2), and context level 2c (j3);
is the precision-weighted grand mean of the outcome across all three contexts, holding covariates constant;
is a vector of individual-level covariates and their associated parameter values;u0(j1) is the random effect parameter for context 2a-level variance (u0(j1) ~ N (0));
u0(j2) is the random effect parameter for context 2 b-level variance (u0(j2) ~ N (0));
u0(j3) is the random effect parameter for context 2c-level variance (u0(j3) ~ N (0));
is the random effect for the individual (e0i ~ N (0))
References
- Aerenhouts D., Clarys P., Taeymans J., Cauwenberg J.v. Estimating body composition in adolescent sprint athletes: Comparison of different methods in a 3 years longitudinal design. PLoS One. 2015;10(8) doi: 10.1371/journal.pone.0136788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aitkin M., Anderson D., Hinde J. Statistical modelling of data on teaching styles. Journal of the Royal Statistical Society: Series A. 1981;144(4):419–461. doi: 10.2307/2981826. [DOI] [Google Scholar]
- Ali M., Thiem V.D., Park J.K., Ochiai R.L., Canh D.G., Danovaro-Holliday M.C. Geographic analysis of vaccine uptake in a cluster-randomized controlled trial in Hue, Vietnam. Health & Place. 2007;13(3):577–587. doi: 10.1016/j.healthplace.2006.07.004. [DOI] [PubMed] [Google Scholar]
- Aminzadeh K., Denny S., Utter J., Milfont T.L., Ameratunga S., Teevale T. Neighbourhood social capital and adolescent self-reported wellbeing in New Zealand: A multilevel analysis. Social Science & Medicine. 2013;84:13–21. doi: 10.1016/j.socscimed.2013.02.012. [DOI] [PubMed] [Google Scholar]
- Ananth C.V., Keyes K.M., Wapner R.J. Pre-eclampsia rates in the United States, 1980-2010: age-period-cohort analysis. BMJ. 2013;347:f6564. doi: 10.1136/bmj.f6564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atkin A.J., Foley L., Corder K., Ekelund U., van Sluijs E.M.F. Determinants of three-year change in children's objectively measured sedentary time. PLoS One. 2016;11(12):1–13. doi: 10.1371/journal.pone.0167826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atkin A.J., Sharp S.J., Harrison F., Brage S., Van Sluijs E.M.F. Seasonal variation in children's physical activity and sedentary time. Medicine & Science in Sports & Exercise. 2016;48(3):449–456. doi: 10.1249/MSS.0000000000000786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bardo A.R. Miami University; 2015. Age-Period-Cohort trends in subjective well-being and happy life expectancy among those with and those without physical disability. Doctor of Philosophy. [Google Scholar]
- Becker S.J., Bruinsma W.E., Guitton T.G., van der Horst C.M., Strackee S.D., Ring D. Interobserver agreement of the eaton-glickel classification for trapeziometacarpal and scaphotrapezial arthrosis. J Hand Surg Am. 2016;41(4):532–540. doi: 10.1016/j.jhsa.2015.12.028. e531. [DOI] [PubMed] [Google Scholar]
- Beck A.N., Finch B.K., Lin S.-F., Hummer R.A., Masters R.K. Racial disparities in self-rated health: Trends, explanatory factors, and the changing role of socio-demographics. Social Science & Medicine. 2014;104:163–177. doi: 10.1016/j.socscimed.2013.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell A. Life-course and cohort trajectories of mental health in the UK, 1991-2008 - a multilevel age-period-cohort analysis. Social Science & Medicine. 2014;120:21–30. doi: 10.1016/j.socscimed.2014.09.008. [DOI] [PubMed] [Google Scholar]
- Bell A. Age Period Cohort analysis: A review of what we should and shouldn't do. Annals of Human Biology. 2020;47(2):208–217. doi: 10.1080/03014460.2019.1707872. [DOI] [PubMed] [Google Scholar]
- Bell A., Jones K. Another 'futile quest'? A simulation study of Yang and land's hierarchical age-period-cohort model. Demographic Research. 2014;30:333–360. doi: 10.4054/DemRes.2014.30.11. [DOI] [Google Scholar]
- Bell A., Jones K. The hierarchical age–period–cohort model: Why does it find the results that it finds? Quality and Quantity. 2018;52:783–799. doi: 10.1007/s11135-017-0488-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Block J.P., Christakis N.A., O'Malley A.J., Subramanian S.V. Proximity to food establishments and body mass index in the framingham heart study offspring cohort over 30 years. American Journal of Epidemiology. 2011;174(10):1108–1114. doi: 10.1093/aje/kwr244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolker B. lmer. RDocumentation. 2020. https://www.rdocumentation.org/packages/lme4/versions/1.1-23/topics/lmer Retrieved from.
- Bozorgmehr K., Maier W., Brenner H., Saum K.-U., Stock C., Miksch A. Social disparities in disease management programmes for coronary heart disease in Germany: A cross-classified multilevel analysis. Journal of Epidemiology & Community Health. 2015;69(11):1091–1101. doi: 10.1136/jech-2014-204506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronfenbrenner U., Morris P.A. The bioecological model of human development. In: Lerner R.M., editor. Handbook of child psychology (Vol. 1: Theoretical models of human development. John Wiley and Sons; Hoboken, NJ: 2006. pp. 793–828. [Google Scholar]
- Browne W.J., Goldstein H., Rasbash J. Multiple membership multiple classification (MMMC) models. Statistical Modelling. 2001;1(2):103–124. doi: 10.1177/1471082X0100100202. [DOI] [Google Scholar]
- Cafri G., Fan J. Between-within effects in survival models with cross-classified clustering: Application to the evaluation of the effectiveness of medical devices. Statistical Methods in Medical Research. 2018;27(1):312–319. doi: 10.1177/0962280216628561. [DOI] [PubMed] [Google Scholar]
- Carroll-Scott A., Gilstad-Hayden K., Rosenthal L., Eldahan A., McCaslin C., Peters S.M. Associations of neighborhood and school socioeconomic and social contexts with body mass index among urban preadolescent students. American Journal of Public Health. 2015;105(12):2496–2502. doi: 10.2105/AJPH.2015.302882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaix B., Bean K., Daniel M., Zenk S.N., Kestens Y., Charreire H. Associations of supermarket characteristics with weight status and body fat: A multilevel analysis of individuals within supermarkets (record study) PLoS One. 2012;7(4):1–10. doi: 10.1371/journal.pone.0032908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaurasiya D. age-Period-cohort analysis of non-communicable diseases in India. Asian Journal of Epidemiology. 2018;11:1–7. [Google Scholar]
- Cheung C., Goodman D., Leckie G., Jenkins J.M. Understanding contextual effects on externalizing behaviors in children in out-of-home care: Influence of workers and foster families. Children and Youth Services Review. 2011;33(10):2050–2060. doi: 10.1016/j.childyouth.2011.05.036. [DOI] [Google Scholar]
- Chum A., O'Campo P. Contextual determinants of cardiovascular diseases: Overcoming the residential trap by accounting for non-residential context and duration of exposure. Health & Place. 2013;24:73–79. doi: 10.1016/j.healthplace.2013.07.007. [DOI] [PubMed] [Google Scholar]
- Congdon P., Best N. Small area variation in hospital admission rates: Bayesian adjustment for primary care and hospital factors. Journal of the Royal Statistical Society - Series C: Applied Statistics. 2000;49:207–226. doi: 10.1111/1467-9876.00188. [DOI] [Google Scholar]
- D'Haese S., Dyck D.v., Bourdeaudhuij I.d., Deforche B., Cardon G. The association between objective walkability, neighborhood socio-economic status, and physical activity in Belgian children. International Journal of Behavioral Nutrition and Physical Activity. 2014;11(104):23. doi: 10.1186/s12966-014-0104-1. August 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D'Haese S., Gheysen F., De Bourdeaudhuij I., Deforche B., Van Dyck D., Cardon G. The moderating effect of psychosocial factors in the relation between neighborhood walkability and children's physical activity. International Journal of Behavioral Nutrition and Physical Activity. 2016;13 doi: 10.1186/s12966-016-0452-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Clercq B., Pfoertner T.-K., Elgar F.J., Hublet A., Maes L. Social capital and adolescent smoking in schools and communities: A cross-classified multilevel analysis. Social Science & Medicine. 2014;119:81–87. doi: 10.1016/j.socscimed.2014.08.018. [DOI] [PubMed] [Google Scholar]
- De Meester F., Van Dyck D., De Bourdeaudhuij I., Deforche B., Cardon G. Changes in physical activity during the transition from primary to secondary school in Belgian children: What is the role of the school environment? BMC Public Health. 2014;14(1):261–275. doi: 10.1186/1471-2458-14-261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dedrick R.F., Ferron J.M., Hess M.R., Hogarty K.Y., Kromrey J.D., Lang T.R. Multilevel modeling: A review of methodological issues and applications. Review of Educational Research. 2009;79(1):69–102. doi: 10.3102/0034654308325581. [DOI] [Google Scholar]
- Delaruelle K., Buffel V., Bracke P. Educational expansion and the education gradient in health: A hierarchical age-period-cohort analysis. Social Science & Medicine. 2015;145:79–88. doi: 10.1016/j.socscimed.2015.09.040. [DOI] [PubMed] [Google Scholar]
- Di Martino M., Alagna M., Cappai G., Mataloni F., Lallo A., Perucci C.A. Adherence to evidence-based drug therapies after myocardial infarction: Is geographic variation related to hospital of discharge or primary care providers? A cross-classified multilevel design. BMJ Open. 2016;6(4) doi: 10.1136/bmjopen-2015-010926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Martino M., Ventura M., Cappai G., Lallo A., Davoli M., Agabiti N. Adherence to long-acting bronchodilators after discharge for COPD: How much of the geographic variation is attributable to the hospital of discharge and how much to the primary care providers? COPD: Journal of Chronic Obstructive Pulmonary Disease. 2017;14(1):86–94. doi: 10.1080/15412555.2016.1202225. [DOI] [PubMed] [Google Scholar]
- Diez Roux A.V. Bringing context back into epidemiology: Variables and fallacies in multilevel analysis. American Journal of Public Health. 1998;88(2):216–222. doi: 10.2105/ajph.88.2.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez Roux A.V. A glossary for multilevel analysis. Journal of Epidemiology & Community Health. 2002;56:588–594. doi: 10.1136/jech.56.8.588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doumouras A.G., Hamidi M., Lung K., Tarola C.L., Tsao M.W., Scott J.W. Non-technical skills of surgeons and anaesthetists in simulated operating theatre crises. British Journal of Surgery. 2017;104(8):1028–1036. doi: 10.1002/bjs.10526. [DOI] [PubMed] [Google Scholar]
- Dundas R., Leyland A.H., Macintyre S. Early-life school, neighborhood, and family influences on adult health: A multilevel cross-classified analysis of the aberdeen children of the 1950s study. American Journal of Epidemiology. 2014;180(2):197–207. doi: 10.1093/aje/kwu110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn E.C., Masyn K.E., Yudron M., Jones S.M., Subramanian S.V. Translating multilevel theory into multilevel research: Challenge and opportunities for understanding the social determinants of psychiatric disorders. Social Psychiatry and Psychiatric Epidemiology. 2014;49:859–872. doi: 10.1007/s00127-013-0809-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn E.C., Milliren C.E., Evans C.R., Subramanian S.V., Richmond T.K. Disentangling the relative influence of schools and neighborhoods on adolescents' risk for depressive symptoms. American Journal of Public Health. 2015;105(4):732–740. doi: 10.2105/AJPH.2014.302374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn E.C., Richmond T.K., Milliren C.E., Subramanian S.V. Using cross-classified multilevel models to disentangle school and neighborhood effects: An example focusing on smoking behaviors among adolescents in the United States. Health & Place. 2015;31:224–232. doi: 10.1016/j.healthplace.2014.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ecob R., Croudace T.J., White I.R., Evans J.E., Harrison G.L., Sharp D. Multilevel investigation of variation in HoNOS ratings by mental health professionals: A naturalistic study of consecutive referrals. International Journal of Methods in Psychiatric Research. 2004;13(3):152–164. doi: 10.1002/mpr.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ecochard R., Clayton D. Multi-level modelling of conception in artificial insemination by donor. Statistics in Medicine. 1998;17:1137–1156. doi: 10.1002/(sici)1097-0258(19980530)17:10<1137::aid-sim822>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- Evans C.R., Onnela J.-P., Williams D.R., Subramanian S.V. Multiple contexts and adolescent body mass index: Schools, neighborhoods, and social networks. Social Science & Medicine. 2016;162:21–31. doi: 10.1016/j.socscimed.2016.06.002. [DOI] [PubMed] [Google Scholar]
- Fielding A. Teaching groups as foci for evaluating performance in cost-effectiveness of GCE advanced level provision: Some practical methodological Innovations 1. School Effectiveness and School Improvement. 2002;13(2):225–246. doi: 10.1076/sesi.13.2.225.3435. [DOI] [Google Scholar]
- Fielding A., Goldstein H. University of Birmingham; Birmingham, England: 2006. Cross-classified and multiple membership structures in multilevel models: An introduction and review (vol. Research report RR791) [Google Scholar]
- Fienberg S.E., Mason W.M. Identification and estimation of age-period-cohort models in the analysis of discrete archival data. Sociological Methodology. 1979;10:1–67. doi: 10.2307/270764. [DOI] [Google Scholar]
- Fischbach L.A., Goodman K.J., Feldman M., Aragaki C. Sources of variation of Helicobacter pylori treatment success in adults worldwide: A meta-analysis. International Journal of Epidemiology. 2002;31(1):128–139. doi: 10.1093/ije/31.1.128. [DOI] [PubMed] [Google Scholar]
- Fu Q., Land K.C. The increasing prevalence of overweight and obesity of children and youth in China, 1989–2009: An age– period–cohort analysis. Population Research and Policy Review. 2015;34:901–921. [Google Scholar]
- Gifford E., Foster E.M. Provider-level effects on psychiatric inpatient length of stay for youth with mental health and substance abuse disorders. Medical Care. 2008;46(3):240–246. doi: 10.1097/MLR.0b013e318158aee7. [DOI] [PubMed] [Google Scholar]
- Giordano G.N., Ohlsson H., Kendler K.S., Winkleby M.A., Sundquist K., Sundquist J. Age, period and cohort trends in drug abuse hospitalizations within the total Swedish population (1975–2010) Drug and Alcohol Dependence. 2014;134:355–361. doi: 10.1016/j.drugalcdep.2013.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glenn N.D. Cohort analysts' futile quest: Statistical attempts to separate age, period, and cohort effects. American Sociological Review. 1976;41:900–904. doi: 10.2307/2094738. [DOI] [Google Scholar]
- Goldstein H. Multilevel cross-classified models. Sociological Methods & Research. 1994;22(3):364–375. doi: 10.1177/0049124194022003005. [DOI] [Google Scholar]
- Goldstein H. Cross-classified data structures. In: Goldstein H., editor. Multilevel statistical models. 4th ed. Wiley; Chichester, UK: 2011. [Google Scholar]
- Groenewegen P.P., Zock J.-P., Spreeuwenberg P., Helbich M., Hoek G., Ruijsbroek A. Neighbourhood social and physical environment and general practitioner assessed morbidity. Health & Place. 2018;49:68–84. doi: 10.1016/j.healthplace.2017.11.006. [DOI] [PubMed] [Google Scholar]
- Gross C.P., Herrin J., Wong N., Krumholz H.M. Enrolling older persons in cancer trials: The effect of sociodemographic, protocol, and recruitment center characteristics. Journal of Clinical Oncology. 2005;23(21):4755–4763. doi: 10.1200/jco.2005.14.365. [DOI] [PubMed] [Google Scholar]
- Gustafsson P.E., Bozorgmehr K., Hammarstrom A., San Sebastian M. What role does adolescent neighborhood play for adult health? A cross-classified multilevel analysis of life course models in northern Sweden. Health & Place. 2017;46:137–144. doi: 10.1016/j.healthplace.2017.04.013. [DOI] [PubMed] [Google Scholar]
- Hidehiro S., Ken H., Yoko S., Shizuko Y., Masaya S. Socioeconomic status and self-rated health of Japanese people, based on age, cohort, and period. Population Health Metrics. 2016;14:1–11. doi: 10.1186/s12963-016-0095-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofer T.P., Asch S.M., Hayward R.A., Rubenstein L.V., Hogan M.M., Adams J. Profiling quality of care: Is there a role for peer review? BMC Health Services Research. 2004;4(1):9. doi: 10.1186/1472-6963-4-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooiveld M., Smit L.A.M., Sman-de Beer F.v. d., Wouters I.M., Dijk C.E.v., Spreeuwenberg P. Doctor-diagnosed health problems in a region with a high density of concentrated animal feeding operations: A cross-sectional study. Environmental Health. 2016;15(24) doi: 10.1186/s12940-016-0123-2. 17 February 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hox J. 2nd ed. Routledge; New York: 2010. Chapter 9: Cross-classified multilevel models in multilevel analysis Techniques and applications. [Google Scholar]
- Huijts T., Kraaykamp G. Immigrants' health in europe: A cross-classified multilevel approach to examine origin country, destination country, and community effects. International Migration Review. 2012;46(1):101–137. doi: 10.1111/j.1747-7379.2012.00882.x. [DOI] [PubMed] [Google Scholar]
- IDRE SPSS mixed command. 2020. https://stats.idre.ucla.edu/spss/seminars/spss-mixed-command/ Retrieved from.
- Kendler K., Ohlsson H., Sundquist K., Sundquist J. Environmental clustering of drug abuse in households and communities: Multi-level modeling of a national Swedish sample. Social Psychiatry and Psychiatric Epidemiology. 2015;50(8):1277–1284. doi: 10.1007/s00127-015-1030-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes K.M., Gary D., O'Malley P.O., Hamilton A., Schulenberg J. Recent increases in depressive symptoms among US adolescents: Treats from 1991 to 2018. Social Psychiatry and Psychiatric Epidemiology. 2019 doi: 10.1007/s00127-019-01697-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirby J.B. Poor people, poor places and access to health care in the United States. Social Forces. 2008;87(1):325–355. [Google Scholar]
- Kraus L., Tinghog M.E., Lindell A., Pabst A., Piontek D., Room R. Age, period and cohort effects on time trends in alcohol consumption in the Swedish adult population 1979-2011. Alcohol and Alcoholism. 2015;50(3):319–327. doi: 10.1093/alcalc/agv013. [DOI] [PubMed] [Google Scholar]
- Krieger N. A glossary for social epidemiology. Journal of Epidemiology & Community Health. 2001;55:693–700. doi: 10.1136/jech.55.10.693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N., Chen J., Coull B., Beckfield J., Kiang M., Waterman P. Jim crow and premature mortality among the US black and white population, 1960–2009: An age–period–cohort analysis. Epidemiology. 2014;25(4):494–504. doi: 10.1097/EDE.0000000000000104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwon S., Schafer M.H. Improving but unequal: Temporal trends in Chinese self-rated health, 1990–2012. SSM Population Health. 2016;2:77–83. doi: 10.1016/j.ssmph.2016.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langford I.H., Bentham G. Regional variations in mortality rates in England and Wales: An analysis using multi-level modelling. Social Science & Medicine. 1996;42(6):897–908. doi: 10.1016/0277-9536(95)00188-3. [DOI] [PubMed] [Google Scholar]
- Leckie G., Bell A. University of Bristol: Centre for Multilevel Modeling; 2013. Cross-classified multilevel models. [Google Scholar]
- Leckie G., Charlton C. Runmlwin: A program to run the MLwiN multilevel modeling software from within Stata. Journal of Statistical Software. 2013;1(11) 2013. [Google Scholar]
- Levac D., Colquhoun H., O'Brien K.K. Scoping studies: Advancing the methodology. Implementation Science. 2010;5:69. doi: 10.1186/1748-5908-5-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leyland A.H., Naess O. The effect of area of residence over the life course on subsequent mortality. Journal of the Royal Statistical Society - Series A: Statistics in Society. 2009;172:555–578. doi: 10.1111/j.1467-985X.2008.00581.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li L., Georgiou A., Vecellio E., Eigenstetter A., Toouli G., Wilson R. The effect of laboratory testing on emergency department length of stay: A multihospital longitudinal study applying a cross-classified random-effect modeling approach. Academic Emergency Medicine. 2015;22(1):38–46. doi: 10.1111/acem.12565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin S.-F., Beck A.N., Finch B.K. Black–white disparity in disability among U.S. older adults: Age, period, and cohort trends. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2014;69(5):784–797. doi: 10.1093/geronb/gbu010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin S.-F., Beck A.N., Finch B.K. The Dynamic contribution of chronic conditions to temporal trends in disability among U.S. adults. Disability and Health Journal. 2016;9(2):332–340. doi: 10.1016/j.dhjo.2015.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linton S.L., Jennings J.M., Latkin C.A., Kirk G.D., Mehta S.H. The association between neighborhood residential rehabilitation and injection drug use in Baltimore, Maryland, 2000-2011. Health & Place. 2014;28:142–149. doi: 10.1016/j.healthplace.2014.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livingston M., Raninen J., Slade T., Swift W., Lloyd B., Dietze P. Understanding trends in Australian alcohol consumption—an age–period–cohort model. Addiction. 2016;111(9):1590–1598. doi: 10.1111/add.13396. [DOI] [PubMed] [Google Scholar]
- Luo H.B., Pan W., Sloan F., Feinglos M., Wu B. Forty-year trends in tooth loss among American adults with and without diabetes mellitus: An age-period-cohort analysis. Preventing Chronic Disease. 2015;12 doi: 10.5888/pcd12.150309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mair C.F., Diez Roux A.V., Galea S. Are neighborhood characteristics associated with depressive symptoms? A critical review. Journal of Epidemiology & Community Health. 2008;62(11):940–946. doi: 10.1136/jech.2007.066605. [DOI] [PubMed] [Google Scholar]
- Masters R.K. Uncrossing the U.S. Black-white mortality crossover: The role of cohort forces in life course mortality risk. Demography. 2012;49:773–796. doi: 10.1007/s13524-012-0107-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masters R.K., Hummer R.A., Powers D.A. Educational differences in U.S. Adult mortality: A cohort perspective. American Sociological Review. 2012;77(4):548–572. doi: 10.1177/0003122412451019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masters R.K., Reither E.N., Powers D.A., Yang Y.C., Burger A.E., Link B.G. The impact of obesity on US mortality levels: The importance of age and cohort factors in population estimates. American Journal of Public Health. 2013;103(10):1895–1901. doi: 10.2105/AJPH.2013.301379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNeish D.M., Stapleton L.M. The effect of small sample size on two-level model estimates: A review and illustration. Educational Psychology Review. 2016;28(2):295–314. doi: 10.1007/s10648-014-9287-x. [DOI] [Google Scholar]
- Merlo J., Chaix B., Ohlsson H., Beckman A., Johnell K., Hjerpe P. A brief conceptual tutorial of multilevel analysis in social epidemiology: Using measures of clustering in multilevel logistic regression to investigate contextual phenomena. Journal of Epidemiology & Community Health. 2006;60(4):290. doi: 10.1136/jech.2004.029454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meunier J.C., Bisceglia R., Jenkins J.M. Differential parenting and children's behavioral problems: Curvilinear associations and mother-father combined effects. Developmental Psychology. 2012;48(4):987–1002. doi: 10.1037/a0026321. [DOI] [PubMed] [Google Scholar]
- Meyers J.L., Beretvas S.N. The impact of inappropriate modeling of cross-classified data structures. Multivariate Behavioral Research. 2006;41(4):473–497. doi: 10.1207/s15327906mbr4104_3. [DOI] [PubMed] [Google Scholar]
- Milliren C.E., Evans C.R., Richmond T.K., Dunn E.C. Does an uneven sample size distribution across settings matter in cross-classified multilevel modeling? Results of a simulation study. Health & Place. 2018;52:121–126. doi: 10.1016/j.healthplace.2018.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milliren C.E., Richmond T.K., Evans C.R., Dunn E.C., Johnson R.M. Contextual effects of neighborhoods and schools on adolescent and young adult marijuana use in the United States. Substance Abuse. 2017;11 doi: 10.1177/1178221817711417. 1178221817711417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D., Shamseer L., Clarke M., Ghersi D., Liberati A., Petticrew M. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic Reviews. 2015;4:1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore K., Diez Roux A.V., Auchincloss A., Evenson K.R., Kaufman J., Mujahid M. Home and work neighbourhood environments in relation to body mass index: The multi-ethnic study of atherosclerosis (MESA) Journal of Epidemiology & Community Health. 2013;67(10):846–853. doi: 10.1136/jech-2013-202682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morton K.L., Corder K., Suhrcke M., Harrison F., Jones A.P., van Sluijs E.M. School polices, programmes and facilities, and objectively measured sedentary time, LPA and MVPA: Associations in secondary school and over the transition from primary to secondary school. International Journal of Behavioral Nutrition and Physical Activity. 2016;13:54. doi: 10.1186/s12966-016-0378-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muntaner C., Li Y., Ng E., Benach J., Chung H. Work or place? Assessing the concurrent effects OF workplace exploitation and area-of-residence economic inequality ON individual health. International Journal of Health Services. 2011;41(1):27–50. doi: 10.2190/HS.41.1.c. [DOI] [PubMed] [Google Scholar]
- Muntaner C., Li Y., Xue X., O'Campo P., Chung H.J., Eaton W.W. Work organization, area labor-market characteristics, and depression among U.S. Nursing home workers: A cross-classified multilevel analysis. International Journal of Occupational and Environmental Health. 2004;10(4):392–400. doi: 10.1179/oeh.2004.10.4.392. [DOI] [PubMed] [Google Scholar]
- Muntaner C., Li Y., Xue X., Thompson T., Chung H., O'Campo P. County and organizational predictors of depression symptoms among low-income nursing assistants in the USA. Social Science & Medicine. 2006;63(6):1454–1465. doi: 10.1016/j.socscimed.2006.03.042. [DOI] [PubMed] [Google Scholar]
- Muntaner C., Li Y., Xue X., Thompson T., O'Campo P., Chung H. County level socioeconomic position, work organization and depression disorder: A repeated measures cross-classified multilevel analysis of low-income nursing home workers. Health & Place. 2006;12(4):688–700. doi: 10.1016/j.healthplace.2005.09.004. [DOI] [PubMed] [Google Scholar]
- Murray E.T., Ben-Shlomo Y., Tilling K., Southall H., Aucott P., Kuh D. Area deprivation across the life course and physical capability in midlife: Findings from the 1946 British birth cohort. American Journal of Epidemiology. 2013;178(3):441–450. doi: 10.1093/aje/kwt003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohlsson H., Merlo J. Place effects for areas defined by administrative boundaries: A life course analysis of mortality and cause specific morbidity in scania, Sweden. Social Science & Medicine. 2011;73(8):1145–1151. doi: 10.1016/j.socscimed.2011.08.005. [DOI] [PubMed] [Google Scholar]
- Pedan A., Varasteh L.T., Schneeweiss S. Analysis of factors associated with statin adherence in a hierarchical model considering physician, pharmacy, patient, and prescription characteristics. Journal of Managed Care Pharmacy. 2007;13(6):487–496. doi: 10.18553/jmcp.2007.13.6.487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen W., Bakken A., Soest T. Neighborhood or school? Influences on alcohol consumption and heavy episodic drinking among urban adolescents. Journal of Youth and Adolescence. 2017;47:2073–2087. doi: 10.1007/s10964-017-0787-0. [DOI] [PubMed] [Google Scholar]
- Penfold R., Deena C., Benedict N., Kelleher K. Geographic disparities in the risk of perforated appendicitis among children in Ohio: 2001--2003. International Journal of Health Geographics. 2008;7:56–64. doi: 10.1186/1476-072X-7-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickett K.E., Pearl M. Multilevel analyses of neighbourhood socioeconomic context and health outcomes: A critical review. Journal of Epidemiology & Community Health. 2001;55(111–122) doi: 10.1136/jech.55.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilbery R., Teare M.D., Goodacre S., Morris F. The recognition of STEMI by paramedics and the effect of computer inTerpretation (RESPECT): A randomised crossover feasibility study. Emergency Medicine Journal. 2016;33(7):471–476. doi: 10.1136/emermed-2015-204988. [DOI] [PubMed] [Google Scholar]
- Piontek D., Kraus L., Müller S., Pabst A. To what extent do age, period, and cohort patterns account for time trends and social inequalities in smoking? Sucht - Zeitschrift für Wissenschaft und Praxis. 2010;56(5):361–371. doi: 10.1024/0939-5911/a000047. [DOI] [Google Scholar]
- Piontek D., Kraus L., Pabst A., Legleye S. An age-period-cohort analysis of cannabis use prevalence and frequency in Germany, 1990-2009. Journal of Epidemiology & Community Health. 2012;66(10):908–913. doi: 10.1136/jech-2011-200180. [DOI] [PubMed] [Google Scholar]
- Pruitt S.L., Leonard T., Zhang S., Schootman M., Halm E.A., Gupta S. Physicians, clinics, and neighborhoods: Multiple levels of influence on colorectal cancer screening. Cancer Epidemiology Biomarkers & Prevention. 2014;23(7):1346–1355. doi: 10.1158/1055-9965.epi-13-1130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasbash J., Goldstein H. Efficient analysis of mixed hierarchical and cross-classified random structures using a multilevel model. Journal of Educational and Behavioral Statistics. 1994;19(4):337–350. [Google Scholar]
- Ratnapradipa K.L., Lian M., Jeffe D.B., Davidson N.O., Eberth J.M., Pruitt S.L. Patient, hospital, and geographic disparities in laparoscopic surgery use among surveillance, epidemiology, and end results-medicare patients with colon cancer. Diseases of the Colon & Rectum. 2017;60(9):905–913. doi: 10.1097/dcr.0000000000000874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raudenbush S.W., Bryk A.S. 2nd ed. Sage Publications; Thousand Oaks, CA: 2002. Hierarchical linear models: Applications and data analysis method. [Google Scholar]
- Reither E.N., Hauser R.M., Yang Y. Do birth cohorts matter? age-Period-cohort analyses of the obesity epidemic in the United States. Social Science & Medicine. 2009;69:1439–1448. doi: 10.1016/j.socscimed.2009.08.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richmond T.K., Dunn E.C., Milliren C.E., Evans C.R., Subramanian S.V. Disentangling overlapping influences of neighborhoods and schools on adolescent body mass index. Obesity. 2016;24(12):2570–2577. doi: 10.1002/oby.21672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riva M., Gauvin L., Apparicio P., Brodeur J.M. Disentangling the relative influence of built and socioeconomic environments on walking: The contribution of areas homogenous along exposures of interest. Social Science & Medicine. 2009;69(9):1296–1305. doi: 10.1016/j.socscimed.2009.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan-Ibarra S., Milet M., Lutzker L., Rodriguez D., Induni M., Kreutzer R. Age, period, and cohort effects in adult lifetime asthma prevalence in California: An application of hierarchical age-period-cohort analysis. Annals of Epidemiology. 2016;26(2):87–92. doi: 10.1016/j.annepidem.2015.12.002. e82. [DOI] [PubMed] [Google Scholar]
- Schofield P., Das-Munshi J., Mathur R., Congdon P., Hull S. Does depression diagnosis and antidepressant prescribing vary by location? Analysis of ethnic density associations using a large primary-care dataset. Psychological Medicine. 2016;46(6):1321–1329. doi: 10.1017/S0033291715002913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schootman M., Lian M., Pruitt S.L., Hendren S., Mutch M., Deshpande A.D. Hospital and geographic variability in two colorectal cancer surgery outcomes: Complications and mortality after complications. Annals of Surgical Oncology. 2014;21(8):2659–2666. doi: 10.1245/s10434-013-3472-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharp G., Denney J.T., Kimbro R.T. Multiple contexts of exposure: Activity spaces, residential neighborhoods, and self-rated health. Social Science & Medicine. 2015;146:204–213. doi: 10.1016/j.socscimed.2015.10.040. [DOI] [PubMed] [Google Scholar]
- Sink D.W., Hope S.A.E., Hagadorn J.I. Nurse:patient ratio and achievement of oxygen saturation goals in premature infants. Archives of Disease in Childhood - Fetal and Neonatal Edition. 2011;96(2):F93–F98. doi: 10.1136/adc.2009.178616. [DOI] [PubMed] [Google Scholar]
- Stokols D. Translating social ecological theory into guidelines for community health promotion. American Journal of Health Promotion. 1996;10:282–298. doi: 10.4278/0890-1171-10.4.282. [DOI] [PubMed] [Google Scholar]
- Subramanian S.V., Jones K., Duncan C. Multilevel methods for public health research. In: Kawachi I., Berkman L.F., editors. Neighborhoods and health. Oxford University Press; New York, NY: 2003. pp. 65–111. [Google Scholar]
- Sugisawa H., Shimizu Y., Kumagai T., Sugisaki H., Ohira S., Shinoda T. Effects of socioeconomic status on physical and mental health of hemodialysis patients in Japan: Differences by age, period, and cohort. International Journal of Nephrology and Renovascular Disease. 2016;9:171–182. doi: 10.2147/IJNRD.S107031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang Z. They are richer but are they happier? Subjective well-being of Chinese citizens across the reform era. Social Indicators Research. 2014;117(1):145–164. doi: 10.1007/s11205-013-0339-2. [DOI] [Google Scholar]
- Teisl M.F., Lando A.M., Levy A.S., Noblet C.L. Importance of cohorts in analyzing trends in safe at-home food-handling practices. Food Control. 2016;62:381–389. [Google Scholar]
- Teitler J.O., Weiss C.C. Effects of neighborhood and school environments on transitions to first sexual intercourse. Sociology of Education. 2000;73(2):112–132. [Google Scholar]
- Thibodeau L. Cohort size and suicide mortality in Canada: An assessment of the easterlin and preston theories in the GI through the Y generations. Population Review. 2015;54(2):47–67. [Google Scholar]
- Thomas K.S., Rahman M., Mor V., Intrator O. Influence of hospital and nursing home quality on hospital readmissions. American Journal of Managed Care. 2014;20(11):E523–+. [PMC free article] [PubMed] [Google Scholar]
- Thorpe R.J., Fesahazion R.G., Parker L., Wilder T., Rooks R.N., Bowie J.V. Accelerated health declines among african Americans in the USA. Journal of Urban Health. 2016;93(5):808–819. doi: 10.1007/s11524-016-0075-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Townsend N., Rutter H., Foster C. Age differences in the association of childhood obesity with area-level and school-level deprivation: Cross-classified multilevel analysis of cross-sectional data. International Journal of Obesity. 2012;36(1):45–52. doi: 10.1038/ijo.2011.191. [DOI] [PubMed] [Google Scholar]
- Tsugawa Y. ProQuest Information & Learning; US: 2018. Variation in quality and costs of care across physicians and its determinants. (78)http://ezp-prod1.hul.harvard.edu/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=psyh&AN=2017-43830-093&site=ehost-live&scope=site Available from EBSCOhost psyh database Retrieved from. [Google Scholar]
- Twenge J.M., Sherman R.A., Wells B.E. Sexual inactivity during young adulthood is more common among U.S. Millennials and iGen: Age, period, and cohort effects on having No sexual partners after age 18. Archives of Sexual Behavior. 2017;46:433–440. doi: 10.1007/s10508-016-0798-z. [DOI] [PubMed] [Google Scholar]
- Urquia M.L., Frank J.W., Glazier R.H. From places to flows. International secondary migration and birth outcomes. Social Science & Medicine. 2010;71(9):1620–1626. doi: 10.1016/j.socscimed.2010.08.006. [DOI] [PubMed] [Google Scholar]
- Urquia M.L., Frank J.W., Glazier R.H., Moineddin R., Matheson F.I., Gagnon A.J. Neighborhood context and infant birthweight Among recent immigrant mothers: A multilevel analysis. American Journal of Public Health. 2009;99(2):285–293. doi: 10.2105/ajph.2007.127498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urquia M., Frank J., Moineddin R., Glazier R. Does time since immigration modify neighborhood deprivation gradients in preterm birth? A multilevel analysis. Journal of Urban Health. 2011;88(5):959–976. doi: 10.1007/s11524-011-9569-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Utter J., Denny S., Robinson E., Ameratunga S., Milfont T.L. Social and physical contexts of schools and neighborhoods: Associations with physical activity among young people in New Zealand. American Journal of Public Health. 2011;101(9):1690–1695. doi: 10.2105/ajph.2011.300171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vigil J.M., Coulombe P., Alcock J., Stith S.S., Kruger E., Cichowski S. How nurse gender influences patient priority assignments in US emergency departments. Pain. 2017;158(3):377–382. doi: 10.1097/j.pain.0000000000000725. 03043959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Virtanen M., Kivimaki M., Pentti J., Oksanen T., Ahola K., Linna A. School neighborhood disadvantage as a predictor of long-term sick leave among teachers: Prospective cohort study. American Journal of Epidemiology. 2010;171(7):785–792. doi: 10.1093/aje/kwp459. [DOI] [PubMed] [Google Scholar]
- Volken T., Wieber F., Ruesch P., Huber M., Crawford R.J. Temporal change to self-rated health in the Swiss population from 1997 to 2012: The roles of age, gender, and education. Public Health. 2017;150:152–165. doi: 10.1016/j.puhe.2017.07.007. [DOI] [PubMed] [Google Scholar]
- Weich S., McBride O., Twigg L., Duncan C., Keown P., Crepaz-Keay D. Variation in compulsory psychiatric inpatient admission in england: A cross-classified, multilevel analysis. The Lancet Psychiatry. 2017;4(8):619–626. doi: 10.1016/S2215-0366(17)30207-9. [DOI] [PubMed] [Google Scholar]
- West P., Sweeting H., Leyland A. School effects on pupils' health behaviours: Evidence in support of the health promoting school. Research Papers in Education. 2004;19(3):261–291. doi: 10.1080/0267152042000247972. [DOI] [Google Scholar]
- Wilk P., Clark A.F., Maltby A., Smith C., Tucker P., Gilliland J.A. Examining individual, interpersonal, and environmental influences on children's physical activity levels. SSM Popul Health. 2018;4:76–85. doi: 10.1016/j.ssmph.2017.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilk P., Maltby A., Cooke M. Changing BMI scores among Canadian Indigenous and non-Indigenous children, youth and young adults: Untangling age, period, and cohort effects. Canadian Studies in Population. 2017;44(1–2):28–41. doi: 10.25336/P6HK5D. [DOI] [Google Scholar]
- Williams J., Scarborough P., Townsend N., Matthews A., Burgoine T., Mumtaz L. Associations between Food Outlets around Schools and BMI among Primary Students in England: A Cross-Classified Multi-Level Analysis (vol 10, e0132930, 2015) PLoS One. 2016;11(1) doi: 10.1371/journal.pone.0147164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willson R., Abbott J.H. Age, period and cohort effects on body mass index in New Zealand, 1997–2038. Aust NZ J Public Health. 2018;42:396–402. doi: 10.1111/1753-6405.12804. [DOI] [PubMed] [Google Scholar]
- Winpenny E.M., Corder K.L., Jones A., Ambrosini G.L., White M., van Sluijs E.M.F. Changes in diet from age 10 to 14 years and prospective associations with school lunch choice. Appetite. 2017;116:259–267. doi: 10.1016/j.appet.2017.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young R.L., Weinberg J., Vieira V., Aschengrau A., Webster T.F. A multilevel non-hierarchical study of birth weight and socioeconomic status. International Journal of Health Geographics. 2010;9 doi: 10.1186/1476-072x-9-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu R., Wong M., Chang B., Lai X., Lum C.M., Auyeung T.W. Trends in activities of daily living disability in a large sample of community-dwelling Chinese older adults in Hong Kong: An age-period-cohort analysis. BMJ Open. 2016;6(12) doi: 10.1136/bmjopen-2016-013259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaccarin S., Rivellini G. Multilevel analysis in social research: An application of a cross-classified model. Statistical Methods and Applications. 2002;11(1):95–108. doi: 10.1007/bf02511448. [DOI] [Google Scholar]
- Zhang L. An age–period–cohort analysis of religious involvement and adult self-rated health: Results from the USA, 1972–2008. Journal of Religion and Health. 2017;56(3):916–945. doi: 10.1007/s10943-016-0292-x. [DOI] [PubMed] [Google Scholar]
- Zheng H., Yang Y., Land K.C. Variance function regression in hierarchical age-period- cohort models: Applications to the study of self-reportedS health. American Sociological Review. 2011;76(6):955–983. doi: 10.1177/0003122411430940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng H., Yang Y.C., Land K.C. Age-specific variation in adult mortality rates in developed countries. Population Research and Policy Review. 2016;35:49–71. doi: 10.1007/s11113-015-9379-4. [DOI] [PMC free article] [PubMed] [Google Scholar]