To the Editor:
Critically ill patients are often unable to communicate, placing the onus on clinicians in ICUs to engage family members. In the United States, practice has gradually shifted toward including family members in ICU rounds (1). However, the novel coronavirus disease (COVID-19) pandemic dramatically altered hospital care in the United States. For example, early reports suggested many hospitals restricted access to visitors (2). We sought to understand changes to visitation policies and strategies used to communicate with family members because of COVID-19.
We identified all hospitals with ICUs in the state of Michigan using the 2018 American Hospital Association annual survey database and by Internet searches. In early April, Michigan’s statewide ICU occupancy was 71%, the fifth highest in the United States (3). Within each hospital, an ICU physician or nurse leader from a medical ICU was identified and surveyed over the telephone between April 6, 2020, and May 8, 2020. If the ICU leader was unavailable by telephone, an online survey was conducted.
Participants were asked 1) whether their hospital made any changes to its visitation policy; 2) what changes were made; 3) whether their ICU had changed the way it routinely communicated with family members; and 4) what strategies their ICU was using to communicate with family members. χ2 and t tests were used to compare responding and nonresponding hospitals. All tests were two sided, with a P value of less than 0.05 considered significant. This research was deemed to be exempt from review by the University of Michigan Institutional Review Board (HUM00179422).
We surveyed 49 out of 89 Michigan hospitals with ICUs (response rate = 55%). Characteristics between responding and nonresponding hospitals were similar (Table 1). All 49 responding hospitals had changes to their visitation policies because of COVID-19 (Figure 1). One hospital (2%) indicated that visitation was still allowed but had been restricted to one visitor per ICU patient. All other hospitals (98%) had implemented “no visitor” policies; 19 (39%) prohibited all visitors without exceptions, and 29 (59%) prohibited visitors but allowed for certain exceptions.
Table 1.
Characteristics of Michigan Hospitals by Survey Response from 2018 AHA Data
| Characteristics | Responding Hospitals (n = 49)* | Nonresponding Hospitals (n = 40)† | P Value |
|---|---|---|---|
| Urban | 29 (67.4) | 26 (74.3) | 0.51 |
| Hospital beds | 0.67 | ||
| <100 | 20 (46.5) | 18 (51.4) | |
| ≥100 | 23 (53.5) | 17 (48.6) | |
| ICU beds | 0.82 | ||
| <20 | 21 (48.8) | 18 (51.4) | |
| ≥20 | 22 (51.2) | 17 (48.6) | |
| Teaching hospital | 4 (9.3) | 3 (8.6) | 0.91 |
| Critical access hospital | 1 (2.3) | 3 (8.6) | 0.21 |
| Telehealth available | 22 (51.2) | 12 (34.3) | 0.14 |
| Intensivists provide care | 26 (60.5) | 26 (76.5) | 0.14 |
Definition of abbreviation: AHA = American Hospital Association.
Data are provided as n (%) unless otherwise specified.
Six responding hospitals did not participate in the AHA database.
Five nonresponding hospitals did not participate in the AHA database.
Figure 1.
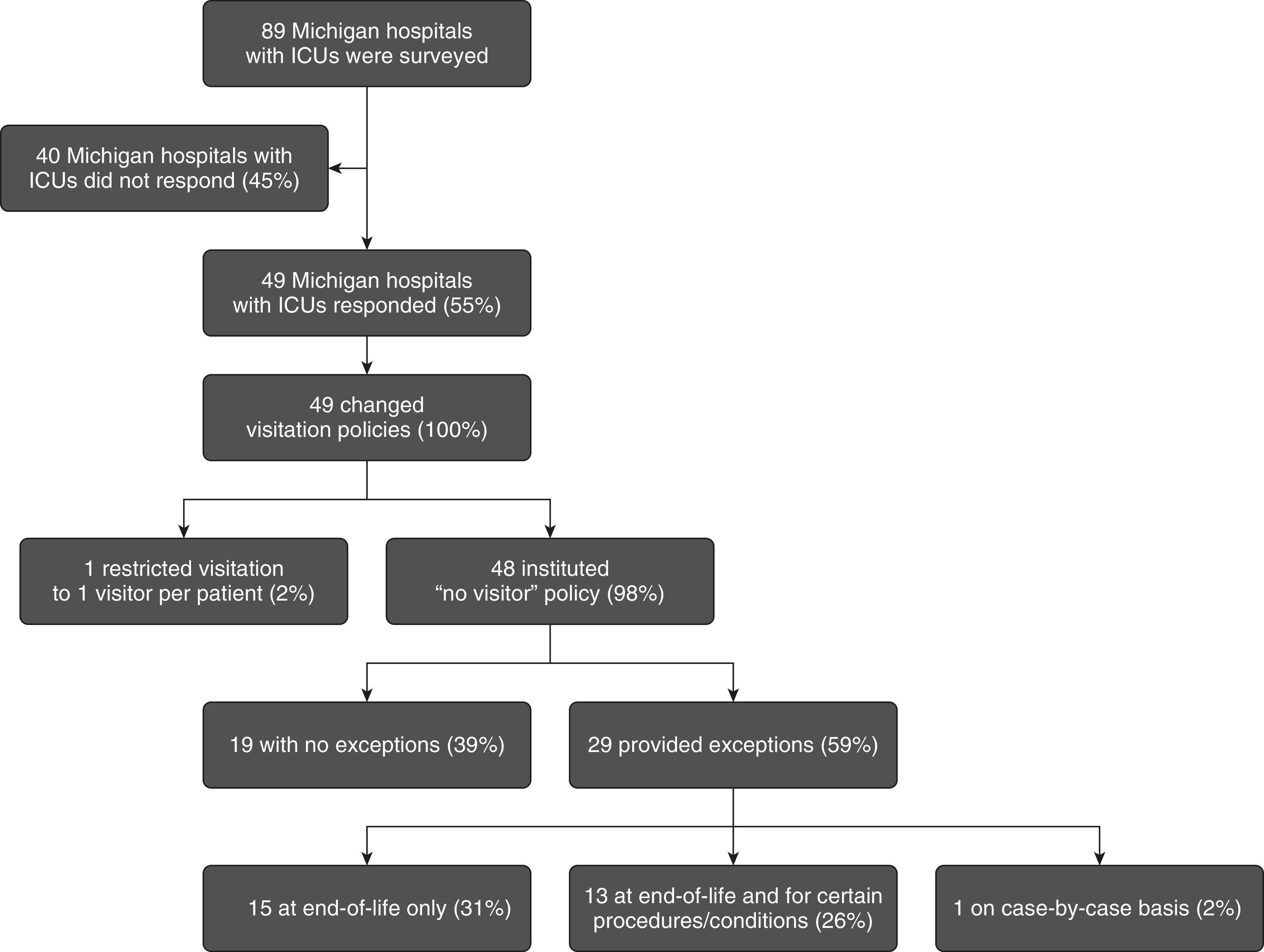
Changes to visitation policies in Michigan ICUs due to coronavirus disease (COVID-19).
Of these 29 hospitals, 15 (31%) allowed visitors at the end of life only. In addition to the end of life, 13 hospitals (26%) also made exceptions for other conditions or procedures, such as birth or surgery, or for pediatric patients. One hospital (2%) allowed visitors on a case-by-case basis only. Nine (18%) hospitals permitted only one visitor for exceptions to the no visitor policy, whereas the other 20 (41%) either limited the number of visitors or did not specify a number. Five hospitals (10%) mentioned additional restrictions placed on visitors, such as requiring visitors to be COVID-19 negative or wear personal protective equipment.
Forty hospitals (82%) reported changes to how clinicians routinely communicated with family members. These hospitals indicated that changes in communication strategies focused on virtual forms of communication, such as telephone calls or video conferencing. Of these 40 hospitals, 17 (35%) provided additional details about the mode of communication that clinicians were using, as follows: 11 (23%) used telephones, whereas six (12%) used video conferencing.
For patient–family communication, 34 hospitals (69%) encouraged video communication between patients and family members using tablets or smart phones, whereas one hospital (2%) was in the process of securing tablets for patients. Two hospitals (4%) required patients to have their own device to communicate with family members.
We found that all surveyed Michigan hospitals had changed their visitation policies, with the majority prohibiting visitors. These restrictions were in place in urban areas as well as rural locations less affected by COVID-19. As a result of these changes, hospitals leaned heavily on virtual forms of communication with family, predominantly using telephones for clinician–family communication and video for patient–family communication.
Our findings should be considered in the context of certain limitations. We cannot account for visitation policies at nonresponding hospitals, although characteristics between respondents and nonrespondents were similar. We surveyed ICU leaders and cannot delineate whether visitation policies may have differed outside of the ICU or whether individual clinicians may have used alternative strategies for communication. We cross-sectionally surveyed hospitals at the height of the spring 2020 COVID-19 pandemic in Michigan, and policies changed over time. Future work should consider specific details as to how these changes were implemented and their impact.
Restrictions to hospital visitation policies were placed for public health reasons to protect patients, family members, and healthcare staff (2). However, this dramatic change in visitation policies and communication practices has major implications for patients, family members, clinicians, and health care at large.
For patients, early reports of COVID-19 described high rates of delirium and sedation requirements (4). Access to family members could reduce delirium and sedative use, which have been associated with increased mortality, cognitive impairment, and functional disability (5, 6). Family members play a crucial role for critically ill patients without decision-making capacity. Their bedside presence may be important to understanding the patient experience, promoting effective surrogate decision-making, and preparing for postdischarge recovery. Family members of ICU patients are at risk for depression, anxiety, and posttraumatic stress (7). The extent to which restricted access to their loved ones and changes in communication with clinicians might influence emotional distress is unknown. Clinicians who care for patients with COVID-19 may suffer grave moral distress (8). A driver for this distress may include the inability to have difficult conversations with family members in person.
Finally, for health care at large, numerous reports have identified stark racial and socioeconomic inequities in the incidence and severity of COVID-19 (9). Restricted visitation may inadvertently exacerbate preexisting disparities. For example, underserved communities may have less access to technology (10), and digital communication may hamper the ability to adapt to differences in communication styles (11). In addition, the implementation of restricted visitation policies, particularly in situations in which exceptions exist, could result in biased application of policies both within and across hospitals (12, 13).
In the context of uncertainties related to the future of COVID-19 and other pandemics, we must consider whether no-visitor policies are essential for continued infection prevention and to what extent restricted visitation and changes in communication practices might unintentionally foster poor health outcomes, inequity, and animosity toward health care (13).
Supplementary Material
Footnotes
Supported by NIH grant K23-HL140165 (T.S.V.). The funding organization had no role in the design and conduct of the study; in the collection, analysis, and interpretation of the data; or in the preparation, review, or approval of the manuscript.
Author Contributions: T.S.V. had full access to all of the data in the study and takes full responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: T.S.V. and A.S. Acquisition of data: T.S.V., A.S., M.T.N., L.J.M., K.L., S.W.K., M.K., C.E.H., E.A.H., and K.H. Analysis and interpretation of data: T.S.V., A.S., M.T.N., L.J.M., K.L., S.W.K., M.K., C.E.H., E.A.H., and K.H. Drafting of the manuscript: T.S.V., A.S., and K.H. Critical revision of the manuscript for important intellectual content: T.S.V., A.S., M.T.N., L.J.M., K.L., S.W.K., M.K., C.E.H., E.A.H., and K.H. Statistical analysis: T.S.V. Obtained funding: T.S.V.
Data sharing: Survey data are available for sharing for research purposes. Please contact the corresponding author for access.
Originally Published in Press as DOI: 10.1164/rccm.202005-1706LE on July 20, 2020
Author disclosures are available with the text of this letter at www.atsjournals.org.
References
- 1.Jacobowski NL, Girard TD, Mulder JA, Ely EW. Communication in critical care: family rounds in the intensive care unit. Am J Crit Care. 2010;19:421–430. doi: 10.4037/ajcc2010656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Griffin KM, Karas MG, Ivascu NS, Lief L. Hospital preparedness for COVID-19: a practical guide from a critical care perspective. Am J Respir Crit Care Med. 2020;201:1337–1344. doi: 10.1164/rccm.202004-1037CP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Healthcare Safety Network. Atlanta, GA: Centers for Disease Control and Prevention; 2020. COVID-19 module data dashboard – overview.https://www.cdc.gov/nhsn/covid19/report-overview.html [accessed 2020 Jun 21]. Available from. [Google Scholar]
- 4.Kotfis K, Williams Roberson S, Wilson JE, Dabrowski W, Pun BT, Ely EW. COVID-19: ICU delirium management during SARS-CoV-2 pandemic. Crit Care. 2020;24:176. doi: 10.1186/s13054-020-02882-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ely EW, Shintani A, Truman B, Speroff T, Gordon SM, Harrell FE, Jr, et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA. 2004;291:1753–1762. doi: 10.1001/jama.291.14.1753. [DOI] [PubMed] [Google Scholar]
- 6.Herridge MS, Tansey CM, Matté A, Tomlinson G, Diaz-Granados N, Cooper A, et al. Canadian Critical Care Trials Group. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med. 2011;364:1293–1304. doi: 10.1056/NEJMoa1011802. [DOI] [PubMed] [Google Scholar]
- 7.Cameron JI, Chu LM, Matte A, Tomlinson G, Chan L, Thomas C, et al. RECOVER Program Investigators (Phase 1: towards RECOVER); Canadian Critical Care Trials Group. One-year outcomes in caregivers of critically ill patients. N Engl J Med. 2016;374:1831–1841. doi: 10.1056/NEJMoa1511160. [DOI] [PubMed] [Google Scholar]
- 8.Greenberg N, Docherty M, Gnanapragasam S, Wessely S. Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ. 2020;368:m1211. doi: 10.1136/bmj.m1211. [DOI] [PubMed] [Google Scholar]
- 9.Dorn AV, Cooney RE, Sabin ML. COVID-19 exacerbating inequalities in the US. Lancet. 2020;395:1243–1244. doi: 10.1016/S0140-6736(20)30893-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Velasquez D, Mehrotra A. Health Affairs Blog. Ensuring the growth of telehealth during COVID-19 does not exacerbate disparities in care. [online ahead of print] 8 May 2020; DOI: 10.1377/hblog20200505.591306. [Google Scholar]
- 11.Pérez-Stable EJ, El-Toukhy S. Communicating with diverse patients: how patient and clinician factors affect disparities. Patient Educ Couns. 2018;101:2186–2194. doi: 10.1016/j.pec.2018.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cooper LA, Roter DL, Carson KA, Beach MC, Sabin JA, Greenwald AG, et al. The associations of clinicians’ implicit attitudes about race with medical visit communication and patient ratings of interpersonal care. Am J Public Health. 2012;102:979–987. doi: 10.2105/AJPH.2011.300558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Netzer G, Iwashyna TJ. Fair is fair: just visiting hours and reducing inequities. Ann Am Thorac Soc. 2017;14:1744–1746. doi: 10.1513/AnnalsATS.201706-471OI. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


