Abstract
Background:
Heart failure (HF) patients are at increased risk for unmet palliative care needs. The International Classification of Diseases Ninth Revision (ICD-9) code, V66.7, can identify palliative care services. However, code validity for specialist palliative care in the Veterans Health Administration (VHA) has not been determined.
Objective:
To validate the ICD-9 code for specialist palliative care and determine common reasons for specialist palliative care consultation among VHA patients hospitalized with HF.
Design:
Electronic health record review of data from the Veterans Aging Cohort Study.
Setting/Subjects:
The sample included 100 patients hospitalized with HF from 2003–2012.
Measurements:
Data from 50 patients with V66.7 were matched by age, race, site of care, hospital length of stay, ICU admission, and fiscal year of study discharge to 50 HF patients without V66.7 who had died within a year of hospitalization. We calculated positive and negative predictive values (PPV, NPV), sensitivity, and specificity.
Results:
All patients included in the sample were male, 66% Black ethnicity, and mean age=65 years (standard deviations (SD) ±11; SD±10). Specialist palliative care was documented for 49/50 patients with V66.7 (PPV=98%, 95% Confidence Interval (CI) 88–99) and 9/50 patients without the code (NPV=82%, 95% CI 68–91). Sensitivity was 84% (95% CI 72–92), and specificity was 98% (95% CI 86–99). Establishing goals of care was the most frequent reason for palliative care consultation (43% of the sample).
Conclusion:
ICD-9 code V66.7 identifies specialist palliative care for hospitalized HF patients in the VHA. Replication of findings in other data sources and populations is needed.
Keywords: heart failure, palliative care, hospitalization, International Classification of Diseases Ninth Revision (ICD-9) code, hospice
Introduction
Adults with heart failure (HF) suffer from significant symptom burden, complex medical regimens, frequent hospitalizations and readmissions, and prognostic uncertainty.1,2 Approximately 20–25% of HF patients are readmitted within one month of hospital discharge, and 20–40% die within a year of hospitalization.3,4 Given the significant morbidity and mortality associated with HF, management guidelines recommend referral to palliative care for patients with advanced disease, including those who are symptomatic despite optimization of guideline-based therapies.1,5,6 However, rates of palliative care delivery for HF patients during hospitalization vary widely7–10, and remain substantially lower than patients with cancer.11 A recent study of patterns of palliative care delivery among decedents within the Veterans Health Administration (VHA) found that 47% of decedents with cardiopulmonary failure received palliative care during hospitalization within 90-days of death compared to 74% of decedents with cancer.11
In acute care settings, trained and typically palliative-certified specialists (specialist palliative care) address many of the physical, psychological, existential and spiritual symptoms patients may have during hospitalization. Specialty palliative care clinicians may also serve as hospice providers, or attend on inpatient palliative care units. Specialist palliative care can be identified by electronic health record (EHR) reviews, use of national palliative care and hospice registries, and administrative databases and claims records.2–4 Within administrative databases, researchers often use the International Classification of Diseases Ninth Revision (ICD-9) diagnosis code V66.7 as a means of identifying palliative care.12–15
The ICD-9 code V66.7, “Encounter for Palliative Care,” applies to instances in which specialist or non-specialist clinicians provide palliative, end-of-life, or terminal care services, primarily within inpatient settings.16 Use of V66.7 for research purposes remains controversial due to concerns over code validity in identifying palliative care.17–19 Prior research has found variation in code sensitivity ranging from 45 – 82% in samples including patients with HF.19–21 The VHA has directed that V66.7 be used for palliative care workflow capture since 2002.22,23 However, the V66.7 code has not been validated in this healthcare system. Code validation could lead to increased utilization in research aimed at understanding disparities in the use of specialist palliative care among patients with HF within the VHA. Therefore we validated the ICD-9 code for palliative care, V66.7, using EHR reviews as the reference and determined reasons for specialist palliative care consultations during hospitalization in patients hospitalized with HF.
Methods
Study patients were sampled from the Veterans Aging Cohort Study (VACS). VACS is an EHR-based cohort of all HIV infected Veterans engaged in care within the VHA system matched 1:2 with uninfected Veterans by age, race, gender, and site of care.24 VACS data sources include EHR, laboratory, pharmacy, and administrative data.25 Study approval was obtained from the Institutional Review Boards in which the study was conducted.
Sample
Among 7,496 patients hospitalized with HF (ICD-9 code 425.x and 428.x)26 between fiscal years 2003 and 2012, we found 235 patient records that included the ICD-9 code V66.7. We randomly selected 50 of these patients for review, using the first HF hospitalization with code V66.7. From the 7,261 patients hospitalized with HF without the V66.7 code, we then identified 2,722 patients who had died within one year of hospital admission. Using the last hospitalization prior to death, we matched 50 of these patients to those patients with V66.7 by age (+/−5 years), race, site of care, hospital length of stay (+/− 3 days), intensive care unit (ICU) admission during hospitalization, and fiscal year of study discharge (+/− 3 years). Patients without V66.7 who were still alive one year after admission were not included in the analysis. The final sample was 100 patients characterized using both EHR data and manual EHR review.
Procedures and Study Variables
Two authors (SLF and KMA) both clinicians trained in palliative care, reviewed progress notes (EHR note titles and unstructured text), provider consultation notes, discharge summaries, and other clinical data for documentation of palliative care during the hospitalization. Criteria for specialist palliative care included evidence of any of the following: palliative care consultation or follow-up by any palliative care consultation service team member; care in an inpatient palliative care or hospice unit; or care in a non-hospice unit with hospice services. We determined the primary reason for specialist palliative care from palliative care providers’ initial consult notes or from admission notes to inpatient palliative care and hospice units documented in the EHR. Primary reasons for specialist palliative care were grouped based on national clinical guidelines27 into mutually exclusive categories: goals of care, management of physical symptoms, management of psychological symptoms, social services and discharge planning, spiritual care, end-of-life care, and ethical or legal care (including code status discussions). To account for potential overlap among categories, for example in cases where goals of care conversations include discussions of discharge planning or end-of-life care, reviewers only selected goals of care if the phrase “goals of care” was documented in the specialist palliative care consultation note. Reviewers entered EHR review data using the Research Electronic Data Capture (REDcap) platform,28 a secure, web-based application designed to support data capture research studies. Inter-rater reliability was determined by review of 31 patients’ charts by two investigators (SLF and KMA).
Extracted data included demographics, comorbidities and laboratory tests. The HF diagnosis was classified as principal (primary condition associated with the entire hospitalization), or secondary if the HF code appeared in any other diagnosis fields. To describe the degree of cardiac dysfunction, we collected ejection fraction (EF) measurements from the first measurement during hospitalization, or if unavailable, the lowest measurement within six months prior to hospital admission. We assessed comorbidities commonly found in the VACS cohort and those frequently associated with HF.10–15 Comorbidities were identified by one inpatient or two outpatient ICD-9 codes for the condition within 30-days of the index admission, a previously established approach that improves coding accuracy compared with using a single instance.25 We included acute renal failure, anemia, chronic renal failure, chronic obstructive pulmonary disease (COPD), coronary artery disease, depression, diabetes mellitus, drug abuse, and hypertension. We identified diabetes mellitus by the ICD-9 code or by evidence of serum glucose meeting diagnostic criteria for diabetes mellitus.24,25 Hepatitis C and HIV infection were determined by a combination of ICD-9 codes, positive antibody tests, or detectable plasma HCV-RNA or HIV-1 RNA, respectively. Comorbidities present in more than 25% of the sample were included in the analysis.
To measure severity of illness, we used the VACS Index, a validated risk score of HIV-specific and general organ injury that predicts all-cause mortality, medical ICU (MICU) admission, and MICU mortality among HIV-infected and uninfected adults.29–31 VACS Index variables include age, CD4 cell count, HIV-1 RNA, hemoglobin, liver transaminases (aspartamine aminotransferase (AST); alanine transaminase (ALT), platelets, creatinine and Hepatitis C virus coinfection. Higher scores are associated with increased hospital and long-term mortality.32 The VACS Index was calculated for those patients with complete lab values on the first day of hospital admission or within six months prior to hospitalization using the values closest to admission.
Statistical Analysis
We assessed the ability of ICD-9 code V66.7 to identify specialist palliative care using EHR documentation as the reference standard. We calculated positive and negative predictive values (PPV, NPV), sensitivity, and specificity. We assessed inter-rater reliability with the Kappa statistic to determine agreement between reviewers regarding palliative care documentation within the EHR. Statistical significance was defined as a p-value of <0.05. We performed statistical analysis with SAS 9.4 (SAS Institute, Cary, North Carolina, USA).
Results
The sample was 100% male, and the mean age was 64.62 (standard deviation (SD) ±10.51) years for patients with V66.7 and 64.81 (SD = 9.82) years for the comparison group (Table 1). The sample was racially and ethnically diverse (66% Black; 24% White; 10% Hispanic), reflecting characteristics consistent with VACS overall.24,25 HF was the principal diagnosis for 36% of patients with V66.7 and 22% among the comparison group (p = 0.21). Ejection fraction measurements were available for 50% of patients with V66.7 and 60% of the comparison group. EF measurements were lower among those with V66.7 (median EF, [interquartile range (IQR)]=20%; [10 – 34]) compared to those without V66.7 (39% [25 – 45]) (p = 0.02). Comorbidities were common, and most comorbidities did not vary by group. Those with V66.7 were less likely than the comparison group to have anemia (42% versus 64%, p = 0.05) and acute renal failure (36% versus 58%, p = 0.02). Twenty-eight percent of patients with V66.7 and 48% of matches were HIV-infected (p = 0.06). Median VACS risk scores were similar in the two groups (59[40 – 75] verses 51[43 – 79] respectively (p = 0.35).
Table 1.
Demographic and clinical characteristics of patients hospitalized with heart failure by ICD-9 palliative care status
| Variable | Palliative Care by ICD-9 V66.7 (n=50) | Matched (n=50) | P-value |
|---|---|---|---|
| Age, mean (SD)a | 64.62 (10.51) | 64.81 (9.82) | 0.59 |
| Male, n (%)a | 50 (100) | 50 (100) | -- |
| Race, n (%)a | 0.89 | ||
| Black | 33 (66) | 33 (66) | -- |
| White | 12 (24) | 12 (24) | -- |
| Hispanic | 5 (10) | 5 (10) | -- |
| Fiscal year of study dischargea | 0.49 | ||
| 2003 | 0 | 1 | -- |
| 2004 | 2 | 0 | -- |
| 2005 | 2 | 4 | -- |
| 2006 | 1 | 2 | -- |
| 2006 | 5 | 4 | -- |
| 2008 | 6 | 3 | -- |
| 2009 | 7 | 10 | -- |
| 2010 | 6 | 3 | -- |
| 2011 | 5 | 11 | -- |
| 2012 | 16 | 12 | -- |
| Seen by palliative care consultation service | 45 (90) | 8 (16) | -- |
| Primary claim diagnosis code of heart failure for hospitalization, n (%) | 18 (36) | 11 (22) | 0.21 |
| Comorbidities, n (%) | |||
| Hypertension | 45 (90) | 48 (96) | 0.26 |
| Coronary artery disease | 38 (76) | 36 (72) | 0.66 |
| Chronic obstructive pulmonary disease | 25 (50) | 26 (52) | 0.86 |
| Anemia | 21 (42) | 32 (64) | 0.05 |
| Chronic renal failure | 21 (42) | 28 (56) | 0.16 |
| Diabetes mellitus | 21 (42) | 26 (52) | 0.34 |
| Acute renal failure | 18 (36) | 29 (58) | 0.02 |
| Depression | 18 (36) | 20 (40) | 0.70 |
| Drug abuse | 18 (36) | 13 (26) | 0.20 |
| Hepatitis C | 16 (32) | 17 (34) | 0.78 |
| HIV, n (%) | 14 (28) | 24 (48) | 0.06 |
| VACS Index, median (IQR)b,c | 59 (40 – 75) | 51 (43 – 79) | 0.35 |
| ICU admission during index hospitalizationa | 7 (14) | 7 (14) | -- |
| Hospital length of stay in days, mean (SD)a | 8.06 (7.01) | 7.72 (7.53) | 0.22 |
SD = standard deviation, IQR = interquartile range;
Matching criteria, site of care not included;
Calculated from lab values collected closest to the day of hospital admission and up to six months prior;
Missing 8% of palliative care and 14% of matches
Validation of the ICD-9 V66.7 Palliative Care Code.
Specialist palliative care was documented for 49/50 (PPV 98%, 95% CI 88 – 99) patients whose records included V66.7 and for 9/50 (NPV 82%, 95% CI 68 – 91) patients without the code (Table 2). The sensitivity of the ICD code for specialist palliative care was 84% (95% CI 72 – 92), and specificity was 98% (95% CI 86 – 99). One patient with code V66.7 did not have documented evidence of specialist palliative care and was discharged alive to home without additional services such as home hospice. The Kappa statistic for inter-rater reliability between reviewers for documentation of specialist palliative care was 1.0, reflecting 100% agreement.
Table 2.
Validity of the ICD-9 diagnostic code V66.7 for specialist palliative care in patients hospitalized with heart failure within the Veterans Health Administration
| Electronic Health Record | ||||
|---|---|---|---|---|
| Palliative Care | No Palliative Care | Total | Positive Predictive Value = 49/50 = 98% (95% CI 88 – 99) | |
| ICD-9 V66.7 | 49 | 1 | 50 | Negative Predictive Value = 41/50 = 82% (95% CI 68 – 91) |
| No ICD-9 V66.7 | 9 | 41 | 50 | Sensitivity = 49/58 = 84% (95% CI 72 – 92) |
| Total | 58 | 42 | 100 | Specificity = 41/42 = 98% (95% CI 86 – 99) |
CI = Confidence Interval
Primary Reason for Specialist Palliative Care
Of the total sample, 58 patients had documented evidence of specialist palliative care. Ninety-one percent of patients who had documented evidence of specialist palliative care (n = 53) were seen by a palliative care consultation service (Table 1). Primary reasons for specialist palliative care included establishing goals of care (43%), end-of-life care (21%), and the management of physical symptoms including pain (17%) (Figure 1).
Figure 1.
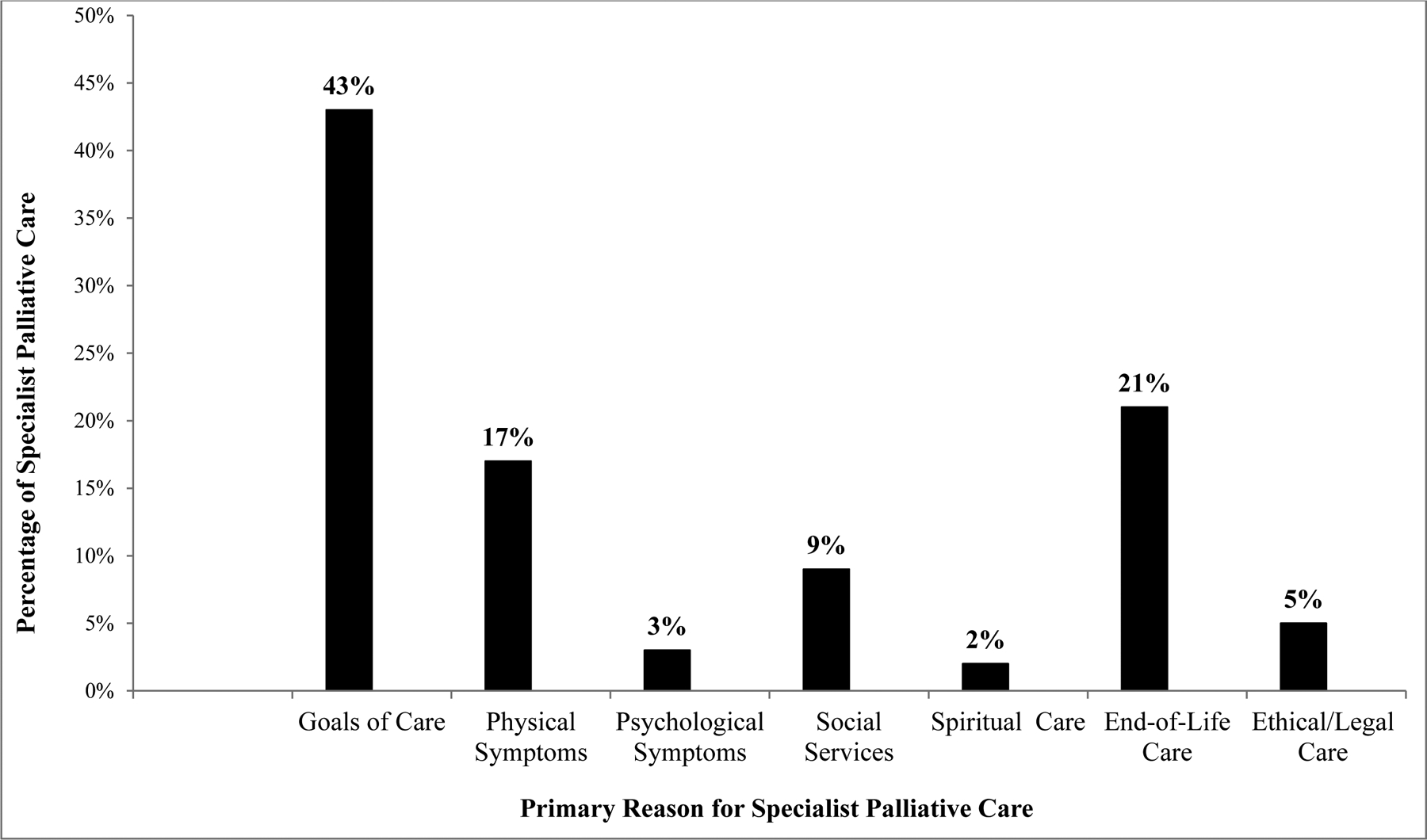
Primary reason for specialist palliative care identified in electronic health record review (n = 58)
Discussion
To our knowledge, our study represents the first time the V66.7 code has been validated within the VHA. We found the V66.7 code to have higher sensitivity but similar specificity (sensitivity 84%, specificity 98%) compared to other validation studies in both patients with and without HF.23, 25 For example, prior work has identified V66.7 validity in capturing withdrawal of life-sustaining therapies of patients with acute ischemic stroke at two teaching hospitals (sensitivity 81%, specificity 97%).21 Another single-center study found that the V66.7 code had a sensitivity of 50% and specificity of 99% for specialist palliative care for all hospitalized patients.19 In analyses restricted to patients with HF, performance of the code decreased considerably, with a sensitivity of 45% and a specificity of 98%. In a larger study of patients with cancer, HF, and chronic obstructive pulmonary disease from 33 hospitals involved in the University HEalthSystem Consortium, V66.7 coding and documentation were infrequent among patients who received specialist palliative care, with only 48% of those receiving palliative care noted to have a documented V66.7 code in the EHR.20
There are likely several explanations for the variation in code validity found in our study compared with prior work. First, differences in code sensitivity may reflect variations in billing and coding practices across healthcare systems as well as the coding input for their respective administrative datasets. The VHA directed that the ICD-9 code for palliative care be used for palliative care workflow capture in a nationwide directive starting in 2002 and reinstituted the directive in 2008.22,23 Consistent billing and coding practices across all VHA health centers, clinicians, and hospital coders could lead to increased application of the ICD-9 code. Our study findings may also reflect the VHA’s emphasis on increasing patient access to palliative care, as the VHA directed that all inpatient facilities provide palliative care consultative services starting in 2003.23,33
Second, code validity may vary based on who delivers palliative care and by the specific characteristics of palliative care delivery. For this study, we chose not to validate the utility of the code in capturing primary palliative care, that is palliative care delivered by non-palliative specialists during hospitalization, or in identifying specific processes of palliative care, such as withdrawal of life-sustaining treatments, symptom management, or discussions of goals of care. Primary palliative care may more likely be documented in unstructured text fields of patient progress notes and nursing notes rather than note titles and discharge summaries, potentially making recognition by medical coders difficult.22 Of these palliative care characteristics, others have validated the code’s ability to capture withdrawal of care21, but validation of the ICD-9 code’s ability to capture other processes of palliative care such as symptom management or represent primary palliative care delivery is not known.
A strength of the study is in the use of a large nationwide sample of hospitalized patients with HF from the VHA. However, this study has several limitations. Although patients were matched on several demographic and clinical variables, we could not control for unmeasured differences. In addition, other matching criteria or methods such as propensity score matching may have also yielded well-matched groups. While we did not have data on such variables as the New York Heart Association functional class or complete ejection fraction data, our analysis revealed no differences between groups in terms of a principal hospital diagnosis of HF and the VACS risk score, which suggests that both groups were likely similar in terms of disease severity.
Our validation findings are based on the assumption that if specialist palliative care was provided during hospitalization, it was documented within the EHR. Palliative care provided but not documented would bias our results, potentially underrepresenting receipt of palliative care. However, this limitation applies to any study using data other than direct observation for analysis. There may also be differences in case mix between VHA and non-VHA hospitals regarding the availability of palliative care services, provider preferences in referral to palliative care, and patient populations. Our study sample was comprised only of men with HF, who were younger than other research cohorts of HF patients receiving palliative care.7,8 This, in addition to the small sample size, may limit the generalizability of study findings. Prevalence of palliative care in this study was 50% by study design, in samples where the prevalence of specialist palliative care is lower, this could potentially lower the PPV of the code. A final caveat is that we validated the ICD-9 diagnosis code for palliative care rather than the ICD-10 iteration, z51.5. However, the ICD-9 diagnosis code V66.7 converts directly to z51.5 in ICD-10 and is considered an equivalent of the ICD-9 version.34
Our findings have several implications for future research. In the creation of our study sample we found that 235 (3.1%) patients out of 7,496 patients hospitalized with HF during the study period had an ICD-9 code for palliative care. The percentage of HF patients who had the ICD-9 diagnostic code is lower than the estimated 6% of all hospital discharges palliative care could potentially serve.35 This may suggest underutilization of palliative care for hospitalized HF patients, however additional research is needed.
Future work should examine the validity of the ICD-9 V66.7 code in other EHR systems with different patient populations and conditions, using other study designs and matching methods. Coding algorithms that include V66.7 in addition to other ICD-9 codes may facilitate further validation of the V66.7 code and allow for the identification of palliative care among multiple data sources. Over 28% of patients with V66.7 and 48% of matches were HIV infected. HIV-infected patients with HF have less access to advanced HF therapies including heart transplants and left ventricular assist devices compared to HF patients who are uninfected.36,37 Differences in referral to palliative care and coding of palliative care services by HIV status should also be investigated. Alternative measurement solutions for palliative care that capture specialist palliative care, primary palliative care, and processes of palliative care are also needed.27 Use of informatics-based techniques, such as text mining, may facilitate data retrieval of palliative care and palliative care processes from unstructured text. These methods could also identify palliative care delivered by a variety of clinicians, perhaps providing a more comprehensive depiction of palliative care service delivery.
Conclusion
In a sample of patients hospitalized with HF, we found that the predictive values and sensitivity of the palliative care diagnosis code V66.7 in capturing specialist palliative care was high. The diagnosis code for palliative care is likely accurate in identifying specialist palliative care for patients hospitalized with HF in the VHA. Replication of findings in other data sources is warranted, however, future work should also seek to identify alternative techniques that can capture primary palliative care and processes of palliative care.
Acknowledgements
The work is supported by the following: Hartford Centers for Gerontological Nursing Excellence, Jonas Center for Nursing and Veterans Healthcare, National Institute on Alcohol Abuse and Alcoholism (U10 AA013566-completed, U24 AA020794, U01 AA020790), and by the Department of Veterans Affairs, Veterans Health Administration Office of Research and Development.
Footnotes
Publisher's Disclaimer: DISCLAIMER: The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs.
Author disclosure statement
The authors report that no competing financial interests exist.
References
- 1.Gadoud A, Jenkins SMM, Hogg KJ. Palliative care for people with heart failure: Summary of current evidence and future direction. Palliat Med. 2013;27(9):822–828. [DOI] [PubMed] [Google Scholar]
- 2.Khan FR, Feder S, Goldsetin NE, Chaudhry SI. Symptom burden among patients who were hospitalized for heart failure. JAMA Intern Med. 2015;175(10):1713–1714. [DOI] [PubMed] [Google Scholar]
- 3.Lassus JPE, Siirilä-Waris K, Nieminen MS, et al. Long-term survival after hospitalization for acute heart failure--differences in prognosis of acutely decompensated chronic and new-onset acute heart failure. Int J Cardiol. 2013;168(1):458–462. [DOI] [PubMed] [Google Scholar]
- 4.Van Deursen VM, Urso R, Laroche C, et al. Co-morbidities in patients with heart failure: An analysis of the European Heart Failure Pilot Survey. Eur J Heart Fail. 2014;16(1):103–111. [DOI] [PubMed] [Google Scholar]
- 5.Goodlin S. Palliative care in congestive heart failure. J Am Coll Cardiol. 2009;54(5):386–396. [DOI] [PubMed] [Google Scholar]
- 6.Yancy CW, Jessup M, Bozkurt B, et al. 2015 ACCF/AHA guideline for the management of heart failure: A report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2015;128(16):e240–319. [DOI] [PubMed] [Google Scholar]
- 7.Bakitas M, Macmartin M, Trzepkowski K, et al. Palliative care consultations for heart failure patients: how many, when, and why? J Card Fail. 2013;19(3):193–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Greener DT, Quill T, Amir O, Szydlowski J, Gramling RE. Palliative care referral among patients hospitalized with advanced heart failure. J Palliat Med. 2014;17(10):1115–1120.. [DOI] [PubMed] [Google Scholar]
- 9.Gupta N, Shahreyar M, Muppidi V, Gaglianello N, Papp MA, Cinquegrani MP. Abstract 13065: Trends, Predictors and Outcomes in Heart Failure Patients undergoing Palliative Care. Circ . 2014;130(Suppl 2):A13065–A13065. [Google Scholar]
- 10.Beernaert K, Cohen J, Deliens L, et al. Referral to palliative care in COPD and other chronic diseases: a population-based study. Respir Med. 2013;107(11):1731–1739. [DOI] [PubMed] [Google Scholar]
- 11.Wachterman MW, Pilver C, Smith D, Ersek M, Lipsitz SR, Keating NL. Quality of end-of-life care provided to patients with different serious illnesses. JAMA Intern Med. 2016;176(8):1095–1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Olmsted CL, Johnson AM, Kaboli P, Cullen J, Vaughan-Sarrazin MS. Use of palliative care and hospice among surgical and medical specialties in the Veterans Health Administration. JAMA Surg. 2014;149(11):1169–1175. [DOI] [PubMed] [Google Scholar]
- 13.Murthy SB, Moradiya Y, Hanley DF, Ziai WC. Palliative care utilization in nontraumatic intracerebral hemorrhage in the United States. 2016; 44(3):575–582. [DOI] [PubMed] [Google Scholar]
- 14.Keenan HT, Sheetz J, Bratton SL. Differences in characteristics of dying children who receive and do not receive palliative care. 2013;132(1):72–78. [DOI] [PubMed] [Google Scholar]
- 15.Okafor PN, Stobaugh DJ, Nnadi AK, Talwalkar JA. Determinants of palliative care utilization among patients hospitalized with metastatic gastrointestinal malignancies. 2015; 34(3):269–274. [DOI] [PubMed] [Google Scholar]
- 16.Centers for Disease Control. International Classifiication of Diseases Ninth Revision, Clinical Modification. Available from http://www.cdc.gov/nchs/icd/icd9cm.htm. Accessed May 1st, 2017.
- 17.Cassel JB, Jones AB, Meier DE, Smith TJ, Spragens LH, Weissman D. Hospital mortality rates : How is palliative care taken into account ? J Pain Symptom Manage. 2010;40(6):914–925. [DOI] [PubMed] [Google Scholar]
- 18.Capello CF, Meier DE, Cassel CK. Payment code for hospital-based palliative care: Help or hindrance? J Palliat Med. 1998;1(2):155–163. [DOI] [PubMed] [Google Scholar]
- 19.Hua M, Li G, Clancy C, Morrison RS, Wunsch H. Validation of the V66.7 code for palliative care consultation in a single academic medical center. J Palliat Med. 2017;20(4):372–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Szekendi MK, Vaughn J, Lal A, Ouchi K, Williams MV. The prevalence of inpatients at 33 U.S. hospitals appropriate for and receiving referral to palliative care. J Palliat Med. 2016;19(4):360–372. [DOI] [PubMed] [Google Scholar]
- 21.Qureshi AI, Adil MM, Suri MFK, et al. Rate of utilization and determinants of withdrawal of care in acute ischemic stroke treated with thrombolytics in USA. Med Care. 2013;51(12):1094–1100. [DOI] [PubMed] [Google Scholar]
- 22.Veterans Health Administration. VHA Directive 2008 – 041:Hospice and palliative care workload capture. Available from https://www.va.gov/vhapublications/publications.cfm?pub=1. Accessed May 1st, 2017.
- 23.Wolfsfeld L, Zhu S, Hendricks A. HCFE data brief: Hospice and palliative care for VA patients. 2004. Available from https://www.hcfe.research.va.gov/docs/db_2004_06.pdf. Accessed May 1st, 2017.
- 24.Fultz SL, Skanderson M, Mole LA, et al. Development and verification of a “virtual” cohort using the National VA Health Information System. Med Care. 2006;44(8 Suppl 2):S25–30. [DOI] [PubMed] [Google Scholar]
- 25.Justice AC, Dombrowski E, Conigliaro J, et al. Veterans Aging Cohort Study (VACS): Overview and description. Med Care. 2006;44:1–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rosenman M, He J, Martin J, et al. Database queries for hospitalizations for acute congestive heart failure: Flexible methods and validation based on set theory. J Am Med Inform Assoc. 2014;21(2):345–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.National Consensus Project For Quality Palliative Care. Clinical practice guidelines for quality palliative care. 3rd ed. Pittsburg, PA: Available from www.nationalconsensusproject.org. Accessed October 1st, 2016. [Google Scholar]
- 28.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research Electronic Data Capture (REDCap) - A metadata driven methodology and workflow process for providing translational research informatict support. J Biomed Inform. 2009;42(2):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Justice AC, McGinnis KA, Skanderson M, et al. Towards a combined prognostic index for survival in HIV infection: The role of “non-HIV” biomarkers. HIV Med. 2010;11(2):143–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Akgün KM, Tate JP, Crothers K, et al. An adapted frailty-related phenotype and the VACS Index as predictors of hospitalization and mortality in HIV-Infected and uninfected Individuals. 2014;67(4):7–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Akgün KM, Gordon K, Pisani M, et al. Risk factors for hospitalization and medical intensive care unit (MICU) admission among HIV-infected Veterans. J Acquir Immune Defic Syndr. 2013;62(1):52–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Salinas JL, Rentsch C, Marconi VC, et al. Baseline, time-updated, and cumulative HIV care metrics for predicting acute myocardial infarction and all-cause mortality. Clin Infect Dis. 2016:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Veterans Health Administration. VHA Directive 2008 – 039. Palliative care consult teams (PCCT). Available from https://www.va.gov/vhapublications/publications.cfm?pub=1. Accessed March 1st, 2017.
- 34.Centers for Medicare and Medicaid Services. 2016. ICD-10-CM and general equivalency mappings. Available from https://www.cms.gov/Medicare/Coding/ICD10/2016-ICD-10-CM-and-GEMs.html. Accessed January 1, 2016.
- 35.Meier DE. Increased access to palliative care and hospice services: Opportunities to improve value in health care.Milbank quarterly. 2011;89(3):343–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Johnston B, Conly J. Solid organ transplantation and HIV: A changing paradigm. Can J Infect Dis Med Microbiol. 2008;19(6):425–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Uriel N, Nahumi N, Colombo PC, et al. Advanced heart failure in patients infected with human immunodeficiency virus: Is there equal access to care? J Hear Lung Transplant. 2014;33(9):924–930. [DOI] [PubMed] [Google Scholar]


