Highlights
-
•
Diagnosis of abdominal tuberculosis is challenging due to non-specific findings and clinical signs.
-
•
A high index of suspicion of abdominal tuberculosis should be kept especially in endemic areas and for immune compromised patients who present with non-specific abdominal symptoms.
-
•
Abdominal tuberculosis rarely presents as umbilical hernias with only 1 reported case in the literature.
-
•
Routine histopathologic examination of hernial sacs should be considered in high endemic areas of abdominal tuberculosis.
Keywords: Emergency surgery, Tuberculosis (TB), Paraumbilical hernia
Abstract
Introduction
Abdominal tuberculosis is a common form of extrapulmonary tuberculosis. Clinical manifestations and presentations are diverse depending on the organ involved within the abdominal cavity.
Presentation of case
26-year-old female with a background history of human immunodeficiency virus (HIV) presented with multiple irreducible para-umbilical hernias as the primary presentation of abdominal tuberculosis. Emergency hernia repair surgery revealed features of abdominal TB that was confirmed on polymerase chain reaction and histopathology. The patient was initiated on anti-tuberculosis therapy and was in a stable condition upon discharge.
Discussion
The uncommon presentation described is very rare with only one documented case of abdominal tuberculosis diagnosis with an umbilical hernia. Abdominal tuberculosis can present with a wide range of symptoms with a variety of imaging and invasive modalities available to confirm the diagnosis.
Conclusion
This case report is the second documented case of abdominal tuberculosis within a paraumbilical hernia. The case report highlights paucity within literature related to the histopathological diagnosis of hernial sacs within an endemic area of tuberculosis. Further research within hernia registries of the histopathological diagnosis of hernia sacs will be beneficial for surgeons in endemic areas of abdominal tuberculosis.
1. Introduction
Abdominal tuberculosis (TB) is a very common form of tuberculosis compromising around 5 percent of all cases of TB worldwide. It can present with involvement of any of the intra-abdominal organs which causes a wide range of clinical manifestations that can pose a diagnostic challenge. This case presented at a public healthcare facility within Sub-Saharan Africa. The presentation of abdominal tuberculosis at a as irreducible hernias is rare with few case reports documenting an incidental diagnosis of abdominal tuberculosis on hernial sacs [1]. This case report highlights the second documented case of abdominal tuberculosis within an umbilical hernia. The diagnosis of abdominal tuberculosis was confirmed on histopathology and the patient was started on anti-tuberculosis therapy. This case highlights the paucity within the literature related to routine PCR/histopathological analysis of hernial sacs within endemic area of abdominal tuberculosis. There is limited literature describing surgical management of abdominal tuberculosis within hernial sacs. This work has been reported in accordance to the Surgical Case Report (SCARE) guidelines [2].
2. Presentation of case
A 26-year-old female known with Human Immunodeficiency Virus (HIV) was referred from a peripheral clinic with a 6-day history of abdominal pain and multiple, irreducible, umbilical masses. This was preceded by a 6-month history of multiple, painless swellings around the umbilicus, that were previously reduced by the patient. No associated abdominal distension, weight-loss, reflux or change in bowel habits were noted. Background history revealed a diagnosis of HIV in 2013, with subsequent Anti-retroviral (ARV) initiation soon after. The patient reported good compliance and routine follow up, with no adverse incidents/reactions associated with ARV use. Alcohol, cigarette smoking, and alternative medication use were denied. Surgical history revealed a Pfannenstiel caesarean section performed in 2012. Although living in a high endemic area of pulmonary tuberculosis (TB), no contact history was forthcoming.
On examination, the patient appeared healthy, with a normal body mass index (BMI) and no obvious HIV associated stigmata. The patient was apyrexic, blood pressure and pulse recorded were within normal parameters. Abdominal examination revealed two tender irreducible para-umbilical hernias at 9 and 12’oclock in relation to the umbilicus. A Pfannenstiel incision scar was present, however, no abdominal distension, ascites, or masses were noted. Digital rectal examination revealed soft brown stools. Relevant systemic history and examination were unremarkable.
Relevant blood chemistry analysis demonstrated renal functions and electrolytes to be within normal parameters. A raised C-Reactive protein (CRP) 137 mg/L, with a low haemoglobin (Hb) 11.2 g/dL and normal white cell count (WCC) 4.60 × 109/L was noted. The patient's absolute CD4 count was 656 cells/uL and the HIV Viral Load 691 copies/mL respectively. Pre-operative chest X-ray was unremarkable.
The patient was diagnosed with two irreducible para-umbilical hernias and was consented for an emergency hernia repair by a specialist general surgeon and medical officer. A midline incision over the hernial sac was made however due to the substantial amount of herniated omentum, the incision was converted to a midline laparotomy. Upon laparotomy, intraoperative findings included 2 separate 1 cm defects at 9 and 12 o’clock in relation to the umbilicus. The herniated contents included thickened omentum adhered to the hernial sac. Furthermore, blood-stained peritoneal fluid, extensive lymphadenopathy and liver nodules were reported. Due to the intra-operative findings the peritoneal fluid, omental tissue and hernial sac were sent for histopathology. In lieu of contaminated surgical field
hernial defects repaired without mesh.
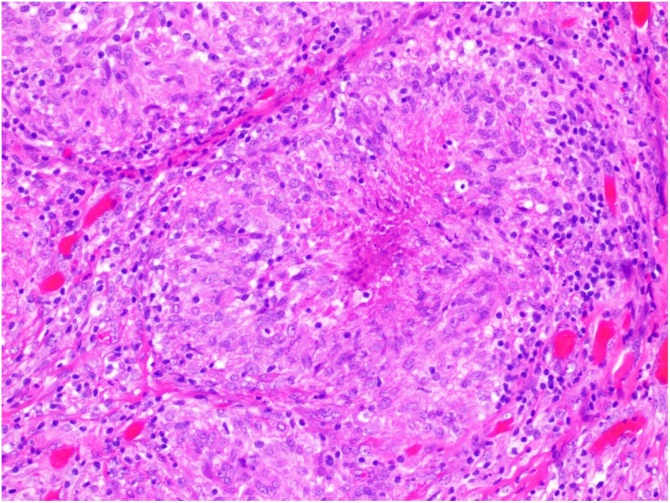
Polymerase chain reaction (PCR) results from both peritoneal fluid and omental tissue confirmed drug-sensitive M. tuberculosis and the patient was promptly initiated on antituberculous therapy. TB culture was positive, and histopathology confirmed the presence of caseous necrosis without acid-fast bacilli (Fig. 1.4 for Microscopy). Post-operative management was unremarkable and at discharge, no issues were raised by the patient. Although concerned about the unexpected diagnosis of abdominal tuberculosis, she received extensively education and counselling with regards to the illness. Routine anti-tuberculosis therapy was initiated and follow up was prescribed at specialist TB facility. The diagnosis of abdominal TB was not anticipated pre-operatively due to the atypical presentation and absence of applicable clinical findings.
Fig. 1.
H&E section demonstrating necrotising granulomatous inflammation (original magnification × 200).
3. Discussion
Abdominal tuberculosis (TB) is a very common form of tuberculosis compromising around 5 percent of all cases of TB worldwide. It can present with involvement of any of the following sites: peritoneum, oesophagus, stomach, intestinal tract, hepatobiliary tree, pancreas, perianal area, and lymph nodes. The most common forms of the disease include involvement of the peritoneum, intestine, and liver [1,3,4]. Reactivation of latent TB infection or ingestion of the mycobacteria from unpasteurized milk or undercooked meat can result in abdominal TB. Furthermore, hematogenous or contiguous spread from infected organs have also been implicated [1,3].
Abdominal tuberculosis can present in a myriad of different ways and often depends on the form of the disease. Vague, non-specific symptoms can be overlooked and lead to diagnostic difficulties. Clinical manifestations of abdominal TB depend on the form of the disease and may include fever, weight loss, abdominal pain and/or distension, ascites, hepatomegaly, diarrhoea, bowel obstruction, and intra-abdominal mass [5]. Most patients with tuberculous peritonitis have straw-coloured, lymphocytic ascites. Intestinal obstruction secondary to stricture formation is the most common complication, with long and multiple strictures often responding poorly to anti-tuberculous therapy and often require surgical intervention. Patients with biliary obstruction due to stricture may require biliary reconstruction. Risk factors for the development of abdominal TB include cirrhosis, HIV infection, diabetes mellitus, underlying malignancy, treatment with anti-tumour necrosis factor (TNF) agents, as well as the use of peritoneal dialysis [1].
There is scant literature describing abdominal hernias secondary to abdominal tuberculosis. Of the 12 case reports confirming abdominal TB in hernias, 11 of these were inguinal hernias. There is one case report confirming abdominal TB in the hernial sac of a 40-year-old patient with an umbilical hernia [6]. However, in aforementioned the diagnosis of tuberculosis was unexpected due to the unique presentation of the patient and was made because of the routine practice of sending all hernial sacs for histopathological examination [6].
Computed tomography (CT) is the preferred radiographic imaging modality for abdominal tuberculosis as it allows evaluation for the involvement of the liver and other organs as well. Findings are diverse and related to the organ involved: hepatic, intestinal or peritoneal; and include ascites, Lymphadenopathy with hypodense centres, thickening of the mesentery and omentum, and thickening of the peritoneum. Hepatic disease demonstrates multiple low-density micronodules dispersed throughout the liver, however, local hepatic TB can appear as solitary or multiple nodules [7]. Ultrasound is useful for detecting lymphadenopathy, ascites, peritoneal thickening, omental thickening, and bowel wall thickening which may be suggestive of abdominal tuberculosis [1,3].
Early diagnosis is imperative as abdominal tuberculosis in its varying forms can have the ultimately sinister complications of perforation, abscess, fistula, bleeding, and/or high-grade obstruction. This can result in serious morbidity and death [7]. The definite diagnosis of abdominal TB remains a demonstration of M. tuberculosis in peritoneal fluid or a biopsy specimen of an involved site (such as the peritoneum, intestine, or liver) via mycobacterial culture and/or nucleic acid amplification test (NAAT).
The sensitivity of AFB smear and mycobacterial culture for biopsy specimens is low (less than 50%). PCR is more sensitive and specific for the diagnosis of TB, and a quicker turnover time than cultures. The utility of PCR varies depending on the tissue type; sensitivity and specificity are high for peritoneal fluid and pancreatic and hepatic tissue, but intestinal tissue may be associated with false-positive PCR results. Stool PCR may be a useful adjunct for diagnosis. Histopathology is suggestive of tuberculosis but is not pathognomonic [5,7]. However, the sensitivity of AFB smear and mycobacterial culture for ascitic fluid is low, and the utility of ascitic fluid NAAT for diagnosis of tuberculous TB peritonitis has not been well established [8,9].
Laparoscopy, endoscopy and radiographic-guided interventions are frequently used tools for obtaining biopsy specimens, especially if ascites fluid is nondiag3nostic or absent. The approach to obtaining biopsy specimens should be tailored to the individual, site of involvement and associated risks and benefits [1,10]. Laparoscopy is useful for visualization of the peritoneum and peritoneal biopsy. Findings include thickened peritoneum, adhesions, a fibro adhesive pattern, enlarged lymph nodes, "violin-string" fibrinous strands, and omental thickening. Reported sensitivity and specificity of laparoscopic examination in one systematic review in making the diagnosis of peritoneal TB was as high as 93 and 98 percent, respectively [1,10]. Endoscopic findings of intestinal TB may include ulcers, strictures, nodules, pseudopolyps, fibrous bands, fistulas, and/or deformed ileocecal valve [11].
4. Conclusion
We present the second reported case of paraumbilical hernia secondary to abdominal tuberculosis without the classical clinical features of abdominal tuberculosis. Clinical diagnosis of abdominal TB is difficult and should be complemented by relevant radiological investigations preceding to a definitive diagnosis based on NAAT testing of the biopsy specimens. A high index of suspicion should be had for any patient with abdominal symptoms with risk factors for having tuberculosis. All patients with risk factors of developing abdominal tuberculosis should be medically investigated with thorough imaging and specimen to reach a diagnosis. Our rationale for operative management of this patient was based on the symptoms of an irreducible paraumbilical hernia. This case report highlights the need for a database for histopathological diagnoses of hernial sacs within endemic areas of TB that will serve as guideline for future cases.
Declaration of Competing Interest
The authors report no declarations of interest.
Sources of funding
There was no source of funding for this research. Any costs were covered by the authors.
Ethical approval
University of Free-State Health Sciences Research Ethics Committee have granted ethical clearance for this project.
Ethical clearance number: UFS-HSD2020/0673/3006.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
Mark Herbert Wellmann: Case Report concept, Case Report write-up, Literature review.
Hassan Ali Tariq: Case report design, Case report editing, Literature review.
Chantele De-Jager-Wood: Supervisor role, Editing of the case report.
Registration of research studies
N/A.
Guarantor
HA Tariq.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Contributor Information
Mark Herbert Wellmann, Email: mhwellmann@gmail.com.
Hassan Ali Tariq, Email: alitariq994@gmail.com.
Chantele De Jager-Wood, Email: crdejager001@gmail.com.
References
- 1.Rathi P., Gambhire P. Abdominal tuberculosis. J. Assoc. Phys. India. 2016;64:38–47. [online]. Available at: https://www.japi.org/february_2016/06_ra_abdominal_tuberculosis.pdf. (Accessed 1 May 2020) [PubMed] [Google Scholar]
- 2.Agha R.A., Borrelli M.R., Farwana R., Koshy K., Fowler A., Orgill D.P., For the SCARE Group The SCARE 2018 statement: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2018;60:132–136. doi: 10.1016/j.ijsu.2018.10.028. [DOI] [PubMed] [Google Scholar]
- 3.Debi U. Abdominal tuberculosis of the gastrointestinal tract: revisited. World J. Gastroenterol. 2014;20(40):14831. doi: 10.3748/wjg.v20.i40.14831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Evans R., Mourad M., Dvorkin L., Bramhall S. Hepatic and intra-abdominal tuberculosis: 2016 update. Curr. Infect. Dis. Rep. 2016;18(12) doi: 10.1007/s11908-016-0546-5. [DOI] [PubMed] [Google Scholar]
- 5.Ramadass B., Chittaranjan S., Subramanian V., Ramakrishna B. Fecal polymerase chain reaction for Mycobacterium tuberculosis IS6110 to distinguish Crohn’s disease from intestinal tuberculosis. Indian J. Gastroenterol. 2010;29(4):152–156. doi: 10.1007/s12664-010-0022-3. [DOI] [PubMed] [Google Scholar]
- 6.Datey S., Charles N., Vashishtha R., Patel S. Tuberculosis in the sac of paraumbilical hernia. J. Evol. Med. Dent. Sci. 2015;4(96):16201–16202. doi: 10.14260/jemds/2015/2381. [DOI] [Google Scholar]
- 7.Donoghue H., Holton J. Intestinal tuberculosis. Curr. Opin. Infect. Dis. 2009;22(5):490–496. doi: 10.1097/qco.0b013e3283306712. [DOI] [PubMed] [Google Scholar]
- 8.Al-Quorain A.A., Facharzt, Satti M.B. Abdominal tuberculosis in Saudi Arabia: a clinicopathological study of 65 cases. Am. J. Gastroenterol. 1993;88(Jan. (1)):75–79. [PubMed] [Google Scholar]
- 9.Marshall J.B. Tuberculosis of the gastrointestinal tract and peritoneum. Am. J. Gastroenterol. 1993;88:989. [PubMed] [Google Scholar]
- 10.Bhargava D.K., Shriniwas, Chopra P. Peritoneal tuberculosis: laparoscopic patterns and its diagnostic accuracy. Am. J. Gastroenterol. 1992;87:109. [PubMed] [Google Scholar]
- 11.Alvares J., Devarbhavi H., Makhija P., Rao S., Kottoor R. Clinical, colonoscopic, and histological profile of colonic tuberculosis in a tertiary hospital. Endoscopy. 2005;37(4):351–356. doi: 10.1055/s-2005-861116. [DOI] [PubMed] [Google Scholar]