Dear editor,
Since the end of 2019, Corona Virus Disease 2019 (COVID-19) has caused a worldwide pandemic. One study had found significant psychological distress even after hospital discharge in patients infected with severe acute respiratory syndrome (SARS) (Cheng et al., 2004), indicating that the mental status of COVID-19 patients shouldn’t be ignored as well. Actually, a “tsunami of psychiatric illness” is being predicted and actions such as calling for a special research topic and accelerating the manuscript review process have been taken to deal with the lacking of useful information in the mental health crisis (Tandon, 2020). Though some studies assessed the prevalence of depressive symptoms and potential influencing factors in hospitalized (Ma et al., 2020) and discharged (Liu et al., 2020) COVID-19 patients, these results might be misleading due to limited sample size. Thus, in this letter, we aimed to provide a rapid meta-analysis of the prevalence of depressive symptoms in COVID-19 patients and potential influencing factors based on published studies which might be the reference for mental health intervention during the epidemic.
We searched PubMed, EMBASE, and Cochrane Library using the following keywords from inception to July 30, 2020: “depression”, “depressive”, “COVID-19”, “2019nCoV” and “novel coronavirus” etc. Studies were included if: (1) all participants were diagnosed with COVID-19; (2) prevalence rates of depressive symptoms or related influencing factors with adjusted odds ratio (OR) and 95 % confidence interval (CI) were reported; (3) depressive symptoms occurred after the diagnosis of COVID-19; (4) published in English in a peer-reviewed journal. In case of multiple publications on a single data set, the study with the largest sample size was included. Paired reviewers selected the articles and extracted data independently and then cross-checked. Any dispute was resolved by consensus. The prevalence of depressive symptoms was pooled using a random-effect model. Sensitivity analysis was conducted by excluding each study one by one and then the primary results were recalculated. Subgroup analysis was conducted based on whether to be discharged from the hospital and severity of depressive symptoms. I2 was used to evaluate the heterogeneity between studies. ORs with their 95 %CI of the same influencing factors were also pooled using random-effect model.
Eight cross-sectional studies were included after selection involving 2206 individuals with 1040 cases with depressive symptoms (Guo et al., 2020; Hu et al., 2020; Liguori et al., 2020; Liu et al., 2020; Ma et al., 2020; Nie et al., 2020; Yuan et al., 2020; Zhang et al., 2020), among which two studies considered cured patients discharged from the hospital (Liu et al., 2020; Yuan et al., 2020). One study (Liguori et al., 2020) came from Italy while the others were all from China. As for diagnostic criteria of depressive symptoms, four studies used Patient Health Questionnaire (9-item version, PHQ-9) or its Chinese version (Liu et al., 2020; Guo et al., 2020; Hu et al., 2020; Ma et al., 2020), two studies used Zung Self-rating Depression Scale (SDS) (Nie et al., 2020; Yuan et al., 2020), one study used the Chinese version of Hospital Anxiety and Depression Scale (HADS) (Zhang et al., 2020), and one study didn’t report specific scale (Liguori et al., 2020).
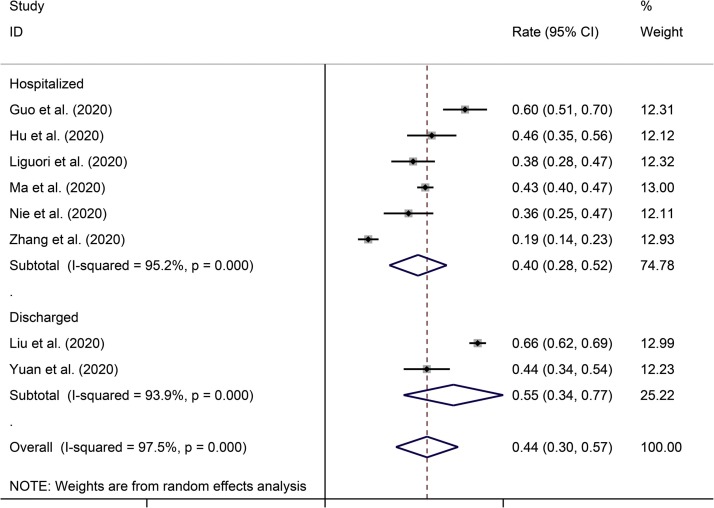
The total prevalence of depressive symptoms in COVID-19 patients was 44 % (95 %CI, 30 %–57 %; I2 = 97.5 %). Subgroup analysis presented that the prevalence of depressive symptoms in hospitalized and discharged patients were: 40 % (95 %CI, 28 %–52 %; I2 = 95.2 %), and 55 % (95 %CI, 34 %–77 %; I2 = 93.9 %) (Fig. 1 ) respectively. Sensitivity analysis when excluding each study one by one still showed a significantly high heterogeneity between the pooled studies. Subgroup analysis based on the depression severity showed a decreasing trend of prevalence that was 31 % (95 %CI: 19 %–43 %; I2 = 95.9 %) for mild, 13 % (95 %CI: 11 %–15 %; I2 = 0 %) for moderate, and 5 % (95 %CI: 2 %–8 %; I2 = 74.3 %) for severe, respectively (Supplementary Table S1). As there were less than ten studies, publication bias analysis or meta-regression were not conducted.
Fig. 1.
Prevalence of depressive symptoms in hospitalized and discharged patients with COVID-19.
We summarized the potential influencing factors reported in included studies in Supplementary Table S2. Meta-analysis was conducted for factors that were reported twice at least. For factors after meta-analysis, only family members diagnosed with COVID-19 (RR = 1.35, 95 %CI:1.00–1.84, P = 0.051) and higher disease severity (RR = 2.68, 95 %CI: 1.04–6.91, P = 0.042) might be correlated with depressive symptoms. Factors reported in single study such as smoke, more clinical symptoms after discharge, and perceived discrimination might be risk factors while frequent social media use and high level of resilience might be protective factors (Supplementary Table S2).
In this study, we firstly reported the pooled prevalence of depressive symptoms and potential influencing factors in COVID-19 patients. Highly elevated prevalence of depressive symptoms was found in COVID-19 patients not only when treated in hospital but also after hospital discharge, in which a considerable part appeared severe symptoms. Our results highlight an urgent need for psychological support and counseling for COVID-19 patients in the pandemic of the world although most of the research originated from China associated with significant heterogeneity. In fact, the severity of COVID-19 (Guo et al., 2020; Hu et al., 2020) and diagnosis criteria of depressive symptoms based on different scales (Ma et al., 2020; Nie et al., 2020) and cutoffs (Ma et al., 2020; Liu et al., 2020) in included studies might contribute to a certain heterogeneity. Furthermore, data on potential influencing factors was far from robust which should be clarified more in the further so as to better prevent and intervene depressive symptoms in COVID-19 patients. Anyway, we call to focus on the depressive symptoms in COVID-19 patients throughout this pandemic.
Funding source
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of Competing Interest
The authors report no declarations of interest.
Acknowledgement
None.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.ajp.2020.102421.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- Cheng S.K., Wong C.W., Tsang J., Wong K.C. Psychological distress and negative appraisals in survivors of severe acute respiratory syndrome (SARS) Psychol. Med. 2004;34(7):1187–1195. doi: 10.1017/s0033291704002272. [DOI] [PubMed] [Google Scholar]
- Guo Q., Zheng Y., Shi J., Wang J., Li G., Li C., Fromson J.A., Xu Y., Liu X., Xu H., Zhang T., Lu Y., Chen X., Hu H., Tang Y., Yang S., Zhou H., Wang X., Chen H., Wang Z., Yang Z. Immediate psychological distress in quarantined patients with COVID-19 and its association with peripheral inflammation: a mixed-method study. Brain Behav. Immun. 2020;88:17–27. doi: 10.1016/j.bbi.2020.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu Y., Chen Y., Zheng Y., You C., Tan J., Hu L., Zhang Z., Ding L. Factors related to mental health of inpatients with COVID-19 in Wuhan, China. Brain Behav. Immun. 2020:1–7. doi: 10.1016/j.bbi.2020.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liguori C., Pierantozzi M., Spanetta M., Sarmati L., Cesta N., Iannetta M., Ora J., Mina G.G., Puxeddu E., Balbi O., Pezzuto G., Magrini A., Rogliani P., Andreoni M., Mercuri N.B. Subjective neurological symptoms frequently occur in patients with SARS-CoV2 infection. Brain Behav. Immun. 2020;88:11–16. doi: 10.1016/j.bbi.2020.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu D., Baumeister R.F., Veilleux J.C., Chen C., Liu W., Yue Y., Zhang S. Risk factors associated with mental illness in hospital discharged patients infected with COVID-19 in Wuhan, China. Psychiatry Res. 2020;292 doi: 10.1016/j.psychres.2020.113297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma Y.F., Li W., Deng H.B., Wang L., Wang Y., Wang P.H., Bo H.X., Cao J., Wang Y., Zhu L.Y., Yang Y., Cheung T., Ng C.H., Wu X., Xiang Y.T. Prevalence of depression and its association with quality of life in clinically stable patients with COVID-19. J. Affect. Disord. 2020;275:145–148. doi: 10.1016/j.jad.2020.06.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nie X.D., Wang Q., Wang M.N., Zhao S., Liu L., Zhu Y.L., Chen H. Anxiety and depression and its correlates in patients with coronavirus disease 2019 in Wuhan. Int. J. Psychiatry Clin. Pract. 2020:1–6. doi: 10.1080/13651501.2020.1791345. [DOI] [PubMed] [Google Scholar]
- Tandon R. COVID-19 and mental health: preserving humanity, maintaining sanity, and promoting health. Asian J. Psychiatr. 2020;51 doi: 10.1016/j.ajp.2020.102256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan B., Li W., Liu H., Cai X., Song S., Zhao J., Hu X., Li Z., Chen Y., Zhang K., Liu Z., Peng J., Wang C., Wang J., An Y. Correlation between immune response and self-reported depression during convalescence from COVID-19. Brain Behav. Immun. 2020;88:39–43. doi: 10.1016/j.bbi.2020.05.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J., Yang Z., Wang X., Li J., Dong L., Wang F., Li Y., Wei R., Zhang J. The relationship between resilience, anxiety, and depression among patients with mild symptoms of COVID-19 in China: a cross-sectional study. J. Clin. Nurs. 2020:1–24. doi: 10.1111/jocn.15425. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.