Abstract
Background
Healthcare resources have been greatly limited by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic halting non-essential surgical cases without clear service expansion protocols.
Questions/Purposes
We sought to compare the peri-operative outcomes of patients undergoing spine surgery during the SARS-CoV-2 pandemic to a matched cohort prior to the pandemic.
Methods
We identified a consecutive sample of 127 adult patients undergoing spine surgery between March 9, 2020, and April 10, 2020, corresponding with the state of emergency declared in New York and the latest possible time for 1-month surgical follow-up. The study group was matched one-to-one based on age, gender, and body mass index with eligible control patients who underwent similar spine procedures prior to the SARS-CoV-2 outbreak. Surgeries performed for infectious or oncologic indications were excluded. Intra- and post-operative complication rates, re-operations, hospital length of stay, re-admissions, post-operative visit format, development of post-operative fever and/or respiratory symptoms, and SAR-CoV2 testing.
Results
A total of 254 patients (127 SARS-CoV-2 pandemic, 127 matched controls) were included. One hundred fifty-eight were male (62%), and 96 were female (38%). The mean age in the pandemic group was 59.8 ± 13.4 years; that of the matched controls was 60.3 ± 12.3. All patients underwent general anesthesia and did not require re-intubation. There were no significant differences in 1-month post-operative complication rates (16.5% pandemic vs. 12.6% control). There was one death in the pandemic group. No patients tested positive for the virus.
Conclusion
This study represents the first report of post-operative outcomes in a large group of spine surgical patients in an area heavily affected by the SARS-CoV-2 pandemic.
Electronic supplementary material
The online version of this article (10.1007/s11420-020-09797-x) contains supplementary material, which is available to authorized users.
Keywords: SARS-CoV-2, COVID-19, coronavirus, orthopedics, spine surgery, elective surgery, telemedicine
Introduction
Despite a plethora of editorials and expert opinions, scientific literature exploring the peri-operative outcomes of patients undergoing surgical procedures during the COVID-19 pandemic is sparse [2, 3, 7, 13, 17]. A single case series of 34 Chinese patients who developed pneumonia due to infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) shortly after elective surgery reported catastrophic results, with 44% needing intensive care and 20% not surviving [9]. However, this experience was in the incubation phase of the pandemic, when pre-operative patient screening, scrupulous use of personal protective equipment, and knowledge of critical risks factors for poor outcomes were not available. Tracking the peri-operative and post-operative course of patients undergoing essential, non-infectious, non-oncologic surgery in an epicenter of SARS-CoV-2 cases that was subject to detailed government-led restrictions on social distancing and travel restrictions could help medical institutions, local governments, and public health agencies better determine when to transition surgical care to non-emergent conditions [4, 5, 15].
Our tertiary referral center is located in New York City and has provided emergency orthopedic services to patients in the Northeastern USA. Due to the time-sensitive nature of certain spinal pathologies, the spine service has been the most active surgical service during this time, caring for patients presenting with progressive neurological deficits, myelopathy with cord at risk, spine trauma with instability, and cauda equina syndrome. The purpose of this study was to describe the peri-operative outcomes of patients undergoing spine surgery for spine pathology during the heights of the COVID-19 pandemic in New York City, including particular attention to the development of SARS-CoV-2 symptoms, post-operative complications, and patient monitoring following hospital discharge during the early post-operative period.
Patients and Methods
Following institutional review board approval, a retrospective, single-center study was performed to identify all patients undergoing spine surgery at a tertiary referral orthopedic hospital located in New York City from March 9 to April 10, 2020. The surgical dates were chosen specifically to correspond to the weeks in which a state of emergency was declared in New York State and the latest possible time by which a 1-month surgical follow-up of all patients was possible. This minimum follow-up requirement was chosen to cover the 14-day known typical incubation period of SARS-CoV-2 infection, whereby viral exposure can subsequently lead to manifestation of symptoms [18]. The surgical dates also encompass a period of time in which the institution (1) followed state directives to suspend elective surgery and instead utilize strict criteria to define essential surgical cases (Table 1), (2) dispensed personal protective equipment to medical personnel, (3) selectively performed post-admission SARS-CoV-2 testing (Cepheid Xpert Xpress SARS-CoV-2 RT-PCR, Sunnyvale, CA, USA) following patient assessment by a multidisciplinary team, (4) initiated a telehealth service for post-operative follow-up, and (5) began a progressively intensive patient screening process (Fig. 1).
Table 1.
Defining essential surgery at our institution
| All service lines | |
| Any infection, chronic or acute, requiring surgical intervention | |
| Any surgical wounds requiring surgical intervention | |
| Compartment syndrome | |
| Dislocation of native or prosthetic joint requiring reduction in the OR | |
| Malignant or benign tumors with impending fracture or neurovascular compromise | |
| Fractures (peri-prosthetic or native bone) | |
| Tendon injuries requiring surgical intervention | |
| Any loose body in the joint or displaced cartilage causing a locked joint | |
| Any injury to the lower extremity where the patient has an inability to bear weight or walk | |
| Any vascular or neurologic injuries | |
| Any injury where prompt intervention significantly improves outcomes | |
| Spine surgery | |
| Progressive weakness on physical exam or weakness with active denervation on EMG | |
| Myelopathy with cord at risk | |
| Fracture or trauma with spinal instability | |
| Cauda equina syndrome |
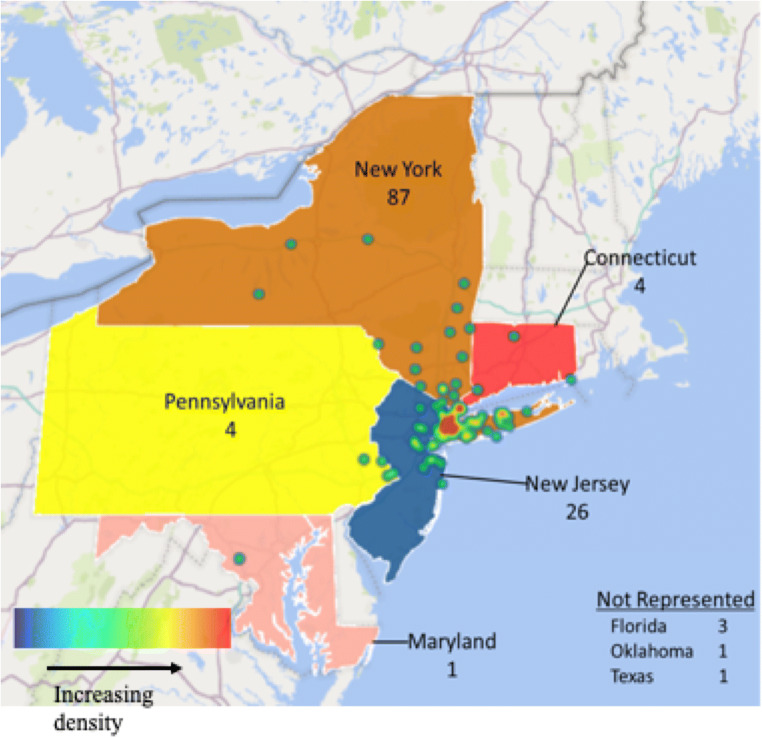
Fig. 1.
Heatmap representing primary residence of surgical patients. This heatmap depicts the location of the surgical patients’ primary residence. The numbers listed describe the number of patients who reside in that respective state. The greatest density of patients presented from downstate New York.
The study group was matched one-to-one with eligible control patients who underwent similar spine procedures for similar indications within our institution prior to the SARS-CoV-2 infection based on age, gender, and body mass index (BMI). Study exclusion criteria included patients with less than 2 weeks of follow-up and patients undergoing surgery for infectious or oncology-related reasons. The latter criterion was chosen to permit the study group to be more generalizable to elective surgical patients and to minimize confounding reasons for post-operative fever and thromboembolic complications [14].
Rationale for “Essential Surgery”
In the earliest phases of the COVID-19 pandemic in the USA (early March 2020), prevailing epidemiological models predicted that the number of critically ill patients would vastly exceed the number of intensive care unit (ICU) beds and ventilators available. In conjunction with the state government, New York State hospitals developed plans to create additional ICU beds and to limit elective surgery in order to prevent exposure to patients and healthcare workers and also to conserve resources (personal protective equipment, ventilators, ICU beds) for the anticipated wave of critically ill patients. Recognizing not only that the pandemic would likely preclude elective surgery for several months, but also that delay of surgical treatment for several months could result in permanent disability or neurological impairment in a subset of spine surgery patients, the following “essential surgery” criteria were determined: progressive weakness on exam or weakness with active denervation on electromyography, myelopathy with cord at risk, fracture or trauma with spinal instability, or cauda equina syndrome (Table 1). Of note, New York State banned elective surgery on March 25, 2020; thus, our hospital suspended elective surgery 9 days prior to the state’s mandate.
Screening Protocol
Scheduled patients underwent a brief pre-operative phone screen, which consisted of 2 major points: (1) asking patients if they were known to have SARS-CoV-2 and (2) a review of symptoms within the last 2 weeks including fever, cough, shortness of breath, sore throat, loss of taste/smell, myalgias, or abdominal pain/diarrhea. In person, patients underwent oxygen saturation measurement on room air and a temperature check. If there was concern that a patient had SARS-CoV-2, the patient was promptly placed on the appropriate isolation precautions and tested according to clinical impression.
Data Collection
Pre-operative patient demographics including age, gender, and body mass index were collected, as well as indicators of relevant comorbidities, including their American Society for Anesthesiology (ASA) score and Charlson comorbidity index (CCI) score. The zip code, city, county, and state of the patients’ primary residence were collected to determine their geographic distribution and if they resided within counties with over twelve thousand reported SARS-CoV-2 cases within their respective state. These counties included the seven highest in New York (Bronx, Kings, Manhattan, Nassau, Suffolk, Queens, Westchester) and five highest in New Jersey (Bergen, Essex, Hudson, Middlesex, Passaic, Union). Pre-operatively, surgical indications and the status of the patient upon presentation for surgery, including specific indicators of possible viral pneumonia (presence of fever, abnormal acute findings on chest radiographs), were recorded. Surgical data included the operative procedure/levels, operative time, and the occurrence of any intra-operative complications.
Post-operatively, the presence of a fever (temperature > 38.1°C), the number of fever readings, the subsequent medical workup, and SARS-CoV-2 viral testing were recorded. Inpatient complications, necessity for blood transfusions, and length of stay were recorded. Following discharge from the hospital, all post-operative encounters between patients and medical personnel were analyzed, with the type of encounter (in-person, telephone call, scheduled telehealth visit) and if common symptoms concerning for SARS-CoV-2 infection (fever, cough, shortness of breath, new myalgias or arthralgias unrelated to the surgical site, and loss of taste or smell) were discussed. Admission to any hospital and any re-operations within the follow-up period were also recorded.
Statistical Analysis
Univariate comparisons were performed between patients operated during the pandemic versus historical controls. Furthermore, a subgroup comparison was performed among pandemic study patients who underwent surgery before versus after the suspension of elective procedures. Continuous variables were assessed for normality using the Kolmogorov-Smirnov test, with unpaired 2-tailed t tests and Mann-Whitney tests used where appropriate (SigmaPlot, San Jose, CA, USA). Categorical variables were compared using the χ-square test. p values of less than 0.05 for associations were considered to indicate statistical significance. All analyses were reviewed with a statistician. A geographic heatmap of study patients was generated using the 3D map function in Microsoft Excel (Redmond, WA, USA) 2016.
Results
A total of 146 patients underwent spine surgery within the specified dates during the COVID-19 pandemic, with 127 meeting criteria for study inclusion. Of the qualifying patients, 112 (88%) resided in counties with the highest number of SARS-CoV-2 within their respective state, comprising downstate New York and eastern New Jersey (Fig. 1). The historical control group consisted of 127 patients. There was no significant difference in age (59.8 ± 13.4 vs. 60.3 ± 12.3 years; p = 0.800), gender (79:48 male:female vs. 79:48; p = 0.263), and BMI (29.1 ± 5.2 vs. 29.1 ± 4.8; p = 0.685) between the pandemic-period patients and the historical control, respectively (Table 2). Additionally, the ASA scores, CCI scores, indications for surgery, and surgical procedure were similar between the two groups (p = 0.764, 0.823, 0.530, 0.645, respectively).
Table 2.
Patient demographics and surgical indications
| Operated during pandemic (mean ± standard deviation) | Historical cohort | p value | |
|---|---|---|---|
| N | 127 | 127 | - |
| Age (years) | 59.8 ± 13.4 | 60.3 ± 12.3 | 0.917 |
| Gender (male:female) | 79:48 | 79:48 | 0.263 |
| BMI | 29.1 ± 5.2 | 29.1 ± 4.8 | 0.809 |
| ASA score | 2.1 ± 0.4 | 2.1 ± 0.4 | 0.764 |
| Charlson comorbidity score | 1.6 ± 1.6 | 1.5 ± 1.1 | 0.823 |
| Indication for surgery | 0.530 | ||
| Intractable pain | 116 | 116 | |
| Sensory deficit | 87 | 83 | |
| Motor weakness (radicular) | 64 | 63 | |
| Myelopathy | 19 | 15 |
The distribution of surgical procedures that comprised each group was similar as lumbar decompression/discectomies (32.3% SARS-CoV-2 period vs. 34.6% control) were the most common procedures, while anterior cervical surgeries (28.3% vs. 29.9%) and lumbar fusions (25.2% vs. 32.3%) were the second and third most common, respectively (p = 0.645; Table 3). Operative durations were similar between both groups of patients (2 h 42 min ± 1 h 29 min SARS-CoV-2 vs. 2 h 38 min ± 1 h 46 min; p = 0.273). There were 5 reported intra-operative complications (all durotomies) in the pandemic group and 8 intra-operative complications (all durotomies) in the control group. All patients underwent general anesthesia and did not require re-intubation. There were no differences in post-operative complication rates within the 1-month following surgery (16.5% SARS-CoV-2 period vs. 12.6% control; p = 0.464). Of note, there was one death in the pandemic period. Approximately 10 days following a L4–5 posterior decompression and fusion for cauda equina syndrome, the 94-year-old patient developed fevers at home. Given the high risk of SARS-CoV-2 exposure in the local emergency departments (ED), the patient was recommended against presenting to the ED. Four days later, the patient passed away at home, without formal SARS-CoV-2 viral testing. There were no reported deaths in the historical control group.
Table 3.
Peri-operative outcomes
| Operated during pandemic (mean ± standard deviation) | Historical cohort | p value | |
|---|---|---|---|
| Type of surgery | < 0.01* | ||
| Ambulatory | 12 | 14 | |
| Inpatient | 115 | 113 | |
| Location of surgery | 0.935 | ||
| Cervical | 43 | 42 | |
| Thoracic | 2 | 4 | |
| Thoracolumbar | 82 | 81 | |
| Surgical procedures | 0.645 | ||
| Lumbar decompression/discectomy | 41 | 44 | |
| ACDF/CDR | 36 | 38 | |
| Lumbar fusion | 32 | 41 | |
| Posterior cervical surgery | 7 | 7 | |
| Other | 11 | 7 | |
| Surgical duration (h:min) | 2:42 ± 1:29 | 2:38 ± 1:46 | 0.273 |
| Intra-operative complications (total) | 5 | 8 | 0.419 |
| Post-operative complications | 21 | 16 | 0.464 |
| Dysphagia | 7 | 3 | |
| New-onset motor weakness | 4 | 4 | |
| Wound drainage | 3 | 0 | |
| New-onset atrial fibrillation | 2 | 1 | |
| Urinary tract infection | 2 | 4 | |
| Pulmonary embolism | 1 | 0 | |
| Pneumonia | 1 | 2 | |
| Hematoma | 0 | 1 | |
| Ileus | 0 | 1 | |
| Death | 1 | 0 |
Following surgery, the length of hospitalization was similar between both groups (3.1 ± 4.2 days SARS-CoV-2 period vs. 2.6 ± 3.0 days control; p = 0.540) (Table 4). There were significant differences in the format of post-operative visits (p < 0.01). In total, 80 patients (63.0%) in the pandemic group underwent formal telehealth visits, while only 3 patients (2.4%) underwent in-person visits. In contrast, no patients in the historical control group participated in formal telehealth visits and 117 (96.7%) returned for in-person post-operative visits.
Table 4.
Post-operative outcomes
| Operated during pandemic (mean ± standard deviation) | Historical cohort | p value | |
|---|---|---|---|
| Length of stay (days) | 3.1 ± 4.2 | 2.6 ± 3.0 | 0.540 |
| Follow-up post-discharge | |||
| Formal telemedicine visit | 80 | 0 | 1.0 |
| Telephone call | 127 | 127 | |
| In-person visit | 3 | 121 | |
| Tested for COVID: COVID +ve | 1.0 | ||
| In-hospital: positive | 8:0 | 0:0 | |
| Following discharge: positive | 3:0 | 0:0 | |
| Fever | 0.680 | ||
| In-hospital: COVID +ve | 9:0 | 5:0 | |
| Post-discharge: COVID +ve | 8:0 | 2:0 | |
| Respiratory symptoms | 0.111 | ||
| In-hospital: COVID +ve | 2:0 | 1:0 | |
| Post-discharge: COVID +ve | 3:0 | 0:0 | |
| Required blood transfusion post-operatively | 4 | 10 | |
| Re-admission within 30 days | 3 | 7 | 0.057 |
| Re-operation within 30 days | 3 | 5 | 0.327 |
| Mortality within 30 days | 1 | 0 | - |
No patients during the SARS-CoV-2 period who were tested for SARS-CoV-2 (8 inpatient and 3 post-discharge) tested positive, and no patients in the historical control underwent viral testing. Similar findings were observed with the development of a fever (9 inpatient and 8 post-discharge [SARS-CoV-2 period] vs. 5 inpatient and 2 post-discharge; p = 0.680) and respiratory symptoms (2 inpatient and 3 post-discharge [SARS-CoV-2 period] vs. 1 inpatient and 0 post-discharge [historical control]; p = 0.111). However, given the small number of patients presenting with respiratory symptoms, our findings do show a trend towards an increased incidence of post-operative respiratory symptoms in the pandemic group (Fig. 2).
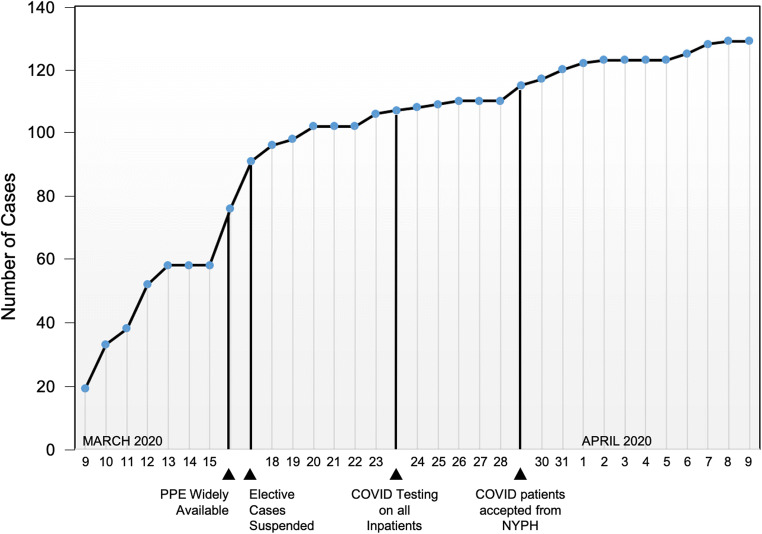
Fig. 2.
Surgical volume and pertinent milestones during the pandemic. The graph represents cumulative surgical volume over the study period. Specific milestones are described and marked by a vertical line. On March 16, 2020, PPE became widely available for all hospital staff. The next day on March 17, the hospital suspended all elective surgeries. On March 23, COVID-19 testing became available for all inpatients and operative patients. Lastly on March 29, our hospital began accepting COVID-19-positive patients from a nearby hospital.
The historical control patients presented with a greater number of re-admissions within 30 days (7 vs. 1; p = 0.057), but there was no significant difference in re-operation rates between groups (p = 0.348). Three patients in the pandemic group required a re-operation within 30 days of surgery. One patient underwent surgery to revise a medial pedicle screw breach resulting in L5 motor weakness. The second patient underwent an irrigation and debridement (I&D) of a lumbar spine hematoma, and the last patient underwent revision decompression for an acute recurrent disc herniation following a single-level lumbar decompression surgery. In the historical control, 5 patients required re-operation. Two patients experienced radicular symptoms from an epidural hematoma, which required an irrigation and debridement of the lumbar spine, and 2 patients presented with acute recurrent lumbar disc herniations, which necessitated revision decompression surgeries. The final re-operation in the historical group was a patient who developed an abscess in the neck following an ACDF (without evidence of esophageal perforation), which required a cervical irrigation and debridement.
When comparing surgical cases performed before (76 cases) and after (51 cases) the suspension of elective cases, there was a significant decline in the number of cases performed per day, indicating surgeon adherence to institutional guidelines (12.6 ± 5.9 vs. 3.0 ± 2.9 cases per day, p < 0.01). Furthermore, we identified no difference in patient demographics (age, p = 0.248; gender, p = 0.876; BMI, p = 0.465; ASA, p = 0.304; CCI, p = 0.50), peri-operative characteristics (surgical time, p = 0.404; post-operative complications, p = 0.989), or post-operative course (length of stay, p = 0.909; post-operative fever, p = 0.989; re-operations, p = 1.0).
Discussion
Despite rigorous efforts of containment and quarantine, the incidence of SARS-CoV-2 continues to steadily rise globally [18]. Although viral titers and antibody testing are becoming available across several countries, it remains unclear if patients who (1) actively have SARS-CoV-2 infection, (2) have recovered and do or do not have high circulating antibody titers, or (3) have not yet been exposed are at an increased risk for developing peri-operative or post-operative complications. In fact, to date extremely limited outcome data of any kind on patients undergoing surgery during the pandemic is available, making it difficult for physicians and institutions to determine how to stratify patient risk factors when providing surgical services. This study is the first to describe the in-hospital course and short-term outcomes of over one hundred patients living in the global epicenter of SARS-CoV-2 who underwent spine surgery for essential spine pathologies. With pre-operative viral testing not being available for the majority of the study period, our study cohort was mostly screened using clinically based parameters—a simple questionnaire regarding recent respiratory symptoms, temperature measurements on hospital presentation, and a pre-operative chest X-ray. With this combination of (1) a simplified screening process, (2) clear indications for essential surgery, (3) inpatient isolation protocols, (4) viral testing based on clinical impression, and (5) discharge instructions that emphasized social distancing with close telephone/telehealth follow-up, we found that patients operated on during the pandemic did not have a significantly higher risk of peri-operative complications including post-operative fever and/or respiratory distress compared with a carefully matched pre-pandemic group.
We acknowledge limitations in this study. Despite a strong likelihood of patients being infected with SARS-CoV-2, the lack of formal viral testing prior to surgery makes it impossible for us to verify this claim. There were likely asymptomatic SARS-CoV-2-positive patients in the cohort, but the number of these is difficult to quantify, similar to the general public. Post-discharge symptoms were self-reported by patients at the time of telemedicine or telephone interactions, meaning it was not possible to verify if SARS-CoV-2-related symptoms such as fever or hypoxia were truly occurring. This finding reinforces several consensus documents which recommend that surgery be deferred in such high-risk groups [6, 10]. Despite this, most patients returned home to counties with a “high” number of SARS-CoV-2-positive individuals and have done well overall with proper instruction and communication in the first month after surgery. Lastly, our cohort sizes may be small to detect significant differences in post-operative complications; however, given this public health crisis and government mandates, we were limited to treating patients who met essential requirements for surgery.
The mortality we describe occurred in a healthy 94-year-old man who had developed cauda equina syndrome. The posterior decompression and fusion for cauda equina syndrome was performed without complication. Prior to the onset of fever 10 days after surgery, he had been progressing well. Although we did not observe any statistical difference in post-operative complications, the presence of a SARS-CoV-2-related mortality in our study cohort is a pertinent finding that does highlight the known risk association of age as well as comorbidity profile with serious illness secondary to viral infection [8, 19].
Two-thirds of our study cohort presented from counties that have the highest number of SARS-CoV-2 cases, making it highly likely that more than one patient underwent surgery while being actively infected with the virus. Although very recently published consensus statements have emphasized that all patients undergoing surgery should be screening for SARS-CoV-2, the non-significant differences in the post-operative course of our study cohort question the relevance of viral screening in asymptomatic patients who are clinically well, but require urgent surgery. Furthermore, given the likelihood of study patients having undetected viral disease, our inability to find a higher incidence of post-operative pulmonary complications despite vigorous inflammatory provocation (general anesthesia and surgery) encourages future research on the “cytokine storm” associated with SARS-CoV-2 infection and the likelihood to occur post-operatively [12]. Although future investigations involving pre-operative viral testing will clarify this question, our study findings suggest that pre-surgical clinical status and patient comorbidity status are important predictors of post-operative performance rather than pre-operative viral status alone.
Our study has also demonstrated that close outpatient surveillance through telephone and telemedicine follow-up is safe and effectively avoids putting patients at risk of SARS-CoV-2 exposure by returning to the hospital. Although telemedicine has been previously shown to be cost-effective, its utility in the context of a pandemic is now clear [1, 11]. Although virtual visits for new patients require modified physical examination techniques and pre-visit patient instructions, the capability to evaluate surgical wounds, respiratory symptoms, and a patient’s general status make this interaction modality an essential tool that should be utilized across the surgical subspecialties for post-operative care [16].
In conclusion, this study represents the first report of post-operative outcomes in a large group of patients in an area heavily affected by the COVID-19 pandemic. Our findings illustrate the challenges that institutions face in providing surgical care during a pandemic, and directly demonstrate how innovative interventions (such as telemedicine and patient education regarding social distancing and symptom reporting) can maximize patient safety following surgery.
Electronic supplementary material
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1225 kb)
(PDF 1224 kb)
(PDF 1224 kb)
Compliance with Ethical Standards
Conflict of Interest
Philip K. Louie, MD; Lauren A. Barber, MD; Kyle W. Morse, MD; Marie Syku, BS; Virginie Lafage, PhD; Russel C. Huang, MD; and Alberto V. Carli, MD, declare that they have no conflicts of interest. Sheeraz A. Qureshi, MD, MBA, reports personal fees from Stryker K2M, Globus Medical, Inc., Paradigm Spine, RTI Surgical Inc., AMOpportunities, Healthgrades, and Simplify Medical, Inc.; investment or ownership interest in Avaz Surgical and Vital 5; committee or board membership in the International Society for the Advancement of Spine Surgery, Global Spine Journal, The American Orthopaedic Association, North American Spine Society, LifeLink.com Inc., Association of Bone and Joint Surgeons, Society of Lateral Access, Spine (Journal), The Spine Journal, Society of Minimally Invasive Spine Surgery, Minimally Invasive Spine Study Group, Spinal Simplicity, LLC, Contemporary Spine Surgery, Annals of Translational Medicine, Journal of American Academy of Orthopaedic Surgeons, and Cervical Spine Research Society, outside the submitted work.
Human/Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013.
Informed Consent
Informed consent was waived from all patients for being included in this study.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Footnotes
Level of Evidence: Level III: Therapeutic Study
References
- 1.Buvik A, Bergmo TS, Bugge E, Smaabrekke A, Wilsgaard T, Olsen JA. Cost-Effectiveness of Telemedicine in Remote Orthopedic Consultations: Randomized Controlled Trial. J Med Internet Res. 2019;21(2):e11330. doi: 10.2196/11330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Coccolini F, Perrone G, Chiarugi M, Di Marzo F, Ansaloni L, Scandroglio I, et al. Surgery in COVID-19 patients: operational directives. World J Emerg Surg. 2020;15(1):1–7. doi: 10.1186/s13017-019-0285-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Coimbra R, Edwards S, Kurihara H, Bass GA, Balogh ZJ, Tilsed J, et al. European Society of Trauma and Emergency Surgery (ESTES) recommendations for trauma and emergency surgery preparation during times of COVID-19 infection. Eur J Trauma Emerg Surg. 2020. 10.1007/s00068-020-01364-7 [DOI] [PMC free article] [PubMed]
- 4.Collaborative C. Global guidance for surgical care during the COVID-19 pandemic. Br J Surg. 2020. 10.1002/bjs.11646 [DOI] [PMC free article] [PubMed]
- 5.de Caro F, Hirschmann TM, Verdonk P. Returning to orthopaedic business as usual after COVID-19: strategies and options. Knee Surg Sports Traumatol Arthrosc. 2020. 10.1007/s00167-020-06031-3
- 6.Diaz A, Sarac BA, Schoenbrunner AR, Janis JE, Pawlik TM. Elective surgery in the time of COVID-19. Am J Surg. 2020. 10.1016/j.amjsurg.2020.04.014 [DOI] [PMC free article] [PubMed]
- 7.Givi B, Schiff BA, Chinn SB, Clayburgh D, Iyer NG, Jalisi S, et al. Safety recommendations for evaluation and surgery of the head and neck during the COVID-19 pandemic. JAMA Otolaryngol Head Neck Surg. 2020. 10.1001/jamaoto.2020.0780 [DOI] [PubMed]
- 8.Gold JA, Wong KK, Szablewski CM, Patel PR, Rossow J, da Silva J, et al. Characteristics and Clinical Outcomes of Adult Patients Hospitalized with COVID-19—Georgia, March 2020. MMWR Morb Mortal Wkly Rep. 2020;69(18):545–550. doi: 10.15585/mmwr.mm6918e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lei S, Jiang F, Su W, Chen C, Chen J, Mei W, et al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClinicalMedicine. 2020. 10.1016/j.eclinm.2020.100331 [DOI] [PMC free article] [PubMed]
- 10.Parvizi J, Gehrke T, Krueger CA, Chisari E, Citak M, Van Onsem S, et al. Resuming Elective Orthopaedic Surgery During the COVID-19 Pandemic: Guidelines Developed by the International Consensus Group (ICM). J Bone Joint Surg Am. In press. [DOI] [PMC free article] [PubMed]
- 11.Pastora-Bernal JM, Martín-Valero R, Barón-López FJ, Estebanez-Pérez MJ. Evidence of Benefit of Telerehabitation After Orthopedic Surgery: A Systematic Review. Journal Med Internet Res. 2017;19(4):e142. doi: 10.2196/jmir.6836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ruscitti P, Berardicurti O, Iagnocco A, Giacomelli R. Cytokine storm syndrome in severe COVID-19. Autoimmun Rev. 2020. 10.1016/j.autrev.2020.102562 [DOI] [PMC free article] [PubMed]
- 13.Sarac NJ, Sarac BA, Schoenbrunner AR, Janis JE, Harrison RK, Phieffer LS, et al. A Review of State Guidelines for Elective Orthopaedic Procedures During the COVID-19 Outbreak. J Bone Joint Surg Am. 2020. doi:10.2106/JBJS.20.00510 [DOI] [PMC free article] [PubMed]
- 14.Seo J, Park JH, Song EH, Lee YS, Jung SK, Jeon SR, et al. Post-operative Nonpathologic Fever After Spinal Surgery: Incidence and Risk Factor Analysis. World Neurosurg. 2017;103:78–83. doi: 10.1016/j.wneu.2017.03.119. [DOI] [PubMed] [Google Scholar]
- 15.Stahel PF. How to risk-stratify elective surgery during the COVID-19 pandemic? Patient Saf Surg. 2020;14:8. doi: 10.1186/s13037-020-00235-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tanaka MJ, Oh LS, Martin SD, Berkson EM. Telemedicine in the Era of COVID-19: The Virtual Orthopaedic Examination. J Bone Joint Surg Am. 2020. doi:10.2106/JBJS.20.00609 [DOI] [PMC free article] [PubMed]
- 17.Topf MC, Shenson JA, Holsinger FC, Wald SH, Cianfichi LJ, Rosenthal EL, et al. A framework for prioritizing head and neck surgery during the COVID-19 pandemic. Head Neck. 2020. doi:10.1002/hed.26184 [DOI] [PMC free article] [PubMed]
- 18.US Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19). Available at: https://www.cdc.gov/coronavirus/2019-ncov/index.html. Accessed 3 May 2020.
- 19.Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1225 kb)
(PDF 1224 kb)
(PDF 1224 kb)