Abstract
Background and Objectives
This review synthesizes the current literature surrounding chronic disease outcomes after weather- and climate-related disasters among older adults. The associations between exposure of older adults to weather- and climate-related disasters and the primary outcomes of diabetes, end-stage renal disease (ESRD), congestive heart failure (CHF), and chronic obstructive pulmonary disease (COPD) were examined.
Research Design and Methods
A systematic review of studies reporting on clinical outcomes of four chronic diseases after disaster exposure was performed. Under the direction of an informationist, the databases PubMed, Scopus, EMBASE, and Web of Science (Science and Social Science Citation Index) were searched from inception to July 2019.
Results
Of 5,229 citations identified, 17 articles met the study criteria. Included articles were retrospective observational in nature and focused on earthquakes (24%, n = 4), hurricane (41%, n = 7), and wildfire (35%, n = 6) disasters. Outcome data by disease process included COPD (35%, n = 6), ESRD (41%, n = 7), CHF (24%, n = 4), and diabetes (29%, n = 5). Three main categories were identified: access to health care, postdisaster health care utilization, and study rigor. The age-stratified analyses reported in this review found multiple instances where disasters have limited or insignificant effects on older adults relative to younger populations.
Discussion and Implications
Disaster research faces unique methodological challenges, and there remains a need for data-driven conclusions on how best to care for older adults before, during, and after disasters. To encourage consistent dialogue among studies, we advocate for the use of rigorous and standardized scientific methodology to examine the health impacts of disasters on adults with chronic disease.
Keywords: Multiple chronic conditions, Emergency planning, Health services for the aged
Weather- and climate-related disasters have become more frequent and more severe, increasing by almost 50% worldwide since the year 2000 (Watts et al., 2018). The United States in particular has been affected by historic storms and wildfires in the past 3 years. The impact of these disasters is expected to continue to increase in response to a changing climate (Watts et al., 2018). With increasing numbers of disasters come increasing disaster recovery, at enormous cost. In 2018, 14 separate billion-dollar disaster events occurred, and 16 disasters occurred in 2017 where total costs exceeded $300 billion, setting a new U.S. annual record (National Centers for Environmental Information, 2019). Among the costs of disaster recovery are those associated with health and health care. Disasters affect ongoing health conditions, contribute to new health concerns, and disrupt access to health care. All of these can complicate and exacerbate existing health conditions.
During any disaster, older adults may be particularly vulnerable. Older adults experience interruptions in health care when disasters destroy or prevent access to infrastructure and/or cause evacuations or relocations. For example, in 2012, Hurricane Sandy forced over 31 nursing homes to close and 4,500 older adult residents to evacuate (Office of Emergency Management, 2014). Disproportionate outcomes, including an increased risk of death, have been reported among older adults for a variety of physiological and mental health outcomes across multiple disaster settings, including Hurricanes Sandy, Rita, and Katrina, as well as the Great East Japan Earthquake (Cherry et al., 2011; Cherry et al., 2017; Klinenberg, 2015; Tanji et al., 2017).
Critically, up to 81% of older adults in the United States are currently diagnosed with multiple chronic conditions (Buttorff, Ruder, & Bauman, 2017). Because older adults with chronic conditions use health care services more frequently, an interruption of care could further exacerbate disproportionate outcomes for this population. Understanding the health needs of older adults with and without chronic conditions before, during, and after disasters as well as the effect of a disaster on health outcomes (and the factors that may mitigate them) for older adults with chronic health conditions remains a great need. Therefore, the purpose of this systematic review is to synthesize and categorize existing research that describes associations between weather- and climate-related disasters and four types of chronic diseases: congestive heart failure (CHF), chronic obstructive pulmonary disease (COPD), end-stage renal disease (ESRD), and diabetes.
Definitions
Disaster
Disasters were defined using the International Federation of Red Cross and Red Crescent Societies (2017) definition of “a sudden, calamitous event that seriously disrupts the functioning of a community or society and causes human, material, and economic or environmental losses that exceed the community’s or society’s ability to cope using its own resources,” and further limited to weather- and climate-related disasters.
Chronic Disease
Outcomes associated with one of the four chronic conditions of interest were studied: COPD, CHF, ESRD, and type 2 diabetes (diabetes). Although numerous chronic conditions could be studied, these were chosen based on both clinical relevance and literature review as previous studies have suggested these conditions are exacerbated by disasters (Fonseca et al., 2009; Foster et al., 2011; Kobayashi et al., 2013; Rappold et al., 2012).
Older Adults
Older adults were defined as adults aged 65 or older (Office of Disease Prevention and Health Promotion, 2017).
Methods
This review follows the reporting guidelines and criteria specified in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) and was registered in the PROSPERO Database (registration number CRD42017065128). For the purposes of this review, we examined the associations between older adults, disasters, and the primary outcomes measures of four selected chronic diseases. We were also interested in examining principal summary measures used, specifically effect size.
Inclusion and Exclusion Criteria
The study inclusion criteria were as follows:
(1) Studies that met the definition for weather- and climate-related disaster as detailed earlier were included. Heat waves were excluded from this study, due to a lack of a consensus definition.
(2) Studies examining any of the four chronic conditions were included CHF, COPD, ESRD, and diabetes. Broader categories, such as “all chronic diseases” or “all respiratory diseases,” were excluded.
(3) Studies reporting data on adults aged 65 or older were included. Studies investigating outcomes that did not specifically study older adults or that did not report separate data on older adults aged 65 years and older were excluded.
(4) Original, peer-reviewed journal articles including those using qualitative or quantitative methods such as cross-sectional, prospective, and retrospective cohort, and case–control designs were included. Systematic reviews and meta-analyses, theses, dissertations, books and book chapters, conference papers and presentations, and conference proceedings and abstracts were excluded, as were letters to the editor and case studies.
(5) No date restrictions were applied.
(6) Only English-language articles were included.
Search Strategy and Data Extraction
With the support and guidance of a health informationist, an initial systematic search of the following databases from inception to April 2019, was conducted: PubMed, Scopus, Embase, and Web of Science (Science and Social Science Citation Index). A Google Scholar search was also initiated but did not yield additional, nonduplicate results. The search strategies are detailed in Supplementary Appendix 1. Prior to submission in July 2019, the search was rerun, but did not yield additional articles for conclusion.
Search results were imported into the systematic review software system (Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia). Three reviewers (S.A.B., J.H., and C.T.) independently screened all titles and abstracts to assess eligibility for inclusion according to the criteria listed earlier. The full text of articles passing initial title and abstract screening were further assessed for inclusion using the same criteria by the same three reviewers. The reference lists of articles included were subsequently hand-searched but did not lead to further articles for inclusion.
Data from the included studies were independently entered into a standardized extraction template, based on the Cochrane Public Health Group’s (2018 data extraction template. For all studies, the following information was extracted: study design, objectives, geographic location, setting, inclusion criteria, method of participant selection, sample size, participant age, study design, type of disaster, type of chronic disease, primary outcome, and secondary outcomes. In addition, for each study, reviewers independently assessed and categorized the studies into groups by types of outcomes and themes. This tool is included in Supplementary Appendix 2.
Assessment of Study Quality
Assessment of study quality was performed using two instruments specific for observational studies; the Newcastle-Ottawa Quality Assessment for Cohort Studies (NOS) and the National Heart, Lung and Blood Institute’s (NHLBI) Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies. The NOS scale, recommended by The Cochrane Collaboration (2011), evaluates risk of bias of cohort studies within three domains: selection, comparability, and outcomes (Stang, 2010). Studies can be given up to one star (or point) for each numbered item within the selection and outcome categories, and a maximum of two stars for comparability. The NHLBI Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies was used as a second measure of quality assessment (National Heart Lung and Blood Institute [NHLBI], 2014). This tool measures 14 different criteria that used to give each study an overall quality rating of good, fair, or poor (Harris, Moniz, Iott, Power, & Griggs, 2016). Two reviewers (S.A.B. and J.H.) independently applied the NOS tool to each study. In case of disagreement, a consensus was reached through a discussion.
Results
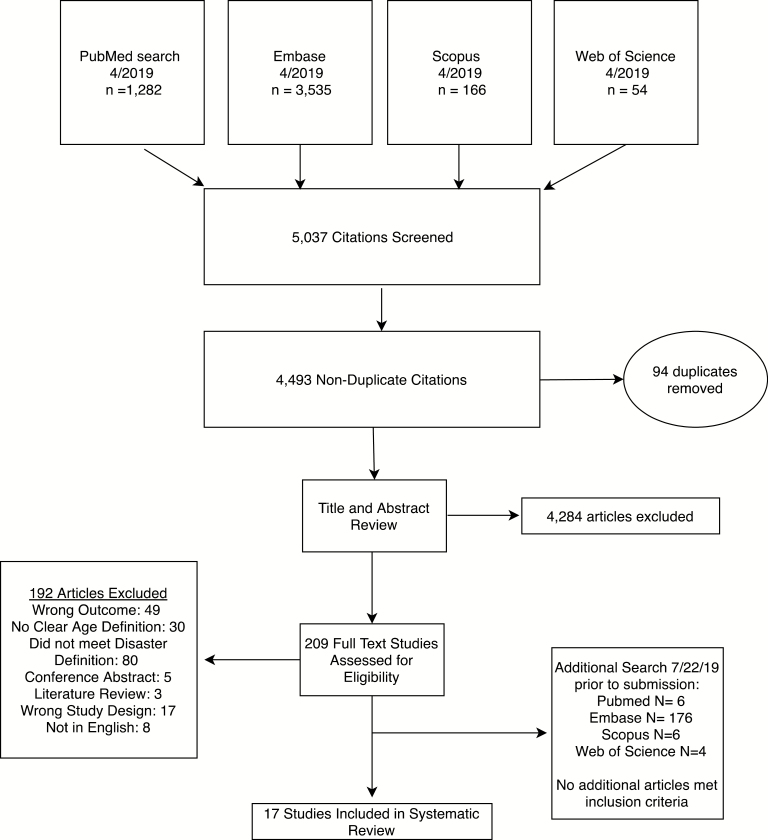
An initial search in April of 2019 found total of 5,037 titles were screened for study inclusion. After 94 duplicates were deleted, 4,284 articles were excluded on title and abstract review, leaving 209 full-text articles, which were further assessed for inclusion. After full-text review, 17 articles met the inclusion criteria and were included in the study. Table 1 summarizes the study design, sample description, and conclusions relevant to this review for each of the 17 studies. An additional search was performed prior to submission in July 2019, yielding 192 articles, of which none met the criteria for inclusion.
Table 1.
Description of Included Studies
| Author (year) | Purpose | Study design | Disease state studied | Type of disaster | Sample size and description | Findings specific to outcomes of interesta |
|---|---|---|---|---|---|---|
| Kirizuka et al. (1997) | Examine whether an earthquake disturbs glycemic control in diabetic patients | Cohort analysis | Diabetes | Earthquake | Diabetic patients in Japan (n = 177) | HbA1c levels for patients increased from 7.74% (± 1.82) before the earthquake to 8.34% (± 2.07), p < .01 ~2 mo after earthquake. |
| Nishikawa et al. (2015) | Assess the effect of an earthquake on diabetes outpatient care | Cohort analysis | Diabetes (type 2) | Earthquake | Diabetic patients in Japan (n = 575) | No significant differences in mean HbA1c levels were observed among disaster-affected patients with type 2 diabetes. |
| Ohkouchi et al. (2013) | Examine long-term health effects and exacerbations of existing conditions associated with the East Japan Earthquake | Cohort analysis | COPD | Earthquake | Patients admitted to respiratory units Hospital in Japan from March 11 to April 10, 2010 (n = 447) and also from March 11 to April 10, 2011 (n = 1,223) | COPD exacerbations were 2.5 times higher from March to April in the earthquake year (2011) than the year before. |
| Sugisawa et al. (2017) | Explore factors related to earthquake preparedness in Japanese hemodialysis patients | Cross-sectional | ESRD | Earthquake | Chronic kidney disease patients in Japan (n = 1,841) | Patients with higher social support from family (OR 1.080 [95% CI 1.029, 1.132], p = .002) and friends (OR 1.078 [95% CI 1.042, 1.115], p = .001) scored higher on earthquake preparedness measure. |
| Anderson et al. (2009) | Examine the extent of missed dialysis sessions after Hurricane Katrina and the factors that contributed missed sessions | Cross-sectional | ESRD | Hurricane | Hemodialysis patients near New Orleans, LA (n = 386) | Adults aged 65 or over were less likely to miss 1–2 dialysis sessions after disaster than participants younger than 50 (OR 2.44 [95% CI 1.21, 4.95]). |
| Gotanda et al. (2015) | Evaluate older adults’ emergency department and hospital use in lower Manhattan after Hurricane Sandy | Cohort analysis | Overall ED usage | Hurricane | ED visits (n = 3513) and hospitalizations (n = 940) to Beth Israel Medical Center (New York, NY) between May 7, 2012 and April 28, 2013. (Sample size given for pre-Sandy and immediately post-Sandy time periods.) | ED visits and hospital admissions for dialysis-related concerns increased across all age groups studied (18–64, 65–79, and 80+), p < .05 |
| Hyre et al. (2007) | Assess PTSD symptoms and dialysis-related factors (among others) after Hurricane Katrina landfall | Cross-sectional | ESRD | Hurricane | Hemodialysis patients near New Orleans, LA (n = 391) | 24% of patients experienced PTSD, with no significant differences observed for adults aged 50–64 (adj. prevalence ratio 1.24 [95% CI 0.87, 1.77]) or 65+ (adj. prevalence ratio 1.00 [95% CI 0.65, 1.54]) with respect to adults younger than 50. |
| Lee et al. (2016) | Assess geographic distribution and postdisaster medical needs of different Hurricane Sandy evacuation zones | Cohort analysis | Diabetes | Hurricane | ED visits in New York City in 2012 (n = 50,996 records pre-hurricane, n = 46,131 post-hurricane) | Following Hurricane Sandy landfall, the proportion of adults aged 65+ that visited the ED with a secondary diagnosis of diabetes increased from 50% to 60% (p < .01). |
| Lurie et al. (2015) | Evaluate outcomes for ESRD patients who received early dialysis before Hurricane Sandy | Cohort analysis | ESRD | Hurricane | Hemodialysis patients in New York City and New Jersey (n = 13,836) | Patients undergoing early dialysis before the hurricane were less likely to visit the ED (OR 0.75 [95% CI 0.63, 0.89]) or be hospitalized (OR 0.77 [95% CI 0.65, 0.92]) during the week of the hurricane than patients who did not undergo early dialysis. |
| Malik et al. (2018) | Evaluate the acute impact of disasters on diabetic patients using the ED | Cohort analysis | ED visits | Hurricane | ED visits in 2012 before and after Hurricane Sandy (sample size not reported) | Medicare patients presenting to an ED with a primary diagnosis of diabetes increased proportionately (from 41% to 55%, p = .04). |
| Sharma et al. (2008) | Characterize ED visits for chronic disease conditions at emergency departments after Hurricane Katrina | Cross-sectional | ESRD/diabetes | Hurricane | ED visits in hospitals near New Orleans, LA, from September 8 to October 22, 2005 (n = 21673 ED visits) | After Hurricane Katrina, (i) renal failure accounted for 2.5% of ED visits among all patients; (ii) renal failure accounted for 14% of ED visits by adults aged 80 or older; and (iii) diabetic concerns accounted for 7% of ED visits by adults aged 80 or older. |
| Delfino et al. (2009) | To evaluate the relationship of cardiorespiratory outcomes to wildfire-related particulate matter (PM2.5) during California wildfires in October 2003 | Cohort analysis | COPD/CHF | Wildfire | Hospital admissions in southern California, from October 1 to November 15, 2003 (n = 40,856 visits) | COPD-related hospital admissions were smaller for adults aged 65 and older (3%, no CI reported) compared with adults aged 20–64 (7% [95% CI 0.9, 13.1]). |
| Mott et al. (2005) | To determine the effects of wildfires on cardiorespiratory hospitalizations and re-admissions, and to examine longer-term health effects | Cohort analysis | COPD/CHF | Wildfire | Hospitalization records in the Kuching region of Malaysia from January 1, 1995 to December 31, 1998 (n = 190,016). | Wildfire was associated with a smaller increase in COPD-related ED visits for those aged 65+ (42%) versus 50% for patients aged 40–64. |
| Parthum et al. (2017) | Geospatially analyze public health outcomes related to wildfire smoke | Cohort analysis | COPD/CHF | Wildfire | ED visits in the Tidewater region of Virginia from June 9 to October 13, 2008 (n = 548) | Wildfire was associated with increased likelihood of COPD-related (cRR 1.73 [95% CI 1.06, 2.83] for adults 18+ [65+ not specifically reported]) and CHF-related (cRR 1.37 [95% CI 1.01, 1.85] for adults 65+, 18–64 not studied) ED visits in exposed counties during the wildfire. |
| Rappold et al. (2011) | Investigate health effects associated with air pollution from wildfires | Cohort analysis | COPD/CHF | Wildfire | ED visits in North Carolina, USA between June 1 and July 14, 2008 | COPD results for adults aged 65+ (cRR 1.48 [95% CI 0.74, 2.97]) and CHF results for both age groups (cRR 1.34 [95% CI 0.78, 2.32] and 1.29 [95% CI 0.89, 1.87], respectively) were not significant. Adults younger than 65 had increased COPD outcomes (cRR 2.02 [95% CI 1, 4.05]) in wildfire-exposed counties compared with referent counties. |
| Reid et al. (2016) | Examine the effects of long wildfire exposure on cardiorespiratory outcomes interpreted across geography and time | Cohort analysis | COPD/CHF | Wildfire | 102,311 hospitalizations and ED visits in northern California from May 6 to September 15, 2008 | A 5 µg/m3 increase in PM2.5 emissions from wildfire was associated with an overall increase in COPD-related ED visits (RR 1.022 [95% CI 1.006, 1.039]), significant for adults aged 20–64 (RR 1.062 [95% CI 1.033, 1.092]), but not for adults 65+ (RR 1.002 [95% CI 0.979, 1.026]). |
| Tinling et al. (2016) | Examine the relationship between cardiorespiratory outcomes and wildfire smoke exposure in an attempt to replicate a previous study on a similar fire | Cohort analysis | COPD/CHF | Wildfire | ED visits in 28 North Carolina counties between May 5 and June 19, 2011 (57,650 records) | No significant association was observed in older adults between COPD and PM2.5 [cRR 0.92 (95% CI 0.83, 1.02)] or between CHF and PM2.5 (cRR 0.92 [95% CI 0.84, 1.01]). |
Notes: CI = confidence interval; cRR = cumulative relative risk; ED = emergency department; OR = odds ratio; PM2.5 = particulate matter ≤ 2.5 µm in diameter. aEffect size reported when available.
Study Characteristics
Most studies included in this sample were published either between 2011 and 2015 (29%, n = 5) or between 2016 and present time (35%, n = 6). Multiple study designs were employed, though all were retrospective and observational in nature. The United States was the primary setting (71%, n = 12). Effect sizes reported include odds ratios (18%, n = 3), relative risk (18%, n = 3), cumulative relative risk (12%, n = 2), z-scores (12%, n = 2), and single studies reporting prevalence ratios, regression coefficients, and prediction intervals. In 24% of studies (n = 4), descriptive or bivariate statistics only were reported. Four studies (24%) were survey based, and the remainder used existing data. The PRISMA diagram that details the full selection process is in Figure 1. Table 1 presents relevant characteristics of each study.
Figure 1.
PRISMA diagram.
Quality Assessment
Using the NHLBI Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies, we rated 15 studies at a “good” quality rating and 2 studies at a “fair” quality rating. Using the Newcastle-Ottawa Quality Assessment, we rated 16 of 17 studies as “good” and one as “fair.” All studies used either survey instruments or administrative health data sets. A key differentiating factor was a lack of reporting of confounding variables. No studies reported a sample size justification or randomization, making selection bias across studies a potential concern (see Tables 2 and 3 for quality assessment).
Table 2.
Critical Appraisal Using NHLBI Quality Assessment Tool for Observational Cohort and Cross-sectional Studies
| Author (year) | Research question stated | Study population defined | Inclusion/exclusion stated | Sample size justification | Timeframe sufficient | Exposure measures defined | Outcome measures clearly defined | Confounding variables measured and adjusted | Quality rating |
|---|---|---|---|---|---|---|---|---|---|
| Kirizuka et al. (1997) | No | Yes | Yes | No | Yes | Yes | Yes | Yes | Fair |
| Nishikawa et al. (2015) | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Good |
| Ohkouchi et al. (2013) | Yes | No | No | No | Yes | Yes | Yes | No | Fair |
| Sugisawa et al. (2017) | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Good |
| Anderson et al. (2009) | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Good |
| Gotanda et al. (2015) | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Good |
| Hyre et al. (2007) | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Good |
| Lee et al. (2016) | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Good |
| Lurie et al. (2015) | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Good |
| Malik et al. (2018) | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Good |
| Sharma et al. (2008) | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Good |
| Delfino et al. (2009) | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Good |
| Mott et al. (2005) | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Good |
| Parthum et al. (2017) | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Good |
| Rappold et al. (2011) | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Good |
| Reid et al. (2016) | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Good |
| Tinling et al. (2016) | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Good |
Table 3.
NOS Tool Critical Appraisal
| Author (year) | Selection | Comparability | Outcome | Quality rating | |||
|---|---|---|---|---|---|---|---|
| Representativeness of the exposed cohort | Ascertainment of the exposure | Outcome not present at start of study | Study controls applied and reported | Assessment of the outcome | Statistical tests appropriate | ||
| Kirizuka et al. (1997) | No | Yes | Yes | Yes | Yes | Yes | Good |
| Nishikawa et al. (2015) | No | Yes | Yes | Yes | Yes | Yes | Good |
| Ohkouchi et al. (2013) | No | Yes | Yes | No | Yes | No | Fair |
| Sugisawa et al. (2017) | No | Yes | Yes | Yes | Yes | Yes | Good |
| Anderson et al. (2009) | No | Yes | Yes | Yes | Yes | Yes | Good |
| Gotanda et al. (2015) | No | Yes | Yes | Yes | Yes | Yes | Good |
| Hyre et al. (2007) | No | Yes | Yes | Yes | Yes | Yes | Good |
| Lee et al. (2016) | No | Yes | Yes | Yes | Yes | Yes | Good |
| Lurie et al. (2015) | No | Yes | Yes | Yes | Yes | Yes | Good |
| Malik et al. (2018) | No | Yes | Yes | Yes | Yes | Yes | Good |
| Sharma et al. (2008) | No | Yes | Yes | No | Yes | No | Good |
| Delfino et al. (2009) | No | Yes | Yes | Yes | Yes | Yes | Good |
| Mott et al. (2005) | No | Yes | Yes | Yes | Yes | Yes | Good |
| Parthum et al. (2017) | No | Yes | Yes | Yes | Yes | Yes | Good |
| Rappold et al. (2011) | No | Yes | Yes | Yes | Yes | Yes | Good |
| Reid et al. (2016) | No | Yes | Yes | Yes | Yes | Yes | Good |
| Tinling et al. (2016) | No | Yes | Yes | Yes | Yes | Yes | Good |
Types of Disasters
Although any disaster meeting the study definition could be included in this review, the included articles that met study criteria focused on earthquakes (24%, n = 4), hurricanes (41%, n = 7), and wildfires (35%, n = 6).
Health Outcomes by Condition
Of the 17 included studies, data were available on ESRD (41%, n = 7), COPD (35%, n = 6), diabetes (29%, n = 5), and CHF (24%, n = 4). Several studies included analysis on multiple diseases. Across reviewed studies, only one study focused exclusively on older adults. See Table 1 for more detailed characteristics of the included studies.
A majority of studies (53%, n = 9), used ICD-9 codes to classify outcomes. All studies for CHF were coded using international classification of disease code version-9 (ICD-9) code number 428 (heart failure); one also used 402 (hypertensive heart disease) as a secondary code. All of the U.S.-based studies evaluating COPD in this review used ICD-9 codes, although variability in how COPD was defined existed. Two studies limited the classification of COPD to ICD-9 codes 491 (chronic bronchitis) and 492 (emphysema), whereas two others also included 496 (COPD not elsewhere classified). The remaining two studies used the broadest definitions of COPD, with one including 490 (Bronchitis, not specified acute or chronic), 491, 492, and 496, and the other including all codes between 490 and 496 (Chronic Obstructive Pulmonary Disease and Allied Conditions). The final study classified COPD based on a questionnaire completed about their inpatient population. Only two of the studies examining ESRD used an ICD-9 code to define ESRD, but the authors did not publish the ICD-9 code used. Other studies classified patients with ESRD based on the fact that they were either patients at a dialysis clinic, a Medicare beneficiary of ESRD services, or a member of the Japan Association of Kidney Disease Patients. Diabetes was largely defined by patients who were being seen as a patient for a diabetic condition; only one author identified diabetes using an ICD-9 code (250.00–250.93), which includes diabetes diagnosis with and without complications.
Discussion
This systematic review reports on health outcomes after disaster for adults aged 65 and older. Of the 17 articles included, three types of weather- and climate-related disasters were identified. In multiple articles, results indicated that older adults may fare better after disasters. This surprising result is contrary to both anecdotal knowledge and published studies, albeit with different study criteria than used here, differing most notably in age ranges. These results may be a result of limitations reported in each article, including small sample size and limited study power. Research has found that differences exist across the spectrum of aging, specifically for young-old, middle-old, and very-old age groups. This review highlights the need for age-stratified analyses in disaster research.
Knowledge on Specific Disasters
Articles in this review reported on only three types of weather- and climate-related disasters—earthquakes, wildfires, and hurricanes—despite the fact that the search criteria included 14 types of disasters and nine broad-based weather- and climate-related disaster terms. For comparison, only 12% of U.S. federal disaster declarations between 1996 and 2017 included these types of disasters, indicating an absence of research around the more frequent types of disasters. Tornadoes, for example, account for nearly one quarter of Federal Emergency Management Agency (2019) disaster declarations between 1996 and 2017. Although other studies have reported more broadly on multiple types of disasters, as outcome data using specific age categories and the four chronic diseases of interest specified for inclusion in this review were not reported, these articles were not included in this analysis.
Of our chronic diseases of interest, the earthquake-related studies included in our review covered diabetes, ESRD, and COPD. Kirizuka and colleagues (1997) showed that approximately 2 months after the Great Hanshin-Awaji Earthquake, glycated hemoglobin (HbA1c) levels were elevated in their patient sample. The Nishikawa and colleagues’ (2015 study of the Great East Japan Earthquake showed that diabetic patients who visited the hospital periodically did not experience an increase in HbA1c levels, suggesting that regular access to care can maintain status quo for diabetes patients. However, both studies found insignificant differences between older adults and the general study population. Sugisawa and colleagues (2017) measured earthquake preparedness among ESRD patients in areas that had been previously affected by the 2011 Great East Japan Earthquake. Although earthquake preparedness was not found to correlate significantly with age, a number of social support factors including support from family and friends had a significant association with earthquake preparedness. Examining COPD, Ohkouchi and colleagues (2013) found that COPD exacerbations during the 2011 earthquake year were 2.5 times higher than the same time period during the previous year; however, this finding was not significant by age group and the proportion of COPD patients relative to other inpatients changed by less than 1%.
The hurricane-related studies included in our review primarily focus on ESRD and diabetes. ESRD patients rely on regular hemodialysis sessions to manage their condition, and disasters can interrupt regular care and produce negative health outcomes. Hurricanes were associated with an increase in dialysis-related (Gotanda et al., 2015; Sharma, 2015) and diabetes-related (Lee et al., 2016; Sharma et al., 2008) emergency department (ED) visits and hospitalizations. Effects were generally not reflective of disproportionate health outcomes for older adults versus other age groups, aside from a study by Lee and colleagues (2016) which noted a 10% increase in the proportion of ED visitors over 65 years of age with a secondary diagnosis of diabetes in the aftermath of Hurricane Sandy.
The six studies dealing with wildfires examined associations between the consequent increase in particulate matter (PM2.5) concentration in the air and a variety of respiratory and cardiovascular outcomes, including the outcomes of COPD and CHF relevant to the current review. Generally, studies found that adverse COPD outcomes increased in association with increasing PM2.5. In contrast, CHF outcomes were not significantly affected. Rather than drawing the conclusion that wildfires do not influence CHF outcomes, these findings were attributed to study limitations such as small sample sizes (Rappold et al., 2011), lack of access to ED admission data (Rappold et al., 2012), and limited size of the wildfires (Delfino et al., 2009).
Although associations were observed between COPD outcomes and increasing PM2.5, these effects were not specific to older adults. In fact, five of the six studies observed that an increase in COPD outcomes was only significant for younger age groups (typically age 40–64; Delfino et al., 2009; Parthum, Pindilli, & Hogan, 2017; Rappold et al., 2011; Reid et al., 2016; Tinling, West, Cascio, Kilaru, & Rappold, 2016). Only one study (Mott et al., 2005) found a significant increase in COPD-related hospitalizations after a wildfire, and the increase for older adults (42%) was less than the increase for younger age groups (50%).
Commonalities
Access to care
Disasters place an increased demand on the health care system during the response and recovery phase. Many of the studies in this review focus on the aftereffects of natural disasters. Appropriate planning in the preparedness phase of chronic disease for older adults can help mitigate the effects of disaster, where a preventative approach to accessing health care services and health resources may lessen adverse outcomes in the event of a disaster for which individuals can plan (such as a hurricane). Early dialysis is one example: Lurie and colleagues (2015) found that patients who received dialysis ahead of Hurricane Sandy had better outcomes when compared with those who did not. In this study, patients more likely to receive early dialysis were older adults.
The findings by Sugisawa and colleagues (2017) that participants with greater social support were more prepared for earthquakes parallels other research findings that communities with more social cohesion are more resilient (Aldrich, 2012; Aldrich & Kyota, 2017). Although the study’s findings were not unique to older adults, other studies echo this, finding that older adults are more likely to have the kinds of social networks that could engender more beneficial outcomes after disaster (Aldrich, 2012; Aldrich & Kyota, 2017; Cherry et al., 2011).
Postdisaster health care utilization
The need for postdisaster health care varied by disease process. Included articles that studied the effects of wildfire-associated exposure to particulate matter found that CHF and COPD were not associated with increased ED and hospital admissions in older adults. These studies instead indicated less health care utilization, specific to ED visits and hospital admissions, after exposure to particular matter from wildfires among older adults when compared with younger adults. This finding was surprising as causal associations between inhalation of particulate matter and cardiovascular and respiratory morbidity and mortality have been found in multiple studies on air pollution (Johnston et al., 2014; Kollanus, Tiittanen, Niemi, & Lanki, 2016; Rappold et al., 2014; Rappold, Reyes, Pouliot, Cascio, & Diaz-Sanchez, 2017; Tinling et al., 2016) and other disasters such as dust storms (Chiu et al., 2008).
Among those with ESRD, older adults were less likely than younger participants to miss dialysis sessions (Anderson et al., 2009). Factors that mitigated likelihood of missing a dialysis session included being aware of their organization’s disaster/emergency plans, not living alone and not having to move to a shelter. Conversely, after Hurricane Katrina, ED visits for renal failure among adults 80 and older accounted for an increase of 14% of visits (Sharma et al., 2008).
Associations were found between hurricanes and the need for diabetes care. After Hurricane Sandy, older diabetic patients were more at risk for requiring postdisaster emergency care compared with other vulnerable populations (Lee et al., 2016; Malik et al., 2018). After Hurricane Katrina, adults 80 and older with diabetic concerns accounted for 7% of total visits (Sharma et al., 2008). However, adults across age categories with type 2 diabetes experienced increased HbA1c levels immediately following a disaster (Kirizuka et al., 1997; Lee et al., 2016). Kirizuka and colleagues (1997) found that 56% of diabetic patients had a temporary mean increase in HbA1c levels after the Great East Japan Earthquake. Not following a diabetic diet was identified as a key factor to increased HbA1c levels. However, no significant difference was identified between older and younger adults.
Challenges in Conducting Disaster Research
The elements of disorganization and the unexpected in a disaster makes research in this area a challenge (Birnbaum, Daily, O’Rourke, & Loretti, 2015a). Methodological challenges identified throughout this review included limited observation periods, differing effects of similar disasters, underpowered studies, and ecological fallacy. Underpowered studies were a commonly cited limitation due to limited sample size, where affected populations were not large enough for robust confidence intervals (Rappold et al., 2011). Delfino and colleagues (2009) cited a short observation period relative to other time-series investigations as the reason for loss of statistical power in their study. Ecological fallacy was a concern in Rappold and colleagues’ (2012 study of North Carolina peat bog wildfires because exposures and modifiers were only known at an aggregate level.
No two disasters are the same, which makes study replication and generalization difficult in this area. Tinling and colleagues attempted to replicate the findings of Rappold and colleagues’ (2011 study of the 2008 Evans Road fire in North Carolina with a study of a similar 2011 North Carolina fire. Despite the similarities between these fires (geographic location, time of year), Tinling and colleagues (2016) found a different distribution of health effects than in the earlier study. The authors attributed the differences in findings to environmental conditions caused by recent weather conditions, where the 2011 fire led to a greater amount of smoke, thus increasing the PM2.5 levels relative to the 2008 fire.
Implications for Future Research
Data-driven comparisons can identify areas for improvement and prepare responders and health care providers to save lives in the next disaster. An important recommendation from reviewing the 17 papers included in this study is the need to follow stringent guidelines for disaster health research such as those developed by Birnbaum, Daily, O’Rourke, and Loretti (2015b); Birnbaum, Daily, and O’Rourke (2015a, 2015b); Birnbaum, Daily, O’Rourke, and Kushner (2016); Birnbaum, Daily, O’Rourke, and Loretti (2015a, 2016); and Birnbaum, Loretti, Daily, and O’Rourke (2016).
A strong need exists for causal evidence on the effect of disasters on chronic disease, which can more effectively influence policy change and contribute to improving health. Because disasters vary across settings, populations, and intensity, implementing a standard for data collection methods, as well as data sharing, could provide the ability to make generalizations. A disaster-relevant core outcome set might be of value (Prinsen et al., 2014). Large-scale, standardized data can be analyzed to draw scientific and policy-relevant conclusions, thereby improving response to future disasters by better equipping disaster responders in reducing health consequences to people affected by disasters. Data collection can be addressed with coordinated efforts on the federal, state, and local level, with funding and trained experts ready to be deployed. These data can then be used to compare and make generalizations across multiple populations and disasters. As an example, two studies included in this review had the same study design and hazard type, but different findings. With more, and more coordinated, replication studies of multiple disasters of the same hazard, the results could be pooled to make estimates of causal effect.
Disaster health research can be improved by strengthening partnerships between federal, state, and local emergency managers, volunteer organizations active in disaster and the academic community to facilitate safe access to disaster environments. However, because baseline effects are often not available in a disaster-affected community, interpreting findings can be difficult to impossible; further evaluation of interventions cannot occur until after the next disaster (Birnbaum et al., 2015b, 2015c). Given these limitations, it is understandable that studies on older adults and disasters remain limited. Although it is true that research is expanding—with most of the studies included in this review published after 2011—the absolute levels of research remain quite low and there is limited standardization across studies.
Finally, health outcomes after disaster will vary not only by age, but also by race/ethnicity, gender, and income, to name only a few sociodemographics that should be considered for inclusion in statistical analyses. Furthermore, social support, built environment, and limitation of resources have been linked to chronic disease outcomes among older adults (Cockerham, Hamby, & Oates, 2017; Vogeli et al., 2007; Wolff, Starfield, & Anderson, 2002). Many of the studies included in this review did include these factors. These studies are important contributions to the literature in that they can both inform mechanistic understandings of disasters and determine where best to target relief efforts.
Limitations
This study was designed to identify the impact of weather- and climate-related disasters on the health of older adults who had one of the four chronic conditions. Thus, a body of literature exists that did not meet these criteria, including studies of human-induced disasters such as terrorism or systems failures. Studies were eliminated if they did not specifically include at least one categorical age category of individuals aged 65 and older. Studies were also excluded if they did not relate specifically to a single disaster. As such, studies that examined the health outcomes of disasters in a general sense, or over a longer period of time were eliminated from this study (i.e., the impacts of wildfires in a specific geographic region over a 10-year period). This review also excluded studies that did not specifically include data on one of the four chronic conditions outlined in this study. Finally, although chronic disease outcomes may be affected by stress reactions resulting from disaster, we did not specifically study this pathway, rather the outcome itself.
Conclusion
Our review comprehensively organizes and synthesizes the limited body of literature that examines health outcomes of disasters on older adults with the goal of defining areas for future research. We find that many studies contradict the prevailing literature precedent that older adults are disproportionately affected by disasters compared with younger age groups. These findings, along with methodological limitations identified by the study authors, demonstrate the need for further investigation using rigorous, standardized, scientific methodology to examine the health impacts of disaster on adults with chronic disease through the full disaster management cycle of mitigation, preparedness, response, and recovery. In presenting this data for analysis and highlighting areas for future research, we hope to enable policy that anticipates and addresses chronic health needs related to disaster exposure based on rigorous, standardized scientific data.
Funding
This work was supported by the National Institute on Aging of the National Institutes of Health under award number K23AG059890 (S.A.B., PI). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict of Interest
None reported.
Supplementary Material
Acknowledgments
The authors acknowledge Whitney Townsend for conducting the literature searches, Christine Tracy for article synthesis, and James Brancho, PhD, for editorial assistance.
References
- Aldrich D. P. (2012). Building resilience: Social capital in post-disaster recovery. Chicago, IL: University of Chicago Press. [Google Scholar]
- Aldrich D. P., & Kyota E (2017). Creating community resilience through elder-led physical and social infrastructure. Disaster Medicine and Public Health Preparedness, 11, 120–126. doi:10.1017/dmp.2016.206 [DOI] [PubMed] [Google Scholar]
- Anderson A. H., Cohen A. J., Kutner N. G., Kopp J. B., Kimmel P. L., & Muntner P (2009). Missed dialysis sessions and hospitalization in hemodialysis patients after Hurricane Katrina. Kidney International, 75, 1202–1208. doi:10.1038/ki.2009.5 [DOI] [PubMed] [Google Scholar]
- Birnbaum M. L., Daily E. K., O’Rourke A. P., & Loretti A. (2015a). Research and evaluations of the health aspects of disasters, part I: An overview. Prehospital and Disaster Medicine, 30, 512–522. doi:10.1017/S1049023X15005129 [DOI] [PubMed] [Google Scholar]
- Birnbaum M. L., Daily E. K., O’Rourke A. P., & Loretti A. (2015b). Research and evaluations of the health aspects of disasters, part II: The disaster health conceptual framework revisited. Prehospital and Disaster Medicine, 30, 523–538. doi:10.1017/s1049023x15005130 [DOI] [PubMed] [Google Scholar]
- Birnbaum M. L., Daily E. K., & O’Rourke A. P. (2015a). Research and evaluations of the health aspects of disasters, part III: Framework for the temporal phases of disasters. Prehospital and Disaster Medicine, 30, 628–632. doi:10.1017/s1049023x15005336 [DOI] [PubMed] [Google Scholar]
- Birnbaum M. L., Daily E. K., & O’Rourke A. P. (2015b). Research and evaluations of the health aspects of disasters, part IV: Framework for societal structures: The societal systems. Prehospital and Disaster Medicine, 30, 633–647. doi:10.1017/S1049023X15005348 [DOI] [PubMed] [Google Scholar]
- Birnbaum M. L., Daily E. K., & O’Rourke A. P. (2015c). Research and evaluations of the health aspects of disasters, part V: Epidemiological Disaster Research. Prehospital and Disaster Medicine, 30, 648–656. doi:10.1017/S1049023X1500535X. [DOI] [PubMed] [Google Scholar]
- Birnbaum M. L., Daily E. K., O’Rourke A. P., & Kushner J (2016). Research and evaluations of the health aspects of disasters, part vi: Interventional research and the disaster logic model. Prehospital and Disaster Medicine, 31, 181–194. doi:10.1017/s1049023x16000017 [DOI] [PubMed] [Google Scholar]
- Birnbaum M. L., Daily E. K., O’Rourke A. P., & Loretti A (2016). Research and evaluations of the health aspects of disasters, Part IX: Risk-Reduction Framework. Prehospital and Disaster Medicine, 31, 309–325. doi:10.1017/S1049023X16000352 [DOI] [PubMed] [Google Scholar]
- Birnbaum M. L., Loretti A., Daily E. K., & O’Rourke A. P (2016). Research and evaluations of the health aspects of disasters, Part VIII: Risk, risk reduction, risk management, and capacity building. Prehospital and Disaster Medicine, 31, 300–308. doi:10.1017/s1049023x16000285 [DOI] [PubMed] [Google Scholar]
- Buttorff C., Ruder T., & Bauman M (2017). Multiple chronic conditions in the United States. Retrieved from Santa Monica, CA: https://www.rand.org/content/dam/rand/pubs/tools/TL200/TL221/RAND_TL221.pdf [Google Scholar]
- Cherry K. E., Brown J. S., Marks L. D., Galea S., Volaufova J., Lefante C.,…Jazwinski S. M (2011). Longitudinal assessment of cognitive and psychosocial functioning after hurricanes Katrina and Rita: Exploring disaster impact on middle-aged, older, and oldest-old adults. Journal of Applied Biobehavioral Research, 16, 187–211. doi:10.1111/j.1751-9861.2011.00073.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherry K. E., Sampson L., Galea S., Marks L. D., Baudoin K. H., Nezat P. F., & Stanko K. E (2017). Health-related quality of life in older coastal residents after multiple disasters. Disaster Medicine and Public Health Preparedness, 11, 90–96. doi:10.1017/dmp.2016.177 [DOI] [PubMed] [Google Scholar]
- Chiu H. F., Tiao M. M., Ho S. C., Kuo H. W., Wu T. N., & Yang C. Y (2008). Effects of Asian dust storm events on hospital admissions for chronic obstructive pulmonary disease in Taipei, Taiwan. Inhalation Toxicology, 20, 777–781. doi:10.1080/08958370802005308 [DOI] [PubMed] [Google Scholar]
- Cochrane Public Health (2018). Cochrane public health extraction template. London, UK: Cochrane Public Health. [Google Scholar]
- Cockerham W. C., Hamby B. W., & Oates G. R (2017). The social determinants of chronic disease. American Journal of Preventive Medicine, 52 (1 Suppl 1), S5–S12. doi:10.1016/j.amepre.2016.09.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delfino R. J., Brummel S., Wu J., Stern H., Ostro B., Lipsett M.,…Gillen D. L (2009). The relationship of respiratory and cardiovascular hospital admissions to the southern California wildfires of 2003. Occupational and Environmental Medicine, 66, 189–197. doi:10.1136/oem.2008.041376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Federal Emergency Management Agency (2019). Disaster declarations Retrieved from https://www.fema.gov/disasters
- Fonseca V. A., Smith H., Kuhadiya N., Leger S. M., Yau C. L., Reynolds K.,…John-Kalarickal J (2009). Impact of a natural disaster on diabetes: Exacerbation of disparities and long-term consequences. Diabetes Care, 32, 1632–1638. doi:10.2337/dc09-0670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster M., Brice J. H., Shofer F., Principe S., Dewalt D., Falk R., & Ferris M (2011). Personal disaster preparedness of dialysis patients in North Carolina. Clinical Journal of the American Society of Nephrology, 6, 2478–2484. doi:10.2215/CJN.03590411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gotanda H., Fogel J., Husk G., Levine J. M., Peterson M., Baumlin K., & Habboushe J (2015). Hurricane sandy: Impact on emergency department and hospital utilization by older adults in lower Manhattan, New York (USA). Prehospital and Disaster Medicine, 30, 496–502. doi:10.1017/S1049023X15005087 [DOI] [PubMed] [Google Scholar]
- Harris J. A., Moniz M. H., Iott B., Power R., & Griggs J. J (2016). Obesity and the receipt of influenza and pneumococcal vaccination: A systematic review and meta-analysis. BMC Obesity, 3, 24. doi:10.1186/s40608-016-0105-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyre A. D., Cohen A. J., Kutner N., Alper A. B., & Muntner P (2007). Prevalence and predictors of posttraumatic stress disorder among hemodialysis patients following Hurricane Katrina. American Journal of Kidney Diseases, 50, 585–593. [DOI] [PubMed] [Google Scholar]
- International Federation of Red Cross and Red Crescent Societies (2017). What is a disaster? Retrieved from http://www.ifrc.org/en/what-we-do/disaster-management/about-disasters/what-is-a-disaster/ [DOI] [PubMed]
- Johnston F. H., Purdie S., Jalaludin B., Martin K. L., Henderson S. B., & Morgan G. G (2014). Air pollution events from forest fires and emergency department attendances in Sydney, Australia 1996–2007: A case-crossover analysis. Environmental Health, 13, 105. doi:10.1186/1476-069X-13-105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirizuka K., Nishizaki H., Kohriyama K., Nukata O., Arioka Y., Motobuchi M.,…Tsuboi S (1997). Influences of the great Hanshin-Awaji Earthquake on glycemic control in diabetic patients. Diabetes Research and Clinical Practice, 36, 193–196. [DOI] [PubMed] [Google Scholar]
- Klinenberg E. (2015). Heat wave: A social autopsy of disaster in Chicago (1st ed). Chicago, IL: University of Chicago Press. [DOI] [PubMed] [Google Scholar]
- Kobayashi S., Hanagama M., Yamanda S., Satoh H., Tokuda S., Kobayashi M.,…Yanai M (2013). Impact of a large-scale natural disaster on patients with chronic obstructive pulmonary disease: The aftermath of the 2011 Great East Japan Earthquake. Respiratory Investigation, 51, 17–23. doi:10.1016/j.resinv.2012.10.004 [DOI] [PubMed] [Google Scholar]
- Kollanus V., Tiittanen P., Niemi J. V., & Lanki T (2016). Effects of long-range transported air pollution from vegetation fires on daily mortality and hospital admissions in the Helsinki metropolitan area, Finland. Environmental Research, 151, 351–358. doi:10.1016/j.envres.2016.08.003 [DOI] [PubMed] [Google Scholar]
- Lee D. C., Smith S. W., Carr B. G., Doran K. M., Portelli I., Grudzen C. R., & Goldfrank L. R (2016). Geographic distribution of disaster-specific emergency department use after hurricane sandy in New York City. Disaster Medicine and Public Health Preparedness, 10, 351–361. doi:10.1017/dmp.2015.190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lurie N., Finne K., Worrall C., Jauregui M., Thaweethai T., Margolis G., & Kelman J (2015). Early dialysis and adverse outcomes after hurricane sandy. American Journal of Kidney Diseases, 66, 507–512. doi:10.1053/j.ajkd.2015.04.050 [DOI] [PubMed] [Google Scholar]
- Malik S., Lee D. C., Doran K. M., Grudzen C. R., Worthing J., Portelli I.,…Smith S. W (2018). Vulnerability of older adults in disasters: Emergency department utilization by geriatric patients after hurricane sandy. Disaster Medicine and Public Health Preparedness, 12, 184–193. doi:10.1017/dmp.2017.44 [DOI] [PubMed] [Google Scholar]
- Mott J. A., Mannino D. M., Alverson C. J., Kiyu A., Hashim J., Lee T.,…Redd S. C (2005). Cardiorespiratory hospitalizations associated with smoke exposure during the 1997, Southeast Asian forest fires. International Journal of Hygiene and Environmental Health, 208, 75–85. doi:10.1016/j.ijheh.2005.01.018 [DOI] [PubMed] [Google Scholar]
- National Centers for Environmental Information (2019). Billion-dollar weather and climate disasters Retrieved from https://www.ncdc.noaa.gov/billions/
- National Heart Lung and Blood Institute (NHLBI) (2014). Quality assessment tool for observational cohort and cross-sectional studies Retrieved from https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools
- Nishikawa Y., Fukuda Y., Tsubokura M., Kato S., Nomura S., & Saito Y (2015). Managing type 2 diabetes mellitus through periodical hospital visits in the aftermath of the great east Japan earthquake disaster: A retrospective case series. PLoS One, 10, e0125632. doi:10.1371/journal.pone.0125632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office of Disease Prevention and Health Promotion (2017). Healthy People 2020: Older adults Retrieved from https://www.healthypeople.gov/2020/topics-objectives/topic/older-adults
- Office of Emergency Management (2014). New York City Hazard Mitigation Plan 2014: Hurricane sandy retrospective analysis. New York City, NY: Retrieved from http://www.nyc.gov/html/oem/downloads/pdf/hazard_mitigation/plan_update_2014/3.12_sandy_public_review_draft.pdf [Google Scholar]
- Ohkouchi S., Shibuya R., Yanai M., Kikuchi Y., Ichinose M., & Nukiwa T (2013). Deterioration in regional health status after the acute phase of a great disaster: Respiratory physicians’ experiences of the Great East Japan Earthquake. Respiratory Investigation, 51, 50–55. doi:10.1016/j.resinv.2012.12.003 [DOI] [PubMed] [Google Scholar]
- Parthum B., Pindilli E., & Hogan D (2017). Benefits of the fire mitigation ecosystem service in the Great Dismal Swamp National Wildlife Refuge, Virginia, USA. Journal of Environmental Management, 203, 375–382. doi:10.1016/j.jenvman.2017.08.018 [DOI] [PubMed] [Google Scholar]
- Prinsen C. A., Vohra S., Rose M. R., Boers M., Tugwell P., Clarke M., Williamson P. R., & Terwee C. B (2014). How to select outcome measurement instruments for outcomes included in a “Core Outcome Set” – A practical guideline. Trials, 17, 449. doi:10.1186/s13063-016-1555-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rappold A. G., Cascio W. E., Kilaru V. J., Stone S. L., Neas L. M., Devlin R. B., & Diaz-Sanchez D (2012). Cardio-respiratory outcomes associated with exposure to wildfire smoke are modified by measures of community health. Environmental Health, 11, 71. doi:10.1186/1476-069X-11-71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rappold A. G., Fann N. L., Crooks J., Huang J., Cascio W. E., Devlin R. B., & Diaz-Sanchez D (2014). Forecast-based interventions can reduce the health and economic burden of wildfires. Environmental Science & Technology, 48, 10571–10579. doi:10.1021/es5012725 [DOI] [PubMed] [Google Scholar]
- Rappold A. G., Reyes J., Pouliot G., Cascio W. E., & Diaz-Sanchez D (2017). Community vulnerability to health impacts of wildland fire smoke exposure. Environmental Science & Technology, 51, 6674–6682. doi:10.1021/acs.est.6b06200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rappold A. G., Stone S. L., Cascio W. E., Neas L. M., Kilaru V. J., Carraway M. S.,…Devlin R. B (2011). Peat bog wildfire smoke exposure in rural North Carolina is associated with cardiopulmonary emergency department visits assessed through syndromic surveillance. Environmental Health Perspectives, 119, 1415–1420. doi:10.1289/ehp.1003206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid C. E., Jerrett M., Tager I. B., Petersen M. L., Mann J. K., & Balmes J. R (2016). Differential respiratory health effects from the 2008 northern California wildfires: A spatiotemporal approach. Environmental Research, 150, 227–235. doi:10.1016/j.envres.2016.06.012 [DOI] [PubMed] [Google Scholar]
- Sharma V. (2015). Effects of voice inter-relating process and OM mantra enchanting in adolescents diabetic patients in south Delhi metro population. Pediatric Diabetes, 16, 100. doi:10.1111/pedi.12309 [Google Scholar]
- Sharma A. J., Weiss E. C., Young S. L., Stephens K., Ratard R., Straif-Bourgeois S.,…Rubin C. H (2008). Chronic disease and related conditions at emergency treatment facilities in the New Orleans area after Hurricane Katrina. Disaster Medicine and Public Health Preparedness, 2, 27–32. doi:10.1097/DMP.0b013e31816452f0 [DOI] [PubMed] [Google Scholar]
- Stang A. (2010). Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. European Journal of Epidemiology, 25, 603–605. doi:10.1007/s10654-010-9491-z [DOI] [PubMed] [Google Scholar]
- Sugisawa H., Shimizu Y., Kumagai T., Sugisaki H., Ohira S., & Shinoda T (2017). Earthquake preparedness among Japanese Hemodialysis patients in Prefectures Heavily Damaged by the 2011 Great East Japan Earthquake. Therapeutic Apheresis and Dialysis, 21, 334–344. doi:10.1111/1744-9987.12542 [DOI] [PubMed] [Google Scholar]
- Tanji F., Sugawara Y., Tomata Y., Watanabe T., Sugiyama K., Kaiho Y.,…Tsuji I (2017). Psychological distress and the incident risk of functional disability in elderly survivors after the Great East Japan Earthquake. Journal of Affective Disorders, 221, 145–150. doi:10.1016/j.jad.2017.06.030 [DOI] [PubMed] [Google Scholar]
- The Cochrane Collaboration (2011). Cochrane handbook for systematic reviews of interventions (Higgins J. P. T. & Green S. Eds., Version 5.1.0). London, UK: The Cochrane Collaboration. [Google Scholar]
- Tinling M. A., West J. J., Cascio W. E., Kilaru V., & Rappold A. G (2016). Repeating cardiopulmonary health effects in rural North Carolina population during a second large peat wildfire. Environmental Health, 15, 12. doi:10.1186/s12940-016-0093-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogeli C., Shields A. E., Lee T. A., Gibson T. B., Marder W. D., Weiss K. B., & Blumenthal D (2007). Multiple chronic conditions: Prevalence, health consequences, and implications for quality, care management, and costs. Journal of General Internal Medicine, 22(Suppl 3), 391–395. doi:10.1007/s11606-007-0322-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watts N., Amann M., Ayeb-Karlsson S., Belesova K., Bouley T., Boykoff M.,…Costello A (2018). The Lancet Countdown on health and climate change: From 25 years of inaction to a global transformation for public health. The Lancet, 391, 581–630. doi:10.1016/S0140-6736(17)32464-9 [DOI] [PubMed] [Google Scholar]
- Wolff J. L., Starfield B., & Anderson G (2002). Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Archives of Internal Medicine, 162, 2269–2276. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.