Abstract
Objective
The number of liver cancer patients in China accounts for more than half of the world. However, China currently lacks national, multicenter economic burden data, and meanwhile, measuring the differences among different subgroups will be informative to formulate corresponding policies in liver cancer control. Thus, the aim of the study was to measure the economic burden of liver cancer by various subgroups.
Methods
A hospital-based, multicenter and cross-sectional survey was conducted during 2012-2014, covering 39 hospitals and 21 project sites in 13 provinces across China. The questionnaire covers clinical information, sociology, expenditure, and related variables. All expenditure data were reported in Chinese Yuan (CNY) using 2014 values.
Results
A total of 2,223 liver cancer patients were enrolled, of whom 59.61% were late-stage cases (III-IV), and 53.8% were hepatocellular carcinoma. The average total expenditure per liver cancer patient was estimated as 53,220 CNY, including 48,612 CNY of medical expenditures (91.3%) and 4,608 CNY of non-medical expenditures (8.7%). The average total expenditures in stage I, II, III and stage IV were 52,817 CNY, 50,877 CNY, 50,678 CNY and 54,089 CNY (P>0.05), respectively. Non-medical expenditures including additional meals, additional nutrition care, transportation, accommodation and hired informal nursing were 1,453 CNY, 839 CNY, 946 CNY, 679 CNY and 200 CNY, respectively. The one-year out-of-pocket expenditure of a newly diagnosed patient was 24,953 CNY, and 77.2% of the patients suffered an unmanageable financial burden. Multivariate analysis showed that overall expenditure differed in almost all subgroups (P<0.05), except for sex, clinical stage, and pathologic type.
Conclusions
There was no difference in treatment expenditure for liver cancer patients at different clinical stages, which suggests that maintaining efforts on treatment efficacy improvement is important but not enough. To furtherly reduce the overall economic burden from liver cancer, more effort should be given to primary and secondary prevention strategies.
Keywords: Liver cancer, medical expenditure, non-medical expenditure, economic burden
Introduction
The GLOBOCAN estimates that liver cancer is listed as the sixth most frequently diagnosed cancer and the fourth leading cause of cancer death worldwide in 2018, with 841,000 new cases and 782,000 deaths each year; the number of liver cancer patients in China accounts for more than half of the world (1). The National Cancer Center of China estimated that the number of new liver cancer cases was 466,100 in China in 2015, and the number of deaths was 422,100 (2). However, China currently lacks national, multicenter economic burden data, and meanwhile measuring the differences among different subgroups will be informative to formulate corresponding policies in liver cancer control.
World Health Organization (WHO) emphasizes that the most effective strategies for the prevention and control of cancer are early detection, diagnosis and treatment. The central government of China has been providing continuous support to the early detection and treatment research of cancers, which eventually led this to become one of national major public health projects in 2012. The project, officially named the Cancer Screening Program in Urban China (CanSPUC), has mainly covered population aged 40−69 years, and expanded to 17 provinces and regions since August 2012. The project consists of three parts, assessment of high-risk groups (community-based), hospital-based clinical screening, and a multi-stage comprehensive health economic evaluation.
As a part of the overall health economic evaluation component, the aim of the current study was to measure the economic burden of liver cancer by various subgroups.
Materials and methods
Overall design and study sites selection
This is a hospital-based, multicenter, cross-sectional survey. From 2012 to 2014, a total of 39 hospitals and 21 project sites were designated by the government from 13 provinces or cities, including Beijing, Chongqing, Jinan in Shandong province, Nantong, Xuzhou in Jiangsu province, Guangzhou, Dongguan, Foshan, Shenzhen and Zhongshan in Guangdong province, Hangzhou, Ningbo in Zhejiang province, Tangshan in Hebei province, Tieling in Liaoning province, Changsha in Hunan province, Harbin, Daqing in Heilongjiang province, Zhengzhou in Henan province, Urumqi in Xinjiang province, Lanzhou, Jinchang in Gansu province. Summary of study sites and hospitals involved is listed in Supplementary Table S1 .
S1. Summary of study sites and hospitals involved in 13 provinces or cities in China.
| Province | General information at provincial level | Specific information on study sites and hospitals involved | |||||
| Population size in 2013* (×104) | GDP per capita in 2013* (CNY) | No. of sites (city) | Total No. of hospitals | General hospitals (n) | Specialized hospitals (n) | ||
| *, Based on China Statistical Yearbook 2014, available from http://www.stats.gov.cn/tjsj/ndsj/2014/indexce.htm; **, Including Guangzhou, Shenzhen, Zhongshan, Dongguan and Foshan. | |||||||
| Shandong | 9,733 | 56,323 | 1 (Jinan) | 1 | 0 | 1 | |
| Beijing | 2,115 | 93,213 | 1 (Beijing) | 3 | 1 | 2 | |
| Jiangsu | 7,939 | 74,607 | 2 (Nantong, Xuzhou) | 2 | 0 | 2 | |
| Guangdong | 10,644 | 58,540 | 5 (Five cities**) | 6 | 5 | 1 | |
| Zhejiang | 5,498 | 68,462 | 2 (Hangzhou, Ningbo) | 2 | 1 | 1 | |
| Hebei | 7,333 | 38,716 | 1 (Tangshan) | 3 | 3 | 0 | |
| Liaoning | 4,390 | 61,686 | 1 (Tieling) | 1 | 1 | 0 | |
| Hunan | 6,691 | 36,763 | 1 (Changsha) | 1 | 0 | 1 | |
| Heilongjiang | 3,835 | 37,509 | 2 (Harbin, Daqing) | 6 | 5 | 1 | |
| Henan | 9,413 | 34,174 | 1 (Zhengzhou) | 1 | 0 | 1 | |
| Xinjiang | 2,264 | 37,181 | 1 (Urumchi) | 1 | 0 | 1 | |
| Gansu | 2,582 | 24,296 | 2 (Lanzhou, Jinchang) | 9 | 7 | 2 | |
| Chongqing | 2,970 | 42,795 | 1 (Chongqing) | 1 | 0 | 1 | |
| Overall | − | − | 21 | 37 | 23 | 14 | |
Considering the budget from the government and previous experience, a total of 3,120 liver cancer patients were expected for the 13 study provinces. For each province, in accordance with a uniform design scheme, a stratified convenience sampling approach was used for selecting 240 clinically confirmed, primary prevalent liver cancer patients who were undergoing treatment in the study hospitals (including both newly and previously diagnosed patients). All respondents were interviewed face-to-face using a structured questionnaire at the time of discharge when most treatment expenditures were incurred. Prior to the survey, we registered participation of all invited patients; we also recorded basic information including age, sex and cancer stage to facilitate exclusion. For patients who were in very poor condition, family member(s) or other caregivers helped with the interview; all the other interviewees were the patients themselves.
This study was approved by the Institutional Review Board of Cancer Hospital, Chinese Academy of Medical Sciences, as part of a broader health economic evaluation project based on the CanSPUC program. All subjects participated were aware of the investigation process and signed informed consent forms.
Data collection
The designed questionnaire mainly covered the following parts: 1) demographic and societal information (e.g. name, sex, age, education, occupation, previous-year household income, and healthcare insurance type); 2) clinical information (e.g. clinical stage, pathologic diagnosis and therapeutic regimen); 3) by-clinical-visit expenditure occurred until the survey date, covering both outpatient and inpatient, occurring either within or outside the study hospitals, e.g. the start date of treatment, hospitalization duration, overall medical expenditure, overall and detailed non-medical expenditure (e.g. transportation, additional meals and nutrition, accommodation, fee of hiring informal nursing), predicted reimbursement ratio, and self-reported financial pressure; and 4) time loss of the to-date whole course to clinical visits, including working days loss of patients and of accompanying persons or informal caregivers (relatives and friends).
Quality control
All the investigators have received the standard consultants and training program. One-on-one, face-to-face interview form was conducted by trained interviewers. The interviewers record the details of each participant and their collaboration rating at the end of the questionnaire. Then they evaluate by segment the reliability of the data collected. The questionnaire consists of a multilevel quality control procedure: first of all, the interviewer conducts the self-evaluation, then the quality control staff will check the result again within 2 d after the interview. If necessary, we correct the mistakes and fill in the missing parts of the clinical information not obtained by using the electronic medical system.
Several rounds of verification of on-site input data and EpiData software (Version 3.1; The EpiData Association, Odense, Denmark) were used to conduct the double entry. Furthermore, they process the logical verification and data analysis on SAS software (Version 9.2; SAS Institute Inc., Cary, USA), eliminating records of all variables like sex, age, total medical and non-medical expenditures that did not come from first-tier hospitals.
Statistical analysis
Group variables include clinical stage, type of hospital, age, sex, education, occupation, health insurance type, family income, pathological types, therapeutic regimen and region. The medical and non-medical expenditures, average total expenditures of each patient were compared between subgroups. Analyzing successively possible factors of average total expenditures, the economic pressure on patient families after average total expenditures reimbursement, the composition of non-medical expenditures and time loss of patients and their family members, we defined a newly diagnosed course as 2 months before diagnosis and 10 months after diagnosis, and all patient-paid medical expenditure items and non-medical expenditure of a newly diagnosed course as out-of-pocket expenditure. At the same time, we used generalized linear models-gamma conjugate (A1) for multivariate analysis, applied the natural logarithmic conversion for expenditures data that has larger degree of dispersion, compared two independent samples with the student’s t test, compared more than two groups by using variance-analysis and using Student-Newman-Keuls Test (SNK) test pairwise comparisons within the group, and compared rates with Chi-square test. All data statistics were tested bilaterally, and P<0.05 was considered statistically significant. All expenditure data were converted using local consumer price index in 2014.
Results
A total of 2,223 patients with liver cancer were included in the current analysis, and mean age at diagnosis was 55.7±11.2 years. Of the overall patients, 79.2% were males, 75.6% were from specialized hospitals, 40.0% owned a New Cooperative Medical Scheme (NCMS) medical insurance and the median income per patient in last 5 years was 20,000 Chinese Yuan (CNY) (P25−P75: 10,000−40,000). Patients with liver cancer at stage I, II, III and IV accounted for 13.5%, 22.2%, 42.6 and 17.1% of the overall cases (remaining were reported), respectively. More than half (53.8%) of the overall pathological types were hepatocellular carcinoma (HCC) and more than half (50.2%) of the patients received symptomatic treatment or palliative care alone.Table 1 shows additional details.
1. Characteristics of included liver cancer patients (N=2,223).
| Variables | n (%) |
| CNY, Chinese Yuan. | |
| Hospital type | |
| General | 543 (24.4) |
| Specialized | 1,680 (75.6) |
| Age at diagnosis (year) | |
Mean age at diagnosis (
 )
)
|
55.7±11.2 |
| <45 | 362 (16.3) |
| 45−54 | 633 (28.5) |
| 55−64 | 745 (33.5) |
| ≥65 | 483 (21.7) |
| Gender | |
| Male | 1,760 (79.2) |
| Female | 463 (20.8) |
| Education | |
| Primary school or below | 652 (29.3) |
| Junior high school | 800 (36.0) |
| Senior high school | 565 (25.4) |
| Undergraduate or over | 206 (9.3) |
| Occupation | |
| Farmer | 902 (40.6) |
| Enterprise or company employee/worker | 567 (25.5) |
| Self-employed or unemployed | 312 (14.0) |
| Retiree | 236 (10.6) |
| Staff in institution/civil servant | 173 (7.8) |
| Other | 33 (1.5) |
| Previous year household income
(N=2,153) (  ) (CNY)
) (CNY)
|
56,468±42,696 |
| Previous year household income (N=2,153) [median (P25−P75)] (CNY) | 48,000
(28,000−75,000) |
| Previous year household income (CNY) | |
| <20,000 | 250 (11.6) |
| 20,000−39,999 | 606 (28.1) |
| 40,000−69,999 | 654 (30.4) |
| ≥70,000 | 643 (29.9) |
Average income per patient in last 5 years (N=2,188) (
 ) (CNY)
) (CNY)
|
29,958±27,692 |
| Median income per patient in last 5 years (N=2,188) [median (P25−P75)] (CNY) | 20,000
(10,000−40,000) |
| Number of family members (N=2,195) [median (P25−P75)] | 4 (2−5) |
| Health-care insurance type | |
| Urban employees basic medical insurance | 852 (38.3) |
| Urban residents basic medical insurance | 400 (18.0) |
| New rural cooperative medical scheme | 890 (40.0) |
| Commercial insurance | 19 (0.9) |
| Self-financed | 40 (1.8) |
| Other | 22 (1.0) |
| Clinical stage | |
| I | 299 (13.5) |
| II | 493 (22.2) |
| III | 946 (42.6) |
| IV | 379 (17.1) |
| Not reported | 106 (4.8) |
| Pathological type | |
| Hepatocellular carcinoma | 1,196 (53.8) |
| Other | 235 (10.6) |
| Not reported | 792 (35.6) |
| Therapeutic regimen (N=2,040) | |
| Surgery | 438 (21.5) |
| Chemotherapy | 354 (17.4) |
| Surgery and postoperative chemotherapy | 127 (6.2) |
| Symptomatic treatment | 1,024 (50.2) |
| Concurrent chemoradiotherapy | 20 (1.0) |
| Radiotherapy | 33 (1.6) |
| Neoadjuvant chemoradiotherapy and surgery | 44 (2.2) |
| Number of clinical visits [median (P5−P95)] | 2 (1−5) |
| Number of admissions [median (P5−P95)] | 1 (1−5) |
Length of stay per case (N=2,222) (
 ) (d)
) (d)
|
27±33 |
| Length of stay per case (N=2,222) [median (P25−P75)] (d) | 19 (11−32) |
The average total expenditure per liver cancer patient was estimated as 53,220 CNY, including 48,612 CNY of medical expenditure and 4,608 CNY of non-medical expenditure. There are significantly differences among different subgroups, including hospital type, age, education, occupation, insurance type, household income and treatment (all P values <0.005). Table 2 shows more subgroup results on the overall, medical and non-medical expenditure. Further, the multivariate analysis (Table 3 ) confirmed that patients in specialized hospitals, patients who were diagnosed <45 years, patients with education level of university or higher, patients who were public sector employee, patients with urban employee basic medical insurance or patients with higher household income were likely to spend more on treatment, whereas patients with commercial insurance, patients received surgery and postoperative chemotherapy or neoadjuvant chemotherapy and surgery spent less on treatment compared with patients received only surgery.
2. Overall and subgroup analysis of medical and non-medical expenditure for liver cancer diagnosis and treatment per case.
| Variables | Medical expenditure (CNY) | Non-medical
expenditure (CNY) |
Overall expenditure | ||
| Value (CNY) | Statistics* | P* | |||
| *, Two-sample Student test after logarithm transition for two groups comparative analysis, analysis of variance (ANOVA) test after logarithm transition for more than two groups comparative analysis. | |||||
| Total | 48,612 | 4,608 | 53,220 | − | − |
| Hospital type | |||||
| General | 40,570 | 3,773 | 44,343 | −5.56 | <0.001 |
| Specialized | 51,211 | 4,878 | 56,089 | ||
| Age at diagnosis (year) | |||||
| <45 | 52,605 | 4,880 | 57,485 | 2.65 | 0.047 |
| 45−54 | 50,595 | 4,779 | 55,374 | ||
| 55−64 | 46,474 | 4,745 | 51,219 | ||
| ≥65 | 46,318 | 3,967 | 50,285 | ||
| Gender | |||||
| Male | 49,294 | 4,630 | 53,924 | 1.28 | 0.201 |
| Female | 46,018 | 4,525 | 50,543 | ||
| Education | |||||
| Primary school or below | 43,080 | 3,597 | 46,677 | 23.21 | <0.001 |
| Junior high school | 45,280 | 3,994 | 49,274 | ||
| Senior high school | 52,873 | 5,381 | 58,254 | ||
| Undergraduate or over | 67,373 | 8,073 | 75,446 | ||
| Occupation | |||||
| Farmer | 42,643 | 3,702 | 46,345 | 9.55 | <0.001 |
| Enterprise or company employee/worker | 49,453 | 4,508 | 53,961 | ||
| Self-employed or unemployed | 48,402 | 4,738 | 53,140 | ||
| Retiree | 56,053 | 7,255 | 63,308 | ||
| Staff in institution/civil servant | 67,797 | 5,794 | 73,591 | ||
| Other | 45,513 | 4,696 | 50,209 | ||
| Health-care insurance type | |||||
| Urban employees basic medical insurance | 53,250 | 5,286 | 58,536 | 8.49 | <0.001 |
| Urban residents basic medical insurance | 51,452 | 4,798 | 56,250 | ||
| New rural cooperative medical scheme | 43,515 | 3,933 | 47,448 | ||
| Commercial insurance | 20,876 | 1,345 | 22,221 | ||
| Self-financed | 44,158 | 4,345 | 48,503 | ||
| Other | 55,604 | 5,513 | 61,117 | ||
| Previous year household income | |||||
| <20,000 | 40,684 | 4,212 | 44,896 | 8.57 | <0.001 |
| 20,000−39,999 | 45,170 | 4,390 | 49,560 | ||
| 40,000−69,999 | 50,461 | 4,814 | 55,275 | ||
| ≥70,000 | 53,402 | 4,720 | 58,122 | ||
| Clinical stage | |||||
| I | 48,644 | 4,173 | 52,817 | 1.56 | 0.198 |
| II | 46,616 | 4,261 | 50,877 | ||
| III | 46,319 | 4,359 | 50,678 | ||
| IV | 49,063 | 5,026 | 54,089 | ||
| Therapeutic regimen | |||||
| Surgery | 57,641 | 4,970 | 62,611 | 19.82 | <0.001 |
| Chemotherapy | 45,773 | 4,652 | 50,425 | ||
| Surgery and postoperative chemotherapy | 55,042 | 5,070 | 60,112 | ||
| Symptomatic treatment | 44,837 | 4,644 | 49,481 | ||
| Concurrent chemoradiotherapy | 50,892 | 4,524 | 55,416 | ||
| Radiotherapy | 56,251 | 4,943 | 61,194 | ||
| Neoadjuvant chemoradiotherapy and surgery | 42,449 | 4,747 | 47,196 | ||
| Pathological type | |||||
| Hepatocellular carcinoma | 50,937 | 4,592 | 55,529 | 0.96 | 0.338 |
| Other | 48,143 | 4,213 | 52,356 | ||
3. Multivariate analysis of overall expenditure for diagnosis and treatment of patients with liver cancer.
| Characteristic | Estimate (95% Cl) | P |
| 95% CI, 95% confidence interval. | ||
| Intercept | 10.4 (10.2, 10.7) | <0.001 |
| Hospital type (Ref=general) | ||
| Specialized | 0.2 (0.1, 0.3) | <0.001 |
| Age at diagnosis (year) (Ref≥65) | ||
| <45 | 0.2 (0.0, 0.3) | 0.030 |
| 45−54 | 0.1 (0.0, 0.3) | 0.080 |
| 55−64 | 0.0 (−0.2, 0.1) | 0.443 |
| Sex (Ref=females) | ||
| Males | 0.0 (−0.1, 0.1) | 0.828 |
| Education (Ref=primary school or below) | ||
| Junior high school | 0.0 (−0.1, 0.1) | 0.573 |
| Senior high school | 0.1 (−0.1, 0.2) | 0.388 |
| Undergraduate or higher | 0.2 (0.0, 0.4) | 0.015 |
| Occupation (Ref=self-employee or unemployee) | ||
| Farmer | 0.0 (−0.2, 0.1) | 0.604 |
| Enterprise or company employee/worker | 0.1 (−0.1, 0.2) | 0.248 |
| Retiree | 0.0 (−0.2, 0.2) | 0.983 |
| Staff in institution/civil servant | 0.5 (0.3, 0.7) | <0.001 |
| Other | 0.0 (−0.3, 0.4) | 0.879 |
| Healthcare insurance type (Ref=new rural cooperative medical scheme) | ||
| Urban employee basic medical insurance | 0.2 (0.0, 0.3) | 0.034 |
| Urban resident basic medical insurance | 0.1 (0.0, 0.2) | 0.196 |
| Commercial insurance | −0.6 (−1.1, −0.1) | 0.031 |
| Self-financed | 0.1 (−0.3, 0.4) | 0.663 |
| Other | 0.3 (−0.1, 0.7) | 0.132 |
| Previous-year household income (CNY) (Ref<20,000) | ||
| 20,000−39,999 | 0.1 (−0.1, 0.3) | 0.240 |
| 40,000−69,999 | 0.2 (0.0, 0.3) | 0.032 |
| ≥70,000 | 0.2 (0.0, 0.4) | 0.022 |
| Clinical stage (Ref=I) | ||
| II | −0.1 (−0.2, 0.0) | 0.100 |
| III | 0.1 (−0.1, 0.2) | 0.375 |
| IV | 0.1 (−0.1, 0.3) | 0.183 |
| Pathologic type (Ref=others) | ||
| Adenocarcinoma | 0.0 (−0.1, 0.1) | 0.810 |
| Therapeutic regimen (Ref=surgery) | ||
| Chemotherapy | −0.1 (−0.4, 0.2) | 0.493 |
| Surgery and postoperative chemotherapy | −0.2 (−0.4, −0.1) | <0.001 |
| Symptomatic treatment | −0.1 (−0.2, 0.1) | 0.552 |
| Concurrent chemoradiotherapy | −0.1 (−0.4, 0.1) | 0.289 |
| Radiotherapy | 0.0 (−0.5, 0.5) | 0.934 |
| Neoadjuvant chemotherapy and surgery | −0.2 (−0.3, −0.1) | <0.001 |
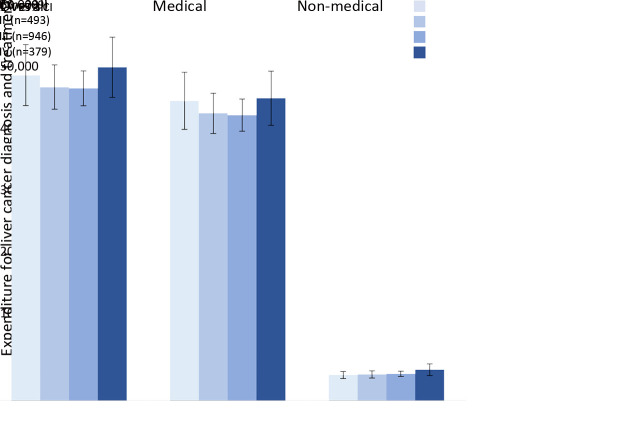
However, no statistical difference of average total expenditure was found among patients with liver cancer at stage I−IV, which were 52,817 CNY, 50,877 CNY, 50,678 CNY and 54,089 CNY, respectively (P=0.198 inTable 2 and all P values >0.05 in the multivariate analysis in Table 3 ). There is only about 300 CNY difference between stage I and IV, which is also less clinically significant. Figure 1 presents more details on the medical and non-medical expenditures in different clinical stages. In addition, there was also no expenditure difference among patients with different genders and pathological types (Table 2 ,3 ).
1.
Medical and non-medical expenditure for liver cancer diagnosis and treatment, by clinical stage. 95% CI, 95% confidence interval; CNY, Chinese Yuan.
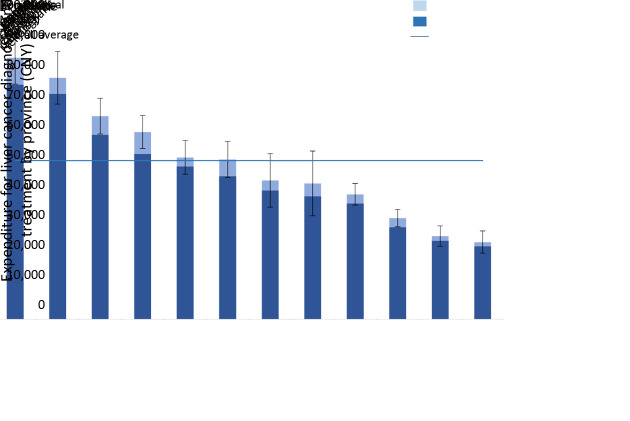
Expenditure heterogeneity was observed among regions. Expenditures of 8 provinces appeared higher and 6 provinces seemed lower than the national average. Live cancer patients treated in Beijing, Xinjiang and Shandong usually spent more on treatment; while, live cancer patients treated in Hebei, Chongqing and Heilongjiang usually spent less on treatment. Figure 2 shows more information of more provinces.
2.
Medical and non-medical expenditure for liver cancer diagnosis and treatment, by province. 95% CI, 95% confidence interval; CNY, Chinese Yuan.
Table 4 shows the overall expenditure of a newly diagnosed course, the pocket expenditures of the patients and their situation of economic pressure. The total expenditure of a newly diagnosed course is equal to 46,070 CNY, among which the reimbursed medical expenditures account for 46.9%. The average of pocket expenditures is 24,953 CNY. And 77.2% of the patients cannot afford the non-reimbursed expenditures, 45.8% of them have lots of pressure and 31.4% have a certain pressure.
4. Economic impact of overall expenditure on liver cancer patient’s family.
| Variables | Expenditure of newly diagnosed course/Annual expenditure of illness* (CNY) (N=2,175) | Self-reported predicted reimbursement ratio (%) (N=2,175) | Out-of-pocket expenditure**(A) (CNY) (N=2,175) | Previous year household income (N=2,153 ) | Self-reported degree of economic
pressure (%) (N=2,210) |
||||||
| Amount (B) (CNY) | Ratio (A/B) | Not at all | Somewhat but manageable | Heavy | Overwhelmed | P*** | |||||
| *, The 12-month duration covers 2 months before and 10 months after the diagnosis; **, Out-of-pocket expenditure=(∑(1 − Self-reported predicted reimbursement ratio) × Medical expenditure of newly diagnosed course + Non-medical expenditure of newly diagnosed course)/n; ***, Chi-square tests; CNY, Chinese Yuan. | |||||||||||
| Total | 46,070 | 46.9 | 24,953 | 56,468 | 0.4 | 7.8 | 15.0 | 31.4 | 45.8 | − | |
| Hospital type | |||||||||||
| General | 38,207 | 57.5 | 18,562 | 73,501 | 0.3 | 12.8 | 20.0 | 32.9 | 34.4 | <0.001 | |
| Specialized | 48,611 | 43.3 | 27,074 | 50,961 | 0.5 | 6.2 | 13.4 | 31.0 | 49.5 | ||
| Age at diagnosis (year) | |||||||||||
| <45 | 51,019 | 43.2 | 29,796 | 62,202 | 0.5 | 6.4 | 11.7 | 31.1 | 50.8 | <0.001 | |
| 45−54 | 46,775 | 44.3 | 26,440 | 56,066 | 0.5 | 5.3 | 15.4 | 29.5 | 49.8 | ||
| 55−64 | 45,170 | 48.5 | 24,050 | 54,510 | 0.4 | 8.0 | 14.3 | 32.8 | 44.9 | ||
| ≥65 | 42,824 | 50.5 | 20,660 | 55,676 | 0.4 | 11.9 | 17.9 | 32.2 | 38.0 | ||
| Gender | |||||||||||
| Male | 46,569 | 46.7 | 25,183 | 56,622 | 0.4 | 7.9 | 14.6 | 31.5 | 45.9 | 0.800 | |
| Female | 44,171 | 47.4 | 24,065 | 55,873 | 0.4 | 7.2 | 16.3 | 31.3 | 45.2 | ||
| Education | |||||||||||
| Primary school or below | 40,974 | 41.4 | 23,906 | 43,198 | 0.6 | 6.3 | 11.0 | 32.7 | 50.0 | <0.001 | |
| Junior high school | 42,973 | 44.2 | 24,388 | 54,542 | 0.4 | 5.2 | 16.2 | 32.5 | 46.1 | ||
| Senior high school | 49,755 | 52.0 | 25,614 | 63,641 | 0.4 | 10.9 | 15.5 | 29.1 | 44.5 | ||
| Undergraduate or over | 64,114 | 61.2 | 28,879 | 85,523 | 0.3 | 14.1 | 21.4 | 29.6 | 35.0 | ||
| Occupation | |||||||||||
| Farmer | 41,180 | 36.1 | 26,514 | 41,770 | 0.6 | 2.0 | 8.4 | 33.4 | 56.2 | <0.001 | |
| Enterprise or company
employee/worker |
45,802 | 56.1 | 21,044 | 62,700 | 0.3 | 13.6 | 20.0 | 27.7 | 38.7 | ||
| Self-employed or
unemployed |
46,555 | 41.6 | 27,577 | 72,497 | 0.4 | 8.0 | 15.1 | 30.9 | 46.0 | ||
| Retiree | 54,054 | 60.7 | 25,236 | 67,599 | 0.4 | 15.0 | 20.1 | 29.5 | 35.5 | ||
| Staff in institution/civil
servant |
60,834 | 64.6 | 24,240 | 68,698 | 0.4 | 9.2 | 26.6 | 31.8 | 32.4 | ||
| Other | 45,245 | 42.7 | 26,482 | 56,242 | 0.5 | 3.0 | 9.1 | 60.6 | 27.3 | ||
| Health-care insurance type | |||||||||||
| Urban employees basic
medical insurance |
49,419 | 58.6 | 22,234 | 64,584 | 0.3 | 14.6 | 18.5 | 27.3 | 39.6 | <0.001 | |
| Urban residents basic
medical insurance |
47,668 | 49.8 | 23,591 | 60,320 | 0.4 | 6.0 | 18.8 | 33.8 | 41.4 | ||
| New rural cooperative
medical scheme |
42,510 | 36.8 | 27,571 | 44,620 | 0.6 | 1.9 | 9.6 | 33.6 | 54.8 | ||
| Commercial insurance | 22,221 | 10.6 | 20,336 | 46,842 | 0.4 | 5.3 | 5.3 | 36.8 | 52.6 | ||
| Self-financed | 41,799 | 0.0 | 41,799 | 104,514 | 0.4 | 7.5 | 22.5 | 40.0 | 30.0 | ||
| Other | 59,682 | 69.9 | 20,257 | 72,136 | 0.3 | 13.6 | 18.2 | 40.9 | 27.3 | ||
| Previous year household income (CNY) | |||||||||||
| <20,000 | 39,281 | 38.0 | 24,624 | 10,888 | 2.3 | 0.4 | 4.9 | 20.6 | 74.1 | <0.001 | |
| 20,000−39,999 | 44,199 | 42.0 | 26,124 | 26,983 | 1.0 | 2.7 | 8.1 | 31.6 | 57.6 | ||
| 40,000−69,999 | 45,246 | 46.9 | 24,011 | 50,150 | 0.5 | 8.1 | 16.6 | 31.0 | 44.2 | ||
| ≥70,000 | 51,529 | 55.5 | 25,012 | 108,404 | 0.2 | 15.0 | 24.3 | 35.3 | 25.4 | ||
| Clinical stage | |||||||||||
| I | 45,032 | 48.0 | 23,118 | 57,594 | 0.4 | 5.7 | 15.8 | 28.3 | 50.2 | 0.004 | |
| II | 44,479 | 47.9 | 24,062 | 53,461 | 0.5 | 6.5 | 15.5 | 26.0 | 51.9 | ||
| III | 44,573 | 44.6 | 24,592 | 54,950 | 0.5 | 9.0 | 13.7 | 34.9 | 42.5 | ||
| IV | 45,446 | 48.1 | 25,102 | 61,929 | 0.4 | 7.2 | 17.3 | 29.9 | 45.6 | ||
| Therapeutic regimen | |||||||||||
| Surgery | 59,301 | 47.0 | 32,520 | 61,581 | 0.5 | 8.5 | 14.2 | 36.9 | 40.4 | 0.005 | |
| Chemotherapy | 42,480 | 50.3 | 21,726 | 59,854 | 0.4 | 9.4 | 15.9 | 25.3 | 49.4 | ||
| Surgery and postoperative
chemotherapy |
52,035 | 48.5 | 27,420 | 60,440 | 0.5 | 2.4 | 17.3 | 40.2 | 40.2 | ||
| Symptomatic treatment | 41,113 | 44.5 | 22,958 | 53,408 | 0.4 | 8.26 | 14.65 | 30.68 | 46.4 | ||
| Concurrent
chemoradiotherapy |
52,664 | 39.1 | 35,458 | 59,800 | 0.6 | 15.8 | 26.3 | 36.8 | 21.1 | ||
| Radiotherapy | 49,076 | 52.7 | 24,359 | 54,040 | 0.5 | 6.3 | 21.9 | 25.0 | 46.9 | ||
| Neoadjuvant
chemoradiotherapy and surgery |
44,756 | 56.5 | 23,002 | 61,135 | 0.4 | 0.00 | 18.2 | 45.5 | 36.4 | ||
| Pathological type | |||||||||||
| Hepatocellular carcinoma | 48,150 | 48.1 | 25,896 | 56,536 | 0.5 | 5.2 | 15.2 | 30.5 | 49.1 | <0.001 | |
| Other | 47,567 | 50.2 | 23,787 | 69,449 | 0.3 | 21.5 | 22.3 | 36.5 | 19.7 | ||
The estimated reimbursement percentage of medical expenditures varies with different variables. Among all the variables, general hospital, diagnosed age ≥65 years old, females (sex subgroup), education of university and higher, staff in institution/civil servant (occupation), other (medical insurance types subgroup), family income of last year ≥70,000 CNY, phase IV (clinical stage), neoadjuvant chemoradiotherapy and surgery (therapeutic regimen), other (pathological types subgroup) have the largest proportion in each subgroup.
The same, the ratio of self-financed expenditures to total household income varies in different subgroups. Among all the variables, specialist hospital, diagnosed age <45 years old, males (sex subgroup), education of primary school and below, farmers (occupation), NCMS (medical insurance types subgroup), family income of last 5 year <20,000 CNY, phase II (clinical stage), concurrent chemoradiotherapy (therapeutic regimen), and HCC (pathological types subgroup) have higher ratio.
Table 5 shows the status of working time loss of patients and their accompanying persons (relatives or friends) due to medical treatment. In total, it takes about 73.1 d per person, including 41.7 d for patients and 31.4 d for accompanying persons. The statistical result shows that the loss of working time among sex, occupation, clinical stage and pathological types are not statistically significant. Among all the variables, specialist hospital, diagnosed age from 45 to 54 years old, males (sex subgroup), education of university and higher, staff in institution/civil servant (occupation), other (medical insurance types subgroup), family income of last year (40,000−69,999) CNY, phase II (clinical stage), radiotherapy (therapeutic regimen), and HCC (pathological types subgroup) have more loss of working days in each subgroup.
5. Time lost due to liver cancer diagnosis and treatment.
| Variables | Patients (N=2,139) (d) | Caregivers* (N=2,139) (d) | Overall number of days lost | ||
| Value (d) | Statistics** | P** | |||
| *, Patients’ relatives and friends; **, Two-sample Student test after logarithm transition for two groups comparative analysis; analysis of variance (ANOVA) test after logarithm transition for more than two groups comparison; CNY, Chinese Yuan. | |||||
| Total | 41.7 | 31.4 | 73.1 | − | − |
| Hospital type | |||||
| General | 40.5 | 27.9 | 68.4 | −4.21 | <0.001 |
| Specialized | 42.1 | 32.5 | 74.7 | ||
| Age at diagnosis (year) | |||||
| <45 | 45.2 | 28.6 | 73.8 | 3.45 | 0.016 |
| 45−54 | 45.9 | 34.4 | 80.3 | ||
| 55−64 | 38.0 | 31.3 | 69.3 | ||
| ≥65 | 39.3 | 29.6 | 68.9 | ||
| Sex | |||||
| Male | 42.4 | 31.8 | 74.2 | 0.94 | 0.346 |
| Female | 38.9 | 29.9 | 68.8 | ||
| Education | |||||
| Primary school or below | 38.2 | 30.9 | 69.1 | 2.95 | 0.031 |
| Junior high school | 42.8 | 29.9 | 72.7 | ||
| Senior high school | 41.7 | 33.4 | 75.1 | ||
| Undergraduate or over | 49.0 | 32.8 | 81.8 | ||
| Occupation | |||||
| Farmer | 40.0 | 31.0 | 70.9 | 1.17 | 0.320 |
| Enterprise or company employee/worker | 40.8 | 32.1 | 72.8 | ||
| Self-employed or unemployee | 42.1 | 27.1 | 69.2 | ||
| Retiree | 45.8 | 31.8 | 77.6 | ||
| Staff in institution/civil servant | 48.9 | 38.8 | 87.7 | ||
| Other | 37.1 | 29.3 | 66.4 | ||
| Health-care insurance type | |||||
| Urban employees’ basic medical insurance | 47.4 | 33.4 | 80.9 | 5.93 | <0.001 |
| Urban residents’ basic medical insurance | 37.8 | 32.5 | 70.3 | ||
| New rural cooperative medical scheme | 39.0 | 29.5 | 68.5 | ||
| Commercial insurance | 24.5 | 15.0 | 39.5 | ||
| Self-financed | 24.4 | 21.7 | 46.1 | ||
| Other | 46.3 | 37.6 | 84.0 | ||
| Previous year household income (CNY) | |||||
| <20,000 | 37.2 | 32.7 | 69.9 | 4.70 | 0.003 |
| 20,000−39,999 | 43.1 | 32.0 | 75.1 | ||
| 40,000−69,999 | 45.9 | 32.2 | 78.1 | ||
| ≥70,000 | 39.3 | 30.0 | 69.3 | ||
| Clinical stage | |||||
| I | 39.2 | 27.1 | 66.3 | 2.60 | 0.050 |
| II | 44.7 | 34.0 | 78.7 | ||
| III | 42.6 | 30.0 | 72.6 | ||
| IV | 39.5 | 35.2 | 74.7 | ||
| Therapeutic regimen | |||||
| Surgery | 42.6 | 25.5 | 68.1 | 4.05 | <0.001 |
| Chemotherapy | 41.2 | 35.4 | 76.6 | ||
| Surgery and postoperative chemotherapy | 38.7 | 28.4 | 67.1 | ||
| Symptomatic treatment | 43.8 | 32.3 | 76.1 | ||
| Concurrent chemoradiotherapy | 36.6 | 47.2 | 83.8 | ||
| Radiotherapy | 53.5 | 42.0 | 95.5 | ||
| Neoadjuvant chemoradiotherapy and surgery | 63.8 | 31.7 | 95.5 | ||
| Pathological type | |||||
| Hepatocellular carcinoma | 41.4 | 29.1 | 70.5 | 1.17 | 0.243 |
| Other | 41.1 | 27.9 | 69.0 | ||
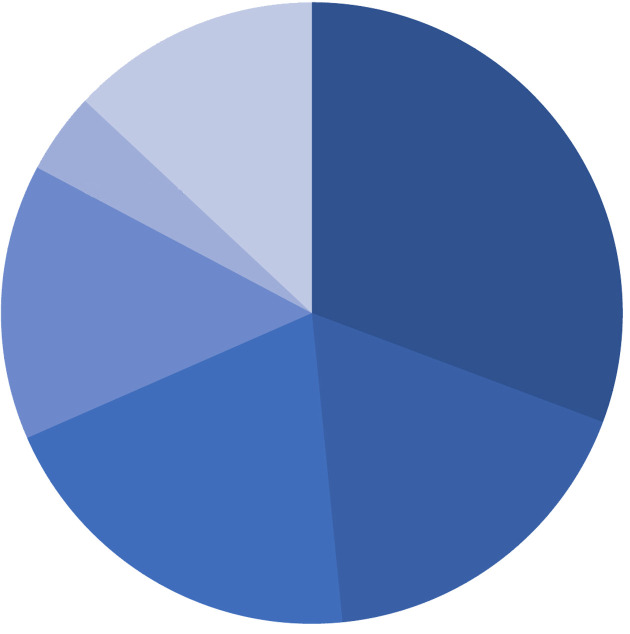
Figure 3 shows the specific composition ratio of non-medical expenditures. Additional meals, additional nutrition care, transportation, accommodation, hired informal nursing and other expenditures are 1,453 CNY, 839 CNY, 946 CNY, 679 CNY, 200 CNY and 616 CNY, respectively. These suggests that the economic burden of non-medical expenditure on liver cancer cannot be ignored.
3.
Proportional breakdown of non-medical expenditure for liver cancer diagnosis and treatment.
Discussion
As a major cancer in China, the medical expenditure of liver cancer accounts for a large proportion of the health economic burden. According to the analysis of Chinese malignant tumor registration data, the estimated age-standardized incidence rate of liver cancer in 2015 was 17.64 per 100,000, and the age-standardized incidence rate of liver cancer in urban China was 15.90 per 100,000. The age-standardized incidence rate of liver cancer in the Chinese male population was 26.74 per 100,000, only second to lung cancer and stomach cancer. It was estimated that the age-standardized mortality rate of liver cancer in China was only second to lung cancer (3). A comparative analysis of liver cancer shows that the incidence and mortality rate of liver cancer in Chinese men and women were both higher than the world average (4). Due to its large population and high incidence, China is the country with the largest number of liver cancer patients in the world, which places a heavy burden on people’s health and social wealth. Our results indicate that HCC is the major pathological type of liver cancer, accounting for approximately 54% of all cases in this study. In recent years, the average total expenditure per HCC patient is significantly higher than that of other pathological types of liver cancer in China. The United States also has a similar economic burden of HCC (5).
For most Chinese families, expensive medical expenditures were a heavy economic burden. From 2012 to 2014, the average medical expenditure of liver cancer was 48,612 CNY per case, and the average medical expenditure of patients with the pathological type of HCC was 50,937 CNY per case. The expenditure in this study was higher than that in previous systematic review and original articles on the economic burden of liver cancer in mainland China (6-9). However, a retrospective survey conducted in 2010 in Shandong, China found that direct medical expenditure in US dollars for inpatients with primary liver cancer amounted to $10,635 (10). According to the China Statistical Yearbook, the medical expenditure for each liver cancer clinic visit was almost equal to the one-year disposable income of urban residents (11). In Taiwan, China, the average 10-year expenditure of liver cancer patients was NT$ 418,554 (~82,706 CNY), which was higher than that in this study (12). For low-income families who usually do not have formal jobs and have lower health insurance, their economic burden on liver cancer will increase and may lead to poverty caused by disease.
The medical treatment expenditure in specialized hospitals is higher than the one in general hospitals. Because specialized hospitals have more various means of cancer treatment, more advanced treatment equipment, and more professional medical staff. In China, the vast majority of cancer patients are willing to choose a specialized hospital for their treatment. Patients with higher education levels have more knowledge about cancer and believe it can be cured, so they want to spend more time and money on cancer treatment. People with higher education levels normally have higher incomes and are able to afford the medical treatment expenditure than those with a lower education level. The total medical expenditures are related to the reimbursement rate and the ability to pay. Patients with high medical insurance reimbursement rates are more willing to receive treatment and spend more money on treatment. Urban employee basic medical insurance has the highest reimbursement rate, which is also consistent with the higher medical expenditure for the staff in the institution or civil servants and highly educated patients.
We found not statistical difference in diagnosis and treatment expenditure for liver cancer patients at different clinical stages, which indicates that liver cancer control in China is more challenging, compared with breast cancer and colorectal cancer (13,14). Maintaining efforts on treatment efficacy improvement is important but not enough. To furtherly reduce the overall economic burden from liver cancer, more effort should be given to primary and secondary prevention strategies.
In addition to calculating direct expenditure by consulting the medical bills of patients with liver cancer, indirect losses such as labor loss caused by liver cancer are huge. Five studies calculated individual-based indirect economic burdens, using the human capital method to combine the time of missed work and early death of liver cancer patients and the time of missed work of caregivers. The results showed that the median indirect economic burden was 73,440 CNY per case, distributed between 35,815 CNY and 166,967 CNY per case (15-19).
Patients with stage IV liver cancer have low survival rates, and high direct expenditure (medical and non-medical expenditures) and indirect expenditure associated with diagnosis and treatment imposes a heavy burden on individuals and families. Therefore, early detection, early diagnosis and early treatment of liver cancer are particularly important.
This study has some limitations. First, only tertiary and secondary hospitals were included in the survey, the situation in lower level hospitals is still not clear. Second, other than the direct medical expenditure for the current hospitalization, which was obtained from hospital financial data, all other outpatient and inpatient expenditures were self-reported and may be subjected to recall bias. Third, the questionnaire was adopted at hospital when patents completed most of the treatments before discharge, which to certain extent missed the expenditure occurred afterwards. Forth, there is a possible selection bias, which might occur because the study was not randomized. This study also has a potential limitation of retrospective nature. Since this study is currently the largest in China about the medical and non-medical expenditure of patients with liver cancer. Although there is a little design flaw, it is still very valuable. It is indeed the first study on the estimation of the economic burden of liver cancer, including medical expenditures and labor value losses.
These results provide evidence to help health policymakers understand the scale of economic burden of liver cancer in China so that the Chinese government can adjust relevant disease prevention and control strategies. In addition, the evidence from our study also contributes to our understanding of potential benefits to society in allocating more resources to prevent and treat liver cancer, as well as increasing insurance coverage in China. These findings have important policy implications for health care reform which is currently underway in China and focuses on how to reduce the burden of catastrophic disease for its citizens.
Conclusions
The findings indicate that there was no difference in treatment expenditure for liver cancer patients at different clinical stages, which suggests that maintaining efforts on treatment efficacy improvement is important but not enough. To further reduce the overall economic burden from liver cancer, more effort should be given to primary and secondary prevention strategies.
Acknowledgements
This study was supported by the State Key Projects Specialized on Infectious Diseases (No. 2017ZX10201201-008-002, No. 2017ZX10201201-006-003), and Sanming Project of Medicine in Shenzhen (No. SZSM201911015), the National Natural Science Foundation of China (No. 81974492, No. 81773521), Chinese Academy of Medical Sciences Innovation Fund for Medical Sciences (No. 2019-I2M-2-004), the Natural Science Foundation of Guangdong Province (No. 2020A151501478).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Contributor Information
Jufang Shi, Email: shijf@cicams.ac.cn.
Wanqing Chen, Email: chenwq@cicams.ac.cn.
References
- 1.Bray F, Ferlay J, Soerjomataram I, et al Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 2.Chen WQ, Zheng RS, Baade PD, et al Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66:115–32. doi: 10.3322/caac.21338. [DOI] [PubMed] [Google Scholar]
- 3.Chen WQ, Sun KX, Zheng RS, et al Cancer incidence and mortality in China, 2014. Chin J Cancer Res. 2018;30:1–12. doi: 10.21147/j.issn.1000-9604.2018.01.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Duan JJ, Yan YQ, Yang NN, et al International comparison analysis of China’s cancer incidence and mortality. Zhongguo Yi Xue Qian Yan Za Zhi. 2016;8:17–23. [Google Scholar]
- 5.Lang K, Danchenko N, Gondek K, et al The burden of illness associated with hepatocellular carcinoma in the United States. J Hepatol. 2009;50:89–99. doi: 10.1016/j.jhep.2008.07.029. [DOI] [PubMed] [Google Scholar]
- 6.Qiu WQ, Shi JF, Guo LW, et al Medical expenditure for liver cancer in urban China: A 10-year multicenter retrospective survey (2002-2011) J Cancer Res Ther. 2018;14:163–70. doi: 10.4103/jcrt.JCRT_709_16. [DOI] [PubMed] [Google Scholar]
- 7.Zhang YF, Guo LW, Bai FZ, et al Daily medical expenditures for patients with liver cancer in China from 2002 to 2011: a multicenter retrospective survey. Zhongguo Xun Zheng Yi Xue Za Zhi. 2018;18:434–41. doi: 10.7507/1672-2531.201802030. [DOI] [Google Scholar]
- 8.Yang J, Wang L, Shi CL, et al Economic burden of liver cancer in China during 1996-2015: a systematic review. Zhonghua Ji Bing Kong Zhi Za Zhi. 2017;21:835–51. doi: 10.16462/j.cnki.zhjbkz.2017.08.020. [DOI] [Google Scholar]
- 9.Hu XB, Bai YN, Pu HQ, et al Disease burden of liver cancer in Jinchang cohort. Zhonghua Liu Xing Bing Xue Za Zhi. 2016;37:321–24. doi: 10.3760/cma.j.issn.0254-6450.2016.03.005. [DOI] [PubMed] [Google Scholar]
- 10.Lu JJ, Xu AQ, Wang J, et al Direct economic burden of hepatitis B virus related diseases: evidence from Shandong, China. BMC Health Serv Res. 2013;13:37. doi: 10.1186/1472-6963-13-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Bureau of Statistics China. China Statistical Yearbook. Beijing: China Statistics Press, 2013.
- 12.Lang HC, Wu JC, Yen SH, et al The lifetime cost of hepatocellular carcinoma: a claims data analysis from a medical centre in Taiwan. Appl Health Econ Health Policy. 2008;6:55–65. doi: 10.2165/00148365-200806010-00005. [DOI] [PubMed] [Google Scholar]
- 13.Shi JF, Liu GX, Wang H, et al Medical expenditures for colorectal cancer diagnosis and treatment: A 10-year high-level-hospital-based multicenter retrospective survey in China, 2002-2011. Chin J Cancer Res. 2019;31:825–37. doi: 10.21147/j.issn.1000-9604.2019.05.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liao XZ, Shi JF, Liu JS, et al Medical and non-medical expenditure for breast cancer diagnosis and treatment in China: a multicenter cross-sectional study. Asia Pac J Clin Oncol. 2018;14:167–78. doi: 10.1111/ajco.12703. [DOI] [PubMed] [Google Scholar]
- 15.LV JJ, Li RP, Xu AQ, et al Economic burden and related factors on inpatients with HBV-related diseases in Shandong province. Zhonghua Liu Xing Bing Xue Za Zhi. 2013;34:267–72. doi: 10.3760/cma.j.issn.0254-6450.2013.03.015. [DOI] [PubMed] [Google Scholar]
- 16.Mao BH, Bai YN, Hu XB, et al Trends of economic burden on patients with four common cancers in rural area. Zhongguo Quan Ke Yi Xue. 2012;15:77–9. doi: 10.3969/j.issn.1007-9572.2012.01.026. [DOI] [Google Scholar]
- 17.Liang S, Zhang SX, Ma QS, et al Financial burden of hepatitis B-related diseases and factors influencing the costs in Shenzhen, China. Zhonghua Liu Xing Bing Xue Za Zhi. 2010;31:1340–5. doi: 10.3760/cma.j.issn.0254-6450.2010.12.004. [DOI] [PubMed] [Google Scholar]
- 18.Xu WY, Shi W, Chen P Analysis of economic burden of malignant tumor in-patients in Xinjiang. Ji Bing Jian Ce. 2006;21:38–40. doi: 10.3784/j.issn.1003-9961.2006.01.016. [DOI] [Google Scholar]
- 19.Hu M, Chen W Assessment of total economic burden of chronic hepatitis B (CHB)-related diseases in Beijing and Guangzhou, China. Value Health. 2009;12(Suppl 3):S89–92. doi: 10.1111/j.1524-4733.2009.00636.x. [DOI] [PubMed] [Google Scholar]