Highlights
-
•
During the COVID-19 outbreak, many radiologists expressed anxiety, depression and insomnia symptoms.
-
•
Working in public hospital was a major protective factor for mental issues.
-
•
Restricted access to education, past medical history and exposition to COVID-19 were common risks factor of anxiety or depression.
Abbreviations: COVID-19, Coronavirus Disease 2019; HADS, Hospital Anxiety and Depression Scale; ISI, Insomnia Severity Index
Keywords: Coronavirus, COVID-19, Radiology, Mental health, Economics
Abstract
Purpose
The COVID-19 pandemic has led to an urgent reorganisation of the healthcare system to prevent hospitals from overflowing and the virus from spreading. Our objective was to evaluate the socioeconomic and psychological impact of the COVID-19 outbreak on radiologists.
Material and methods
French radiologists were invited to answer an online survey during the pandemic through mailing lists. The questionnaire was accessible for nine days. It covered socio-demographic information, exposure to COVID-19 at work and impact on work organisation, and included the Insomnia Severity Index and Hospital Anxiety and Depression Scale. Outcomes were moderate to severe insomnia, definite symptoms of depression or anxiety. Risk and protective factors were identified through multivariate binary logistic regression.
Results
1515 radiologists answered the survey. Overall, 674 (44.5 %) worked in a highCOVID-19 density area, 671 (44.3 %) were women, and 809 (53.4 %) worked in private practice. Among responders, 186 (12.3 %) expressed insomnia, 222 (14.6 %) anxiety, and 189 (12.5 %) depression symptoms. Lack of protective equipment, increased teleradiology activity and negative impact on education were risk factors for insomnia (respectively OR [95 %CI]:1.7[1.1−2.7], 1.5[1.1−2.2], and 2.5[1.8−3.6]). Female gender, respiratory history, working in COVID-19 high density area, increase of COVID-19 related activity, and impacted education were risk factors for anxiety (OR[95 %CI]:1.7[1.2−2.3], 2[1.1−3.4], 1.5[1.1−2], 1.2[1−1.4], and 2.1[1.5−3]). Conversely, working in a public hospital was a protective factor against insomnia, anxiety, and depression (OR[95 %CI]:0.4[0.2−0.7], 0.6[0.4−0.9], and 0.5[0.3−0.8]).
Conclusions
During COVID-19 pandemic, many radiologists expressed depression, anxiety and insomnia symptoms. Working in a public hospital was a protective factor against every psychological symptom. Socio-economic impact was also major especially in private practice.
1. Introduction
Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) is a new coronavirus that has quickly spread worldwide causing COronaVIrus Disease 2019 (COVID-19). On March 11, 2020, the World Health Organization declared COVID-19 a global health emergency [1]. The first confirmed patients with COVID-19 in France were reported on January 24, 2020 and a complete lockdown was implemented by the public authorities, starting on March 17. By April 12, 95403 cases were diagnosed and 14 393 deaths reported [2]. In response to the pandemic and its high number of cases, countries had to reorganize their health systems in order to treat patients with COVID-19 while maintaining essential health care [3].
In order to avoid coronavirus dissemination, non-urgent imaging exams were suspended in both hospital departments and private practices [4,5]. The sharp decrease in radiologic activity was unprecedented with a risk of major economic impact in the short, medium and long term [4]. On the other hand, radiologists were on the front line for COVID-19 patient management. Indeed, although chest CT-scan was not recommended for COVID-19 diagnostis, it demonstrated positive performances for detecting the disease at initial presentation and could be used to triage patients in conjunction with RT-PCR (Reverse Transcriptase Polymerase Chain Reaction) [[6], [7], [8]]. Moreover, healthcare workers in radiology departments had a high virus exposure and thus a high risk of contamination for themselves but also for their family. A previous Chinese study reported that a considerable proportion of healthcare workers experienced psychological distress such as insomnia or depression due to the COVID-19 outbreak, but without specific data regarding radiology professionals [9].
We hypothesized that the COVID-19 pandemic had a profound impact on radiologists and that this impact may differ between hospital radiology departments and private practices, due to differences in organization, economic model and exposure to patients with COVID-19. The aim of our study was to assess the economic, organizational and psychological impact of COVID-19 pandemic among French radiologists.
2. Materials and methods
2.1. Study design
Approval from the Ethics Committee for Research in Imaging (CERIM) was received prior to this study. The survey was anonymous, and confidentiality of information was ensured, with no email collected. At the end of the form, a message provided mental health advice [10]. A national helpline number for psychological support for healthcare professionals was also provided.
During the COVID-19 pandemic, at the time of the fifth week of the lockdown, a self- administered anonymous survey was e-mailed to French radiologists members of the Société Française de Radiologie (SFR), the Fédération Nationale des Médecins Radiologues (FNMR), the Syndicat des Radiologues Hospitaliers (SRH), the Union Nationale des Internes de Radiologie (UNIR), and the Collège des Enseignants de Radiologie Français (CERF). These five organisations include residents and board-certified radiologists from academic and non-academic public hospitals as well as private practices. In 2018, there were 7213 board-certified radiologists including 4000 private practices in France and approximately 1250 radiology residents [11].
The questionnaire was available online from April 10 to April 19, 2020. An introductory note explained the purpose of the study and informed the participant of the ethical approval. In total, the link to the questionnaire was e-mailed three times to members in order to increase response rate. The following demographic data were first collected: age, gender, family and professional situation, location, as well as personal COVID-19 status. Then participants were questioned about changes in their work organisation and the economic impact of the pandemic. Finally, symptoms of insomnia, anxiety and depression were evaluated through validated scales.
2.2. Outcomes
Symptoms of insomnia, anxiety and depression were assessed using two validated scales: the Insomnia Severity Index (ISI) and the Hospital and Anxiety Depression Scale (HADS) [12,13]. ISI was a 7-items self-report questionnaire that assessed sleeping disorders. Each of the 7 items was rated on a 5-point Likert scale (0–4). The total score was obtained by adding the score of the 7 items and varied from 0 to 28. The total ISI score was interpreted as follows: absence of insomnia (0–7), sub-threshold insomnia (8−14), moderate insomnia (15−21), and severe insomnia (22–28). The HADS consisted of 14 questions rated from 0 to 3: seven assessing anxiety (HADS-A) and seven assessing depression (HADS-D). The HADS was chosen because it is not biased by somatic symptoms of anxiety or depression, which could have been driven by COVID-19 (e.g. fatigue, loss of appetite). Two scores were therefore obtained (one for anxiety and one for depression) ranging from 0 to 21, and were interpreted as follows: non-cases (<8), doubtful cases (8–10), definite cases (>10).
2.3. Statistical analysis
Statistical analysis was performed with RStudio© (V 1.2.5033, 2019). Figures were constructed with XlStat© (2020). Quantitative variables were described as medians and interquartile ranges (IQR) and qualitative variables as numbers and percentages. Chi-2 test and student test were performed to compare qualitative and quantitative variables respectively. The Mann-Whitney U test and the Kruskal-Wallis test were used in order to compare the severity of each score for two groups or more. Univariable binary logistic regressions were performed for each variable with symptoms of insomnia, anxiety or depression as dependent variables. When relevant, some categories for qualitative variables with multiple categories were merged to ease the interpretation of findings. For instance, regions were grouped into two categories: most versus least impacted by COVID-19 (i.e. Ile-De-France, Hauts-de-France, Grand-Est, Bourgogne Franche-Comté versus any other regions). Variables were grouped according to three conceptual domains (i.e. socio-demographic and clinical variables, exposure to COVID-19 at work, and impact of COVID-19 pandemic on work) and entered in three separate multivariable models. Variables based on subjective appraisal (e.g. “feeling of usefulness”) were not considered for the models. Relevant independent variables (i.e. age, gender and those with a p-value<0.1) were analysed with a final multivariable binary logistic regression. Finally, relevant variables Odds ratios and 95 % confidence intervals quantified the association with the risk factors for each outcome. Statistical significance was set at p < 0.05. All tests were 2-sided.
3. Results
3.1. Sociodemographic and clinical characteristics
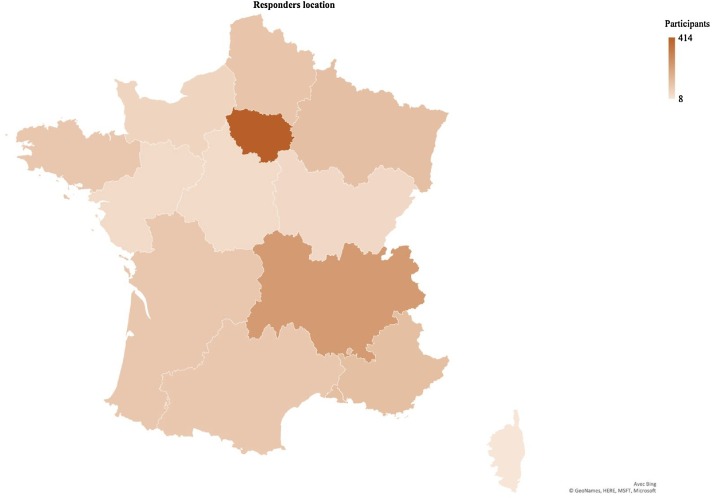
Overall, 1515 radiologists responded to the online survey (21 % response rate) (Table 1 ). Of the 1515 participants, 671 were women (44.3 %). Most participants were aged from 51 years to 60 years (26.7 %), worked in private practice (53.4 %), and were married or in a relationship (82.8 %). A total of 674 (44.5 %) worked in a region with a high rate of patients hospitalized for COVID-19 (Fig. 1, Fig. 2 ). Among the participants, 40 (2.6 %) were personally tested positive to SARS-CoV-2.
Table 1.
Sociodemographic and clinical variables.
| Characteristic | Study population (N = 1515) |
|---|---|
| Age (mean, (SD)) | 45.2 (13.3) |
| <25 years (n, (%)) | 67 (4.4) |
| 26−30 years (n, (%)) | 241 (15.9) |
| 31−40 years (n, (%)) | 319 (21.1) |
| 41−50 years (n, (%)) | 260 (17.2) |
| 51−60 years (n, (%)) | 404 (26.7) |
| >60 years (n, (%)) | 224 (14.7) |
| Gender, n (%) | |
| Women | 671 (44.3) |
| Men | 844 (55.7) |
| Marital status, n (%) | |
| Single | 261 (17.2) |
| In a relationship | 543 (35.8) |
| In a relationship with health worker | 711 (47) |
| Parenthood, n (%) | 1038 (68.5) |
| Past medical history, n (%) | |
| None | 1101 (72.7) |
| Respiratory disease | 91 (6) |
| Psychiatric disease | 66 (4.4) |
| Other diseases | 257 (16.9) |
| Professional status n (%) | |
| Junior (resident of fellow) | 397 (26.2) |
| Academic radiologist | 85 (5.6) |
| Non-academic hospital radiologist | 224 (14.8) |
| Private practice radiologist | 809 (53.4) |
Fig. 1.
Colour-coded geographical distribution of the responders.
Number of responders according to the 13 French administrative regions were colour-coded. The lowest was Corsica with 8 responders, and the highest was Ile-de-France with 414 responders.
Fig. 2.
Colour-coded geographical distribution of COVID-19 patient density.
Ratio of COVID-19 positive patients hospitalised on April 14, 2020 according to the 13 French administrative regions were colour-coded. The lowest was Brittany with 20 patients hospitalised for 100,000 persons, and the highest were Ile-de-France and Grand-Est with 233 patients hospitalised for 100,000 persons.
3.2. Exposure to COVID-19 at work
Among the participants, a slight majority (n = 809, 53.4 %) had less than 25 % of their activity related to COVID-19, had to manage severe patients (n = 913, 60.3 %), and had co-workers with COVID-19 (n = 873, 57.6 %) (Table 2 ). There were 1141 responders (75.3 %) who did not have sufficient access to protective equipment. Overall, radiologists working in public hospitals were more likely to work in a high COVID-19 density area, to have a COVID-19 related activity, to manage patients with severe COVID-19, to have co-workers with COVID-19, to fear contaminating their relatives, and less likely to have insufficient access to protective equipment (all p-values <0.001).
Table 2.
Exposure to the COVID-19 pandemic and its impact on work organisation.
| Characteristic | Study population (N = 1515) | Hospital practice (N = 706) | Private practice (N = 809) | P-value |
|---|---|---|---|---|
| Exposure to COVID-19 at work | ||||
| COVID-19 status, n (%) | 0.4 | |||
| Positive RT-PCR test/symptomatic | 171 (11.3) | 83 (11.8) | 88 (10.9) | |
| Negative RT-PCR test/asymptomatic | 1344 (88.7) | 623 (88.2) | 721 (89.1) | |
| High COVID-19 density areaa, n (%) | 674 (44.5) | 373 (52.8) | 301 (37.2) | <10−3 |
| COVID-19 related activity, n (%) | <10−3 | |||
| 0−25 % | 809 (53.4) | 259 (36.7) | 550 (68) | |
| 25−50 % | 313 (20.7) | 172 (24.4) | 141 (17.4) | |
| 50−75 % | 262 (17.3) | 182 (25.8) | 80 (9.9) | |
| >75 % | 131 (8.6) | 93 (13.1) | 38 (4.7) | |
| Management of severe patients with COVID-19, n (%) | 913 (60.3) | 592 (83.9) | 321 (39.7) | <10−3 |
| Insufficient protective equipment, n (%) | 1141 (75.3) | 452 (64) | 689 (85.2) | <10−3 |
| Infected co-workers, n (%) | 873 (57.6) | 484 (68.6) | 389 (48.1) | <10−3 |
| Fear of contaminating relatives, n (%) | 959 (63.3) | 482 (68.3) | 477 (59) | <10−3 |
| Impact of COVID-19 on work | ||||
| Percentage of activity decrease, median (IQR) | 75 (60−80) | 60 (50−75) | 80 (75−90) | <10−3 |
| >25 %, n (%) | 46 (3) | 35 (5) | 11 (1.4) | |
| 25−50%, n (%) | 304 (20) | 266 (37.7) | 38 (4.7) | |
| 50−75%, n (%) | 505 (33.4) | 288 (40.8) | 217 (26.8) | |
| >75 %, n (%) | 660 (43.6) | 117 (16.6) | 543 (67.1) | |
| Working hours, median (IQR) | 25 (16−28.3) | 36 (30−48) | 20 (10−25) | <10−3 |
| Increased teleradiology activity, n (%) | 336 (22.2) | 163 (23.1) | 173 (21.4) | 0.4 |
| Activity reassignment to other departments, n (%) | 166 (11) | 97 (13.7) | 69 (8.5) | 0.001 |
| Negative impact on education, n (%) | 463 (30.6) | 303 (42.9) | 160 (19.8) | <10−3 |
| Governmental financial aid, n (%) | NA | NA | 675 (83) | NA |
| Fear of work overload fear after crisis, n (%) | 856 (56.5) | 452 (64) | 404 (49.9) | <10−3 |
| Feeling of Usefulness, n (%) | 1055 (69.6) | 528 (74.8) | 527 (65.1) | <10−3 |
| Negative impact on non-COVID-19 patient management, n (%) | 1061 (70) | 451 (63.9) | 610 (75.4) | <10−3 |
| Impact on relations with co-workers, n (%) | ||||
| Unchanged | 627 (41.4) | 331 (46.9) | 296 (36.6) | <10−3 |
| Worse | 134 (8.8) | 67 (9.5) | 67 (8.3) | |
| Better | 235 (15.5) | 133 (18.8) | 102 (12.6) | |
| No more contact with co-workers | 519 (34.3) | 175 (24.8) | 344 (42.5) | |
| Negative economic impact for the radiology department, n (%)* | 598 (39.5) | 82 (55.8) | 516 (72) | <10−3 |
651 had no opinion.
Regions with high numbers of patients with COVID-19 and high mortality: Grand-Est, Ile-De-France, Hauts de France, Bourgogne-Franche-Comté.
3.3. Impact of COVID-19 on work organization
Overall, 1308 radiologists (86.3 %) had to decrease their activity (Table 2). There were 1061 (70 %) responders who felt concerned about the management of non COVID-19 patients. Teleradiology activity was initiated or increased for 336 (22.2 %) of them. On the other hand, 166 (11 %) had to help co-workers in other departments such as the emergency department. Although most participants (627, 41.4 %) did not express any change in their relations with co-workers, 519 (34.3 %) declared having no more contact with co-workers. Overall, 463 (30.6 %) radiologists reported that they were negatively impacted in their medical education. Finally, among private practice radiologists, 675/809 (83.4 %) received financial aid from the government.
Radiologists working in public hospitals decreased their activity less than those in private practices, had more working hours, were most likely to be reassigned to others departments, to experience a negative impact on their education, to fear a work overload after the crisis, to feel useful, and less likely to have no more contact with their co-workers and be concerned by a negative impact for the radiology structure they worked in (all p-values <0.001).
3.4. Psychological outcomes
Symptoms of insomnia, anxiety and depression were expressed by 620 (40.9 %), 513 (35 %), and 464 (30.6 %) participants, respectively (Table 3 ). Regarding levels of symptoms that may be considered clinically significant, moderate to severe insomnia and symptoms corresponding to definite cases of anxiety and depression were self-reported by 186 (12.3 %), 222 (14.6 %) and 188 (12.5 %) participants, respectively (Table 3) Radiologists working in private practice were significantly more likely to experience symptoms of insomnia and depression (p-values = 0.002 and <0.001 respectively).
Table 3.
Severity of psychological outcome scores.
| Scores | Study population N = 1515 | Private practice N = 809 | Public practice N = 706 | p-value |
|---|---|---|---|---|
| ISI (Insomnia), n (%) | 0.002 | |||
| No insomnia (<8) | 895 (59.1) | 458 (56.6) | 437 (61.9) | |
| Sub-threshold (8−14) | 434 (28.6) | 235 (29) | 199 (28.2) | |
| Moderate (15−21) | 161 (10.6) | 98 (12.1) | 63 (8.9) | |
| Severe (>28) | 25 (1.7) | 18 (2.2) | 7 (1) | |
| HAD-A (Anxiety), n (%) | 0.09 | |||
| Non cases (<8) | 984 (65) | 505 (62.4) | 479 (67.8) | |
| Doubtful cases (8−10) | 309 (20.4) | 176 (21.8) | 133 (18.8) | |
| Definite cases (>10) | 222 (14.6) | 128 (15.8) | 94 (13.3) | |
| HAD-D (Depression), n (%) | <0.001 | |||
| Non cases (<8) | 1051 (69.4) | 528 (65.3) | 523 (74.1) | |
| Doubtful cases (8−10) | 275 (18.1) | 158 (19.5) | 117 (16.6) | |
| Definite cases (>10) | 189 (12.5) | 123 (15.2) | 66 (9.4) |
3.5. Risk factors of mental health issues
For each psychological outcome (i.e. moderate to severe insomnia, definite case of anxiety, definite case of depression) and variable conceptual domains, univariable and multivariable logistic regression provided relevant variables for final multivariable binary logistic regression analysis (Supplementary Table).
The lack of sufficient protective equipment, increase of teleradiology activity and negative impact on education were risk factors for insomnia (respectively OR: 1.7, 1.5, and 2.5) (Table 4 ). Conversely, living with another healthcare worker and working in public hospitals were protective factors (respectively OR: 0.6, and 0.4). Regarding anxiety symptoms, being a female, having a previous medical history of respiratory and psychiatric disease, working in a high COVID-19 density area, having a COVID-19 related professional activity, and a negative impact on education were risk factors (respectively OR: 1.7, 2, 1.9, 1.5, 1.2, and 2.1). Similarly, radiologists with previous respiratory or psychiatric history, COVID-19 positive or symptomatic, and who were impacted in their medical education were more likely to report symptoms of depression (OR: 2.7, 2.4, 1.7, and 2.8). Finally, as for insomnia, working in a public hospital was a protective factor against anxiety and depression (OR: 0.6 and 0.5).
Table 4.
Risk factors for mental health outcomes.
| Variables | ISI score (severe), insomnia, OR (95 %CI) | HADS-A, Anxiety, OR (95 %CI) | HAD-DS, Depression OR (95 %CI) |
|---|---|---|---|
| Age (in years)a | 0.9 (0.8−1.1) NS | 0.9 (0.8−1.1) NS | 0.9 (0.8−1) NS |
| Gender | |||
| Men | 1 (reference) | 1 (reference) | 1 (reference) |
| Women | 1.2 (0.9−1.7) NS | 1.7 (1.2−2.3) ** | 1.3 (0.9−1.8) NS |
| Marital status | |||
| Single | 1 (reference) | 1 (reference) | – |
| In couple with a healthcare worker | 0.6 (0.4−0.9) * | 0.7 (0.5−1.1) NS | – |
| In couple but not with a healthcare worker | 0.7 (0.4−1.1) NS | 1.1 (0.7−1.7) NS | – |
| Past medical history | |||
| None | 1 (reference) | 1 (reference) | 1 (reference) |
| Respiratory | 1.4 (0.7−2.5) NS | 2 (1.1−3.4) * | 2.7 (1.5−4.6) *** |
| Psychiatric | 1.6 (0.5−2.4) NS | 1.9 (1.1−3.5) * | 2.4 (1.2−4.5) * |
| Others | 1.3 (0.8−2) NS | 1.4 (1−2.2) NS | 1.5 (1−2.4) NS |
| Work place | |||
| Private practice | 1 (reference) | 1 (reference) | 1 (reference) |
| Public hospital | 0.4 (0.2−0.7) *** | 0.6 (0.4−0.9) * | 0.4 (0.3−0.7) *** |
| COVID-19 status | |||
| Negative | 1 (reference) | 1 (reference) | 1 (reference) |
| Positive | 1.5 (1−2.4) NS | 1.3 (0.8−2) NS | 1.7 (1.1−2.6) * |
| COVID-19 density area | |||
| Low density | 1 (reference) | 1 (reference) | 1 (reference) |
| High densityb | 1.3 (1−1.9) NS | 1.5 (1.1−2) * | 1.4 (1−1.9) NS |
| COVID-19 related activity (in percentage)c | – | 1.2 (1−1.4) * | – |
| Protective equipment | |||
| Sufficient | 1 (reference) | 1 (reference) | 1 (reference) |
| Not sufficient | 1.7 (1.1−2.7) * | 1.4 (0.9−2) NS | 1.5 (1−2.3) NS |
| Activity decrease (in percentage)d | 1 (0.9−1) NS | 1.1 (0.9−1) NS | 1 (0.9−1) NS |
| Increased teleradiology activitye | 1.5 (1.1−2.2) * | 1.3 (0.9−1.9) NS | – |
| Impact on education | |||
| No | 1 (reference) | 1 (reference) | 1 (reference) |
| Yes | 2.5 (1.8−3.6) *** | 2.1 (1.5−3) *** | 2.8 (2−4) *** |
p-value<0.05.
p-value<0.01.
p-value<0.001; CI95= Confident Interval; NS = Not significant; OR = Odd-Ratio.
OR for 10-year incremental unit.
Regions with high numbers of patients with COVID-19 and high mortality: Grand-Est, Ile-De-France, Hauts de France, Bourgogne-Franche-Comté.
OR for 25 % incremental unit.
OR for 25 % decremental unit.
OR for 25 % incremental unit.
4. Discussion
In this study, we demonstrated the significant psychological and socio-economic impact of the COVID-19 pandemic among French radiologists, with differences according to public or private practices. The overall rate of clinically significant levels of insomnia, anxiety or depression symptoms was high in the study population, with identified risk factors such as COVID-19 exposure, or personal medical history, but also protective factors such as working in a public hospital.
Relatively high levels of psychological symptoms have already been reported among radiologists. For instance, symptoms of burnout are common among radiologists, who ranked seventh among all physicians in 2015 vs. 18th in 2013 [14]. In a survey published in 2015, 49 % of radiologists had symptoms of burnout [15]. In a survey among 1300 physicians, Ramirez et al. demonstrated that although radiologists had the lowest scores on stress factors, they had the worst satisfaction scores and reported highest levels of burnout with regards to feelings of low personal accomplishment [16]. Radiologists’ burnout could be explained by their role as a clinical support service with a relative lack of positive feedback from patients or colleagues. Indeed, Magnavita et al. reported that anxiety and depression symptoms were significantly higher among radiologists who were aware of a reward/effort imbalance [17]. One should therefore interpret psychological symptoms measured in the context of the COVID-19 in the light of these pre-existing levels of psychological symptoms.
Exposure or fear of exposure to the virus were important risk factors of psychiatric symptoms. Indeed, working in a high COVID-19 density area, lack of protective equipment, and COVID-19 related activity were significant factors of mental health issues. In these areas, hospitals were reorganised around the management of patients with COVID-19: non-urgent and non-oncological radiologic activities were stopped, and physicians were reallocated to departments managing only patients with COVID-19. As a consequence, physicians were exposed to an increased risk of contamination. These results are in line with Lai et al. who demonstrated that healthcare workers reported more severe psychological symptoms when they worked in Wuhan city, epicenter of the pandemic in China [9]. In addition, more than 70 % of the responders reported a lack of access to protective equipment at work, and this shortage has been reported worldwide [18]. Absence of efficient protection equipment was an insomnia risk factor, as evidenced in previous studies [19].
Psychological distress was also associated with individual factors such as COVID-19 positive status and medical history of respiratory illness. Indeed, threat perception could be intensified for these respondents and reflect their fear of being exposed to the virus or exposing their relatives, as well as a perceived risk of more severe symptoms [20]. A previous study indicated that distress could be related to feelings of vulnerability or loss of control and personal health concerns [21]. This feeling may be accentuated by the media-related information that in China, about 3000 healthcare workers have been infected and at least 22 have died [22].
In this study, radiologists working in private practice were more strongly impacted than public hospital radiologists. First, the activity decrease was more important for them (a majority had >75 % activity decrease). This was due to the cancellation of all’ non-urgent’ medical activities, the complete lockdown and limited access to protective equipment (especially at the beginning of the pandemic) for both radiologists and patients. This drop in activity represents an economic risk, especially for many private practices that had to close and reported a 70 % drop in turnover [23]. However, the association of psychological symptoms with public hospital versus private practice remained significant in the multivariable analysis while activity decrease did not. A large majority of radiologists working in private practice have been able to rely on government financial support as seen in our results. This unprecedented economic crisis, the duration and intensity of which remains unknown to date, may have long-term repercussions with possible closure of some private practices [4]. This difference between radiologist in hospital and private practices can also be explained by the insufficient equipment, a lesser feeling of usefulness (though not statistically significant), and a feeling of isolation (43 % with no more contact with co-workers). The apparent protective effect of working in public hospitals may conversely be related to the more frequent feeling of usefulness for hospital radiologists. Different occupational stress models suggest that the impact of constraints on mental health can be offset by increased rewards [24]. Among these, the societal praise of care work provided by hospital workers appears as a possible short-term protective factor. Working in a public hospital may also have resulted in more frequent opportunities for radiologists to receive logistic support from their institution as well as psychological support from their colleagues and/or dedicated services [10].
Given that radiologists are a population at risk to develop stress at work as has been demonstrated in several studies, our findings would drive to implement protective measures [16]. Radiologists working in private practice, in a high COVID-19 density area, managing patients with COVID-19 and with past medical history seemed to be the most at risk and should be closely monitored. Access to medical education via webinar or e-learning should be emphasized [25].
This study has some strengths, including the large sample size, the wide array of variables considered, and the span of different regions, levels of education or types of practice that were represented in the cohort. This study also has limitations. First, the response rate was low (21 % of French radiologists) limiting the generalisability of our results regarding our descriptive aims. Second, surveys have inherent limitations related to the biases that may affect self-report (e.g. social desirability bias). Confidentiality and the use of validated scales should minimise this possible bias. Third, our study lacks pre-pandemic data so we could not estimate the extent to which the levels of psychological symptoms increased in the context of the COVID-19 pandemic. Finally, the study was carried out during 10 days and lacks longitudinal follow-up. The long-term impact of the outbreak among radiologists remains unknown and will require further investigation.
5. Conclusion
We reported a rate of over one third of depression, anxiety and insomnia symptoms among radiologists in France during the acute crisis of the COVID-19 pandemic. This study also demonstrated major socio-economic impacts especially in private practices linked to psychological outcomes.
CRediT authorship contribution statement
Marie Florin: Conceptualization, Methodology, Investigation, Writing - original draft. Ugo Pinar: Investigation, Writing - original draft, Formal analysis. Eric Chavigny: Investigation, Writing - original draft. Mehdi Bouaboula: Investigation, Writing - original draft. Lamia Jarboui: Investigation, Writing - original draft. Adamfa Coulibaly: Investigation, Writing - original draft. Cédric Lemogne: Conceptualization, Methodology, Writing - original draft, Supervision. Laure Fournier: Conceptualization, Methodology, Writing - original draft, Supervision.
Declaration of Competing Interest
The authors report no declarations of interest.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.ejrad.2020.109285.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- 1.Mahase E. China coronavirus: WHO declares international emergency as death toll exceeds 200. BMJ. 2020;368:m408. doi: 10.1136/bmj.m408. [DOI] [PubMed] [Google Scholar]
- 2.DICOM_astreinte . Ministère des Solidarités et de la Santé; 2020. DICOM_astreinte, Communiqué de presse du 12 avril 2020.http://solidarites-sante.gouv.fr/actualites/presse/communiques-de-presse/article/communique-de-presse-du-12-avril-2020 (Accessed April 17, 2020) [Google Scholar]
- 3.2020. Coronavirus (COVID-19) Events as They Happen. (n.d.). https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen (accessed April 17, 2020) [Google Scholar]
- 4.Cavallo J.J., Forman H.P. The economic impact of the COVID-19 pandemic on radiology practices. Radiology. 2020 doi: 10.1148/radiol.2020201495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Levine R. 2020. Society of Breast Imaging Statement on Breast Imaging During the COVID-19 Pandemic; p. 1. (n.d.) [Google Scholar]
- 6.Fang Y., Zhang H., Xie J., Lin M., Ying L., Pang P., Ji W. Sensitivity of chest CT for COVID-19: comparison to RT-PCR. Radiology. 2020 doi: 10.1148/radiol.2020200432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bai H.X., Hsieh B., Xiong Z., Halsey K., Choi J.W., Tran T.M.L., Pan I., Shi L.-B., Wang D.-C., Mei J., Jiang X.-L., Zeng Q.-H., Egglin T.K., Hu P.-F., Agarwal S., Xie F., Li S., Healey T., Atalay M.K., Liao W.-H. Performance of radiologists in differentiating COVID-19 from viral pneumonia on chest CT. Radiology. 2020 doi: 10.1148/radiol.2020200823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kanne J.P., Little B.P., Chung J.H., Elicker B.M., Ketai L.H. Essentials for radiologists on COVID-19: an update-radiology scientific expert panel. Radiology. 2020 doi: 10.1148/radiol.2020200527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N., Wu J., Du H., Chen T., Li R., Tan H., Kang L., Yao L., Huang M., Wang H., Wang G., Liu Z., Hu S. Factors associated with mental health outcomes among health care workers exposed to Coronavirus Disease 2019. JAMA Network Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.3976. e203976–e203976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.El-Hage W., Hingray C., Lemogne C., Yrondi A., Brunault P., Bienvenu T., Etain B., Paquet C., Gohier B., Bennabi D., Birmes P., Sauvaget A., Fakra E., Prieto N., Bulteau S., Vidailhet P., Camus V., Leboyer M., Krebs M.-O., Aouizerate B. Les professionnels de santé face à la pandémie de la maladie à coronavirus (COVID-19): quels risques pour leur santé mentale? L’Encéphale. 2020 doi: 10.1016/j.encep.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pruvo J., Aucant D., Bartoli J., Beroud P., Beregi J., Boudghene F., Boyer L., Carsin M., Cart P., Claudon M., Dehaene J., Delesalle J., Devred P., Dion E., Frija G., Grenier N., Grenier P., Helenon O., Krause D., Leclerc X., Legman M., Luciani A., Masson J., Meder J., Moulin G., Nahum H., Neuenschwander S., Niney J., Rahmouni A., Rymer R., Silberman B., Soyer P., Taieb A., Thomassin I., Verzaux L., Vilgrain V., Zins M., Naggara O., Pontana F., Ladoux A., Edjlali M., Folhen A., Ohana M., Marco L.D., Dangouloff-Ross V., Jaques T., Bendrihem R., Koumako C., Wu C., Baudoin S., Brige S., Farhra P., Husson R., Kabbaj M., Masson C., Philippe M., Puche D., Remond J., Rose C., Simonnet J., Vincent W., Voix F., Yvanoff I. 2020. Démographie médicale Imagerie en 2019 Télé-radiologie Economie de santé; p. 135. (n.d.) [Google Scholar]
- 12.Bastien C.H., Vallières A., Morin C.M. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2:297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 13.Zigmond A.S., Snaith R.P. The hospital anxiety and depression scale. Acta Psychiatry Scand. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 14.Harolds J.A., Parikh J.R., Bluth E.I., Dutton S.C., Recht M.P. Burnout of radiologists: frequency, risk factors, and remedies: a report of the ACR commission on human resources. J. Am. Coll. Radiol. 2016;13:411–416. doi: 10.1016/j.jacr.2015.11.003. [DOI] [PubMed] [Google Scholar]
- 15.2020. Medscape Radiologist Lifestyle Report 2015. (n.d.). https://www.medscape.com/features/slideshow/lifestyle/2015/radiology (Accessed August 9, 2020) [Google Scholar]
- 16.Ramirez A.J., Graham J., Richards M.A., Cull A., Gregory W.M. Mental health of hospital consultants: the effects of stress and satisfaction at work. Lancet. 1996;347:724–728. doi: 10.1016/s0140-6736(96)90077-x. [DOI] [PubMed] [Google Scholar]
- 17.Magnavita N., Fileni A. Association of work-related stress with depression and anxiety in radiologists. Radiol. Med. 2014;119:359–366. doi: 10.1007/s11547-013-0355-y. [DOI] [PubMed] [Google Scholar]
- 18.Cheng V.C.C., Lau S.K.P., Woo P.C.Y., Yuen K.Y. Severe acute respiratory syndrome coronavirus as an agent of emerging and reemerging infection. Clin. Microbiol. Rev. 2007;20:660–694. doi: 10.1128/CMR.00023-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shanafelt T., Ripp J., Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA. 2020 doi: 10.1001/jama.2020.5893. [DOI] [PubMed] [Google Scholar]
- 20.Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y., Ren R., Leung K.S.M., Lau E.H.Y., Wong J.Y., Xing X., Xiang N., Wu Y., Li C., Chen Q., Li D., Liu T., Zhao J., Liu M., Tu W., Chen C., Jin L., Yang R., Wang Q., Zhou S., Wang R., Liu H., Luo Y., Liu Y., Shao G., Li H., Tao Z., Yang Y., Deng Z., Liu B., Ma Z., Zhang Y., Shi G., Lam T.T.Y., Wu J.T., Gao G.F., Cowling B.J., Yang B., Leung G.M., Feng Z. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N. Engl. J. Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wong T.W., Yau J.K.Y., Chan C.L.W., Kwong R.S.Y., Ho S.M.Y., Lau C.C., Lau F.L., Lit C.H. The psychological impact of severe acute respiratory syndrome outbreak on healthcare workers in emergency departments and how they cope. Eur. J. Emerg. Med. 2005;12:13–18. doi: 10.1097/00063110-200502000-00005. [DOI] [PubMed] [Google Scholar]
- 22.Critical Care Medicine | JAMA | JAMA Network; 2020. Supporting the Health Care Workforce during the COVID-19 Global Epidemic. (n.d.). https://jamanetwork.com/journals/jama/fullarticle/2763136 (Accessed April 17, 2020) [DOI] [PubMed] [Google Scholar]
- 23.2020. COVID-19 : la FNMR publie une lettre ouverte à l’attention du Ministre. (n.d.). http://www.thema-radiologie.fr/actualites/2619/covid-19-la-fnmr-publie-une-lettre-ouverte-a-l-attention-du-ministre.html (Accessed April 17, 2020) [Google Scholar]
- 24.Siegrist J. Adverse health effects of high-effort/low-reward conditions. J. Occup. Health Psychol. 1996;1:27–41. doi: 10.1037//1076-8998.1.1.27. [DOI] [PubMed] [Google Scholar]
- 25.Lewis P.J., Catanzano T.M., Davis L.P., Jordan S.G. Web-based conferencing: what radiology educators need to know. Acad. Radiol. 2020;27:447–454. doi: 10.1016/j.acra.2019.05.017. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.