Abstract
Central giant cell granuloma (CGCG) is an expansile osteolytic lesion of the jawbone. Conventional treatment of CGCG is surgical and vary from simple curettage to more aggressive resection of the jaw. However, surgical management is associated with drawbacks including requirement of hospitalisation and general anaesthesia, damage to vital anatomic structures and continuity defect of the mandible requiring reconstruction surgery. Use of intralesional injections of corticosteroid for the management of CGCG have been inconsistently used as an alternative non-surgical method of management of CGCG with varying success. While the use of such conservative modality over ablative surgery can significantly reduce postoperative morbidity, follow-up of such cases for a long period is important to study the possible recurrence. This paper reports successful treatment of a recurrent CGCG of posterior mandible by intralesional administration of triamcinolone acetonide in a 27-year old female patient, with long-term follow-up of 10 years.
Keywords: dentistry and oral medicine, oral and maxillofacial surgery
Background
Central giant cell granuloma (CGCG) is an uncommon intraosseous, expansile lesion of the jawbone. Although it is regarded as a benign tumour, occasionally it behaves in an aggressive fashion giving rise to extensive bone destruction and high rate of recurrence, if managed conservatively.1 Aggressive and recurrent lesions have been traditionally managed by radical surgical resection often leading to major defects, facial disfigurement and loss of teeth. This is particularly mutilating in patients of younger age group and growing children. An alternative nonsurgical method of managing CGCG by administering intralesional injections of corticosteroid was first reported by Jacoway et al in year 1988.2 Since then, intralesional corticosteroids have been used by multiple authors with varying amount of success and with different durations of follow-up.3–5 This paper describes treatment of recurrent CGCG of posterior mandible by intralesional administration of triamcinolone acetonide in a 27-year young female patient, with a clinical and radiological follow-up of 10 years.
Case presentation
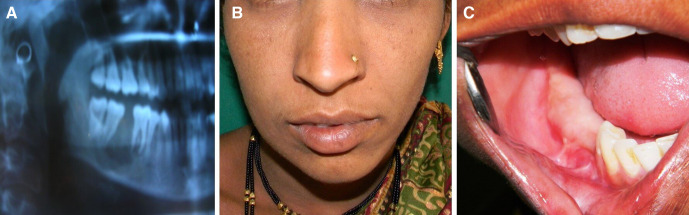
A 27-year-old woman reported to oral and maxillofacial surgery clinic with a complaint of swelling over the right side of the face since past 1 year. Patient gave history of previous surgery in the same region 3 years ago. Evaluation of her medical records, radiograph (figure 1A) and histopathology report, revealed that an intraosseous lytic lesion in posterior mandible histologically diagnosed as CGCG was treated by extraction of teeth and curettage of the lesion under local anaesthesia. Extraoral examination revealed a hard swelling in the right body-angle region of the mandible, extending from 1 cm behind the corner of mouth to the angle of the mandible, measuring approximately 3×3 cm in size (figure 1B). Swelling was hard and non-tender on palpation and caused expansion of buccal and lingual cortices of the mandible over the alveolar bone (figure 1C). An orthopantomogram was advised, which showed well-defined mixed radiolucency with sclerotic border in right body-angle of mandible (figure 2A). Previous diagnosis of CGCG was confirmed by histopathological examination of incision biopsy specimen form the lesion. Blood investigations were carried out to rule out evidence of primary hyperparathyroidism.
Figure 1.
Orthopantomogram from previous medical records of the patient taken 3 years ago showing the jaw lesion (A), clinical photographs showing extraoral (B) and intraoral swelling (C).
Figure 2.
Orthopantomogram before starting intralesional steroid injection (A), othopantomogram at 1 year (B) and 10 years (C) follow-up.
Treatment
Options for the treatment of the lesion using surgical resection and intralesional corticosteroid injection were discussed with the patient and her family. After deliberating on the benefits and limitations of both the procedures, patient opted for intralesional corticosteroid injection. Prior to starting the intralesional corticosteroid administration, diabetes mellitus and presence of peptic ulcer were ruled out. Patient was explained that the use of intralesional corticosteroid would not necessitate removal of the teeth involving or in the vicinity of the lesion. Intralesional injection was prepared by mixing triamcinolone acetonide (kenacort 10 mg/mL, Piramal Healthcare) with equal amount of 2% lignocaine hydrochloride with 1:80 000 epinephrine (Warren Pharmaceuticals). The solution was administered using a 10 mL syringe with 18-gauge needle (Dispovan). Approximately 1 mL of the prepared mixture was injected for every cm of radiolucency measured on the radiograph. The site of injection was the area of maximum bone expansion, that is, the area where bone was thinnest. The needle was redirected in the lesion so as to inject the solution uniformly in all areas of the lesion. Injections were given once, on weekly basis, and treatment was terminated at the eighth week when significant resistance was felt in penetration of the needle and injection of solution into the lesion.
Outcome and follow-up
Patient was kept on regular clinical follow-up. Serial orthopantomograms were taken at every 6 months to evaluate the intraosseous healing and bone fill. At the end of 12 months, there was significant reduction in the size of lesion with reduction in the radiolucency seen on the radiograph (figure 2B). The patient at 10 years follow-up was asymptomatic with no evidence of recurrence on radiographic examination (figure 2C).
Discussion
WHO defines CGCG as an intraosseous lesion consisting of cellular fibrous tissue that contains multiple foci of haemorrhage, aggregations of multinucleated giant cells and occasionally trabeculae of woven bone.6 The lesion was first described by Jaffe in year 1953.7 CGCG contributes to about 10% of the benign lesion of the jawbone and occurs most commonly in young adults in second to fourth decade of life.8 It is more common in females, with reported female-to-male ratio of 2:1. The lesion is more commonly seen in mandible as compared with maxilla.9
CGCG is usually asymptomatic producing painless expansion of the affected jaw, which may get discovered during routine radiography. Rapid growth can occasionally produce pain due to stretching of the periosteum. Larger lesions result in mobility of involved teeth and root resorption. Rarely pathological fracture of the jaw can also be seen. Radiographically, CGCG presents as osteolytic lesion, producing radiolucent area with smooth or a ragged border.10 The radiographic findings are not specifically diagnostic. Small unilocular radiolucencies may be confused with periapical granulomas or cysts. Large multilocular radiolucencies cannot be distinguished radiographically from an ameloblastoma or other multilocular radiolucencies of jaws. Choung et al classified CGCG in aggressive and non-aggressive variants.11 The aggressive variant is characterised by lesions that are rapidly growing and is usually associated with pain. These lesions also lead to cortical perforation, root resorption and are associated with high recurrence rate of approximately 20%–70%. The non-aggressive variant is slow growing and manifests as a variable swelling that is not associated with pain, root resorption or cortical perforation. They are associated with low recurrence rate of 10%–15%.11
Both surgical management and pharmacological management of CGCG have been reported in the literature with varying degree of success and associated advantages and limitations. Conventionally, surgery is the mainstay for the treatment of CGCG. The extent of surgery ranges from conservative enucleation to more radical enbloc resection.12 Although aggressive curettage often combined with peripheral ostectomy provides successful outcome, it is associated with high recurrence rate of up to 70%.11 Enbloc resection yields lesser rate of recurrence, but is associated with higher risk of damage to vital anatomical structures and requirement of demanding reconstruction procedure. Drawback of surgery, especially in children and young adult, has led to an interest in search of more conservative pharmacological management of CGCG. Various chemicals have been reportedly used for the management of CGCG, including antiangiogenic drug (interferon), calcitonin and corticosteroids.12 Use of denosumab and bisphosphonate either alone or in combination with corticosteroid has been reported in successful management of CGCG.13 14
Use of intralesional corticosteroid for the management of CGCG was first reported by Jacoway et al in year 1988.2 It is hypothesised that corticosteroids bring about resolution of the lesion by two mechanisms; by inhibiting the action of bone resorbing lysosomal proteases produced by giant cells in CGCG and by inducing apoptotic cell death of osteoclasts.15 Terry and Jacoway in 1994 proposed the treatment protocol of CGCG with intralesional corticosteroids. This included weekly intralesional injection of mixture of equal parts of triamcinolone acetonide (10 mg/mL) and a local anaesthetic (bupivacaine 0.5% with epinephrine 1:200 000), in recommended dose of 1 mL per cm of radiolucency of CGCG on orthopantomogram.16 Although triamcinolone acetonide is most popularly used, other steroid used for intralesional injection in the management of CGCG includes triamcinolone hexacetonide17 and prednisolone.18 In the present case, injections of triamcinolone acetonide were given weekly, and the treatment was terminated at eighth week when significant resistance was felt to penetration of the needle and injection of solution.
Since the protocol of use of corticosteroids has been proposed, various authors have reported their experience with varying degree of success and with varying follow-up periods.3–5 19 Though corticosteroid is a promising option for conservative management of CGCG, it has not provided positive response in all the cases. The reported results have varied from complete cure4 to no response4 or partial resolution20 21 especially for lesions that are clinically aggressive and have multilocular appearance. Dolanmaz et al in a review of 46 cases (reported in 19 papers, from year 1994 to 2015) reported success rate ranging from 50% to 75%.22 The criteria for success of treatment include stabilisation or regression of lesion size evaluated clinically and/or on radiograph, absence of symptoms (pain or swelling), increased radiopacity representing peripheral and/or central calcification and resistance in infiltrating the solution in the lesion during the sequential application.12 17 Patients treated successfully with intralesional corticosteroid may still need minor surgical procedure of osteoplasty to re-establish jaw contour and facial aesthetics.17 Long-term follow-up of these patients is essential to monitor recurrence and evaluate the success of therapy. According to the literature, the follow-up period has varied from 10 months to 8 years. In this case, the patient was followed for 10 years and showed resolution of swelling clinically. Radiographical review on orthopantomogram showed improved bone fill.
Intralesional corticosteroid is a promising conservative management option for CGGG. However, the success rate associated with it has been variable, warranting a long-term follow-up. The present case highlights successful conservative management of CCGG of posterior mandible in young adult female patient on long-term follow-up.
Patient’s perspective.
I had a previous surgery for the jaw tumour, and almost 3 years later I was diagnosed with recurrence of the disease. It was a difficult news for me. When I was given an option that steroid injections can be used for the cure and surgery can be avoided or postponed, it was a huge relief for me. I was made to understand the need for periodic injection and the importance of long-term check-up visits to evaluate the success of treatment. I have maintained the yearly check-up visits and until I have no signs of the jaw pathology. I intend to keep coming back for the radiological assessment as has been advised to me by my doctors.
Learning points.
Central giant cell granuloma (CGCG) is an uncommon jaw tumour, with varying degree of aggressiveness and risk of recurrence. It usually presents as an intraosseous mass, which may either be discovered during routine radiography or may produce symptoms of jaw swelling, pain, paresthesia, tooth mobility and displacement.
Although surgery remains the mainstay for the management of CGCG, it results in significant morbidity. Loss of bone during resection of the involved jawbone results in aesthetic and functional discrepancies.
Use of intralesional corticosteroid offers a conservative option for the management of these lesions. The procedure is simple and avoids the complications associated with surgical resection. However, long-term follow-up of the patient and periodic radiological assessment is of paramount importance to rule our recurrence and determine efficacy of intralesional corticosteroid therapy in the management of CGCG.
Footnotes
Contributors: KN and AD were involved in patient management. KN and RP were involved in manuscript writing.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Hebbale M, Giroh V, Mhapuskar A, et al. Aggressive central giant cell granuloma – a case series with literature review. J Indian Acad Oral Med Radiol 2019;31:171–5. 10.4103/jiaomr.jiaomr_45_19 [DOI] [Google Scholar]
- 2.Jacoway JR, Howell FV, Terry BC. Central giant cell granuloma: an alternative to surgical therapy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1988;66:572. [Google Scholar]
- 3.de Mendonça RP, Mitre GP, Real FH, et al. Central giant cell granuloma treated with intralesional corticosteroid injections and bisphosphonates: a long-term follow-up case study. Head Neck Pathol 2020;14:497–502. 10.1007/s12105-019-01053-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shirani G, Abbasi AJ, Mohebbi SZ, et al. Management of a locally invasive central giant cell granuloma (CGCG) of mandible: report of an extraordinary large case. J Craniomaxillofac Surg 2011;39:530–3. 10.1016/j.jcms.2010.10.018 [DOI] [PubMed] [Google Scholar]
- 5.Rasband-Lindquist AN, Lindquist JD, Larsen CG, et al. Nonsurgical options to treat giant-cell tumors of the head and neck: a case report and brief review of the literature. Ear Nose Throat J 2016;95:E29–34. [PubMed] [Google Scholar]
- 6.Barnes L, Eveson JW, Reichart P, et al. World Health organization classification of tumors. pathology genetics of head and neck tumors. IARC Press: Lyon, 2005. [Google Scholar]
- 7.De Lange J, Van den Akker HP. Clinical and radiological features of central giant-cell lesions of the jaw. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005;99:464–70. 10.1016/j.tripleo.2004.11.015 [DOI] [PubMed] [Google Scholar]
- 8.Vered M, Buchner A, Dayan D. Central giant cell granuloma of the jawbones--new insights into molecular biology with clinical implications on treatment approaches. Histol Histopathol 2008;23:1151–60. 10.14670/HH-23.1151 [DOI] [PubMed] [Google Scholar]
- 9.Kruse-Lösler B, Diallo R, Gaertner C, et al. Central giant cell granuloma of the jaws: a clinical, radiologic, and histopathologic study of 26 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006;101:346–54. 10.1016/j.tripleo.2005.02.060 [DOI] [PubMed] [Google Scholar]
- 10.Kaffe I, Ardekian L, Taicher S, et al. Radiologic features of central giant cell granuloma of the jaws. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1996;81:720–6. 10.1016/S1079-2104(96)80079-5 [DOI] [PubMed] [Google Scholar]
- 11.Chuong R, Kaban LB, Kozakewich H, et al. Central giant cell lesions of the jaws: a clinicopathologic study. J Oral Maxillofac Surg 1986;44:708–13. 10.1016/0278-2391(86)90040-6 [DOI] [PubMed] [Google Scholar]
- 12.Nilesh K, Vande AV, Tewary S, et al. Giant cell lesion and central giant cell granuloma of jaw: a brief review. AABS 2017;4:R22–9. [Google Scholar]
- 13.Bredell M, Rordorf T, Kroiss S, et al. Denosumab as a treatment alternative for central giant cell granuloma: a long-term retrospective cohort study. J Oral Maxillofac Surg 2018;76:775–84. 10.1016/j.joms.2017.09.013 [DOI] [PubMed] [Google Scholar]
- 14.da Silva NGJ, Carreira ASD, Pedreira EN, et al. Treatment of central giant cell lesions using bisphosphonates with intralesional corticosteroid injections. Head Face Med 2012;8:23. 10.1186/1746-160X-8-23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Carlos R, Sedano HO. Intralesional corticosteroids as an alternative treatment for central giant cell granuloma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002;93:161–6. 10.1067/moe.2002.119971 [DOI] [PubMed] [Google Scholar]
- 16.Terry B, Jacoway J. Management of central giant cell lesions: an alternative to surgical therapy. Oral Maxillofac Surg Clin N Am 1994;6:579–600. [Google Scholar]
- 17.Nogueira RLM, Teixeira RC, Cavalcante RB, et al. Intralesional injection of triamcinolone hexacetonide as an alternative treatment for central giant-cell granuloma in 21 cases. Int J Oral Maxillofac Surg 2010;39:1204–10. 10.1016/j.ijom.2010.06.015 [DOI] [PubMed] [Google Scholar]
- 18.Comert E, Turanli M, Ulu S. Oral and intralesional steroid therapy in giant cell granuloma. Acta Otolaryngol 2006;126:664–6. 10.1080/00016480500468976 [DOI] [PubMed] [Google Scholar]
- 19.El Hadidi YN, Ghanem AA, Helmy I. Injection of steroids intralesional in central giant cell granuloma cases (giant cell tumor): is it free of systemic complications or not? A case report. Int J Surg Case Rep 2015;8:166–70. 10.1016/j.ijscr.2015.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fonseca FP, Ribeiro ACP, Santos-Silva ARdos, et al. Fine needle aspiration cytology and intralesional steroid injection in a central giant cell granuloma affecting the gingiva: a new clinical approach. Braz Dent J 2013;24:420–7. 10.1590/0103-6440201302196 [DOI] [PubMed] [Google Scholar]
- 21.Rachmiel A, Emodi O, Sabo E, et al. Combined treatment of aggressive central giant cell granuloma in the lower jaw. J Craniomaxillofac Surg 2012;40:292–7. 10.1016/j.jcms.2011.04.002 [DOI] [PubMed] [Google Scholar]
- 22.Dolanmaz D, Esen A, Mihmanlı A, et al. Management of central giant cell granuloma of the jaws with intralesional steroid injection and review of the literature. Oral Maxillofac Surg 2016;20:203–9. 10.1007/s10006-015-0530-5 [DOI] [PubMed] [Google Scholar]