Highlights
-
•
Aloe extract inhibits PEDV replication in Vero and IPEC-J2 cells in vitro.
-
•
Aloe extract can inactivate PEDV virions directly.
-
•
Oral administration of Aloe extract can protect newborn piglets against PEDV infection in vivo.
Keywords: Porcine epidemic diarrhea virus (PEDV), Aloe extract, Antiviral activity, Swine
Abstract
Porcine epidemic diarrhea virus (PEDV) causes severe diarrhoea and high mortality in neonatal suckling piglets, leading to significant economic losses to the swine industry. Currently there are no adequate control strategies against circulating PEDV variants, making an urgent need to exploit effect antiviral therapies to compensate for vaccines. Here, we report that Aloe extract can hamper completely the proliferation of PEDV at a non-cytotoxic concentration of 16 mg/mL determined by CCK-8 assay in Vero and IPEC-J2 cells in vitro. Furthermore, time course analysis indicated the extract exerted its inhibition at the late stage of the viral life cycle. Moreover, we also confirmed that the extract can inactivated PEDV directly but did not act on the viral genome and S1 protein. Importantly, the extract at a relatively safety concentration of 100 mg/kg of body weight, which was confirmed in mice, could reduce virus load and pathological change in intestinal tract of pigs and protect newborn piglets from lethal challenge with highly pathogenic PEDV variant GDS01 infection, indicating that Aloe extract efficiently inhibited PEDV infection in vivo. Collectively, our findings suggest that the aqueous extract from the Aloe could inhibit PEDV replication in vitro and in vivo and might be a good target for drug development against PEDV.
1. Introduction
Porcine epidemic diarrhea (PED) caused by Porcine epidemic diarrhea virus (PEDV), is one of the most important disease in the swine industry. PEDV belongs to the genus Alphacoronavirus of the family Coronaviridae (Pensaert and Bouck, 1978), which also includes Transmissible gastroenteritis virus (TGEV) (Doyle and Hutchings, 1946), Porcine deltacoronavirus (PDCoV) (Woo et al., 2012) and Porcine enteric alphacoronavirus (PEAV) (Lang et al., 2017). PEDV genome is an enveloped, single-stranded, positive-sense RNA virus, which is approximately 28 kb in length, and arranged in the order of: 5' UTR-ORF1a/1b-S-ORF3-E-M-N-3' UTR, encoding 16 non-structural proteins and 4 structural proteins (Kocherhans et al., 2001; Song and Park, 2012). It is known that the S protein, which can be divided into domain 1 (S1) and domain 2 (S2), has many important characteristics in coronaviruses (CoVs), such as virus attachment and entry, and induction of neutralizing antibodies in vivo (Wen et al., 2018). PEDV can cause severe watery diarrhea with subsequent dehydration in pigs of all ages, and a high mortality rate in 7-10-day-old suckling piglets (Li et al., 2012; Pijpers et al., 1993; Stevenson et al., 2013). Since PED was first reported in Belgium in 1978, this disease spreaded soon to other regions in Europe and Asia (Pensaert and Bouck, 1978; Song and Park, 2012). Recently, there have been devastating outbreaks of PEDV variants in China and United States, which is characterized by high death rates among infected suckling piglets, result in substantial economic losses to the swine industry (Sun et al., 2016; Vlasova et al., 2014).
To combat the virus, great efforts have been made to prevent and control PEDV since the variants emerged. For virus infection prevention, the administration of vaccines is one of important tool. Currently a number of vaccines including killed, live-attenuated vaccine, recombinant vector vaccine, DNA vaccine and subunit vaccine are widely used to prevent PEDV infection (Collin et al., 2015; Lawrence and Bey, 2015; Lin et al., 2017a; Liu et al., 2012; Meng et al., 2013). However, it still can not stop the PED outbreak, due to these vaccines no capable of inducing solid intestinal mucosal immunity (Wen et al., 2018). Antiviral agents can be used in either a therapeutic or a prophylactic mode to compensate for vaccines. Previous studies have discovered a few natural compounds and compositions such as quercetin 7-rhamnoside (Choi et al., 2009), 2-Deoxy-D-glucose (Wang et al., 2014), glycyrrhizin (Huan et al., 2017), lithium chloride (Li et al., 2018a) and surfactin (Yuan et al., 2018) have antivral activities on PEDV. However, there are no effective commercial antiviral agents available to control PEDV infection until now.
It has been identified that natural products can be candidates as new generations of antiviral agents (Harvey, 2008). Aloe has antiviral activity against a wide range of viruses. Research has proved that Aloe has significant inhibitory effect on influenza virus, pigeon paramyxovirus type 1, Herpes simplex virus type 1 (Dziewulska et al., 2017; Gansukh et al., 2018; Rezazadeh et al., 2016). Antiviral effects are described not only for whole extracts of Aloe, but also for their isolated compounds. It was reported that the constituents of Aloe, such as quercetin, catechin hydrate, kaempferol, aloin and emodin have significant antiviral activity (Huang et al., 2019; Jang-Gi Choi et al., 2019; Li et al., 2014; Lin et al., 2008; Mohammad et al., 2019; Sydiskis et al., 1991). The antiviral activity could be caused by inducing antiviral genes, inhibition of viral enzymes and protein expression into mammalian cells (Huang et al., 2019; Jang-Gi Choi et al., 2019; Li et al., 2014; Lin et al., 2008).
Although Aloe could serve as antiviral angent against many viruses, detailed information about the antiviral capacity against PEDV remain unclear. In this study, we investigated whether the Aloe extract (Ae) had the ability to inhibit PEDV infection. We first examined its potential to inhibit PEDV replication in vitro and determined the stages in the PEDV life cycle that could be blocked by Ae, and then extended our study in newborn piglets at a relatively safety concentration to see if Ae could inhibit PEDV infection in vivo. Our results showed that Ae inhibited PEDV infection both in vitro and in vivo, indicating that Ae can be potentially useful for the development of anti-PEDV therapeutics.
2. Materials and methods
2.1. Cells, virus and virus preparation
African green monkey kidney (Vero) cells were obtained from ATCC (ATCC number: CCL-81) (USA) and Porcine intestinal epithelial cell clone J2 (IPEC-J2) cells were obtained from Wen' s Foodstuffs Group Co, Ltd (Guangdong, China). All cells were cultured in Dulbecco' s modified eagle medium (DMEM) (Hyclone, USA) supplemented with 100 U/mL penicillin, 100 U/mL streptomycin, and 10% fetal bovine serum (FBS) (BOVOGEN, Australia). The maintenance medium for PEDV propagation was DMEM supplemented with 7.5 μg/mL trypsin (Gibco, USA).
The isolation and identification of PEDV GDS01 strain were reported previously by our laboratory (Hao et al., 2014; Li et al., 2018b). Virus propagation was performed as previously described with some modifications (Wen et al., 2018). Briefly, Vero cells were seeded into T175 flasks and cultured for 90% confluent. Fifty microliters of PEDV GDS01 strain together with 50 mL maintenance medium were added to flask after the cell monolayers were washed three times with sterile pH 7.4 1 × phosphate buffered saline (PBS). The virus-inoculated cells were cultured continuously at 37℃ in 5% CO2 to observe cytopathic effect (CPE). Around 1 day post-infection (d.p.i.), > 90% CPE was evidently observed in the inoculated cell monolayers, the flasks were twice frozen at -80℃ and thawed. The cells and supernatants were harvested together and stored at -80℃ until subsequent viral titers determination. Virus titers were determined using the Reed-Muench method (Muench, 1938) and expressed as tissue culture infective dose 50% (TCID50). Plaque forming unit (PFU) was determined according to “PFU = 0.7 × TCID50’’ as described before (Birgit et al., 2007), and the multiplicity of infection (MOI) was calculated based on PFU.
2.2. Preparation of Ae
The dried powder of Ae was purchased from Bioforte Biotechnology Co., Ltd. (Shenzhen, China). One hundred milligram (mg) Ae was dissolved with 1 milliliter (mL) DMEM and filtered with 0.22 mm filters and then stored at -4℃ until use.
2.3. Detection the cytotoxicity of Ae in cells
The cytotoxicity of Ae in Vero and IPEC-J2 cells were detected by using commercial Cell Counting Kit-8 (CCK-8) (Yeasen Biotech, China) in accordance with the manufacturer’s instructions. Briefly, cells were seeded into 96-well plates and cultured for 90% confluent, and then incubated with DMEM or Ae (2-32 mg/mL) for 24 h and 48 h. Then 10 μL CCK-8 reagent and 90 μL DMEM were added to each well and incubated at 37℃ for 1 h. The CCK-8 signal was measured at an absorbance of OD450 nm. The relative viability of the cells was counted based on the expressions: cell survival rate (%) = [OD (sample)-OD (blank)/OD (control) -OD (blank)] × 100%.
2.4. Inhibition of virus infection assay in vitro
Confluent Vero or IPEC-J2 cell monolayers in 12-well plate were inoculated with various concentrations of Ae (4-16 mg/mL) or the control normal DMEM for 1 h, followed by infection with PEDV at an MOI of 0.2 or 0.4 for 1 h, and then the viral inoculums was removed and fresh maintenance medium containing different concentrations of Ae was added. Twenty-four hours later, cells were fixed for indirect immunofluorescent assay as described below. Cells were collected at indicated time points (12 h, 24 h and 48 h), cell lysates were prepared and examined with Western Blot as described below or the viral titers in the cell lysates were determined by TCID50 analysis to calculate PFU as above described.
2.5. Immunofluorescence assay (IFA)
Immunofluorescence assay was conducted to observe PEDV-infected Vero or IPEC-J2 cells as described previously with some modifications (Xu et al., 2019). Briefly, cells were fixed with 4% paraformaldehyde for 15 min and then permeabilized with 0.2% Triton X-100 for 15 min at room temperature. After blocked with 1% bovine serum albumin (BSA), cells were stained with anti-PEDV N polyclonal antibody (Wen' s Foodstuffs Group Co., Ltd, China) (1:1000) at 37℃ for 1 h. Cells were then washed with 1 × PBS and incubated with fluoresceinisothiocyanate (FITC) (1:500) or Cy3-labeled goat anti-mouse secondary antibody (KPL, USA) (1:500) at 37℃ for 1 h. After three washes in 1 × PBS, cells were counter-stained with DAPI and observed with a fluorescence microscope (LEICA DMi8, Germany).
2.6. Western blot analysis
The whole-cell extracts were prepared with RIPA lysis buffer (Beyotime, China) supplemented with 1% protease inhibitors (Yataihengxin, China) and boiled with 6 × SDS loading buffer for 10 min before same volume of protein samples were fractionated by 12% sodium dodecyl sulfate-polyacrylamide gels (SDS-PAGE) electrophoresis, and the resolved proteins were transferred onto PVDF membranes (Millipore, USA). After blocking with 5% skim milk, the membranes were incubated for 1 h at room temperature with anti-PEDV N polyclonal antibody (Wen' s Foodstuffs Group Co., Ltd, China) (1:1000) or anti-GAPDH antibody (Proteintech Group, Inc., USA) (1:1000). The blots were subsequently incubated with HRP-conjugated goat anti-mouse IgG (1:8000) (DingGuoShengWu, China) for 1 h min at room temperature. The blots were visualized using the ECL reagent according to the manufacturer's instructions (CWBio, China).
2.7. Time-of-addition assay
IPEC-J2 cells were seeded on 12-well plates and cultured overnight before infection with PEDV at an MOI of 0.4 and were incubated for 1 h at 4 °C to synchronize infection. The inoculum was removed; 1 mL of DMEM was added to each well; and samples were placed in a humidified incubator at 37 °C. At various time points, a Ae solution was added to the wells or to the virus samples, to a final concentration of 16 mg/mL (Fig. 3 A). After 12 h, the mRNA and protein levels of N in the cells were measured by real-time PCR as described below and Western Blot as above described. Cell lysates were collected and the viral titers were determined by a TCID50 assay to calculate PFU as above described.
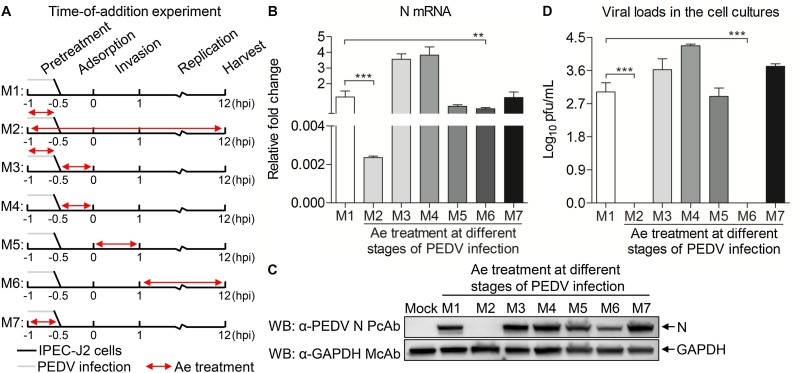
Fig. 3.
Time-of-addition experiments. (A) IPEC-J2 cells or PEDV was treated with Ae at different times before and after infection. Double-headed red arrows indicate the presence of Ae. The experiments are identified in the text by the numbers on the left (M1-M7). Cells were harvested at 12 hpi. (B) The mRNA expression of N was examined with real-time PCR using specific primers. The expression level of mRNA were calculated in relation to the expression level of GAPDH. (C) The N protein of PEDV was detected by Western Blot using anti-PEDV N polyclonal antibody. (D) The viral titers in the culture medium were determined by TCID50 analysis. Results are representative of three independent experiments. Data are represented as mean ± SD, n = 3. **stands for p < 0.01, ***stands for p < 0.001.
2.8. RNA isolation and real-time-PCR analysis
Total viral RNA was prepared from IPEC-J2 cells after infection with PEDV using a RNeasy kit (Magen, China) per the manufacturer' instruction, and was treated with DNase I. Two μg of total RNA was used for cDNA synthesis by reverse transcription using RT-PCR kit (TaKaRa). The specific primers for nucleocapsid (N) gene of PEDV (sense: 5'-TTTCTAAGGTACTTGCAAATAATG-3'; antisense: 5'-TTGGAGATCTGGACCTGTTGTTGC-3'), and glyceraldehyde-3-phosphate dehydrogenase (GAPDH) (sense: 5'-CCTTCCGTGTCCCTACTGCCAAC-3'; antisense: 5'-GACGCCTGCTTCACCACCTTCT-3') were designed with reference to previous publications (Huang et al., 2014; Xiaoliang et al., 2015) and synthesized by Sangon Company (Shanghai, China). The real-time PCR assay was carried out with an Applied Biosystem 7500 instrument (Life Technologies, USA). The PCR was performed in a 20-μL volume containing 1 μL of cDNA, 10 μL of 2 × SYBR green Premix Ex Taq (TaKaRa), and a 0.4 μM of each gene-specific primer. The thermal cycling parameters were as follows: 95 °C for 30 s; 40 cycles of 95 °C for 15 s, 60 °C for 30 s, and 72 °C for 30 s; and 1 cycle of 95 °C for 15 s, 60 °C for 1 min, and 95 °C for 15 s. The final step was to obtain a melt curve for the PCR products to determine the specificity of the amplification. All samples were carried out in triplicate on the same plate, and the GAPDH gene was utilized as the reference gene. Expression levels of N genes were calculated relative to the expression of the GAPDH gene and expressed as fold increase or decrease relative to the control samples.
2.9. Determination of direct virion inactivation activity of Ae
Determination of direct virion inactivation activity of Ae was performed as previously described with some modifications (Gao et al., 2014). Briefly, PEDV GDS01 of 1 × 106 PFU was incubated with Ae at a concentrations of 16 mg/mL for 1 h or 3 h at 37 °C. Following the treatment, viral infectivity was determined on Vero cells and the viral genome after Ae treatment was examined by RT-PCR using the specific primers as previously described (Zhang et al., 2016). To investigate whether Ae could degrade directly S1 protein, Ae at the concentration of 16 mg/mL was incubated with 100 μg purified S1 protein (Wen's Foodstuffs Group Co., Ltd, China) for 1 h or 3 h at 37 °C, and then the mixtures were harvested to analysis by SDS-PAGE gel as above described and the gel was stained with Coomassie blue dye for analysis of specific bands.
2.10. Animal experiments
The animal study was approved by the Institutional Animal Care and Use Committee of the Sun Yat-sen University (Guangdong, China) and animals were treated in accordance with the regulations and guidelines of this committee. The toxicity evaluation and anti-PEDV of Ae in vivo were performed as previously described with some modifications (Yuan et al., 2018). Briefly, 36 BALB/c mice were procured from Yancheng Biological Technology Co, Ltd (Guangzhou, China) and were randomly divided into six groups (6 mice/group) and were housed in six separate rooms. On day 0, mice in group 1 were intragastrically administered with 0.5 mL DMEM and served as controls. Mice in group 2, 3, 4, 5 and 6 were intragastrically administered with 0.5 mL DMEM containing Ae at a dose of 5, 20, 100, 500 and 2500 mg/kg of body weight (bw), respectively. In the acute toxicity study, the death of mice was observed and recorded in 8 days. For subchronic toxicity assessment, after Ae administration, the body weight of each mouse was measured daily and all mice were necropsied at 28 days post inoculation (d.p.i.). At necropsy, blood samples from all mice were collected and blood cells detection were performed.
For the PEDV protection experiment, twelve 4-day-old crossbred conventional newborn piglets produced by Duroc × Landrace × Big White were procured from Wen' s Foodstuffs Group Co, Ltd (Guangdong, China) randomly divided into three groups (4 piglets/group) and were housed in three separate rooms. All pigs were maintained in our animal facility with a mixture of skim milk powder (Zhaoqing Bozheng Technology Co., Ltd, China) with warm water ad libitum for 1 day before the experimentation. Prior to inoculation, newborn piglets were confirmed negative for the major procine enteric viruses (PDCoV, PEDV, TGEV, PRoV) by testing the rectal swabs on day −1 as previously described (Xu et al., 2018). In addition, serum of each piglet was collected and a commercial kit (ALLRIGHT BIOTECHONOLOGY, China) was applied in order to detect PEDV-specific antibody according to the manufacturer' instruction. PEDV-specific antibodies were not detected in all sera samples (data not shown). Piglets in group 2 were orally administered Ae at a dose of 100 mg/kg of bw every 6 h before feeding. Piglets in group 1 and 3 were orally administered the same amount of DMEM at the same time. One day later, piglets in group 2 and 3 were orally challenged with 2 mL DMEM containing a total of 1 × 107 PFU of PEDV GDS01 strain. Piglets that died in the PEDV group were recorded and immediately necropsied and sampled. All piglets were sacrificed 48 h after infection, and the jejuna tissues of piglets were collected and examined by histopathology, immunohistochemical staining.
2.11. Histological and immunohistochemical staining
Histological and Immunohistochemical staining were performed as previously described (Xu et al., 2018). Briefly, tissue samples of jejunum of the piglets from the challenged and control groups were separated and routinely fixed in 10% formalin for 36 h at room temperature, and then dehydrated in graded ethanol, embedded in paraffin, cut in 5-μm sectioned, and mounted onto glass slides. After the sections were deparaffinized, rehydrated, and stained with hematoxylin and eosin (H&E), the slides were examined and analyzed with conventional light microscopy. Sections (5 μm) of formalin-fixed paraffin-embedded tissues were placed onto positively charged glass slides and the slides were air dried for 120 min at 60 °C. The tissue sections were deparaffinized, and then rinsed and incubated with target retrieval solution (Servicebio, China). After being blocked with 1% BSA (Solarbio, China), the sections were incubated with anti-PEDV N polyclonal antibody (Wen's Foodstuffs Group Co., Ltd, China) (1:100) as the primary antibody for 12 h at 4 °C. They were then incubated with peroxidase-labeled goat anti-rabbit IgG secondary antibody (KPL, USA) (1:200) for 50 min at room temperature, and the samples were finally visualized with a 3, 3'-diaminobenzidine (DAB) chromogen kit (Dako, Denmark). Hematoxylin was used for counterstaining. Tissues of piglets from negative control groups were used as negative samples. The immunohistochemistry slides were evaluated by a veterinary pathologist according to the evaluation system of histology and immunohistochemistry by Jung et al. (2014).
2.12. Statistical analysis
Statistical comparisons were performed using GraphPad Prism software. The significance of the differences between the treatment group and control (Cells viability, PFU, N mRNA, WBC, RBC and PLT) was determined by the ANOVA and Mann-Whitney accordingly.
3. Results
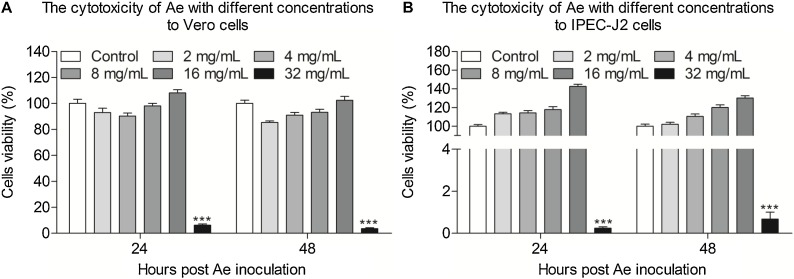
3.1. Evaluation of the cytotoxicity of Ae
To investigate the potential cytotoxicity of Ae, the relative viability rate of Vero and IPEC-J2 cells after Ae treatment was tested via CCK-8 assay. Typically, Vero or IPEC-J2 cells were cultured with Ae at different concentrations for 24 h and 48 h, respectively. As shown in Fig. 1 , after incubation with Ae at the concentrations of 2-16 mg/mL for 24 h and 48 h, the relative viability rate of Vero cells and IPEC-J2 cells was 100%, as compared with the controls, indicating that Ae had the good biocompatibility in cells. However, the cell viability decreased to 20% (p < 0.001) when the concentration was 32 mg/mL, indicating that the antiviral assays were carried out less than a concentration of 16 mg/mL.
Fig. 1.
The cytotoxicity of Ae to Vero and IPEC-J2 cells in vitro. Vero cells (A) or IPEC-J2 cells (B) were cultured with various concentrations of Ae (2-32 mg/mL) or the control normal DMEM for 24 h and 48 h prior to the CCK-8 assay. Results are representative of three independent experiments. Data are represented as mean ± SD, n = 8. ***stands for p < 0.001.
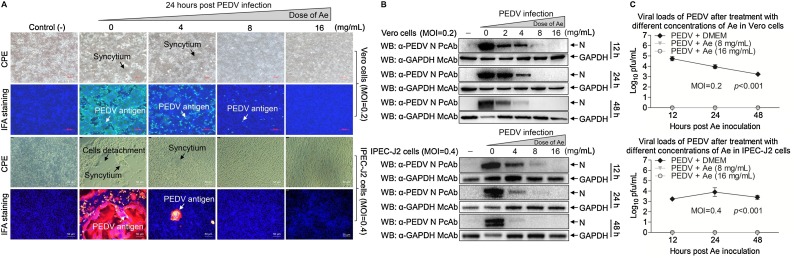
3.2. Ae inhibits PEDV infection in vitro
Since determination the maximum concentration of Ae does not affect the cells viability, we further explored the influence of Ae on PEDV by IFA with PEDV N protein-specific polyclonal antibody. As shown in Fig. 2 A, as the concentrations of Ae increased, the PEDV-specific immunofluorescence gradually reduced in infected Vero and IPEC-J2 cells, as compared to the controls, indicating that the antiviral effect of Ae followed a dose-dependent manner. Surprise, as the concentration of Ae reached 16 mg/mL, none green fluorescence signal was observed in infected cells, indicating PEDV was completely inhibited. To further prove the inhibitory effect of Ae, we also used different concentrations of Ae to treat PEDV-infected Vero and IPEC-J2 cells and examined the level of N protein in infected cells with Western Blot using specific antibodies against N and GAPDH at 12 h, 24 h and 48 h. As a result, as the concentrations of Ae increased, the expression level of N protein gradually reduced in infected cells, as compared to the controls (Fig. 2B). Consistently with the IFA results, as the concentration of Ae reached 16 mg/mL, none specific band was detected in infected cells. To evaluate the influence of Ae on the viral infection activity, one-step growth curves were plotted to detect the changes of virus titers caused by the treatment of Ae at the different concentrations during viral replication. As shown in Fig. 2C, it can be found that the viral titers reduced in the existence of Ae, as compared to the control, indicating that Ae possessed anti-PEDV infection activity. Taken together, Ae could inhibit PEDV replication in vitro.
Fig. 2.
Ae inhibits PEDV replication in vitro. Vero or IPEC-J2 cells were treated with various concentrations of Ae (4-16 mg/mL) or the control normal DMEM for 1 h, followed by infection with PEDV at an MOI of 0.2 or 0.4. After 1 h, the cells were re-treated with Ae of DMEM as control. (A) At 24 h postinoculation, an indirect immunofluorescence assay was performed. CPE and PEDV antigen were indicated by arrows. Vero or IPEC-J2 cells were treated as above described, at indicated time points (12 h, 24 h and 48 h), cell lysates were prepared and examined with Western Blot using anti-PEDV N polyclonal antibody (B) or the viral titers in the cell lysates were determined by TCID50 analysis (C). Results are representative of three independent experiments. Data are represented as mean ± SD, n = 3.
3.3. Ae acts at late stages in the replication cycle
To determine the stage at which Ae exerts its anti-PEDV effect, Ae incubated with the virus or IPEC-J2 cells at different infection process. As shown in Fig. 3 A, the Ae-treatment methods were divided into M1-M7. No Ae was added in the all infection process was set as M1 as control. Ae incubated with the virus and cells in the all infection process was set as M2. Virus was pretreated with Ae and Ae was added in the virus adsorption process was set as M3. Ae was added in the virus adsorption process was set as M4. Ae was added in the virus invasion process was set as M5. Ae was added in the virus replication process was set as M6. Cells were pretreated with Ae was set as M7. Twelve hours after PEDV infection, samples were harvested and were measured the mRNA and protein levels of N, and the samples also were analyzed to determine the titers of infectious particles in the culture medium. As shown in Fig. 3B-D, Ae had no significant effect on the mRNA and protein levels of N and infectious PEDV in the culture medium in M3, M4, M5, M7 treatment groups, but the mRNA and protein level of N and infectious PEDV in the culture medium all decreased in M2 and M6 treatment groups, as compared to the controls, indicating that Ae has inhibitory effect on virus replication, but not in preinfection, virus adsorption and virus invasion stages.
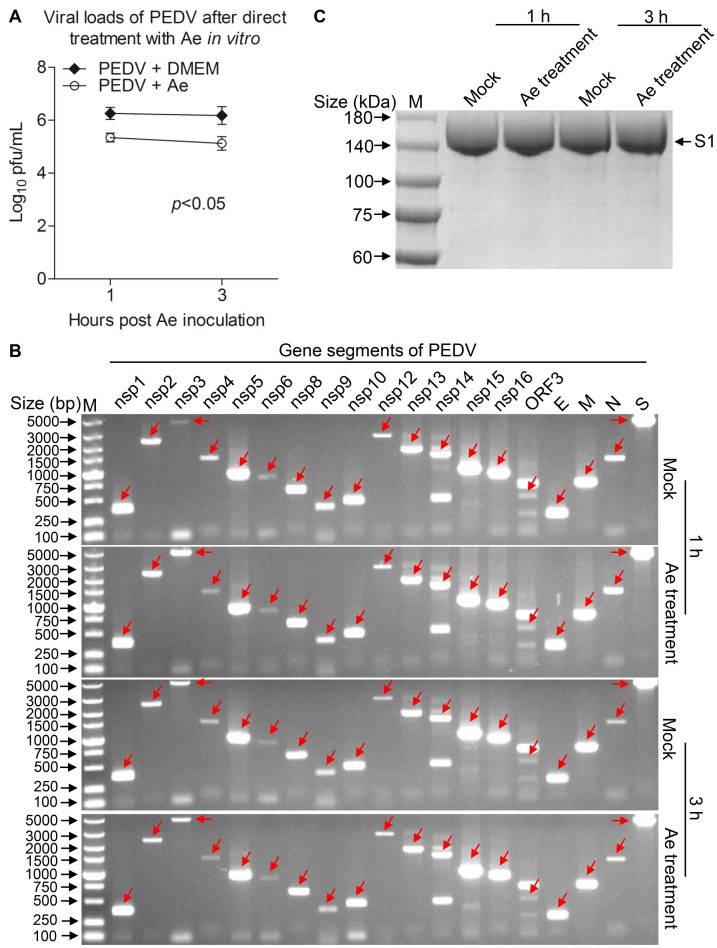
3.4. Ae inactivates PEDV virions directly
To investigate whether Ae can directly inactivate the virus infectivity, we pretreated live PEDV with Ae at 37 °C for 1 h or 3 h, and then tested the infectivity of the treated viruses. As shown in Fig. 4 A, infectivity of viruses treated in this manner was decreased dramatically (p < 0.05), indicating that the inhibitory effect of the Ae is due to partly its direct inactivation of PEDV virion particles. Since We demonstrated that Ae can directly inhibits the virus infectivity, but how it works is still unknown. To verify whether Ae destroys the genome, Ae at the indicated concentrations of 16 mg/mL was incubated with PEDV at 37°C for 1 h or 3 h, and then the mixtures were harvested for RT-PCR. As shown in Fig. 4B, RNA fragments of nsp1-nsp16, ORF3, E, M, N and S were all detectable and did not decrease after Ae treatment, as compared to the controls, indicating that Ae did not destroy the viral genome. The S protein of PEDV can be divided into S1 and S2, and S1 plays an important role in viral cell attachment (Lee et al., 2010; Li et al., 2017). Ae was further incubated with S1 protein at 37 °C for 1 h or 3 h, and then the mixtures were harvested for SDS-PAGE analysis. We found that Ae did not degrade S1 protein directly, as compared to the control (Fig. 4C). These data demonstrate that Ae inactivates PEDV virions directly had nothing to do with viral genome and S1 protein.
Fig. 4.
Ae inactivated PEDV directly but do not act on the viral genome and S1 protein. Incubating PEDV with indicated concentration (16 mg/mL) of Ae at 37 °C for 1 h or 3 h, then virus titer was determined in Vero cells (A), the whole genome sequences of the PEDV were amplified by RT-PCR (B) and the degradation of S1 protein at the indicated times after treatment with Ae was examined by SDS-PAGE analysis (C). Results are representative of three independent experiments. Data are represented as mean ± SD, n = 3.
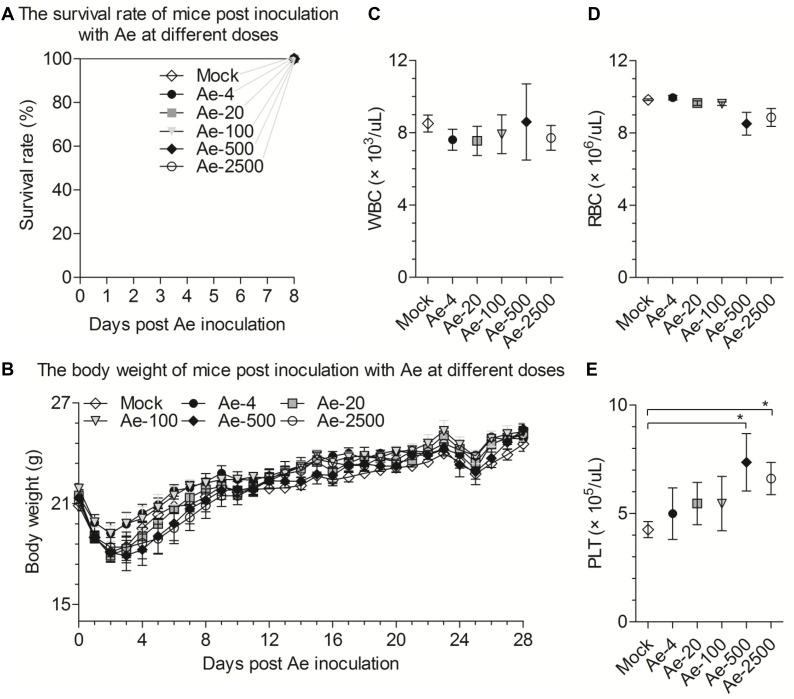
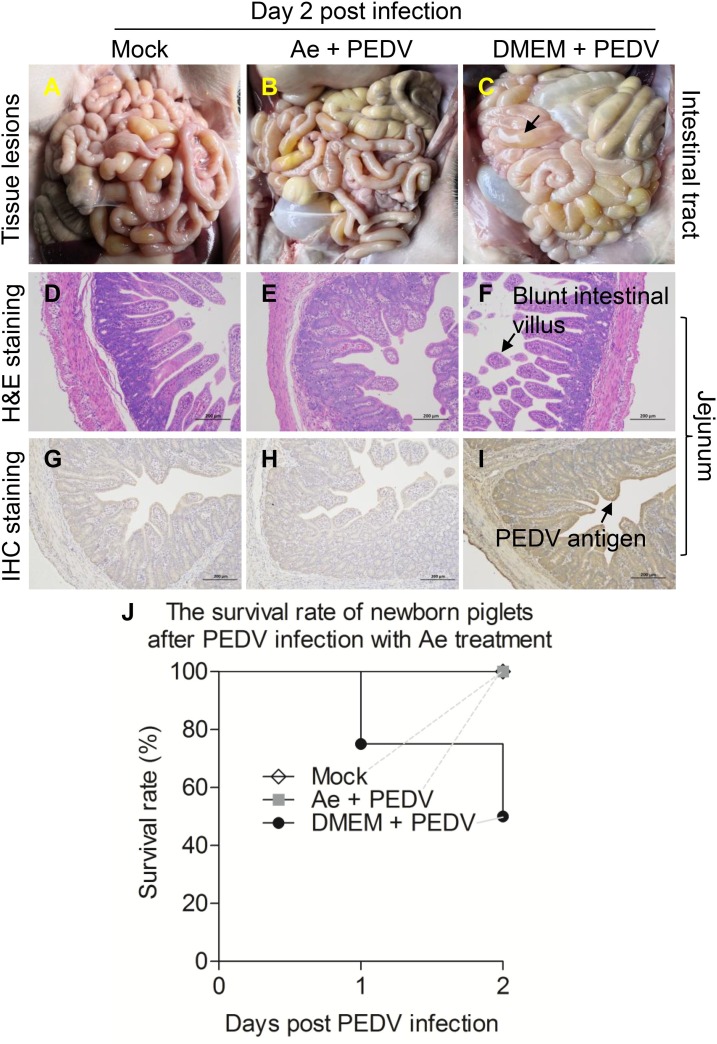
3.5. Ae protects piglets against PEDV infection in vivo
In an acute toxicity study, mice were orally administered Ae in a single dose of 0, 4, 20, 100, 500 or 2500 mg/kg of bw. No death of mice was observed in each dose group in 8 days (Fig. 5 A), indicating that there was no acute toxicity in mice after less than 2500 mg/kg of bw administration. For subchronic toxicity assessment, mice were orally administered Ae at different concentrations for 28 days. During this experiment, all mice lost weight and then gained weight in the first 4 days, but there was no siginificant difference in body weight between the Ae treatment groups and control group in 28 days (Fig. 5B). Oral Ae did not affect white blood cells (WBC) (Fig. 5C), red blood cells (RBC) (Fig. 5D) in mice. However, the level of platelets (PLT) in the blood of the high-dose (500 or 2500 mg/kg) treatment groups was significantly increased (p < 0.05) (Fig. 5E), indicating high dose administration of Ae might increase blood viscosity. Therefore, oral dose was set to 100 mg/kg bw to explore whether Ae can protect piglets from PEDV challenge. As shown in Fig. 6 J, no piglets died in the mock and Ae treatment-PEDV challenge groups (4 piglets/group) in 2 days. In contrast, PEDV challenge without Ae treatment group (4 piglets/group), two piglets died in 2 days. To determine the gross pathological and histological changes in piglets after PEDV infection, all piglets from each group were necropsied at 2 d.p.i.. In the PEDV challenge without Ae treatment group, the small intestinal tract, where yellow watery contents accumulated, were transparent, thin-walled, and gas-distended (Fig. 6C). No lesions or slight lesions were observed in the mock and Ae treatment-PEDV challenge groups (Fig. 6A&B). Microscopic lesions were also analysed. As shown in Fig. 6D-F, abruption of jejunum villus was observed in the PEDV challenge without Ae treatment group, whereas the jejunum was normal in the mock and Ae treatment-PEDV challenge groups. Consistent with the histopathological results, more PEDV antigen was detected in the cytoplasm of the villous enterocytes of the PEDV challenge without Ae treatment piglets by immunohistochemical analysis (Fig. 6G-I). Taken together, these results indicate that Ae could protect piglets against PEDV infection in vivo.
Fig. 5.
The toxicity study of Ae in vivo. (A) Survival curves of mice were orally administered Ae in a single dose of 0, 4, 20, 100, 500, or 2500 mg/kg bw in 8 days. Subchronic toxicity evaluation of oral Ae with a single dose of 0, 4, 20, 100, 500, or 2500 mg/kg bw in mice. (B) The oral doses of Ae for the 6 groups of mice were 0, 4, 20, 100, 500, or 2500 mg/kg bw, respectively. Body weight was monitored and plotted. Mice were sacrificed at day 28, and white blood cells (WBC) (C), red blood cells (RBC) (D), platelets (PLT) (E) were detected. Data are represented as mean ± SD, n = 6. *stands for p < 0.05.
Fig. 6.
Oral administration of Ae can protect piglets against PEDV infection in vivo. (A) Macroscopic picture of intestine from a control piglet at 2 d.p.i. (B-C) Macroscopic pictures of intestine from Ae + PEDV and DMEM + PEDV-challenged piglets at 2 d.p.i. Thin-walled intestinal tracts were indicated by arrows. (D) H&E-stained jejunum tissue section of a control piglet at 2 d.p.i. (E-F) H&E-stained jejunum tissue section of Ae + PEDV and DMEM + PEDV-challenged piglets at 2 d.p.i. Blunt intestinal villus was indicated by arrows. (G) Immunohistochemically stained jejunum tissue section of a control piglet at 2 d.p.i. (H-I) Immunohistochemically stained jejunum tissue section of Ae + PEDV and DMEM + PEDV-challenged piglets at 2 d.p.i.. (J) The mortality of newborn piglets in each group was recorded from 1 to 2 d.p.i.. Data are represented as mean ± SD, n = 4.
4. Discussion
Since PEDV variants emerged in the swine industry, it has caused significant problems in the swine industry (Sun et al., 2016; Vlasova et al., 2014). PEDV invasion of porcine intestinal epithelial cells causes enteritis in swine of all ages and is often fatal in neonatal piglets (Debouck and Pensaert, 1980; Ducatelle et al., 1981). Although vaccines are available for PEDV, they are not optimal in terms of safety and efficacy, and large-scale infections still occur (Yuan et al., 2018). Antiviral drugs that are effective against PEDV are urgently needed to combat these threats. In the present study, we reported that Ae, a common plant extract, inhibited PEDV infection both in vitro and in vivo, might help to control PED in pig farm.
The premise of antiviral test is the cytotoxicity analysis of drug, since the cell toxicity of the drugs may influence the judgment of the antiviral effect of drug in vitro. The MTT [3-(4,5-dimethyl-2-thiazolyl)-2,5-diphenyl-2H-tetrazo-lium bromide] and CCK-8 assays are common used to determinate the cytotoxicity of drug (Gao et al., 2014; Ting et al., 2018). In the study, we chose more sensitive CCK-8 assay to determine the cytotoxicity to Vero and IPEC-J2 cells of Ae, due to these cell types are commonly used to study PEDV (Lin et al., 2017a; Lin et al., 2017b). We found that the concentrations of 2-16 mg/mL of Ae were not cytotoxicity in Vero and IPEC-J2 cells, but the cell viability decreased to 20% when the concentration was 32 mg/mL, indicating that antiviral assays were carried out less than a concentration of 16 mg/mL. In addition, the result demonstrated there exist some compositions in Ae have cytotoxicity, indicating that the toxic ingredients of Ae need to determine and remove.
Plants and plant-derived compounds are exploited extensively as candidates for new antiviral agents due to they produce few side effects and high availabilities and low cost (Hakobyan et al., 2016). Aloe vera belongs to Liliaceae family among the succulent plants, which has got various properties such as immunomodulatory, anti-inflammatory and antiviral in nature (Manigandan et al., 2015; Sudarshan et al., 2014). Aloe or its constituents have significant inhibitory effect on influenza virus, pigeon paramyxovirus type 1, Herpes simplex virus type 1, Japanese encephalitis virus, enveloped viruses and hepatitis B virus (Dziewulska et al., 2017; Gansukh et al., 2018; Lin et al., 2008; Mohammad et al., 2019; Rezazadeh et al., 2016; Sydiskis et al., 1991). In our experiment, we found that Ae could inhibit PEDV infection in Vero and IPEC-J2 cells in vitro. It is known that one of problems of antiviral drugs is resistance, which due to some antiviral drugs can not completely kill virus, then the surviving virus particles will mutate to resist the antiviral drugs (Leen et al., 2014). RNA viruses are more likely to produce resistance than DNA viruses, due to the mutation rate of RNA viruses is higher than DNA viruses (Sanjuan et al., 2010). Interestingly, PEDV was completely inhibited when the concentration of Ae reached 16 mg/mL, indicating that it can reduce the possibility of virus develop resistance and prolong the use of drug. Although it is difficult to definitive regarding how Ae inhibits PEDV infection, our results suggest that it interferes with the stage of virus replication. The mRNA and protein levels of N were reduced and no live virions after Ae treatment in the replication phase, indicating that Ae might block the transcription of viral N genes as well as the synthesis of capsid protein, reducing viral progeny. We also found that Ae could directly inhibit PEDV infection activity but had no effect on virus genome without the presence of cells. In addition, although S1 protein related to virus attachment and entry (Wen et al., 2018), Ae could not degrade S1 protein in vitro, indicating that Ae can directly inactivate the virus infectivity, but no effect on virus nucleic and virus invasion, consistent with the results of time-of-addition assay. It was reported that emodin from Aloe are directly virucidal to enveloped viruses and are related to the partially disruption of viral envelopes (Sydiskis et al., 1991), indicating that the direct inactivation PEDV by Ae might relate to emodin's destruction of the virus envelope.
For a antiviral drug candidate, safety is the top concern. Acute and subacute toxicity are the two important index for drug safety evaluation (Vakili et al., 2017), which can help to determine the scope and the time of the drug use, reduce side effects. In this study, we fed Ae to mice and determined a safe dose of 100 mg/kg of bw by recording the deaths, weight changes and blood cell counts of Ae-treatmented mice. This will provide a reference for the proper use of drugs in pigs. It was reported that PEDV only infects pigs and has most harmful to 7-10-day-old suckling piglets with a high mortality rate (Li et al., 2012; Pijpers et al., 1993; Stevenson et al., 2013). We fed Ae at a safe dose of 100 mg/kg of bw to newborn piglets then challenged with a lethal dose of PEDV, which confirmed that Ae can significantly protect piglets against PEDV infection in vivo, consistant with the results of in vitro experiments, indicating that Ae can be used as one of choice for prevention and control PEDV in pig farm. Although we confirmed that Ae could inhibit PEDV in vivo, slight diarrhea (data not shown) was found in Ae-treatmented piglets, which might be related with Aloe vera ingredient emodin, which used as a laxative (Chen et al., 2012), indicating that the side effect need to pay attention during the use of Ae. Together, all these results confirmed that Ae can inhibit PEDV infection and might serve as a good anti-PEDV agents candidate. However, there are still several important questions remain for us to do. For instance, What’s the key compound of Ae is responsible for the inhibitions of PEDV replication? And what’s the exact underlying mechanism? Can Ae resist other CoVs like TGEV, PEAV and PDCoV in pigs? Elucidation of these questions will help us to develop a safe and efficacious antiviral agent to control swine CoVs.
In conclusion, this study represents an important first report on the anti-PEDV properties of the aqueous extract of Aloe. Our research demonstrated that Ae has antiviral activity against PEDV infection in vitro and in vivo, indicating that it might be developed into a new antiviral agent and used to control PED in pig farm.
Author Contributions
ZCX conceived and designed the experiments; YL and ZCX performed the experiments; ZCX analyzed the data; YCC, PP, YFL, MYH, YHM and CYX contributed reagents/materials/analysis tools; ZCX wrote the paper. YCC checked and finalized the manuscript. All authors read and approved the final manuscript.
Ethical approval
The animal study was supervised by the Institutional Animal Care and Use Committee of Sun Yat-sen University (IACUC DD-18-0111) and used in accordance with regulation and guidelines of this committee.
Declaration of Competing Interest
The authors declare that they have no conflict interest.
Acknowledgements
This work was supported by the grant from State Key Laboratory of Biocontrol of Sun Yat-sen University (#09020-32030002) and the Reaserch Fund of Wen' s Foodstuffs Group Co, Ltd (#ZB20190509CCXY009).
References
- Birgit Quinting, Béatrice Robert, Carine Letellier, Mathieu Boxus, Pierre Kerkhofs. Development of a 1-step enzyme-linked immunosorbent assay for the rapid diagnosis of bovine respiratory syncytial virus in postmortem specimens. J. Vet. Diagn. Invest. 2007;19:238–243. doi: 10.1177/104063870701900302. [DOI] [PubMed] [Google Scholar]
- Chen D., Xiong Y., Wang L., Lv B., Lin Y. Characteristics of emodin on modulating the contractility of jejunal smooth muscle. Can. J. Physiol. Pharmacol. 2012;90:455–462. doi: 10.1139/y2012-004. [DOI] [PubMed] [Google Scholar]
- Choi H.J., Kim J.H., Lee C.H., Ahn Y.J., Song J.H., Baek S.H., Kwon D.H. Antiviral activity of quercetin 7-rhamnoside against porcine epidemic diarrhea virus. Antiviral. Res. 2009;81:77–81. doi: 10.1016/j.antiviral.2008.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collin E.A., Anbalagan S., Okda F., Batman R., Nelson E., Hause B.M. An inactivated vaccine made from a U.S. field isolate of porcine epidemic disease virus is immunogenic in pigs as demonstrated by a dose-titration. BMC. Vet. Res. 2015;11:62. doi: 10.1186/s12917-015-0357-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Debouck P., Pensaert M.B. Experimental infection of pigs with a new porcine enteric coronavirus, CV 777. Am. J. Vet. Res. 1980;41:219–223. [PubMed] [Google Scholar]
- Doyle L.P., Hutchings L.M. A transmissible gastroenteritis in pigs. J. Am. Vet. Med. Assoc. 1946;108:257–259. [PubMed] [Google Scholar]
- Ducatelle R., Coussement W., Charlier G., Debouck P., Hoorens J. Three-dimensional sequential study of the intestinal surface in experimental porcine CV 777 coronavirus enteritis. Zentralbl. Veterinärmed. B. 1981;28:483–493. doi: 10.1111/j.1439-0450.1981.tb01765.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dziewulska, Stenzel, Śmiałek, Tykałowski, Koncicki An evaluation of the impact of aloe vera and licorice extracts on the course of experimental pigeon paramyxovirus type 1 infection in pigeons. Poul. Sci. 2017;97:47–476. doi: 10.3382/ps/pex341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gansukh E., Gopal J., Paul D., Muthu M., Kim D.-H., Oh J.-W., Chun S. Ultrasound mediated accelerated anti-influenza activity of Aloe vera. Sci. Rep. 2018;8:17782. doi: 10.1038/s41598-018-35935-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao L., Sun Y., Si J., Liu J., Sun G., Sun X., Cao L. Cryptoporus volvatus extract inhibits influenza virus replication in vitro and in vivo. PLoS. One. 2014;9 doi: 10.1371/journal.pone.0113604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hakobyan A., Arabyan E., Avetisyan A., Abroyan L., Hakobyan L., Zakaryan H. Apigenin inhibits African swine fever virus infection in vitro. Arch. Virol. 2016;161:3445–3453. doi: 10.1007/s00705-016-3061-y. [DOI] [PubMed] [Google Scholar]
- Hao J., Xue C., He L., Wang Y., Cao Y. Bioinformatics insight into the spike glycoprotein gene of field porcine epidemic diarrhea strains during 2011–2013 in Guangdong, China. Virus. genes. 2014;49:58–67. doi: 10.1007/s11262-014-1055-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey A.L. Natural products in drug discovery. Drug. Discov. Today. 2008;13:894–901. doi: 10.1016/j.drudis.2008.07.004. [DOI] [PubMed] [Google Scholar]
- Huan C.C., Wang H.X., Sheng X.X., Wang R., Wang X., Mao X. Glycyrrhizin inhibits porcine epidemic diarrhea virus infection and attenuates the proinflammatory responses by inhibition of high mobility group box-1 protein. Arch. Virol. 2017;162:1467–1476. doi: 10.1007/s00705-017-3259-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang C.-T., Hung C.-Y., Hseih Y.-C., Chang C.-S., Velu A.B., He Y.-C., Huang Y.-L., Chen T.-A., Chen T.-C., Lin C.-Y. Effect of aloin on viral neuraminidase and hemagglutinin-specific T cell immunity in acute influenza. Phytomedicine. 2019;64:152904. doi: 10.1016/j.phymed.2019.152904. [DOI] [PubMed] [Google Scholar]
- Huang C., Zhang Q., Guo X.K., Yu Z.B., Xu A.T., Tang J., Feng W.H. Porcine reproductive and respiratory syndrome virus nonstructural protein 4 antagonizes beta interferon expression by targeting the NF-kappaB essential modulator. J. Virol. 2014;88:10934–10945. doi: 10.1128/JVI.01396-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jang-Gi Choi H.L., Kim Young Soo, Hwang Youn-Hwan, You-Chang Oh, Lee Bonggi, Moon Kyoung Mi, Cho Won-Kyung, Ma Jin Yeul. Aloe vera and its Components Inhibit Influenza A Virus-Induced Autophagy and Replication. Am. J. Chin. Med. 2019;47:1307–1324. doi: 10.1142/S0192415X19500678. [DOI] [PubMed] [Google Scholar]
- Jung K., Wang Q., Scheuer K.A., Lu Z., Zhang Y., Saif L.J. Pathology of US Porcine Epidemic Diarrhea Virus Strain PC21A in Gnotobiotic Pigs. Emerg. Infect. Dis. 2014;20:668–671. doi: 10.3201/eid2004.131685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kocherhans R., Bridgen A., Ackermann M., Tobler K. Completion of the porcine epidemic diarrhoea Coronavirus (PEDV) genome sequence. Virus. Genes. 2001;23:137–144. doi: 10.1023/A:1011831902219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang G., Jie L., Zhou Q., Xu Z., Li C., Yun Z., Xue C., Wen Z., Cao Y. A new Bat-HKU2–like Coronavirus in Swine, China, 2017. Emerg. Infect. Dis. 2017;23:1607–1609. doi: 10.3201/eid2309.170915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence P., Bey R. 2015. Recombinant Spike Protein Subunit Based Vaccine for Porcine Epidemic Diarrhea Virus (PEDV) [Google Scholar]
- Lee D.K., Park C.K., Kim S.H., Lee C. Heterogeneity in spike protein genes of porcine epidemic diarrhea viruses isolated in Korea. Virus. Res. 2010;149:175–182. doi: 10.1016/j.virusres.2010.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leen D., Nidya S.G., Ali T., Gilles Q., Boris P., Mathy F., Kai D., Dirk J., Piet H., Felio B. Mutations in the chikungunya virus non-structural proteins cause resistance to favipiravir (T-705), a broad-spectrum antiviral. J. Antimicrob. Chemother. 2014;10:2770–2784. doi: 10.1093/jac/dku209. [DOI] [PubMed] [Google Scholar]
- Li C., Li W., Lucio de Esesarte E., Guo H., van den Elzen P., Aarts E., van den Born E., Rottier P.J.M., Bosch B.J. Cell attachment domains of the porcine epidemic diarrhea virus spike protein are key targets of neutralizing antibodies. J. Virol. 2017;91:e00273–71. doi: 10.1128/JVI.00273-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li H.J., Gao D.S., Li Y.T., Wang Y.S., Liu H.Y., Zhao J. Antiviral effect of lithium chloride on porcine epidemic diarrhea virus in vitro. Res. Vet. Sci. 2018;118:288–294. doi: 10.1016/j.rvsc.2018.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Q., Xu Z., Wu T., Peng O., Huang L., Zhang Y., Xue C., Wen Z., Zhou Q., Cao Y. A flagellin-adjuvanted PED subunit vaccine improved protective efficiency against PEDV variant challenge in pigs. Vaccine. 2018;36:4228–4235. doi: 10.1016/j.vaccine.2018.05.124. [DOI] [PubMed] [Google Scholar]
- Li S.W., Yang T.C., Lai C.C., Huang S.H., Liao J.M., Wan L., Lin Y.J., Lin C.W. Antiviral activity of aloe-emodin against influenza A virus via galectin-3 up-regulation. Eur. J. Pharmacol. 2014;738:125–132. doi: 10.1016/j.ejphar.2014.05.028. [DOI] [PubMed] [Google Scholar]
- Li W., Li H., Liu Y., Pan Y., Deng F., Song Y., Tang X., He Q. New variants of porcine epidemic Diarrhea virus, China, 2011. Emerg. Infect. Dis. 2012;18:1350–1353. doi: 10.3201/eid1808.120002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin C.M., Hou Y., Marthaler D.G., Gao X., Liu X., Zheng L., Saif L.J., Wang Q. Attenuation of an original US porcine epidemic diarrhea virus strain PC22A via serial cell culture passage. Vet. Microbiol. 2017;201:62–71. doi: 10.1016/j.vetmic.2017.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin C.W., Wu C.F., Hsiao N.W., Chang C.Y., Li S.W., Lei W., Lin Y.J., Lin W.Y. Aloe-emodin is an interferon-inducing agent with antiviral activity against Japanese encephalitis virus and enterovirus 71. Int. J. Antimicrob. Agents. 2008;32:355–359. doi: 10.1016/j.ijantimicag.2008.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin H., Li B., Chen L., Ma Z., He K., Fan H. Differential protein analysis of IPEC-J2 cells infected with porcine epidemic Diarrhea virus pandemic and classical strains elucidates the pathogenesis of infection. J. Proteome. Res. 2017;16:2113–2120. doi: 10.1021/acs.jproteome.6b00957. [DOI] [PubMed] [Google Scholar]
- Liu D.Q., Ge J.W., Qiao X.Y., Jiang Y.P., Liu S.M., Li Y.J. High-level mucosal and systemic immune responses induced by oral administration with Lactobacillus-expressed porcine epidemic diarrhea virus (PEDV) S1 region combined with Lactobacillus-expressed N protein. Appl. Microbiol. Biotechnol. 2012;93:2437–2446. doi: 10.1007/s00253-011-3734-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manigandan T., Elumalai M., Cholan P., Kaur R.P., Mangaiyarkarasi S. Benefits of Aloe vera in dentistry. J. Pharm. Bioallied Sci. 2015;7:257. doi: 10.4103/0975-7406.155943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meng F., Ren Y., Suo S., Sun X., Li X., Li P., Yang W., Li G., Li L., Schwegmann-Wessels C. Evaluation on the efficacy and immunogenicity of recombinant DNA plasmids expressing spike genes from porcine transmissible gastroenteritis virus and porcine epidemic Diarrhea virus. PLos. One. 2013;8 doi: 10.1371/journal.pone.0057468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohammad K.P., Mohammed S.A.D., Perwez A., MdTabish R., Mohammed F.A., Ali S.A. The anti-hepatitis B virus therapeutic potential of anthraquinones derived from Aloe vera. Phytother. Res. 2019;33:2960–2970. doi: 10.1002/ptr.6471. [DOI] [PubMed] [Google Scholar]
- Muench L.J.R.H. A simple method of extimating fifty per cent endpoints. Am. J. Hyg. 1938;27:493–497. [Google Scholar]
- Pensaert M.B., Bouck P.D. A new coronavirus-like particle associated with diarrhea in swine. Arch.Virol. 1978;58:243–247. doi: 10.1007/BF01317606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pijpers A., Nieuwstadt A.V., Terpstra C., Verheijden J.H. Porcine epidemic diarrhoea virus as a cause of persistent diarrhoea in a herd of breeding and finishing pigs. Vet. Rec. 1993;132:129-. doi: 10.1136/vr.132.6.129. [DOI] [PubMed] [Google Scholar]
- Rezazadeh F., Moshaverinia M., Motamedifar M., Alyaseri M. Assessment of anti HSV-1 activity of Aloe vera gel extract: an in vitro study. J. Dent. 2016;17:49–54. [PMC free article] [PubMed] [Google Scholar]
- Sanjuan R., Nebot M.R., Chirico N., Mansky L.M., Belshaw R. Viral mutation rates. J. Virol. 2010;84:9733–9748. doi: 10.1128/JVI.00694-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song D., Park B. Porcine epidemic diarrhoea virus: a comprehensive review of molecular epidemiology, diagnosis, and vaccines. Virus. Genes. 2012;44:167–175. doi: 10.1007/s11262-012-0713-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevenson G.W., Hai H., Schwartz K.J., Burrough E.R., Kyoungjin J.Y. Emergence of Porcine epidemic diarrhea virus in the United States: clinical signs, lesions, and viral genomic sequences. J. Vet. Diagn. Invest. 2013;25:649–654. doi: 10.1177/1040638713501675. [DOI] [PubMed] [Google Scholar]
- Sudarshan R., Amsigeri R.G., Vijayabala G.S. Aloe vera in dentistry. J. Bergen. Cty. Dent. Soc. 2014;8:01–02. [Google Scholar]
- Sun D., Wang X., Wei S., Chen J., Feng L. Epidemiology and vaccine of porcine epidemic diarrhea virus in China: a mini-review. J. Vet. Med. Sci. 2016;78:355–363. doi: 10.1292/jvms.15-0446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sydiskis R.J., Owen D.G., Lohr J.L., Rosler K.H., Blomster R.N. Inactivation of enveloped viruses by anthraquinones extracted from plants. Antimicrob. Agents. Chemother. 1991;35:2463–2466. doi: 10.1128/aac.35.12.2463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ting D., Dong N., Fang L., Lu J., Bi J., Xiao S., Han H. Multisite inhibitors for enteric Coronavirus: antiviral cationic carbon dots based on curcumin. ACS Appl. Nano Mater. 2018;1:5451–5459. doi: 10.1021/acsanm.0c00970. [DOI] [PubMed] [Google Scholar]
- Vakili T., Iranshahi M., Arab H., Riahi B., Roshan N.M., Karimi G. Safety evaluation of auraptene in rats in acute and subacute toxicity studies. Regul. Toxicol. Pharmacol. 2017;91:159–164. doi: 10.1016/j.yrtph.2017.10.025. [DOI] [PubMed] [Google Scholar]
- Vlasova A.N., Marthaler D., Wang Q., Culhane M.R., Rossow K.D., Rovira A., Collins J., Saif L.J. Distinct characteristics and complex evolution of PEDV strains, North America, May 2013-February 2014. Emerg. Infect. Dis. 2014;20:1620–1628. doi: 10.3201/eid2010.140491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Li J.R., Sun M.X., Ni B., Huan C., Huang L., Li C., Fan H.J., Ren X.F., Mao X. Triggering unfolded protein response by 2-deoxy-d-glucose inhibits porcine epidemic diarrhea virus propagation. Antiviral. Res. 2014;106:33–41. doi: 10.1016/j.antiviral.2014.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen Z., Xu Z., Zhou Q., Li W., Wu Y., Du Y., Chen L., Zhang Y., Xue C., Cao Y. Oral administration of coated PEDV-loaded microspheres elicited PEDV-specific immunity in weaned piglets. Vaccine. 2018;36:6803–6809. doi: 10.1016/j.vaccine.2018.09.014. [DOI] [PubMed] [Google Scholar]
- Woo P.C., Lau S.K., Lam C.S., Lau C.C., Tsang A.K., Lau J.H., Bai R., Teng J.L., Tsang C.C., Wang M., Zheng B.J., Chan K.H., Yuen K.Y. Discovery of seven novel Mammalian and avian coronaviruses in the genus deltacoronavirus supports bat coronaviruses as the gene source of alphacoronavirus and betacoronavirus and avian coronaviruses as the gene source of gammacoronavirus and deltacoronavirus. J. Virol. 2012;86:3995–4008. doi: 10.1128/JVI.06540-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiaoliang Hu, Nannan Li, Zhige Tian, Xin Yin, Liandong Qu. Molecular characterization and phylogenetic analysis of transmissible gastroenteritis virus HX strain isolated from China. BMC. Vet. Res. 2015:21. doi: 10.1186/s12917-015-0387-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Z., Zhang Y., Gong L., Huang L., Lin Y., Qin J., Du Y., Zhou Q., Xue C., Cao Y. Isolation and characterization of a highly pathogenic strain of Porcine enteric alphacoronavirus causing watery diarrhoea and high mortality in newborn piglets. Transbound. Emerg. Dis. 2019;66:119–130. doi: 10.1111/tbed.12992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Z., Zhong H., Zhou Q., Du Y., Chen L., Zhang Y., Xue C., Cao Y. A highly pathogenic strain of porcine deltacoronavirus caused watery Diarrhea in newborn piglets. Virol. Sin. 2018;33:131–141. doi: 10.1007/s12250-018-0003-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan L., Zhang S., Wang Y., Li Y., Wang X., Yang Q. Surfactin inhibits membrane fusion during invasion of epithelial cells by enveloped viruses. J. Virol. 2018:92. doi: 10.1128/JVI.00809-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Q., Shi K., Yoo D. Suppression of type I interferon production by porcine epidemic diarrhea virus and degradation of CREB-binding protein by nsp1. Virology. 2016;489:252–268. doi: 10.1016/j.virol.2015.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]