Abstract
Myocarditis is well known to be caused by viral infections such as Coxsackie virus group B, human herpes virus 6 and parvovirus B19. However, during the current emerging outbreak of SARS-CoV-2, there have been few case reports describing myocarditis as a possible presentation. In our case report we describe, early cardiac manifestations of SARS-CoV-2 in a UK District General Hospital. A 44-year-old Caucasian woman without any comorbidities presented with SARS-CoV-2 related fulminant myocarditis without initial respiratory symptoms. Patient underwent treatment with milrinone and methylprednisolone that showed reduction in myocardial inflammation and significantly improved myocardial contractility. This was then followed by a second phase of SARS-CoV-2 associated pneumonia and renal failure requiring ventilatory support and haemofiltration. Although, not described in the literature, we have found conjunctive use of milrinone and methylprednisolone effective in patient with SARS-CoV-2 fulminant myocarditis.
Keywords: cardiovascular medicine, cardiovascular system, adult intensive care, heart failure, pericardial disease
Background
Myocarditis is well known to be caused by viral infections such as Coxsackie virus group B, human herpes virus 6 and parvovirus B19. However, during the current emerging outbreak of SARS-CoV-2, there have been few case reports describing myocarditis as a possible presentation.1 2 In our case report we describe, early cardiac manifestations of SARS-CoV-2 in a UK District General Hospital.
Case presentation
A 44-year-old Caucasian woman without any previous co-morbidities, presented to the emergency department, with a 3-day history of febrile illness, lethargy, muscle aches and two episodes of syncope. These were not preceded by any warning symptoms and there was no family history of cardiovascular diseases.
She was care provider for a patient suffering from SARS-CoV-2 and had a nasopharyngeal swab specimen for SARS-CoV-2 taken a day before admission and the results were awaited. Despite being in close-contact with a SARS-CoV-2 positive individual, she had no respiratory symptoms on admission. On arrival to the emergency department, her oxygen saturation was 96% on air and blood pressure (BP) was 100/57 mm Hg. Physical examination revealed signs of peripheral hypoperfusion with normal pulmonary auscultation.
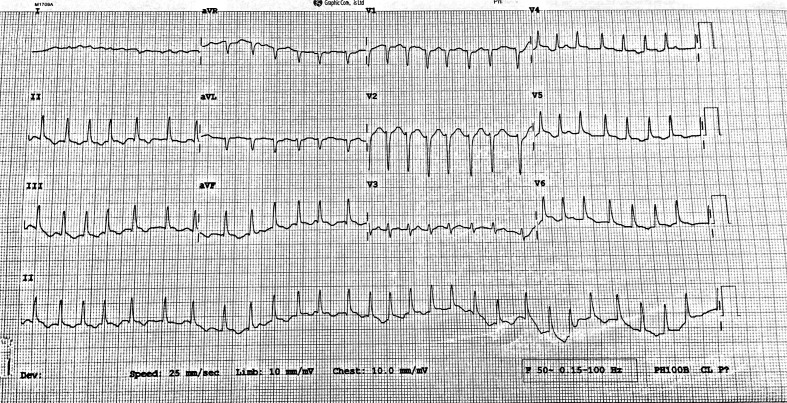
While she was in the emergency department, patient developed a presyncopal episode with hypotension (BP 85/40 mm Hg). A 12-lead ECG demonstrated atrial fibrillation with a ventricular rate of 177 bpm (figure 1) requiring DC cardioversion. This then reverted to sinus rhythm with no features to suggest myocardial ischaemia. The patient did not have chest pain throughout this illness and serial ECGs never identified myocardial ischaemia. Fluid resuscitation was commenced and the intensive care team was involved in the patient’s care.
Figure 1.
ECG shows atrial fibrillation with ventricular rate of 177 bpm.
Investigations
Laboratory investigations on admission revealed elevated high-sensitivity troponin I (639 ng/L), CK (1403 U/L), D-dimer (579 ng/mL), mild leucocytosis (15.8×109/L), lymphocytes (2.0×109/L), CRP (47 mg/L), creatinine (149 µmol/L), eGFR (33 mL/min/1.73 m2) and lactate of 7.1 mmol/L. CT of chest–abdomen–pelvis (figure 2) revealed 1 cm rim of pericardial fluid and minimal bi-basal lung inflammatory changes.
Figure 2.
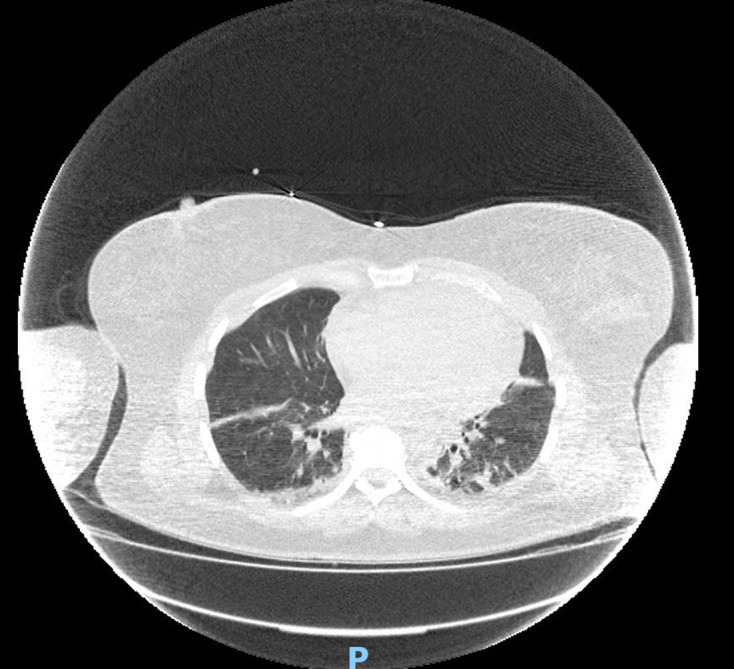
CT of chest–abdomen–pelvis shows minimal bi-basal lung parenchymal inflammatory changes.
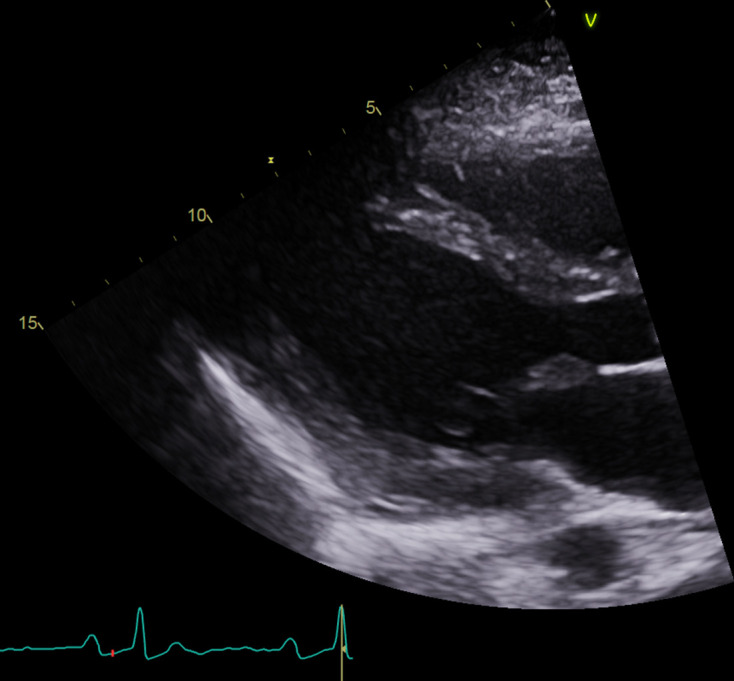
Bedside echocardiography (figure 3) demonstrated moderate concentric biventricular hypertrophy, diffused left ventricular hypokinesia with moderate to severe left-ventricular systolic dysfunction (estimated Ejection Fraction (EF) 37% by Simpsons) and pericardial effusion with no signs of tamponade. PCR for SARS-CoV-2 was positive in both nasopharyngeal swabs taken in the community and at the time of admission. Screening for enteroviruses and parvovirus B19 came back negative.
Figure 3.
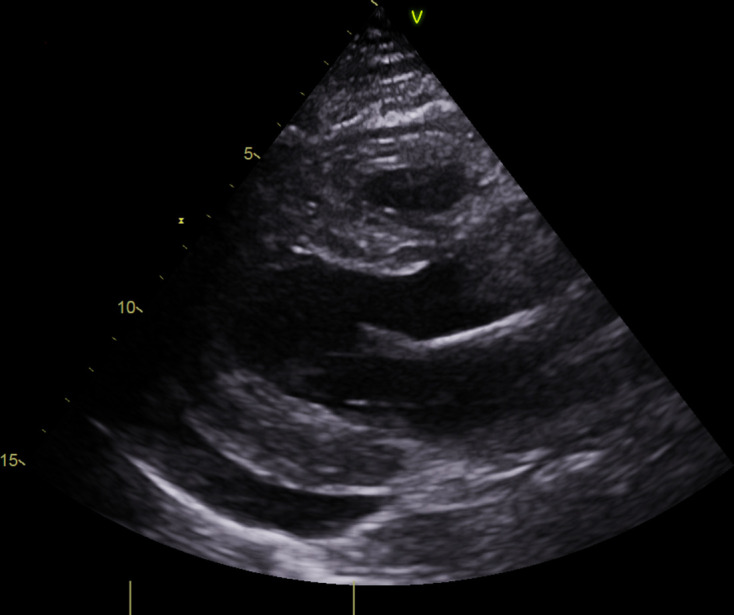
Bedside echocardiography shows moderate concentric biventricular hypertrophy with pericardial effusion.
Serial cardiac biomarkers showed steady decline in high-sensitivity troponin I from initial value of 639–309 ng/L on day 5 and 90 ng/L on day 18.
Moderate increase in inflammatory markers was observed by day 5 (CRP 126 mg/L, WCC 29.2×109/L) with subsequent decline over the course of treatment (CRP 84 mg/L, WCC 7.4×109/L on day 18). Lactate level improved from initial 7.1 mmol/L to 1.0 mmol/L on day 18.
Cardiac MRI was not feasible due to the patient’s critical condition and was deferred for a later date.
Differential diagnosis
Given the clinical picture was highly suggestive of myocarditis (fever, myocardial thickening, pericardial effusion and raised troponins), a diagnosis of SARS-CoV-2 related fulminant myocarditis was made. Echocardiographic findings were not consistent with Takotsubo’s cardiomyopathy (apical ballooning) and therefore this possibility was excluded.
Cardiac dysfunction is a known complication of severe sepsis and septic shock. Sepsis related oxidative stress leads to functional and structural failure of the cardiomyocytes, resulting in cardiac dysfunction. In this case, the level of CRP and WCC at the time of presentation was minimally elevated and there was no pulmonary involvement at the time of significant myocardial dysfunction. There was no clinical or laboratory evidence of overwhelming sepsis that could have lead to sepsis-related cardiomyopathy.
Type 2 myocardial infarction (MI) based on oxygen demand–supply mismatch can be one of the reasons for the elevated cardiac biomarkers. According to the Universal Definition of MI, the diagnosis of MI requires the rise and/or fall of cardiac biomarkers with clinical evidence of ischaemia, defined by symptoms, electrocardiographic changes, or new regional wall motion abnormalities. However, in this case there were no ECG changes consistent with ischaemia and echocardiography demonstrated global myocardial dysfunction rather than regional wall motion abnormalities. Coronary angiography was not performed due to low suspicion of acute coronary syndrome and patient’s haemodynamic instability.
Treatment
Treatment was started with methylprednisolone 1000 mg on the first day and 250 mg/day for the subsequent 2 days with the aim of reducing myocardial inflammation. Antiviral treatments like remdesvir and inflammation modulating immunosuppressive monoclonal antibodies such as tocilizumab were not employed in her care.
In the intensive care unit, patient developed cardiogenic shock with a BP of 60/40 mm Hg despite being on optimally titrated dobutamine infusion. ECG revealed atrial fibrillation with ventricular rate of 140 bpm and patient had signs of peripheral hypoperfusion despite being on inotropic support and amiodarone infusion. She had anuria with significant metabolic acidosis. The pH was 7.192 and had a base excess of −17.5 with partial respiratory compensation (PCO2 3.17; PO2 16.41 on 15 L via non-rebreather mask). Cardiac output monitoring was initiated and the cardiac index was calculated using a pulse contour cardiac output (PICCO) line and the Stewart-Hamilton equation. Patient was commenced on milrinone infusion at 0.375 µg/kg/min and norepinephrine infusion at 0.10–0.20 µg/kg/min was used as an adjunct in order to counteract the vasodilatory effect of milrinone. A loading dose of milrinone was avoided due to high risk of cardio-vascular systemic collapse. The milrinone dose was up-titrated according to clinical response to the maximal dose of 0.6 µg/kg/min. Acid–base balance improved (pH 7.375 with base excess of −9.4, PCO2 3.24; PO2 9.37 on 40% FiO2), though anuria persisted which prompted the initiation of haemofiltration.
Interval echocardiography done on the third day of admission showed normalisation of left ventricular systolic function with biventricular hypertrophy and a small pericardial effusion. By the end of the fourth day, cardiac index had improved from 1.8 to 4. Inotropic support was discontinued, and the patient remained in sinus rhythm. The patient’s oxygen requirement increased on the fifth day and was eventually intubated. Chest X-ray (figure 4) demonstrated bilateral patchy air space shadowing consistent with SARS-CoV-2 pneumonia. Antibiotics were commenced for superadded bacterial infection.
Figure 4.
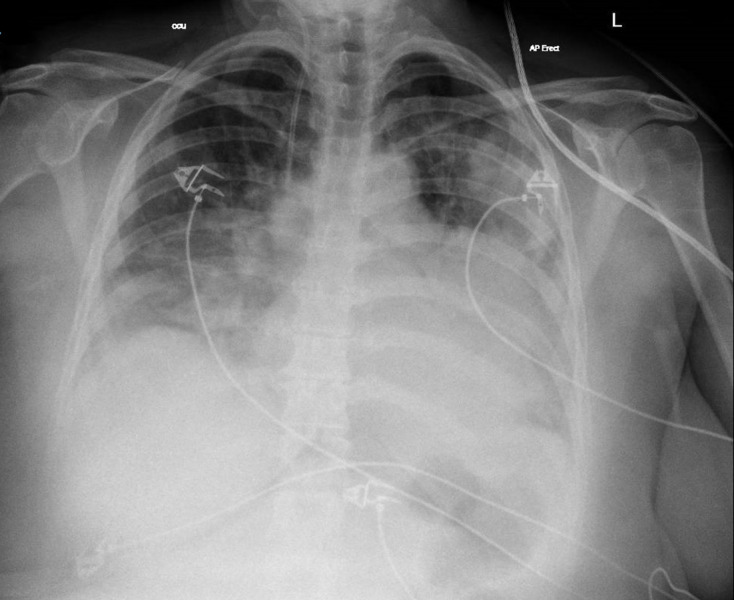
Chest X-ray shows bilateral patchy air space shadowing.
Outcome and follow-up
Interval echocardiography at 2 weeks (figure 5) demonstrated mild residual left ventricular posterior wall hypertrophy with complete resolution of right ventricular hypertrophy and preserved biventricular function. Improvement in respiratory support was observed by day 15 and tracheostomy was performed. Patient continued to improve and was finally discharged on day 41 after closure of her tracheostomy. Patient continues to recover at home.
Figure 5.
Interval echocardiography shows mild residual left ventricular posterior wall hypertrophy with complete resolution of right ventricular hypertrophy.
Due to full recovery of left ventricular (LV) systolic function, drugs which are used to prevent cardiac remodelling like ACE inhibitors and beta-blockers were not started.
Outpatient cardiac MRI has been arranged and cardiology follow-up appointment is booked at 1 month.
Discussion
Clinical presentation of SARS-CoV-2 mainly constitutes of respiratory symptoms. Presentation is, however, very heterogeneous. In our case we describe a predominant cardiac presentation of SARS-CoV-2 in the absence of respiratory symptoms at baseline. This emphasises the importance of having a low index of suspicion for this novel virus as being the underlying aetiology of acute fulminant myocarditis.
While uncommon, fulminant myocarditis is a malignant condition requiring rapid recognition and treatment due to high morbidity and mortality. Our patient had a clinical picture consistent with acute myocarditis with rapid deterioration leading to cardiogenic shock and need for inotropic support. This was followed by a second phase of typical SARS-CoV-2 pneumonia and renal failure. Normal biventricular function was regained within few days on milrinone and methylprednisolone treatment. Milrinone, a phosphodiesterase inhibitor that is selective for cAMP-specific cardiac receptors, is known to be used for acute heart failure resulting from systolic dysfunction secondary to infectious or toxic myocarditis.3 However, at present there is not enough literature of its use in SARS-CoV-2 myocarditis. Individual cases have been reported which show success of methylprednisolone in patients with SARS-CoV-2 myocarditis.4 Though, the use of methylprednisolone in conjunction with milrinone has not been described so far.
Patient’s perspective.
Regarding care, my mum states it was excellent. She says that during sedation she dreamt of half of the staff that was taking care of her. So when she was weaned off sedation she felt as if she knew the staff already despite not seeing them too much before. In her opinion, most of the staff in both units she was in were very caring and compassionate towards her. Initially, after being woken up from sedation she felt that she would be bed bound for life and a burden to the family and that made her feel depressed, but was reassured by staff that this will improve and that made her feel more positive. She feels like she was given a second chance at life. She also missed seeing the family and was aware that this was a difficult time for all of us. She would also like to pass her thanks to you and the rest of the staff for saving her life, and that no words can describe her gratitude for the chance to be with her family again.
I would say the biggest difficulty was the inability to see her during this time, and the feeling that we could not be there in person to support her was daunting. I guess seeing constant media reports of patients dying due to COVID-19 put additional strain on the family. I would also like to thank you and the rest of the staff for the care given and compassion shown to my mum. We are all glad to have her back home and to see that she is improving.
Learning points.
SARS-CoV-2 can present as fulminant myocarditis in absence of respiratory symptoms.
Echocardiography can play a crucial role in the diagnosis and Cardiac MRI (CMR) can be useful in confirmation of diagnosis.
Milrinone and methylprednisolone combination is a viable treatment option for SARS-CoV-2 myocarditis.
Footnotes
Contributors: TN—cardiology registrar—involved in patients care on admission. Involved in data collection, analysis, literature review, image collection article writing and proof reading. AK—internal medicine trainee—Involved in data collection, analysis, literature review, image collection, article writing and proof reading. NP—cardiology consultant in charge of patient care. Reviewed and selected echo images and edited the article. RO’L—ITU consultant in charge of patient care. Provided details of ongoing ITU management and care of the patient.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Doyen D, Moceri P, Ducreux D, et al. Myocarditis in a patient with COVID-19: a cause of raised troponin and ECG changes. The Lancet 2020;395:1516 10.1016/S0140-6736(20)30912-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kim I-C, Kim JY, Kim HA, et al. COVID-19-related myocarditis in a 21-year-old female patient. Eur Heart J 2020;41:ehaa288 10.1093/eurheartj/ehaa288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.DiBianco R. Acute positive inotropic intervention: the phosphodiesterase inhibitors. Am Heart J 1991;121:1871–5. 10.1016/0002-8703(91)90078-V [DOI] [PubMed] [Google Scholar]
- 4.Inciardi RM, Lupi L, Zaccone G, et al. Cardiac involvement in a patient with coronavirus disease 2019 (COVID-19). JAMA Cardiol 2020. 10.1001/jamacardio.2020.1096 [DOI] [PMC free article] [PubMed] [Google Scholar]