Abstract
Background
The psychological health of female sex workers (FSWs) has emerged as a major public health concern in many low- and middle-income countries (LMICs). Key risk factors include poverty, low education, violence, alcohol and drug use, human immunodeficiency virus (HIV), and stigma and discrimination. This systematic review and meta-analysis aimed to quantify the prevalence of mental health problems among FSWs in LMICs, and to examine associations with common risk factors.
Method and findings
The review protocol was registered with PROSPERO, number CRD42016049179. We searched 6 electronic databases for peer-reviewed, quantitative studies from inception to 26 April 2020. Study quality was assessed with the Centre for Evidence-Based Management (CEBM) Critical Appraisal Tool. Pooled prevalence estimates were calculated for depression, anxiety, post-traumatic stress disorder (PTSD), and suicidal behaviour. Meta-analyses examined associations between these disorders and violence, alcohol/drug use, condom use, and HIV/sexually transmitted infection (STI). A total of 1,046 studies were identified, and 68 papers reporting on 56 unique studies were eligible for inclusion. These were geographically diverse (26 countries), representing all LMIC regions, and included 24,940 participants. All studies were cross-sectional and used a range of measurement tools; none reported a mental health intervention. Of the 56 studies, 14 scored as strong quality, 34 scored as moderate, and 8 scored as weak. The average age of participants was 28.9 years (age range: 11–64 years), with just under half (46%) having up to primary education or less. The pooled prevalence rates for mental disorders among FSWs in LMICs were as follows: depression 41.8% (95% CI 35.8%–48.0%), anxiety 21.0% (95% CI: 4.8%–58.4%), PTSD 19.7% (95% CI 3.2%–64.6%), psychological distress 40.8% (95% CI 20.7%–64.4%), recent suicide ideation 22.8% (95% CI 13.2%–36.5%), and recent suicide attempt 6.3% (95% CI 3.4%–11.4%). Meta-analyses found significant associations between violence experience and depression, violence experience and recent suicidal behaviour, alcohol use and recent suicidal behaviour, illicit drug use and depression, depression and inconsistent condom use with clients, and depression and HIV infection. Key study limitations include a paucity of longitudinal studies (necessary to assess causality), non-random sampling of participants by many studies, and the use of different measurement tools and cut-off scores to measure mental health problems and other common risk factors.
Conclusions
In this study, we found that mental health problems are highly prevalent among FSWs in LMICs and are strongly associated with common risk factors. Study findings support the concept of overlapping vulnerabilities and highlight the urgent need for interventions designed to improve the mental health and well-being of FSWs.
Tara Beattie and co-workers assess the evidence on mental ill-health in female sex workers in low- and middle-income countries.
Author summary
Why was this study done?
Understanding the prevalence of mental health problems, and key risk factors associated with poor mental health, is essential for building evidence-based prevention.
To our knowledge, there has been no previous quantitative synthesis of the literature examining the prevalence of mental health problems among female sex workers (FSWs) in low- and middle-income countries (LMICs).
This evidence is critical to inform evidence-based policymaking and intervention design and is timely given the growing interest in mental health globally.
What did the researchers do and find?
We undertook a quantitative systematic review to estimate the prevalence of mental health problems and to estimate the magnitude of associations between mental health problems and sex workers’ experience of violence, harmful alcohol and drug use, condom use, and human immunodeficiency virus (HIV) and sexually transmitted infections (STIs).
Meta-analyses across 31 studies with 18,524 FSWs in 17 LMICs suggest that mental health problems—including depression, anxiety, post-traumatic stress disorder (PTSD), and suicidal thoughts and attempts—are highly prevalent among FSWs.
Sex workers with a mental health problem were more likely to have experienced violence, to report harmful alcohol or drug use, to report inconsistent condom use with clients (but not regular partners), and to be HIV positive compared with sex workers who did not have a mental health problem (18 studies with 14,115 FSWs).
What do these findings mean?
The quantitative evidence clearly demonstrates that mental health problems are an important burden of disease experienced by many FSWs in LMICs, with levels substantially greater than those experienced by women in the general population.
As no study described a mental health intervention, evidence-based mental health interventions for FSWs are urgently required to address the current treatment gap. The prevention and treatment of key risk factors such as violence and harmful alcohol and drug use would also help improve the mental health of FSWs.
Longitudinal research is needed in order to unpack pathways of causation. Future studies should use validated tools and consistent cut-offs and timeframes to enable more rigorous comparisons between studies.
Introduction
Mental health problems are a significant cause of the global burden of disease. In 2010, mental, neurological, and substance use disorders were the leading cause of years lived with disability globally [1]. Worldwide, an estimated 300 million people are affected by depression, and 272 million people by anxiety, with women at higher risk compared with men [2,3]. The treatment gap for common conditions exceeds more than 90% in low-income countries [4]. Left untreated, mental disorders prevent people from reaching their full potential, impair human capital, and are associated with premature mortality from suicide and other illnesses [5]. Suicide is a health outcome strongly associated with mental, neurological, and substance use disorders. Nearly 800,000 people are estimated to die due to suicide each year, with 79% of global suicides occurring in low- and middle-income countries (LMICs) [6]. A range of social determinants affect the risk and outcome of mental disorders. These include demographic factors (such as age, gender, and ethnicity), socioeconomic factors (such as low income, unemployment, and low education), neighbourhood factors (such as inadequate housing and neighbourhood violence), and social change associated with changes in income and urbanisation [1].
Sex work—defined by The Joint United Nations Programme on HIV/AIDS (UNAIDS) as the receipt of money or goods in exchange for sexual services, either regularly or occasionally [7]—is criminalised in most regions of the world [8]. In addition to the social determinants described earlier, women who sell sex face a unique set of structural factors including police harassment and arrests, discrimination, marginalization, poverty, and gender inequality [8,9], as well as extreme occupational hazards such as violence, coercion, deception, alcohol and substance use, and human immunodeficiency virus (HIV)/sexually transmitted infection (STI) [10]. Together, these predispose female sex workers (FSWs) to increased psychological health vulnerabilities. Structural and occupational risks associated with sex work are highly dependent on sociocultural and economic contexts, which means that these hazards may differ for sex workers in LMICs and those in high-income countries. Evidence from high-income countries indicates a high prevalence of mental health morbidity among FSWs, especially post-traumatic stress disorder (PTSD), depression, anxiety, and psychological distress [11–14]. Three previous reviews have examined mental health in the context of STIs/HIV, alcohol use, and violence against sex workers [15–17]. However, no attempt has been made to date to synthesise the evidence or estimate the burden of mental health disorders for FSWs. This is vital to inform policy and programming at the global and country level. The aim of this systematic review is to estimate the prevalence of mental disorders among FSWs in LMICs, and to examine associations with factors that commonly affect their health and well-being (violence, alcohol and drug use, condom use, HIV/STI).
Methods
Search strategy and selection criteria
The review protocol has been registered with PROSPERO, number CRD42016049179 (https://www.crd.york.ac.uk/prospero/). Ethics approval was not required for this study. This study follows the Preferred Reporting Items for Systematic reviews and Meta-Analysis (PRISMA) guidelines (Fig 1; S1 Prisma Checklist). We searched electronic peer-reviewed literature databases (Ovid, PubMed, Web of Science) from first record until 26 April 2020. Search terms included the following: “mental health” OR “mental well-being” OR “psycholog* health” OR “psycholog* distress” OR “mental illness*” OR “mental disorder*” OR “mental health problem*” OR “psychiatr* morbidit*” OR “anxiety” OR “depress*” OR “suicid*” OR “trauma” OR “post-traumatic stress disorder” OR “PTSD”; “sex work*” OR “female sex work*” OR “prostitut*” OR “female prostitut*” OR “sex trad*” OR “transact* sex” OR “FSW*” OR “commercial sex” OR “sex-trade worker*”; “low and middle income countr*” OR “LAMIC*” OR “LMIC*” OR “developing countr*” OR “names of all countries which fit the LMIC criteria.” See S1 Text for full database list and search strategy.
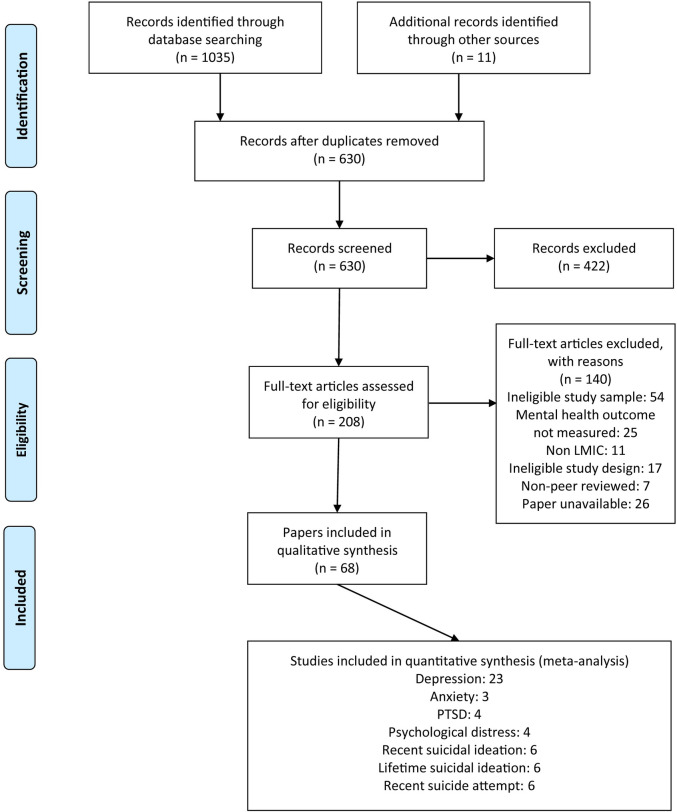
Fig 1. Flow chart of included quantitative studies.
LMIC, low- and middle-income country; PTSD, post-traumatic stress disorder.
Articles were included that measured the prevalence or incidence of mental health problems among FSWs, even if sex workers were not the main focus of the study. Only studies from countries defined as low or middle income, in accordance with the World Bank income groups 2019 [18], were included. Eligible studies had to be peer-reviewed, include females aged 16 or older who were actively engaged in sex work, and include the following study designs: cross-sectional survey, case–control study, cohort study, case series analysis, or experimental study with baseline measures for mental health. Studies were limited to English. We excluded studies that used qualitative methods only, were review papers, were conference abstracts, or were non–peer-reviewed publications. Studies exclusively focused on alcohol and substance use or victims of human trafficking sold into sex work were excluded from this review as reviews have recently been published in these areas [17,19–21]. Studies focused on women engaged in transactional sex only were ineligible for review, as this practice—and its implications on health—is distinct from sex work [22].
Data extraction and quality assessment
All publications were screened by 2 independent reviewers (TB and BS). If either author classed a publication as relevant, the abstract was reviewed, with any disagreements discussed and a consensus reached. If eligibility could not be determined by screening of the title and abstract, the authors reviewed the full text. Three authors (BS, TB, and AM) assessed full texts using the eligibility criteria cited earlier, with any discrepancies resolved through discussion. Data were extracted by 3 authors (TB, BS, and AM) into a structured data extraction sheet.
Study quality was assessed by authors (TB, BS, and AM) using the Centre for Evidence-Based Management (CEBM) Critical Appraisal for Cross-Sectional Surveys Tool (S2 Text). One item on CEBM was removed (Item 12: “Can the results be applied to your organisation?”) as it was not applicable to this review. To assess quality of studies, authors rated each article on 11 items, and an overall score was calculated, with higher scores indicating stronger quality. Studies scoring ≥7 out of 11 points were considered strong quality, between 5 and 7 were rated moderate quality, and ≤4 were scored as weak quality. Individual scores are presented in Table 1, and detailed scoring of each study is presented in S3 Text.
Table 1. Studies and mental health outcomes.
| Author and year | Country/income classification | Sample demographics | Sampling procedure | Outcome(s) of interest | Method of assessing outcome(s) | Events | Sample size | Prevalence (%) | Research quality |
|---|---|---|---|---|---|---|---|---|---|
| AFRICA | |||||||||
| Abelson (2019) | Cameroon, lower-middle income | FSWs Sex work location: Brothel, lodge, bar, other entertainment establishment: 100% Median age: 30.1 y (range: 23–36) Education: Primary/less: 30.9% Secondary/higher: 69.0% Martial status: Never married: 77.3% Currently married/in relationship: 10.7% Divorced/separated/ widowed: 12.0% |
Respondent driven sampling | Depression | PHQ-9 with cut-off > 5 |
1,067 | 2,165 | Any level depression: 49.8% | Strong (7) |
| Akinnawo (1995) | Nigeria, lower-middle income | FSWs Sex work location: Brothel, lodge, bar, other entertainment establishment: 100% Age: 30.5 y (range: not reported) Education: not reported Married status: Never married: 41.6% Currently married/in relationship: 44.0% Divorced/separated/ widowed: 14.4% |
Purposive | Affection/mood disorder | Awaritefe Psychological Index |
36 | 125 | 28.8% | Moderate (5) |
| Neuroticism | Eysenck Personality Inventory | 25 | 20.0% | ||||||
| Barnhart (2019) | Tanzania, low income |
Female bar workers Demographics not reported for FSWs |
Random sampling | Depression | PHQ-9 measuring moderate to severe using cut-off > 10 | 3 | 23 | 13.0% | Moderate (6) |
| PTSD | Primary care PTSD screening tool using cut-off >3 | 3 | 13.0% | ||||||
| Berger (2018) | Swaziland, lower-middle income | FSWs Sex work location: Brothel, lodge, bar, other entertainment establishment: 27.0% Street/public place: 8.7% Home: 57.8% Mean age: 26 y (range: 16–49) Education: Primary/less: 32.4%, Secondary/higher: 67.9% Martial status: Never married: 89.1%, Currently married/in relationship: 4.1% Divorced/separated/widowed: 6.9% |
Respondent driven sampling | Ever suicide ideation | “Have you ever felt like you wanted to end your life?” | 188 | 325 | 58.6% | Moderate (5) |
| Bitty-Anderson (2019)**, Tchankoni (2020)** | Togo, low income | FSWs Sex work location: Brothel, lodge, bar, other entertainment establishment: 100% Median age: 25 y, IQR 21–32 y Education: Primary/less: 44.9% Secondary/higher: 55.1% Marital status: Never married: 86.1% currently married/in relationship: 13.9% Divorced/separated/widowed: 0% |
Respondent driven sampling | Psychological distress | Kessler Psychological Distress Scale (K10) with cut-off scores: Mild: 20–24 Moderate: 25–29 Severe: >30 |
Mild: 223 Severe/moderate: 181 |
952 | Mild: 23.4% Severe/moderate: 19% |
Moderate (6) |
| Cange (2019) | Burkina Faso, low income | FSWs Sex work location: not reported Mean age: 26 y (range: 18–59) Education: Primary/less: 53.8% Secondary/higher: 0.7% Martial status: Never married: 53.6% Currently married/in relationship: 10.9% Divorced/separated/widowed: 35.5% |
Respondent driven sampling | Ever depression | “Ever felt sad or depressed for more than 2 weeks at a time” | 290 | 695 | 41.8% | Moderate (5) |
| Ever suicide ideation | Ever wanting to end their life at least once | 149 | 21.4% | ||||||
| Coetzee (2018) | South Africa, upper-middle income | FSWs Sex work location: not reported Median age: 31 y (IQR: 25–37) Education: Primary/less: 75.6% Secondary/higher: 12.4% Relationship status: not reported |
Respondent driven sampling | Depression | CES-D 20 using cut-off >21 | 349 | 508 | 68.7% | Strong (7) |
| PTSD | PTSD-8 using cut-off >9 | 201 | 39.6% | ||||||
| Suicide ideation in past month and year | “In the past month has the thought of ending your life been in your mind?” “Within the past year have you felt suicidal because you are a sex worker?” |
15 | 2.9% | ||||||
| Suicide attempt in past year | “In past year have you attempted suicide?” | 5 | 1% | ||||||
| Grosso (2019) | Togo and Burkina Faso, low income | FSWs and MSM Sex work location: not reported Median age: not reported Education: primary/higher: 57.0% Martial status: not reported |
Respondent driven sampling | Ever suicide ideation | “Have you ever had suicidal thoughts?” | 284 | 1,383 | 20.5% | Moderate (5) |
| Kim (2018) | Burkina Faso, low income | FSWs and MSM Sex work location: not reported Age (categories): <20: 10.2% 21–29: 37.8% >30: 52% Education: not reported Martial status: Never married: 44.5% Currently married/in relationship: 4.3% Divorced/separated/widowed: 34.0% |
Respondent driven sampling | Ever suicide ideation | “Have you ever felt like you wanted to end your life?” | 80 | 350 | 22.9% | Moderate (5) |
| Lion (2017) | South Africa, upper-middle income | FSWs who use methamphetamines Sex work location: not reported Age: 29 y (range not reported) Education: primary or lower not reported Martial status: not reported |
Respondent driven sampling | Depression | PHQ-9 using cut-off >10 | NA | 53 | NA | Moderate (6) |
| PTSD | PTSD Breslau’s 7 items using cut-off >4 | 21 | 38.7% | ||||||
|
MacLean (2018) |
Malawi, low income | FSWs Sex work location: Not reported Median age: 24 y (IQR: 22–28) Education: Primary/less: 17.0% Secondary/higher: 2.0% Martial status: Never married: 14.0% Currently married/in relationship: 4.0 Divorced/separated/widowed: 81.0% |
Purposive | Depression | PHQ-9 using cut-off >10 | 16 | 200 | 8% | Strong (7) |
| PTSD | PCL using cut-off >38 and >44 | 16 | 8% | ||||||
| Suicide ideation past 2 weeks | Used PHQ-9 item: “Have you had thoughts you would be better off dead” (passive ideation) and “of hurting yourself in some way” (active ideation) | 6 | 3% | ||||||
| Ortblad (2020) | Uganda, low income | FSWs Sex work location: Not reported Median age: 28 y (IQR: 24–32) Education: Primary/less: 55.7% Secondary/higher: 43.1% Marital status: Not reported |
Random sampling | Depression | PHQ-9 using cut-off > 10 | Uganda: 416 | 960 | 43.2% | Strong (10) |
| Suicide ideation past 2 weeks | Used PHQ-9 item: “Have you had thoughts you would be better off dead or of hurting yourself in some way” | 302 | 31.5% | ||||||
| Zambia, lower-middle income | Depression | Zambia: 441 | 965 | 45.7% | |||||
| Suicide ideation past 2 weeks | 540 | 56.7% | |||||||
| Peitzmier (2014)* Sherwood (2015)* |
The Gambia, low income | FSWs Sex work location: Not reported Mean age: 31 y (Range: 17–51) Education: Primary/less: 60.4% Secondary/higher: 39.6% Martial status: ever married: 23.0% Currently married/in relationship: 2.0% Divorced/separated/widowed: 69.8% |
Purposive | Depression | Sad or depressed mood for 2 or more weeks at a time in the past 3 years | 154 | 246 | 62.6% | Moderate (6) |
| Poliah (2017) | South Africa, upper-middle income |
FSWs Sex work location: Not reported Mean age: not reported Education: Primary/less: 65.2% Secondary/higher: 34.8% Martial status: Never married: 94.8% Currently married/in relationship: 2.6% Divorced/separated/widowed: 1.9% |
Purposive | Depression | PHQ-9 using cut-off score >5 | 121 | 150 | 80.9% | Moderate (5) |
| Depression and anxiety | SRQ-20 using cut-off score >7 | 120 | 78.4% | ||||||
| Rhead (2018) | Zimbabwe, lower-middle income | FSWs Sex work location: Not reported Age range: 19–58 y Education: Primary/less: 42.5% Secondary/higher: 57.5% Marital status: Never married: 4.6% Currently married/in relationship: 50.0% Divorced/separated /widowed: 44.8% |
Random sampling of venues followed by respondent driven sampling | Psychological distress | Shona Symptom Questionnaire Cut-off not reported |
43 | 174 | 24.7% | Moderate (6) |
| Roberts (2018) | Kenya, lower-middle income | HIV-negative FSWs Sex work location: Brothel, lodge, bar, other entertainment establishment: 88.0% Street/public place: 0% Home: 12.1% Median age: 33.5 y (IQR: 27.2–40.6) Education: 3.1 y (IQR: 1.2–9.8) Marital status: not reported |
Purposive | Depression | PHQ-9 using cut-off score >10 | 30 | 283 | 10.6% | Moderate (6) |
| PTSD | PCL-C using cut-off score >30 | 63 | 22.1% | ||||||
| EASTERN MEDITERRANEAN | |||||||||
| Lari (2014) | Iran, upper-middle income | FSWs with history of drug use who are engaged with harm reduction centres Sex work location: not reported Mean age: 32.5 y (range: 16–51) Education status: only reported for secondary: 39.2% Marital status: only reported for divorced: >50.0% |
Nonprobability sample | Psychological distress | Symptom Checklist-90 Cut-off not reported |
NA | 125 | NA | Weak (4) |
| Ranjbar (2019) | Iran, upper-middle income | FSWs Sex work location: not reported Age: 30.9 y (range: 18–45) Education and relationship status: not reported |
Purposive | Mental health disorders | GHQ-28 using cut-off score >23 | 30 | 48 | 62.5% | Weak (4) |
| Structured Clinical Interview for DSM-IV mood disorders | 16 | 53.5% | |||||||
| Structured Clinical Interview for DSM-IV anxiety disorders | 11 | 36.7% | |||||||
| EUROPE | |||||||||
| Lang (2011) | Armenia, lower-middle income | FSWs Sex work location: Street/public place: 100% Median age: 33.8 y (range: 20–52) Education and relationship status: not reported |
Purposive | Depressive symptoms | CES-D-8 item using cut-off >7 | 53 | 117 | 45% | Moderate (5) |
| SOUTH EAST ASIA | |||||||||
| Ghose (2015) | India, lower-middle income | HIV-positive FSWs attending an HIV clinic Sex work location: Brothel, lodge, bar, other entertainment establishment: 92% Street/public Place: 8% Mean age: 23 y Education and relationship status: not reported |
Purposive | Depression | Hospital Anxiety Depression Scheme Cut-off not reported |
30 | 100 | 30% | Moderate (5) |
| Anxiety | 44 | 44% | |||||||
| Hengartner (2015) | Bangladesh, lower-middle income | FSWs Sex work location: Brothel, lodge, bar, other entertainment establishment: 71.8% Home: 61.8% Mean age: 23.2 y (range 11–48) Education: Yes: 23.0%; No: 77.0% Marital status: Currently married/in relationship: 23.2% |
Response driven sampling | Major depressive disorder | WHO Mental Health Composite International Diagnostic Interview Cut-off not reported |
11 | 259 | 4.2% | Moderate (6) |
| Generalised anxiety disorder | 54 | 20.8% | |||||||
| PTSD | 8 | 3.1% | |||||||
| Iaisuklang (2017) | India, lower-middle income | FSWs enrolled in an HIV programme Sex work location: not reported Mean age: 29.5 y Educational status: Primary/less: 24.0% Secondary/higher: 45.0% Martial status: Never married: 9.0% Currently married/in relationship: 34.0% Divorced/separated/widowed: 57.0% |
Purposive | Major depressive disorder | MINI International Psychiatric Interview cut-off not reported | 9 | 100 | 9% | Weak (4) |
| Generalised anxiety disorder | 8 | 8% | |||||||
| PTSD | 21 | 21% | |||||||
| Pandiyan (2012) | India, lower-middle income | FSWs who use alcohol or drugs, attending psychiatric outpatient department Demographics not reported |
Purposive | Depression | GHQ items not specified Cut-off not reported Clinical interview to confirm diagnosis |
142 | 200 | 71% | Weak (3) |
| Anxiety | 84 | 42% | |||||||
| Patel (2016) | India, lower-middle income | FSWs Sex work location: Brothel, lodge, bar, other entertainment establishment: 27.6%, street/public place: 4.5%, Home: 13.9%, Mobile phones: 54% Mean age: 31.0 y Education: Yes: 43.8%, No: 56.2% Marital status: Never married: 5.0% Currently married/in relationship: 66.5% Divorced/separated/widowed: 28.5% |
Random sampling | Depression | PHQ-2 using cut-off >3 | 696 | 2,400 | 29% | Strong (9) |
| Patel (2015) | India, lower-middle income | FSWs Sex work location: Brothel, lodge, bar, other entertainment establishment: 7.7% Street/public place: 63.8%, Home: 28.5% Age, education, and relationship status: not reported |
Random sampling | Depression | PHQ-2 using cut-off >3 | 778 | 1,986 | 39.2% | Strong (9) |
| Shahmanesh (2009) | India, lower-middle income | FSWs Sex work location: Brothel, lodge, bar, other entertainment establishment: 57.6% Street/public place: 22.8% Home: 28.1% Mean age: not reported Education: Yes: 32.7%, No: 67.3% Martial status: Never married: 28.4% Currently married/in relationship: 31.3% Divorced/separated/widowed: 40.3% |
Respondent driven sampling | Depression and anxiety | Kessler-10 Cut-off not reported |
NA | 326 | NA | Strong (7) |
| Suicide ideation past 3 months | Suicide items not described | 114 | 34.9% | ||||||
| Suicide attempts past 3 months | 61 | 18.7% | |||||||
| Suresh (2009) | India, lower-middle income | FSWs Sex work location: Street/public place: 100% Mean age: 34 y (range: 20–27) Educational: Secondary: 51% Marital status: not reported |
Purposive | Depression | CES-D cut-off not reported | 49 | 57 | 86% | Weak (4) |
| PTSD | PCL-C using cut-off >45 | 31 | 56% | ||||||
| Ever suicide ideation | Ever having thoughts of suicide at the level of forming a plan | 17 | 30% | ||||||
| WESTERN PACIFIC | |||||||||
| Brody (2016) | Cambodia, low income | Female entertainment workers Sex work location: Brothel, lodge, bar, other entertainment establishment: 100.0% Mean age: 25.6 y Education: Formal education: 6.4 y (mean) Marital status: Never married: 44.1% Currently married/in relationship: 28.6% Divorced/separated/widowed: 27.2% |
Two-stage cluster sampling method | Psychological distress | GHQ-12: mean score for whole sample used as cut-off | 284 | 657 | 43.2% | Strong (8) |
| Suicide ideation past 3 months | Suicide items not described | 128 | 19.5% | ||||||
| Suicide attempts past 3 months | 48 | 7.3% | |||||||
| Carlson (2017) | Mongolia, lower-middle income | FSWs with harmful level of alcohol use Demographics not reported |
Purposive | Depression | BSI depression subscales using cut-off >63 | 134 | 222 | 60.4% | Moderate (5) |
| Chen (2017) | China, upper-middle income | FSWs working in commercial sex venues Sex work location: Brothel, lodge, bar, other entertainment establishment: 100% Mean age: 25.2 y (range: 18–42) Education: Secondary/less: 7.4% Secondary/higher: 25.5% Marital status: Never married: 30.2% Currently married/in relationship: 63.2% Divorced/separated/widowed: 6.0% |
Random sampling venues and purposive selection of FSWs | Depression | CES-D 20 using cut-off score >16 | 189 | 457 | 41.3% | Moderate (5) |
| Gu (2010a) | China, upper-middle income | FSWs who inject drugs Sex work location: Brothel, lodge, bar, other entertainment establishment: 100% Mean age: not reported Education: Secondary/below: 75.5% Secondary/higher: 24.5% Marital status not reported |
Snowball sampling | Depression | Depression subscale of Chinese Depression Anxiety Stress Scale Cut-off not reported |
NA | 234 | NA | Moderate (6) |
| Hopelessness | Chinese Hopelessness Scale Cut-off not reported |
NA | NA | ||||||
| Gu (2010b) | China, upper-middle income | FSWs who inject drugs Sex work location: not reported Mean age: 28.1 y Education: Primary/less: 17.6% Secondary/higher: 82.4% Marital status: Never married: 53.7% Currently married/in relationship: 19.0% Divorced/separated/widowed: 26.4% |
Convenience | Psychological Distress | "You hate yourself very much" | 155 | 216 | 71.8% | Moderate (5) |
| "You feel very depressed" | 167 | 77.3% | |||||||
| "You are suffering from severe insomnia" | 142 | 65.7% | |||||||
| Gu (2014) | China, upper-middle income | FSWs who inject drugs Sex work location: Brothel, lodge, bar, other entertainment establishment: 100% Mean age: 33.9 y Education: Primary/less: 13.6% Secondary/higher: 86.4% Marital status: Never married: 36.0% Currently married/in relationship: 46.5% Divorced/separated/widowed: 17.5% |
Snowball sampling | Depression | Depression subscale of Chinese Depression Anxiety Stress Scale using cut-off >21 | 78 | 200 | 39.0% | Moderate (6) |
| Suicide ideation past 6 months | "Have you thought of committing suicide in the past 6 months?" | 89 | 44.7% | ||||||
| Suicide attempt past 6 months | “Have you attempted to commit suicide in the past 6 months?” | 54 | 26.8% | ||||||
| Hong (2010) | China, upper-middle income | FSWs Sex work location: Brothel, lodge, bar, other entertainment establishment: 100% Median age: 22.5 y (range: 16–42) Education: <6 y: 33.6%, 7–9 y: 48.1% >9 y: 29.6% Marital status: Not married: 85.5%, Currently married/in relationship: 14.5% |
Purposive | Depression | CESD-10 using cut-off score of >16 | 94 | 310 | 30.3% | Moderate (6) |
| Suicide ideation past 6 months | “In the past 6 months, have you thought of committing suicide?” | 55 | 17.8% | ||||||
| Suicide attempt past 6 months | “In the past 6 months, have you attempted to commit suicide?” | 28 | 9.0% | ||||||
| Hong (2007a)***, Fang (2007)***, Wang (2007)*** | China, upper-middle income | FSWs Sex work location: Brothel, lodge, bar, other entertainment establishment: 100.0% Mean age: 23.5 y Education (y): 5.8 y Marital status: Never married: 60.0% Currently married/in relationship: 35.2% Divorced/separated/widowed: 4.9% |
Random sampling venues and purposive selection of FWSs | Suicide ideation past 6 months | “In the past 6 months, have you thought of committing suicide?” | 40 | 454 | 14.2% | Strong (7) |
| Suicide attempt past 6 months | “In the past 6 months, have you attempted to commit suicide?” | 23 | 8.4% | ||||||
| Hong (2007b) | China, upper-middle income | FSWs Sex work location: Street/public place: 100% Mean age: 23.5 y Education (y): 5.84 y (mean) Martial status: Never married: 57.5% Currently married/in relationship: 35.2% Divorced/separated/widowed: 6.9% |
Purposive | Depression | CES-D 10 using cut-off score ≥16 | 174 | 278 | 62.6% | Moderate (6) |
| Hong (2013)†, Su (2014)†, Zhang (2014a)†, Zhang (2014b)†, Zhang (2017)† | China, upper-middle income | FSWs Sex work location: Brothel, lodge, bar, other entertainment establishment: 91.2%, Mini hotels and streets: 8.7% Mean Age: 24.8 y Education status: Primary/less: 63.4% Secondary/higher: 36.6% Marital status: Never in relationship: 71.5% Ever in relationship: 28.5% |
Random sampling venues and purposive selection of FSWs | Depression | CES-D 10 using cut-off score ≥16 | 502 | 1,022 | 49.1% | Strong (8) |
| Severe suicide ideation or suicide attempt | Ever “seriously considered killing yourself” or ever “tried to kill yourself” | 97 | 9.5% | ||||||
| Ever suicide ideation | Ever “seriously considered killing yourself | 83 | 8.0% | ||||||
| Ever suicide attempt | Ever “tried to kill yourself” | 49 | 4.8% | ||||||
|
Huang (2014)§, Zaller (2014)§, Yang (2018)§ |
China, upper-middle income | FSWs Sex work location: Brothel, lodge, bar, other entertainment establishment: 100.0% Median age: 23.5 y (IQR 20.9–26.4 y) Education: Secondary/less: 56.7% Secondary/higher: 43.5% Marital status: Currently married/in relationship: 44.5%, Single/divorced/widowed: 54.4% |
Random sampling venues and purposive selection of FSWs | Depression | CES-D using cut-off >20 | 34 | 154 | 22.1% | Strong (7) |
| Anxiety | Social anxiety scale using cut-off >60 | 6 | 3.9% | ||||||
| Suicide ideation past year | Suicide ideation item not described | 15 | 9.7% | ||||||
| Suicide attempt past year | Suicide attempt item not described (authors noted having plan as indicating an attempt) | 9 | 5.8% | ||||||
| Suicidal behaviour past year | Suicide behavior not described | 8 | 5.2% | ||||||
| Jackson (2013) | China, upper-middle income | FSWs Sex work location: Brothel, lodge, bar, other entertainment establishment and street/public place: 100% Mean age: 26.7 y Education: Primary/less: 13.9% Secondary/higher: 86.9% Marital status: Currently married/in relationship: 64.4% |
Purposive | Depression | CES-D cut-off not reported | NA | 395 | NA | Weak (4) |
| Muth (2017) | Cambodia, lower-middle income | HIV positive FSWs Sex work location: Brothel, lodge, bar, other entertainment establishment: 100.0% Median age: 32 y (IQR: 28–35) Education: Primary/less: 85.0% Secondary/higher: 15.0% Martial status: not reported |
Purposive | Psychological distress | Kessler-10 cut-off not reported | 27 | 88 | 31% | Moderate (6) |
| Offringa (2017) | Mongolia, lower-middle income | FSWs Sex work location: Brothel, lodge, bar, other entertainment establishment and street/public place: 100% Mean age: 35.2 y Education: Primary/less: 7.8% Secondary/higher: 92.2% Martial status: Divorced/separated/widowed: 52.3% |
Random sampling | Depression | BSI depression subscale Cut-off not reported |
NA | 204 | NA | Strong (7) |
| Sagtani (2013) | Nepal, low income | FSWs Demographics not reported |
Snowball sampling | Depression | CES-D 20 using cut-off >16 | 173 | 210 | 82.4% | Strong (8) |
| Shen (2016) | China, upper-middle income | FSWs working in commercial sex venues Sex work location: Brothel, lodge, bar, other entertainment establishment and street/public place: 100% Mean age: not reported Education: Primary/less: 23.4% Secondary/higher: 76.5% Marital status: Not married: 42.3% Currently married: 43.6% |
Convenience sampling | Depression | GHQ-12 Chinese version using sample mean score as cut-off | 342 | 653 | 52.4% | Moderate (6) |
| Shrestha (2017) | Nepal, low income | FSWs (and MSM/trans) Sex work location: Brothel, lodge, bar, other entertainment establishment and street/public place: 100% Mean age: not reported Education by literacy status: Yes: 67.8% No: 32.1% Marital status: Currently married/in relationship: 59.0% |
Random sampling | Depression | CES-D using cut-off >22 | 112 | 610 | 18.3% | Strong (7) |
| Ever suicide ideation | Suicide item not described | 210 | 4.4% | ||||||
| Urada (2013) | Philippines, lower-middle income | FSWs Sex work location: Brothel, lodge, bar, other entertainment establishment: 100.0% Median age: 22 y (IQR: 20–25) Education: 10 y (IQR 9–10) Martial status: Currently married/in relationship: 29.0% Living alone/separated/widowed: 71% |
Purposive | Depression | CES-D 24 using cut-off >23 | 83 | 143 | 58% | Moderate (6) |
| Witte (2010) | Mongolia, lower-middle income | FSWs who had recent unprotected sex with client, enrolled in National AIDs Foundation Program Sex work location: not reported Mean age: 28 y (range 18–40) Education: Secondary/higher: 100% Marital status: Never married: 67.0% |
Purposive | Depression | BSI-depression subscale Cut-off score not reported |
19 | 48 | 38% | Weak (4) |
| Yang (2005) |
China, upper-middle income | Female migrants engaged in sex work Sex work location: Brothel, lodge, bar, other entertainment establishments: 100.0% Mean age: 23.9 y (mean) Education: Secondary/less: 92.3% Marital status: Never married: 76.9% |
Random sampling of venues and convenience sample of FSWs | Depression | CES-D 20 using cut-off >16 | 20 | 40 | 50% | Moderate (6) |
| AMERICAS | |||||||||
| Devóglio (2017) | Brazil, upper-middle income | FSWs Sex work location: not reported Mean age: 26.8 y Education: Secondary/less: 30.1% Higher than secondary: 92.6% Relationship status: Never married: 94.0% Currently married/in relationship: 6.0% Divorced/separated/widowed: 4.8% |
Purposive | Depression | Hospital Anxiety and Depression scale Cut-off not reported |
11 | 83 | 13.2% | Moderate (5) |
| Anxiety | 33 | 39.7% | |||||||
| González-Forteza (2014) | Mexico, upper-middle income | FSWs Sex work location: Brothel, lodge, bar, other entertainment establishment: 48% Street/public place: 16% Median age: 28.8 y Education: Primary/less: 31.4% Secondary/higher: 60.8% Marital status: Never married: 49.0% Currently married/in relationship: 28.0% Divorced/separated/widowed: 22.3% |
Purposive | Depression | MINI International Psychiatric Interview, including suicide risk | 41 | 103 | 39.8% | Weak (3) |
| Ever suicide risk | MINI International Psychiatric Interview, including suicide risk: “Do you ever feel like life is not worth living?” “Have you ever thought about killing yourself. If so, how would you do it?” | 40 | 38.8% | ||||||
| Jain (2019) | Mexico, upper-middle income | FSWs Sex work location: not reported Median age: 38 y (IQR: 20–46) Education: Secondary: 44.1% Marital status: not reported |
Purposive | Depression | Beck Depression Inventory using cut-off score >20 | 106 | 295 | 35.9% | Moderate (5) |
| Logie (2018) | Jamaica, upper-middle income | FSWs who are lesbian and bisexual women Sex work location: not reported Mean age: 27.2 y (range: 19–43) Education: not reported Marital status: Never married: 8.9% Currently married/in relationship: 71.1% |
Purposive | Depression | PHQ-2 using cut-off >3 | 42 | 45 | 93.33% | Moderate (6) |
| Rael (2017a)‡, Rael (2017b)‡ | Dominican Republic, upper-middle income | HIV-negative FSWs with dependent children Sex work location: Brothel, lodge, bar, other entertainment establishment: 70.1% Mean age: 27.5 y Education: 8.4 y (mean) Marital status: Currently married/in relationship: 32.4% |
Purposive sample | Depression | CES-D 10 using cut-off >10 | 245 | 349 | 70.20% | Moderate (6) |
| Semple (2019) | Mexico, upper-middle income | FSWs in street-based work and establishment-based indoor sex work Sex work location: Brothel, lodge, bar, other entertainment establishment: 39.0% Street/public place: 61.0% Mean age: 33.6 y (range: 18–56) Education: Primary/less: 41.8%, secondary/higher: 59.1% Marital status: Never married: 56.0% Currently married/in relationship: 28.8% Divorced/separated/widowed: 14.7% |
Time-location sampling | Depression | Beck Depression Inventory using cut-off score >20 | 155 | 426 | 36.4% | Moderate (6) |
| Ulibarri (2009)Ꝁ, Ulibarri (2014)Ꝁ | Mexico, upper-middle income | HIV-negative FSWs Sex work location: Brothel, lodge, bar, other entertainment establishment: 41.2% Street/public place: 54.8%, Other: 3.2% Mean age: 33.4 y (range 18–64) Education: 6.13 y (mean) Marital status: Never married: 46.0% Currently married/in relationship: 33.0% Divorced/separated/widowed: 26.0% |
Purposive | Psychological distress (depression and somatization) | Brief Symptom Inventory Subscales: depression and somatization (cut-off not reported) |
NA | 916 | NA | Moderate (5) |
| Ulibarri (2013) | Mexico, upper-middle income | FSWs who inject drugs Sex work location: not reported Mean age: 33.7 y Educational status: 7.1 y (mean) Martial status: Never married: 49.0% Currently married/in relationship: 38.0% Divorced/separated/widowed: 13.3% |
Purposive | Depression | CES-D 10 using cut-off >10 | 538 | 624 | 86.2% | Moderate (6) |
| Ulibarri (2015) | Mexico, upper-middle income | FSWs who use drugs and have a regular partner Sex work location: not reported Mean age: 37.3 y (mean) Education: 6.7 y (mean) Marital status: Currently married/in relationship: 98.0% |
Snowball sampling | Depression | CES-D 10 cut-off not reported | NA | 214 | NA | Moderate (5) |
*Papers report findings on same study but explore different associations with outcome of interest.
**Papers report findings on same study but explore different associations with outcome of interest.
***Papers report findings on same study but explore different associations with outcome of interest.
†Papers report findings on same study but explore different associations with outcome of interest.
§Papers report findings on same study but explore different associations with outcome of interest.
‡Papers report findings on same study but explore different associations with outcome of interest.
ꝀPapers report findings on same study but explore different associations with outcome of interest.
Abbreviations: BSI, Brief Symptom Inventory; CES-D, Centre for Epidemiological Studies Depression Scale; DSM-IV, Diagnostic and Statistical Manual of Mental Disorders, 4th edition; FSW, female sex worker; GHQ, General Health Questionnaire; HIV, human immunodeficiency virus; IQR, interquartile range; MINI, Mini-International Neuropsychiatric Interview; MSM, men who have sex with men; NA, not applicable; PCL, PTSD CheckList; PCL-C, PTSD CheckList – Civilian Version; PHQ, Patient Health Questionnaire; PTSD, post-traumatic stress disorder; SRQ, WHO Self-Reporting Questionnaire.
Data analysis
A narrative synthesis was conducted across all studies meeting inclusion criteria. Prevalence estimates were calculated from percentages or raw proportions, and we contacted authors of studies in which raw data were missing. If multiple publications reported results from a single study, we included all studies in Table 1 but only the original study in the narrative synthesis and prevalence analyses. Meta-analyses were conducted on studies that scored moderate to strong in the quality assessment and that used validated measures to assess mental health outcomes; we excluded studies from the meta-analyses that sampled participants based on characteristics that are known to be an independent risk factor for mental health problems (such as injecting drug use or HIV status) and could therefore bias the pooled mental health estimates. Analyses were completed using Comprehensive Meta-Analysis (CMA) software version 3 (Biostat, Englewood, NJ). Pooled estimates were calculated using a random effects model. Variation between studies was determined by heterogeneity tests with the Higgins’ I2 statistic. Relative weights were calculated using the formula 1/V + T2 where V is the error variance and T2 (Tau-squared) is the between-study variance. Subgroup analyses were completed to examine associations between mental health outcomes (e.g., depression) and the following covariates: violence/police arrest, alcohol/drug use, condom use, and HIV/STI. Due to variations between studies in the factors adjusted for in multivariate analyses, unadjusted odds ratios (ORs) were extracted or calculated from raw data. Pooled effect estimates were calculated using a random-effects model.
Results
Study characteristics
The initial electronic search yielded 1,035 results, with 11 more studies identified through reference list screening and online searches. After duplicate records were removed, the titles and abstracts of 630 publications were screened for eligibility. Of those, 208 were identified as potentially relevant publications and reviewed for inclusion. Sixty-eight papers reporting on 56 unique studies with 24,940 participants meeting the inclusion criteria (Fig 1). Eight of these studies did not provide prevalence data on mental health [23–31]; authors of these studies were contacted twice for further information, and 2 authors responded, providing prevalence data [23,27]. In total, 86 prevalence estimates from 48 studies were available (depression n = 37; anxiety n = 7; PTSD n = 8; suicide attempt n = 8; suicide ideation n = 17; psychological distress n = 7; mood disorders n = 2) (Table 1).
Studies were based in 26 LMICs: 13 countries in sub-Saharan Africa, 1 in the Middle East and north Africa region, 1 in Eastern Europe, 2 in South East Asia, 5 in the Western Pacific region, and 4 in Latin America and the Caribbean. Eleven studies reported findings from countries in the low-income group, 20 studies from the low-middle income group, and 26 studies from the upper-middle income group, as per the World Bank income classification. Twenty-nine studies used a purposive sample, 14 used respondent driven sampling techniques, 7 used a random sample, and 6 utilized random sampling techniques to select venues and purposive methodology to recruit FSWs within these venues (Table 1). Most studies recruited FSWs from a variety of venues, such as streets, bars, brothels, and entertainment establishments, with 3 studies selecting women from clinics or hospital settings [26,32,33]. All studies were cross-sectional, with 3 studies including qualitative data alongside survey results [34–36]. Of the 56 studies, 14 scored as strong quality, 34 scored as moderate, and 8 scored as weak (S3 Text). Sixteen studies (14 moderate; 2 weak) selected participants based on harmful alcohol or drug use (n = 9) [24,26,31,33,34,37–40], or positive [32,41] or negative [29,42–45] HIV status (n = 5), and were excluded from the meta-analyses (regardless of CEBM score) to avoid biasing the pooled estimates. Analyses used a variety of validated scales and cut-off points to assess mental disorders (Table 1). None reported a mental health intervention.
The mean age of FSWs in the 42 studies that reported this was 28.9 years (age range: 11–64 years). Thirty-two studies reported sex work locations for their sample; among these studies, 66.3% of FSWs worked in brothels, lodges, bars, or other entertainment establishments; 51.7% worked in streets or public places; 24.7% worked at home; and 36.7% worked in other settings, e.g., via mobile phones (these categories were not mutually exclusive). Thirty-one studies reported education levels of their sample, and among these, nearly one-half of FSWs (45.7%) had an education level of primary school or less. Among the 40 studies that reported marital status for their sample, 48% of FSWs were never married; 32.9% were currently married or in a relationship; and 24.5% were divorced, separated, or widowed.
Mental disorders and suicidal behaviour
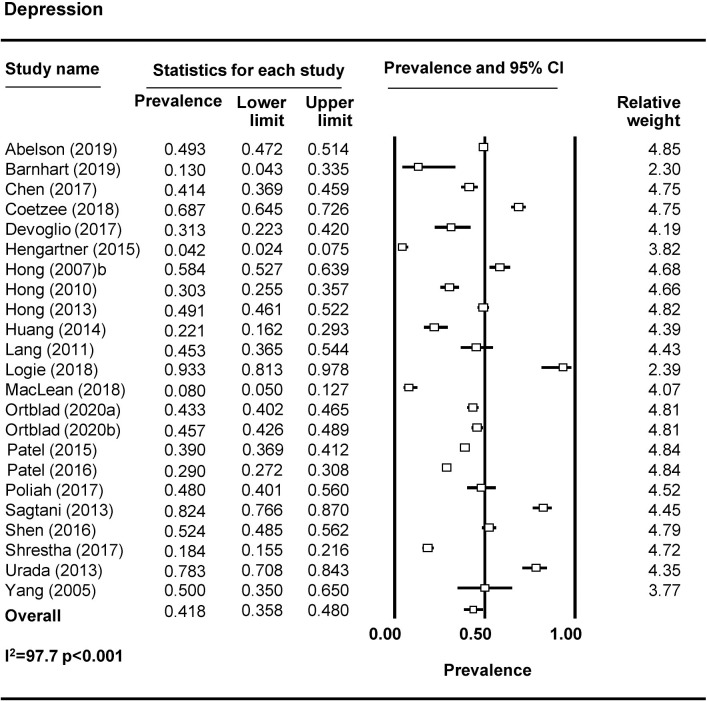
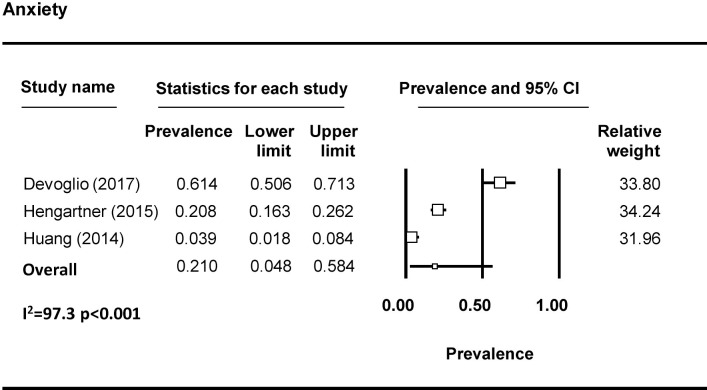
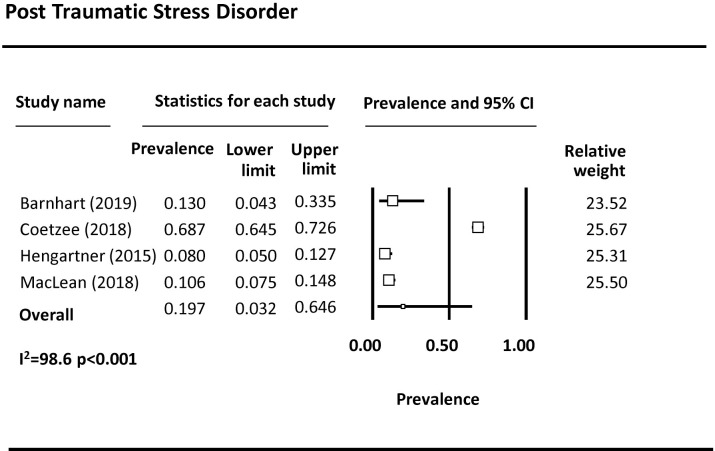
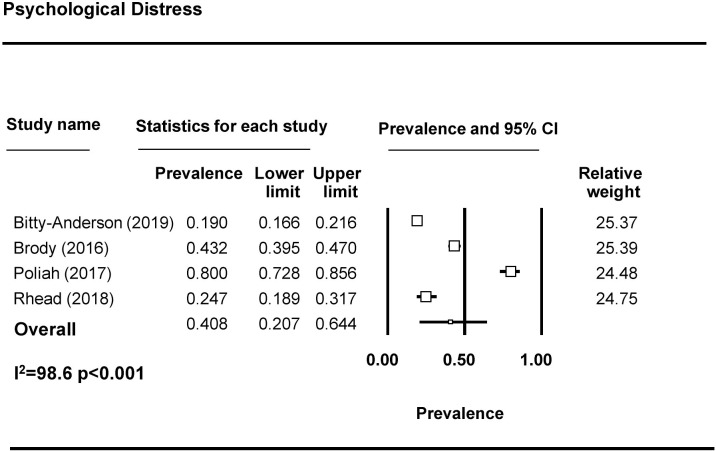
Forty-four studies examined depression among FSWs, with 37 reporting prevalence estimates (Table 1) [9,10,23,27,32–37,39,43–69]. A meta-analysis was conducted with 23 studies (Fig 2). The pooled prevalence of depression among FSWs from LMICs is 41.8% (95% CI 35.8%–48.0%). Seven studies reported on the prevalence of anxiety among FSWs [9,32,33,50,58,64,70], with 3 included in the meta-analysis (Fig 3). The pooled prevalence of anxiety among FSWs from LMICs is 21.0% (95% CI 4.8%–58.4%). PTSD symptomology was reported in 8 studies [9,10,23,40,43,46,47,50] with 4 studies included in the meta-analysis (Fig 4). The pooled prevalence of PTSD symptoms among FSWs from LMICs is 19.7% (95% CI 3.2%–64.6%). Ten studies measured psychological distress among FSWs, with 7 studies providing prevalence estimates [38,41,49,70–73] and 4 studies included in the meta-analysis (Fig 5). The pooled prevalence of psychological distress experienced by FSWs from LMICs was 40.8% (95% CI 20.7%–64.4%). Two studies examined mood disorders [70,74]. Only one study [74] was eligible for inclusion in a meta analysis and thus a pooled prevalence estimate is not available. This study reported a prevalence of affection/mood disorder of 28.8% (95% CI 21.5%–37.3%).
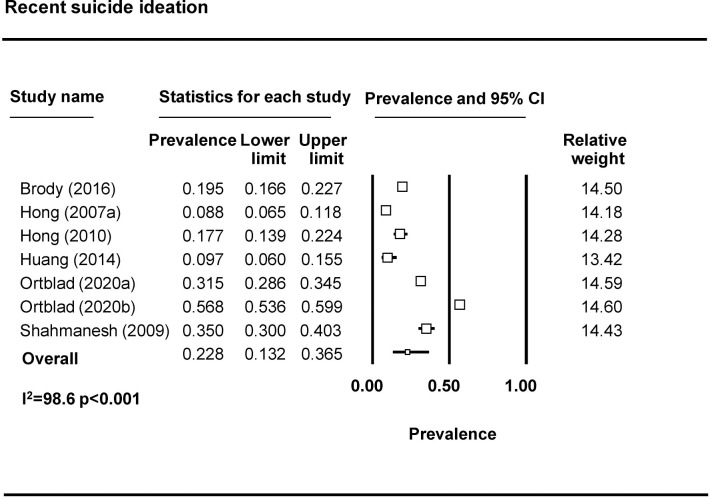
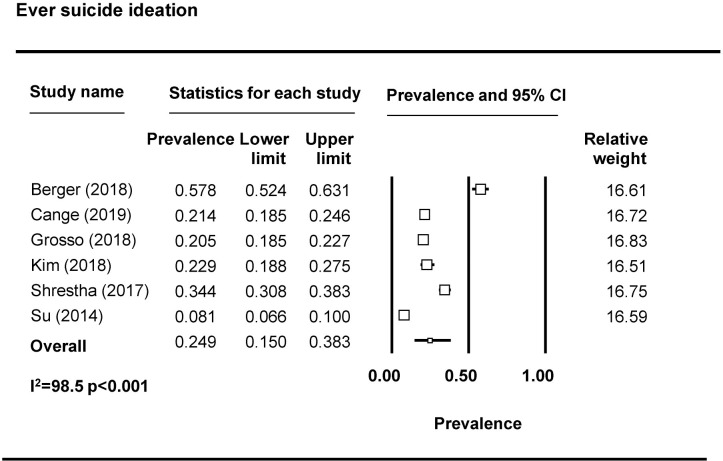
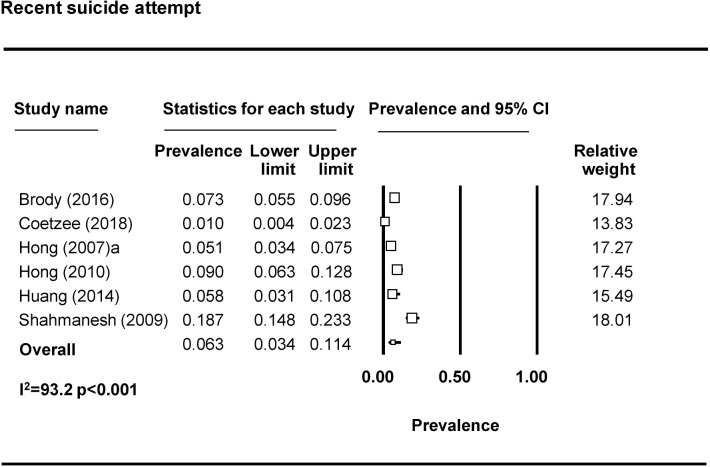
Fig 2. Depression pooled prevalence estimates.
Fig 3. Anxiety pooled prevalence estimates.
Fig 4. PTSD pooled prevalence estimates.
PTSD, post-traumatic stress disorder.
Fig 5. Psychological distress pooled prevalence estimates.
Seventeen studies reported on suicidal ideation [10,36,39,46,47,55,57,58,61,69,71,75–80]. Most assessed suicidal ideation by asking about suicidal thoughts, for example, “have you thought about killing yourself?” and “have you ever felt like you wanted to end your life?” For the meta-analysis, we divided studies based on timeframe into ‘recent’ or ‘ever’ suicidal ideation and removed 3 studies due to limitations in how questions were operationalized [46,47], including one study that combined suicidal thoughts with attempting suicide [65]. The pooled prevalence of recent (past 3 months, 6 months, or year) suicide ideation is 22.8% (95% CI 13.2%–36.5%) (n = 6 studies from 7 countries) (Fig 6). The pooled prevalence of lifetime suicidal ideation is 24.9% (95% CI 15.0%–38.3%) (n = 6 studies) (Fig 7). Eight studies reported on suicide attempts among FSWs [39,46,55,57,58,71,79,80]. The majority assessed suicide attempts through one binary question (yes/no) asking whether the participant had attempted suicide. Prevalence of recent suicide attempt (past 3 months, 6 months, or year) was reported by 6 studies included in the meta-analysis (Fig 8). The pooled prevalence of recent suicide attempts among FSWs from LMICs is 6.3% (95% CI 3.4–11.4%). Only one study reporting on ever suicide attempt was eligible for inclusion in a meta analyses and thus a pooled prevalence estimate is not available. This study reported a prevalence of lifetime suicide attempt of 4.8% (95% CI 3.6%–6.3%) [81].
Fig 6. Recent suicide ideation pooled prevalence estimates.
Fig 7. Ever suicide ideation pooled prevalence estimates.
Fig 8. Recent suicide attempt pooled prevalence estimates.
Associations between mental health and other factors
We conducted subgroup analyses to examine associations between mental health (e.g., depression) and factors commonly experienced by FSWs (violence/police arrest, alcohol/drug use, condom use, and HIV/STI) (Table 2). Findings of the meta-analyses are summarised in Table 3 and displayed in forest plots in S1–S4 Figs.
Table 2. Studies on mental health and outcomes of interest.
| Author and study | Country | Sample | Mental health measure | Outcome(s) of interest | Sample size | Odds in the exposed1 | Odds in the unexposed2 | Crude OR (95% CI) | P value |
|---|---|---|---|---|---|---|---|---|---|
| VIOLENCE | |||||||||
| Berger (2018) | Swaziland | FSWs | Suicide ideation ever | Physical violence (as a result of selling sex) or sexual violence ever | 325 | 124/65 | 67/68 | 1.9 (1.2–3.0) | 0.006 |
| Cange (2019) | Burkina Faso | FSWs | Suicide ideation ever | Physical violence ever | 696 | 106/43 | 318/220 | 1.7 (1.2–2.5) | 0.008 |
| Sexual violence ever | 91/58 | 193/353 | 2.9 (2.0–4.2) | <0.001 | |||||
| Carlson (2017) | Mongolia | FSWs with harmful level of alcohol use | Depression (BSI) | Physical violence ever by client | 222 | 114/20 | 67/21 | 1.8 (0.9–3.5) | 0.09 |
| Sexual violence ever by client | 79/55 | 24/64 | 3.8 (2.1–6.9) | <0.001 | |||||
| Coetzee (2018) | South Africa | FSWs | Depression (CES-D) | Physical or sexual violence past year | 508 | 295/41 | 142/28 | 1.4 (0.8–2.4) | 0.2 |
| PTSD (PTSD-8) | 244/31 | 195/38 | 1.5 (0.9–2.6) | 0.13 | |||||
| Gu (2014) | China | FSWs who inject drugs | Depression (Chinese Depression Anxiety Stress Scale) | Verbal, physical violence or threats past 6 months by clients or gatekeepers | 200 | 25/53 | 25/97 | 1.83 (1.0–3.5) | 0.06 |
| Suicide ideation past 6 months | 33/56 | 16/94 | 3.4 (1.6–7.0) | 0.001 | |||||
| Suicide attempt past 6 months | 22/30 | 26/116 | 3.2 (1.3–7.6) | 0.01 | |||||
| Hong (2007b) |
China | FSWs | Depression (CES-D) | Sexual violence past 6 months | 278 | 17/157 | 3/101 | 1.5 (0.4–5.9) | 0.6 |
| Suicide ideation past 6 months | 18/47 | 52/337 | 2.5 (1.3–4.6) | 0.004 | |||||
| Suicide attempt past 6 months | 14/24 | 60/356 | 3.5 (1.7–7.1) | 0.001 | |||||
| Hong (2013)* Zhang (2017)* |
China | FSWs | Depression (CES-D) | Sexual, physical, or emotional violence ever by client | 1,022 | 252/170 | 244/271 | 1.6 (1.3–2.1) | <0.001 |
| Sexual, physical, or emotional violence ever by intimate partner | 241/189 | 124/189 | 1.9 (1.4–2.6) | <0.001 | |||||
| Suicide ideation or attempt ever | Sexual, physical, or emotional violence ever by client | 55/367 | 37/478 | 1.9 (1.2–3.0) | 0.006 | ||||
| Sexual, physical, or emotional violence ever by intimate partner | 52/378 | 15/298 | 2.7 (1.5–5.0) | 0.001 | |||||
| Depression (CES-D) | Sexual, physical, or emotional violence ever by intimate partner or non-partner | 358/163 | 279/222 | 1.7 (1.4–2.3) | <0.001 | ||||
| Suicide ideation or attempt ever | Sexual, physical, or emotional violence ever by intimate partner or non-partner | 79/18 | 558/367 | 2.9 (1.7–4.9) | <0.001 | ||||
| Jain (2020) | Mexico | FSWs | Depression (PHQ-9) | Physical violence ever by client | 295 | 50/56 | 57/132 | 2.1 (1.3–3.4) | 0.002 |
| Patel (2015) | India | FSWs | Depression (PHQ-2) | Physical violence past 6 months | 1,986 | 158/620 | 189/1020 | 1.4 (1.1–1.7) | 0.008 |
| Police arrest ever | 165/613 | 133/1075 | 2.2 (1.7–2.8) | <0.001 | |||||
| Patel (2016) | India | FSWs | Depression (PHQ-2) | Physical or sexual violence past year | 2,400 | 285/418 | 291/1407 | 3.3 (2.7–4.0) | <0.001 |
| Poliah (2017) | South Africa | FSWs | Depression (PHQ-9) | Violence ever during sex work | 150 | 93/27 | 17/11 | 2.2 (0.9–5.3) | 0.08 |
| Police harassment ever | 85/38 | 19/8 | 0.9 (0.4–2.3) | 0.9 | |||||
| Roberts (2018) | Kenya | HIV-negative FSWs | Depression (PHQ-9) | Sexual, physical, moderate emotional violence ever by intimate partner or non-partner | 283 | 26/4 | 197/56 | 1.8 (0.6–5.5) | 0.3 |
| PTSD (PCL-C) | 41/5 | 182/55 | 2.5 (0.9–6.6) | 0.07 | |||||
| Sagtani (2013) | Nepal | FSWs | Depression (CES-D) | Physical, sexual, or emotional violence past 6 months | 210 | 90/62 | 10/48 | 7.0 (3.2–15.1) | <0.001 |
| Shahmanesh (2009) | India | FSWs | Suicide attempt past 3 months | Sexual violence ever | 326 | 18/55 | 18/234 | 4.3 (2.1–8.7) | <0.001 |
| Sexual, physical, or verbal violence past 12 months by intimate partner | 38/55 | 29/44 | 2.3 (1.2–4.3) | 0.01 | |||||
| Sexual, physical, or verbal violence past 12 months by others | 29/44 | 40/212 | 3.5 (2.0–6.2) | 0.001 | |||||
| Police raid past 12 months | 18/55 | 32/220 | 2.3 (1.2–4.3) | 0.01 | |||||
| Sherwood (2015) | Gambia | FSWs | Sad or depressed mood for more than 2 weeks at a time in past 3 years | Sexual violence ever by client | 251 | 51/100 | 19/71 | 1.9 (1.0–3.5) | 0.05 |
| Ulibarri (2013) | Mexico | FSWs who inject drugs | Depression (CES-D) | Physical violence ever | 624 | 269/269 | 35/49 | 1.4 (0.9–2.2) | 0.1 |
| Physical violence ever by client | 108/430 | 15/69 | 1.2 (0.6–2.1) | 0.6 | |||||
| Sexual violence ever | 283/255 | 30/54 | 2.0 (1.2–3.2) | 0.006 | |||||
| Ulibarri (2014) | Mexico | HIV-negative FSWs | Psychological distress (BSI) | Physical, sexual, or emotional violence past 6 months by clients | 924 | NA | NA | 2.0 (1.6–2.4) | <0.001 |
| ALCOHOL AND DRUG USE | |||||||||
| Bitty-Anderson (2019)*, Tchankoni (2020)* | Togo | FSWs | Psychological distress (Kessler) | Harmful/hazardous alcohol (AUDIT) | 952 | 82/99 | 350/421 | 1.0 (0.7–1.4) | 1.0 |
| Coetzee (2018) | South Africa | FSWs | Depression (CES-D) | Severe binge drinking (AUDIT) | 508 | 196/174 | 81/55 | 0.8 (0.5–1.1) | 0.2 |
| PTSD (PTSD-8) | 99/96 | 179/134 | 0.8 (0.5–1.1) | 0.2 | |||||
| Hong (2007a) | China | FSWs | Depression (CES-D) | Alcohol intoxication past 6 months | 454 | 62/112 | 26/78 | 1.7 (1.0–2.9) | 0.05 |
| Suicide ideation past 6 months | 31/34 | 118/221 | 1.7 (1.0–2.9) | 0.06 | |||||
| Suicide attempt past 6 months | 21/17 | 128/288 | 2.8 (1.4–5.4) | 0.003 | |||||
| Jain (2020) | Mexico | HIV-negative FSWs | Depression (PHQ-9) | Hazardous alcohol past year (AUDIT) | 295 | 57/49 | 79/110 | 1.6 (1.0–2.6) | 0.05 |
| Polydrug use past month | 45/61 | 40/149 | 2.8 (1.6–4.6) | <0.001 | |||||
| Patel (2015) | India | FSWs | Depression (PHQ-2) | Alcohol use past 30 days | 1,986 | 493/285 | 455/751 | 2.9 (2.4–3.4) | <0.001 |
| Zhang (2014a) | China | FSWs | Depression (CES-D) | Illicit drug use ever | 1,022 | 118/403 | 67/434 | 1.9 (1.4–2.6) | <0.001 |
| Zaller (2014)***, Yang (2018)*** | China | FSWs | Depression (CES-D) | Alcohol dependent (AUDIT ≥16) | 358 | 19/32 | 76/231 | 1.8 (1.0–3.4) | 0.06 |
| Suicide ideation past 12 months | Alcohol dependent (AUDIT ≥16) | 11/84 | 22/241 | 1.4 (0.7–3.1) | 0.4 | ||||
| Depression (CES-D) | Illicit drug use ever | 15/96 | 12/235 | 3.1 (1.4–6.8) | 0.005 | ||||
| CONDOM USE | |||||||||
| Abelson (2019) | Cameroon | FSWs | Depression (PHQ-9) | Inconsistent condom use with clients ever | 2,136 | 108/274 | 391/1363 | 1.4 (1.1–1.8) | 0.013 |
| Brody (2016) | Cambodia | FSWs | Psychological distress (GHQ-12) | Inconsistent condom use with clients past 3 months | 657 | 235/49 | 322/51 | 0.8 (0.5–1.2) | 0.2 |
| Inconsistent condom use with partner past 3 months | 255/29 | 340/33 | 0.9 (0.5–1.4) | 0.6 | |||||
| Gu (2010a) | China | FSWs who inject drugs | Depression (Chinese Depression Anxiety Stress Scale) | Inconsistent condom use with clients past 6 months | 234 | NA | NA | 1.2 (1.1–1.3) | <0.001 |
| Hong (2007b) | China | FSWs | Depression (CES-D) | Inconsistent condom use with clients | 278 | 140/34 | 62/42 | 2.8 (1.6–4.8) | <0.001 |
| Patel (2015) | India | FSWs | Depression (PHQ-2) | Inconsistent condom use occasional clients | 1,986 | 274/504 | 277/928 | 1.8 (1.5–2.2) | <0.001 |
| Inconsistent condom use with regular clients | 356/41 | 342/845 | 2.1 (1.8–2.6) | <0.001 | |||||
| Shahmanesh (2009) | India | FSWs | Suicide attempt past 3 months | Inconsistent condom use with clients | 326 | 26/47 | 63/189 | 4.3 (2.1–8.7) | <0.001 |
| Shen (2016) | China | FSWs | Depression (GHQ) | No condom last sex client | 653 | 69/270 | 64/245 | 1.0 (0.7–1.4) | 1.0 |
| No condom last sex partner | 70/138 | 120/105 | 0.4 (0.3–0.7) | <0.001 | |||||
| Urada (2013) | Philippines | FSWs | Depression (CES-D) | Inconsistent condom use with clients | 143 | 47/60 | 13/23 | 1.4 (0.6–3.0) |
0.4 |
| Zaller (2014)***, Yang (2018)*** | China | FSWs | Depression (CES-D) | Inconsistent condom use with clients past 6 months | 358 | 16/95 | 16/231 | 1.6 (1.2–2.1) | 0.018 |
| Inconsistent condom use with partner past 6 months | 67/44 | 138/109 | 1.2 (0.9–1.9) | 0.4 | |||||
| HIV/STIs | |||||||||
| Bitty-Anderson (2019)*, Tchankoni (2020)* | Togo | FSWs | Psychological distress (Kessler) | HIV positive | 952 | 80/101 | 45/726 | 12.8 (8.4–19.5) | <0.001 |
| Cange (2019) | Burkino Faso | FSWs | Suicide ideation ever | HIV positive | 696 | 22/104 | 56/395 | 1.5 (0.9–2.6) | 0.14 |
| Jain (2020) | Mexico | HIV-negative FSWs | Depression (PHQ-9) | Syphilis, chlamydia, or gonorrhoea positive | 295 | 32/74 | 24/165 | 3.0 (1.6–5.4) | <0.001 |
| MacLean (2018) | Malawi | FSWs | Depression (PHQ-9) | HIV positive | 200 | 12/3 | 126/59 | 1.9 (0.5–6.9) | 0.3 |
| PTSD (PCL-C) | 10/6 | 128/56 | 0.7 (0.3–2.1) | 1.6 | |||||
| Ortblad (2020) | Uganda | FSWs | Depression (PHQ-9) | HIV positive | 711 | 57/143 | 136/375 | 1.1 (0.8–1.6) | 0.6 |
| Suicide ideation | 45/93 | 148/425 | 1.4 (0.9–2.1) | 0.11 | |||||
| Zambia | Depression (PHQ-9) | HIV positive | 682 | 65/86 | 158/373 | 1.8 (1.2–2.6) | 0.002 | ||
| Suicide ideation | 85/142 | 138/317 | 1.4 (1.0–1.9) | 0.06 | |||||
| Peitzmeier (2014) | Gambia | FSWs | Sad or depressed mood for more than 2 weeks at a time in past 3 years | HIV positive | 246 | 31/123 | 9/87 | 2.4 (1.1–5.4) | 0.03 |
| Poliah (2017) | South Africa | FSWs | Depression (PHQ-9) | HIV positive | 150 | 93/17 | 22/6 | 1.5 (0.5–4.2) | 0.5 |
| Shen (2016) | China | FSWs | Depression (GHQ) | HIV positive | 653 | 3/339 | 1/310 | 2.7 (0.3–26.5) | 0.4 |
| Syphilis positive | 13/329 | 20/291 | 0.6 (0.3–1.2) | 0.1 | |||||
| Hepatitis C positive | 8/334 | 5/306 | 1.5 (0.5–4.5) | 0.5 | |||||
1Odds in the exposed (e.g., Depression and Violence/Depression and No Violence).
2Odds in the unexposed (e.g., No Depression and Violence/No Depression and No Violence).
*Studies use same data source.
***Studies use same data source but different cut-off for depression.
Abbreviations: AUDIT, Alcohol Use Disorders Identification Test; BSI, Brief Symptom Inventory; CES-D, Centre for Epidemiological Studies Depression Scale; FSW, female sex worker; GHQ, General Health Questionnaire; HIV, human immunodeficiency virus; OR, odds ratio; PCL-C, PTSD CheckList Civilian Version; PHQ, Patient Health Questionnaire; PTSD, post-traumatic stress disorder; STI, sexually transmitted infection.
Table 3. Mental health problems and associations with common risk factors.
| Risk factor | Total number of studies | Number of studies included in meta-analysis | Pooled OR (95% CI) | P value |
|---|---|---|---|---|
| Violence | ||||
| Depression and violence (recent or ever) | 13 | 7 | 2.2 (1.4–3.3) | <0.001 |
| Depression and recent violence | 6 | 5 | 2.3 (1.3–4.2) | 0.005 |
| Recent suicide attempt and violence (recent or ever) | 3 | 2 | 3.5 (2.3–5.5) | <0.001 |
| Alcohol and drug use | ||||
| Depression and alcohol use | 5 | 4 [3 with outlier removed] | 1.6 (0.8–3.1), 2.1 (1.4–3.2) | 0.2, <0.001 |
| Recent suicide ideation and alcohol use | 2 | 2 | 1.6 (1.0–2.5) | 0.003 |
| Depression and illicit drug use | 3 | 2 | 2.1 (1.4–3.1) | <0.001 |
| Condom use | ||||
| Depression and inconsistent condom use with clients | 7 | 6 | 1.6 (1.2–2.1) | 0.001 |
| Depression and inconsistent condom use with a regular partner | 2 | 2 | 0.7 (0.3–1.9) | 0.5 |
| HIV and STIs | ||||
| Depression and HIV | 4 | 4 (5 countries) | 1.4 (1.1–1.8) | 0.005 |
| Suicidal ideation (ever or recent) and HIV | 2 | 2 (3 countries) | 1.4 (1.1–1.8) | 0.04 |
Abbreviations: HIV, human immunodeficiency virus; STI, sexually transmitted infection
Violence
Seventeen studies reported on associations between mental health problems and violence experience [30,34,36,37,39,43,44,46,49,52,53,57,59,75,79,80,82], usually by an intimate partner or a client (Table 2). Measures of violence varied by timeframe (recent versus ever), typology (physical, sexual, emotional) and perpetrator (client, intimate partner, etc.). Overall, 13 studies reported associations between depression and violence [34,37,39,43,44,46,49,52,53,59,79,83], with 7 studies included in the meta-analyses (S1 Fig). The pooled unadjusted OR of depression and violence experience (ever or recent) is 2.2 (1.4–3.3), p < 0.001 (n = 7 studies), and the pooled unadjusted OR of depression and recent violence experience is 2.3 (1.3–4.2), p = 0.005 (n = 5 studies). Two studies [43,46] reported associations between PTSD and violence experience (ever or recent), with only one of these eligible for inclusion in a meta-analysis (unadjusted OR is 1.5 [0.8–2.6], p = 0.13) [46]. One study [30] with HIV-negative FSWs reported associations between psychological distress and recent violence by clients (unadjusted OR 2.0 [1.6–2.4], p < 0.001). One study reported suicide ideation ever and physical (unadjusted OR 1.7 [1.2–2.5], p = 0.008) or sexual violence experience ever (unadjusted OR 2.9 [2.0–4.2], p < 0.001) [36], and 2 studies reported recent suicidal ideation and violence experience (ever or recent), with only one of these eligible for inclusion in a meta-analysis (unadjusted OR 2.5 [1.3–4.7], p = 0.004) [79]. Three studies reported recent suicide attempt and violence experience (ever or recent), with 2 of these eligible for inclusion in a meta-analysis (S1 Fig). The pooled unadjusted OR of recent suicide attempt and violence experience (ever or recent) is 3.5 [2.2–5.5], p < 0.001.
Three studies reported on police violence (harassment, arrest, or raids) and mental health problems (Table 2). While no association was found between police harassment (ever) and current depression (unadjusted OR 0.9 [0.4–2.3], p = 0.9) [49], police arrest (ever) was associated with current depression in one study by Patel and colleagues (unadjusted OR 2.2 [1.7–2.8], p < 0.001) [53], and police raid in the past year was associated with a suicide attempt in the past 3 months (unadjusted OR 2.3 [1.2–4.3], p = 0.01) in a study by Shahmanesh and colleagues [80].
Alcohol and drug use
Associations between mental health problems and alcohol use were reported by 6 studies, but there was marked variation in how alcohol use was measured, with 2 studies asking about alcohol use in the past 30 days [53] or alcohol intoxication in the past 6 months [56] and 4 studies using Alcohol Use Disorders Identification Test (AUDIT) to measure hazardous, harmful, or dependent drinking [44,73,84] or severe binge drinking [46] (Table 2). The pooled unadjusted OR for depression and alcohol use is 1.6 (0.8–3.1), p = 0.2 (n = 4 studies) (S2 Fig); when the outlier study is removed from the analyses, the pooled unadjusted OR is 2.1 (1.4–3.2), p < 0.001 (n = 3 studies) (S2 Fig). Psychological distress and harmful drinking was reported by one study (unadjusted OR 1.0 [0.7–1.4], p = 1.0) [73]. The pooled unadjusted OR of recent suicide ideation and alcohol use is 1.6 (1.0–2.5), p = 0.03 (n = 2 studies) (S2 Fig); one study reported associations between a recent suicide attempt and alcohol use, with an unadjusted OR of 2.8 (1.4–5.5), p = 0.003.
Three studies reported on mental health problems and illicit drug use, again with considerable variation in the way illicit drug use was measured (any illicit drug use ever [85,86] versus polydrug use past month [44]). Two studies were included in the meta-analysis (S3 Fig). The pooled unadjusted OR for depression and illicit drug use is 2.1 (1.4–3.1), p < 0.001.
Condom use
Nine studies reported on mental health problems and condom use with clients and regular partners [24,53,56,60,62,68,71,80,84]. Condom use measurement varied with studies either reporting frequency of condom use (always versus not always) or condom use at last sex (yes/no). The pooled unadjusted OR for depression and inconsistent condom use with clients is 1.6 (1.2–2.1), p = 0.001 (n = 6 studies) (S3 Fig). The pooled unadjusted OR for depression and inconsistent condom use with a regular partner is 0.7 (0.3–1.9), p = 0.5 (n = 2 studies) (S3 Fig). One study reported on recent suicide attempt and inconsistent condom use with clients; the unadjusted OR was 4.3 (2.1–8.7), p < 0.001.
HIV/STIs
Eight studies reported on HIV/STI and mental health problems [36,44,47–49,60,69,73]. One study [48] was excluded from the meta-analyses because it did not use a validated tool to measure depression, and one study was excluded because it only sampled HIV-negative women [44]. The pooled unadjusted OR for depression and HIV is 1.4 (1.1–1.8), p = 0.005 (n = 4 studies from 5 countries) and for suicidal ideation and HIV is 1.4 (1.1–1.8), p = 0.04 (n = 2 studies from 3 countries) (S4 Fig). One study reported associations between depression and current syphilis infection; the unadjusted OR was 0.6 (0.3–1.2), p = 0.1 [60].
Discussion
In this systematic review and meta-analysis using data from 56 studies and 24,940 participants, we found that mental health problems are highly prevalent among FSWs in LMICs and are strongly associated with social and behavioural factors commonly experienced by FSWs. Of note, all studies were cross-sectional, and not a single intervention study designed to address mental disorders among FSWs was identified. The prevalence of mental disorders among FSWs in LMICs was much higher compared with the general population in LMICs. For example, data from 41 LMICs from the 2002–2004 World Health Survey found the prevalence of depression to range between 3.9% and 7.8%, with higher rates among women (7.0%–7.8%) compared with men (3.9%–4.9%) [87]. Additionally, the 12-month prevalence of suicidal behaviour among people in LMICs has been reported to be 2% for suicidal ideation and 0.4% for suicide attempts, with rates higher among women compared with men (ideation: 2.4% women versus 1.6% men; attempt: 0.5% women versus 0.4% men) [88]. FSWs face increased levels of key risk factors for mental disorders and suicidal behaviour, including financial stress, low education, inadequate housing, violence, alcohol and drug use, STIs including HIV, and stigma and discrimination [15, 17, 53, 67], which may help explain the higher prevalence of mental health problems in comparison with the general population. Indeed, findings from our meta-analyses support this hypothesis. Understanding how these social determinants interact with mental disorders and which are modifiable within programmatic timeframes will be crucial to designing holistic interventions for FSWs.
This review adhered to PRISMA guidelines and used a comprehensive search strategy, independent screening and quality appraisal of studies. This study had some limitations. By limiting the search to published studies only, and to literature written in English, we may have missed key studies. We used unadjusted ORs to examine associations between mental health problems and key risk factors to allow like-for-like comparisons between studies; not adjusting for potential confounders may have biased the findings although unadjusted and adjusted ORs were usually similar in individual studies. Where individual studies provided multiple estimates on co-linear outcomes (e.g., depression and violence; depression and police arrest), using unadjusted ORs to calculate the individual associations may have led to participants who had not experienced one outcome (e.g., police arrest) but who had experienced the other (e.g., violence) being included in the reference group and subsequent underestimation of the true association. The removal of studies that sampled participants based on characteristics that are known to be an independent risk factor for mental health problems (such as HIV status, harmful alcohol use) led to fewer studies being included and wider confidence intervals around prevalence estimates and pooled ORs. However, when we re-ran the analyses to include all qualifying studies, regardless of sampling criteria, we did indeed find that estimates were slightly higher, suggesting that inclusion of these studies would have led to an overestimation of the pooled estimates and associations. Several methodological issues across the studies were also observed. All studies were cross-sectional. Longitudinal studies are needed to ascertain direction of causality between mental health problems and other factors common to FSWs, although studies with the general population suggest that these relationships are likely to be bidirectional [89]. Most studies used nonprobability sampling across a wide variety of settings which may introduce selection bias and mean that the most vulnerable women will be missed from these surveys. This in turn may lead to underestimations of mental health estimates. A range of measurement tools was used to capture mental health outcomes, as well as violence, alcohol and drug use, and condom use. Even when studies used the same mental health outcome measures, different cut-off scores were applied. This limits the comparability and reliability of findings across studies and points to a need for establishing more rigorous guidelines on using validated tools with this study population.
To our knowledge, this systematic review is the first globally to estimate the prevalence of mental health problems among FSWs in LMICs and to examine associations between poor mental health and other risk factors common in sex workers’ lives. Our findings and meta-analyses suggest that FSWs experience a high burden of depression, anxiety, PTSD, psychological distress, and suicidal behaviours and that poor mental health is strongly associated with violence experience, drug use, inconsistent condom use, and HIV/STI. Together, this supports the concept of overlapping vulnerabilities and has several important implications.
First, there are no existing studies that we are aware of that describe mental health interventions; low-cost, effective interventions for FSWs with mental health disorders are urgently needed. Among the general population attending primary care services in India and elsewhere, brief psychological interventions delivered by trained lay-counsellors have been shown to effectively treat depression [90,91]. Strategies to prevent suicide could include promoting mental health, limiting access to the means for suicide, reducing harmful alcohol use and violence experience, and training “gatekeepers” to support women at increased risk, such as those who have previously attempted suicide [6]. Such interventions should also be suitable for FSWs and could be adapted and embedded within existing HIV service provision. Second, the strong associations between mental health disorders and key occupational risk factors such as violence and harmful alcohol and drug use support the need for upstream structural interventions as part of holistic HIV prevention programming for FSWs. Again, violence interventions have been shown to be effective in reducing violence among women in LMICs [92,93] as well as among FSWs [94]. Low-cost, brief psychological interventions to treat harmful alcohol use could also be adapted to FSW settings [95]. Third, strong associations between poor mental health and reduced condom use with clients and with HIV infection suggest that treatment of mental health problems may also improve condom use with clients and the sexual and reproductive health of FSWs. In addition, women diagnosed with HIV may require on-going counselling and support, for example, by HIV testing and screening counsellors or FSW peer advocates, which goes beyond CD4 counts and treatment adherence, to also enquire about a woman’s ongoing psychological well-being.
Supporting information
(DOC)
(DOCX)
CEBM, Centre for Evidence-Based Management.
(DOCX)
(DOCX)
(TIF)
(TIF)
(TIF)
HIV, human immunodeficiency virus.
(TIF)
Abbreviations
- AUDIT
Alcohol Use Disorders Identification Test
- CEBM
Centre for Evidence-Based Management
- FSW
female sex worker
- HIV
human immunodeficiency virus
- IQR
interquartile range
- LMIC
low- and middle-income country
- OR
odds ratio
- PRISMA
Preferred Reporting Items for Systematic reviews and Meta-Analysis
- PTSD
post-traumatic stress disorder
- STI
sexually transmitted infection
- UNAIDS
The Joint United Nations Programme on HIV/AIDS
Data Availability
The data underlying the quantitative synthesis are provided in Tables 1 and 2 within the manuscript.
Funding Statement
Funding for this study was provided by the Medical Research Council and the UK Department of International Development (DFID) (MR/R023182/1) as part of the Maisha Fiti study, and by DFID (PO 5244) as part of STRIVE, a 6-year programme of research and action devoted to tackling the structural drivers of HIV ((http://STRIVE.lshtm.ac.uk/). No funding bodies had any role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Patel V, Chisholm D, Parikh R, Charlson FJ, Degenhardt L, Dua T, et al. Addressing the burden of mental, neurological, and substance use disorders: key messages from Disease Control Priorities, 3rd edition. Lancet. 2016;387(10028):1672–85. 10.1016/S0140-6736(15)00390-6 [DOI] [PubMed] [Google Scholar]
- 2.Whiteford HA, Ferrari AJ, Degenhardt L, Feigin V, Vos T. The global burden of mental, neurological and substance use disorders: an analysis from the Global Burden of Disease Study 2010. PLoS One. 2015;10(2):e0116820 10.1371/journal.pone.0116820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Herrman H, Kieling C, McGorry P, Horton R, Sargent J, Patel V. Reducing the global burden of depression: a Lancet-World Psychiatric Association Commission. Lancet. 2019;393(10189):e42–e3. 10.1016/S0140-6736(18)32408-5 [DOI] [PubMed] [Google Scholar]
- 4.Thornicroft G, Chatterji S, Evans-Lacko S, Gruber M, Sampson N, Aguilar-Gaxiola S, et al. Undertreatment of people with major depressive disorder in 21 countries. Br J Psychiatry. 2017;210(2):119–24. 10.1192/bjp.bp.116.188078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Patel V, Saxena S. Achieving universal health coverage for mental disorders. BMJ. 2019;366:l4516 10.1136/bmj.l4516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organisation. Preventing suicide: A global imperative. Geneva, Switzerland. 2014. [cited 2019 Nov 15]. https://apps.who.int/iris/bitstream/handle/10665/131056/9789241564779_eng.pdf;jsessionid=E8AF63B011C3D3467A0D2383EB50A69A?sequence=1.
- 7.UNAIDS. Sex work and HIV/AIDS: Technical Update. Geneva. 2002. [cited 2020 May 26]. http://data.unaids.org/publications/irc-pub02/jc705-sexwork-tu_en.pdf.
- 8.Platt L, Grenfell P, Meiksin R, Elmes J, Sherman SG, Sanders T, et al. Associations between sex work laws and sex workers' health: A systematic review and meta-analysis of quantitative and qualitative studies. PLoS Med. 2018;15(12):e1002680 10.1371/journal.pmed.1002680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hengartner MP, Islam MN, Haker H, Rossler W. Mental Health and Functioning of Female Sex Workers in Chittagong, Bangladesh. Front Psychiatry. 2015;6:176 10.3389/fpsyt.2015.00176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Suresh G, Furr LA, Srikrishnan AK. An assessment of the mental health of street-based sex workers in Chennai, India. J Contemporary Criminal Justice. 2009;25(2):186–201. [Google Scholar]
- 11.el-Bassel N, Schilling RF, Irwin KL, Faruque S, Gilbert L, Von Bargen J, et al. Sex trading and psychological distress among women recruited from the streets of Harlem. Am J Public Health. 1997;87(1):66–70. 10.2105/ajph.87.1.66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rössler W, Koch U, Lauber C, Hass AK, Altwegg M, Ajdacic-Gross V, et al. The mental health of female sex workers. Acta Psychiatr Scand. 2010;122(2):143–52. 10.1111/j.1600-0447.2009.01533.x [DOI] [PubMed] [Google Scholar]
- 13.Roxburgh A, Degenhardt L, Copeland J, Larance B. Drug dependence and associated risks among female street-based sex workers in the greater Sydney area, Australia. Subst Use Misuse. 2008;43(8–9):1202–17. 10.1080/10826080801914410 [DOI] [PubMed] [Google Scholar]
- 14.Surratt HL, Kurtz SP, Weaver JC, Inciardi JA. The Connections of Mental Health Problems, Violent Life Experiences, and the Social Milieu of the “Stroll” with the HIV Risk Behaviors of Female Street Sex Workers. Journal of Psychology & Human Sexuality. 2005;17(1–2):23–44. 10.1300/J056v17n01_03 [DOI] [Google Scholar]
- 15.Deering KN, Amin A, Shoveller J, Nesbitt A, Garcia-Moreno C, Duff P, et al. A systematic review of the correlates of violence against sex workers. Am J Public Health. 2014;104(5):e42–54. 10.2105/AJPH.2014.301909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yuen WW, Tran L, Wong CK, Holroyd E, Tang CS, Wong WC. Psychological health and HIV transmission among female sex workers: a systematic review and meta-analysis. AIDS Care. 2016;28(7):816–24. 10.1080/09540121.2016.1139038 [DOI] [PubMed] [Google Scholar]
- 17.Li Q, Li X, Stanton B. Alcohol use among female sex workers and male clients: an integrative review of global literature. Alcohol Alcohol. 2010;45(2):188–99. 10.1093/alcalc/agp095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.World Bank. World Bank Income Groups. World Bank. 2019. [cited 2019 May 21]. https://data.worldbank.org/income-level/low-and-middle-income.
- 19.Oram S, Stöckl H, Busza J, Howard LM, Zimmerman C. Prevalence and risk of violence and the physical, mental, and sexual health problems associated with human trafficking: systematic review. PLoS Med. 2012;9(5):e1001224 10.1371/journal.pmed.1001224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ottisova L, Hemmings S, Howard LM, Zimmerman C, Oram S. Prevalence and risk of violence and the mental, physical and sexual health problems associated with human trafficking: an updated systematic review. Epidemiol Psychiatr Sci. 2016;25(4):317–41. 10.1017/S2045796016000135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Strathdee SA, West BS, Reed E, Moazen B, Azim T, Dolan K. Substance Use and HIV Among Female Sex Workers and Female Prisoners: Risk Environments and Implications for Prevention, Treatment, and Policies. J Acquir Immune Defic Syndr. 2015;69 Suppl 2(0 1):S110–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stoebenau K, Heise L, Wamoyi J, Bobrova N. Revisiting the understanding of "transactional sex" in sub-Saharan Africa: A review and synthesis of the literature. Soc Sci Med. 2016;168:186–97. 10.1016/j.socscimed.2016.09.023 [DOI] [PubMed] [Google Scholar]
- 23.Barnhart DA, Harling G, Muya A, Ortblad KF, Mashasi I, Dambach P, et al. Structural, interpersonal, psychosocial, and behavioral risk factors for HIV acquisition among female bar workers in Dar es Salaam, Tanzania. AIDS Care. 2019:1–10. 10.1080/09540121.2019.1699642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gu J, Lau JT, Chen H, Chen X, Liu C, Liu J. Mental health and interpersonal factors associated with HIV-related risk behaviors among non-institutionalized female injection drug users who are also sex workers in China. Women Health. 2010;50(1):20–36. 10.1080/03630241003601137 [DOI] [PubMed] [Google Scholar]
- 25.Jackson T, Huang A, Chen H, Gao X, Zhang Y, Zhong X. Predictors of willingness to use HIV pre-exposure prophylaxis among female sex workers in Southwest China. AIDS Care. 2013;25(5):601–5. 10.1080/09540121.2012.726341 [DOI] [PubMed] [Google Scholar]
- 26.Lari MA, Bagheri P, Ameli F. Mental health and HIV-related high-risk behaviors among female sex workers. Shiraz E-Medical Journal. 2014;15(4). [Google Scholar]
- 27.Logie CH, Marcus N, Wang Y, Lacombe-Duncan A, Levermore K, Jones N, et al. Contextualising sexual health practices among lesbian and bisexual women in Jamaica: a multi-methods study. Reprod Health Matters. 2018;26(52):1517543 10.1080/09688080.2018.1517543 [DOI] [PubMed] [Google Scholar]
- 28.Offringa R, Tsai LC, Aira T, Riedel M, Witte SS. Personal and Financial Risk Typologies Among Women Who Engage in Sex Work in Mongolia: A Latent Class Analysis. Arch Sex Behav. 2017;46(6):1857–66. 10.1007/s10508-016-0824-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ulibarri MD, Semple SJ, Rao S, Strathdee SA, Fraga-Vallejo MA, Bucardo J, et al. History of abuse and psychological distress symptoms among female sex workers in two Mexico-U.S. border cities. Violence Vict. 2009;24(3):399–413. 10.1891/0886-6708.24.3.399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ulibarri MD, Strathdee SA, Lozada R, Magis-Rodriguez C, Amaro H, O'Campo P, et al. Prevalence and correlates of client-perpetrated abuse among female sex workers in two Mexico-u.s. Border cities. Violence Against Women. 2014;20(4):427–45. 10.1177/1077801214528582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ulibarri MD, Roesch S, Rangel MG, Staines H, Amaro H, Strathdee SA. “Amar te duele”(“Love hurts”): sexual relationship power, intimate partner violence, depression symptoms and HIV risk among female sex workers who use drugs and their non-commercial, steady partners in Mexico. AIDS Behav. 2015;19(1):9–18. 10.1007/s10461-014-0772-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ghose T, Chowdhury A, Solomon P, Ali S. Depression and anxiety among HIV-positive sex workers in Kolkata, India: Testing and modifying the Hospital Anxiety Depression Scale. Int Social Work. 2015;58(2):211–22. [Google Scholar]
- 33.Pandiyan K, Chandrasekhar H, Madhusudhan S. Psychological morbidity among female commercial sex workers with alcohol and drug abuse. Indian J Psychiatry. 2012;54(4):349–51. 10.4103/0019-5545.104822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ulibarri MD, Hiller SP, Lozada R, Rangel MG, Stockman JK, Silverman JG, et al. Prevalence and characteristics of abuse experiences and depression symptoms among injection drug-using female sex workers in Mexico. J Environ Public Health. 2013;2013:631479 10.1155/2013/631479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Witte SS, Batsukh A, Chang M. Sexual risk behaviors, alcohol abuse, and intimate partner violence among sex workers in Mongolia: implications for HIV prevention intervention development. J Prev Interv Community. 2010;38(2):89–103. 10.1080/10852351003640625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cange CW, Wirtz AL, Ky-Zerbo O, Lougue M, Kouanda S, Baral S. Effects of traumatic events on sex workers' mental health and suicide intentions in Burkina Faso: a trauma-informed approach. Sex Health. 2019;16(4):348–57. 10.1071/SH17213 [DOI] [PubMed] [Google Scholar]
- 37.Carlson CE, Witte SS, Pala AN, Tsai LC, Wainberg M, Aira T. The impact of violence, perceived stigma, and other work-related stressors on depressive symptoms among women engaged in sex work. Glob Soc Welf. 2017;4(2):51–7. 10.1007/s40609-017-0085-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gu J, Lau JT, Chen H, Tsui H, Ling W. Prevalence and factors related to syringe sharing behaviours among female injecting drug users who are also sex workers in China. Int J Drug Policy. 2011;22(1):26–33. 10.1016/j.drugpo.2010.06.005 [DOI] [PubMed] [Google Scholar]
- 39.Gu J, Lau JT, Li M, Li H, Gao Q, Feng X, et al. Socio-ecological factors associated with depression, suicidal ideation and suicidal attempt among female injection drug users who are sex workers in China. Drug Alcohol Depend. 2014;144:102–10. 10.1016/j.drugalcdep.2014.08.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lion RR, Watt MH, Wechsberg WM, Meade CS. Gender and Sex Trading Among Active Methamphetamine Users in Cape Town, South Africa. Subst Use Misuse. 2017;52(6):773–84. 10.1080/10826084.2016.1264964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Muth S, Len A, Evans JL, Phou M, Chhit S, Neak Y, et al. HIV treatment cascade among female entertainment and sex workers in Cambodia: impact of amphetamine use and an HIV prevention program. Addict Sci Clin Pract. 2017;12(1):20 10.1186/s13722-017-0085-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rael CT, Sheinfil A, Hampanda K, Carballo-Dieguez A, Pala AN, Brown W 3rd. Examining the unique characteristics of a non-probability sample of undocumented female sex workers with dependent children: The case of Haitians in the Dominican Republic. Sexuality Cult. 2017;21(3):680–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Roberts ST, Flaherty BP, Deya R, Masese L, Ngina J, McClelland RS, et al. Patterns of Gender-Based Violence and Associations with Mental Health and HIV Risk Behavior Among Female Sex Workers in Mombasa, Kenya: A Latent Class Analysis. AIDS Behav. 2018;22(10):3273–86. 10.1007/s10461-018-2107-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jain JP, Strathdee SA, Patterson TL, Semple SJ, Harvey-Vera A, Magis-Rodriguez C, et al. Perceived barriers to pre-exposure prophylaxis use and the role of syndemic factors among female sex workers in the Mexico-United States border region: a latent class analysis. AIDS Care. 2020;32(5):557–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Semple SJ, Pines HA, Vera AH, Pitpitan EV, Martinez G, Rangel MG, et al. Maternal role strain and depressive symptoms among female sex workers in Mexico: the moderating role of sex work venue. Women Health. 2020;60(3):284–99. 10.1080/03630242.2019.1626792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Coetzee J, Buckley J, Otwombe K, Milovanovic M, Gray GE, Jewkes R. Depression and Post Traumatic Stress amongst female sex workers in Soweto, South Africa: A cross sectional, respondent driven sample. PLoS ONE. 2018;13(7):e0196759 10.1371/journal.pone.0196759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.MacLean SA, Lancaster KE, Lungu T, Mmodzi P, Hosseinipour MC, Pence BW, et al. Prevalence and correlates of probable depression and post-traumatic stress disorder among female sex workers in Lilongwe, Malawi. Int J Ment Health Addict. 2018;16(1):150–63. 10.1007/s11469-017-9829-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Peitzmeier S, Mason K, Ceesay N, Diouf D, Drame F, Loum J, et al. A cross-sectional evaluation of the prevalence and associations of HIV among female sex workers in the Gambia. Int J STD AIDS. 2014;25(4):244–52. 10.1177/0956462413498858 [DOI] [PubMed] [Google Scholar]
- 49.Poliah V, Paruk S. Depression, anxiety symptoms and substance use amongst sex workers attending a non-governmental organisation in KwaZulu-Natal, South Africa. South African Family Practice. 2017;59(3):116–22. [Google Scholar]
- 50.Iaisuklang MG, Ali A. Psychiatric morbidity among female commercial sex workers. Indian J Psychiatry. 2017;59(4):465–70. 10.4103/psychiatry.IndianJPsychiatry_147_16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lang DL, Salazar LF, Diclemente RJ, Markosyan K, Darbinyan N. Predictors of condom errors among sex workers in Armenia. Int J STD AIDS. 2011;22(3):126–30. 10.1258/ijsa.2009.009418 [DOI] [PubMed] [Google Scholar]
- 52.Patel SK, Ganju D, Prabhakar P, Adhikary R. Relationship between mobility, violence and major depression among female sex workers: a cross-sectional study in southern India. BMJ open. 2016;6(9):e011439 10.1136/bmjopen-2016-011439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Patel SK, Saggurti N, Pachauri S, Prabhakar P. Correlates of mental depression among female sex workers in Southern India. Asia Pac J Public Health. 2015;27(8):809–19. 10.1177/1010539515601480 [DOI] [PubMed] [Google Scholar]
- 54.Chen H, Li X, Li B, Huang A. Negative trust and depression among female sex workers in Western China: The mediating role of thwarted belongingness. Psychiatry research. 2017;256:448–52. 10.1016/j.psychres.2017.06.031 [DOI] [PubMed] [Google Scholar]
- 55.Hong Y, Fang X, Li X, Liu Y, Li M, Tai-Seale T. Self-perceived stigma, depressive symptoms, and suicidal behaviors among female sex workers in China. J Transcult Nurs. 2010;21(1):29–34. 10.1177/1043659609349063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hong Y, Li X, Fang X, Zhao R. Depressive symptoms and condom use with clients among female sex workers in China. Sex Health. 2007;4(2):99–104. 10.1071/sh06063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hong Y, Zhang C, Li X, Liu W, Zhou Y. Partner violence and psychosocial distress among female sex workers in China. PLoS ONE. 2013;8(4):e62290 10.1371/journal.pone.0062290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Huang W, Operario D, Dong Y, Zaller N, Song D, He H, et al. HIV-related risk among female migrants working in entertainment venues in China. Prev Sci. 2014;15(3):329–39. 10.1007/s11121-013-0423-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sagtani RA, Bhattarai S, Adhikari BR, Baral D, Yadav DK, Pokharel PK. Violence, HIV risk behaviour and depression among female sex workers of eastern Nepal. BMJ Open. 2013;3(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Shen H, Zou H, Huang S, Liu F, Zhao P, Chen L, et al. Depression and HIV Risk Behaviors among Female Sex Workers in Guangdong, China: A Multicenter Cross-Sectional Study. BioMed Res lnt. 2016;2016:6986173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Shrestha R, Philip S, Shewade HD, Rawal B, Deuba K. Why don't key populations access HIV testing and counselling centres in Nepal? Findings based on national surveillance survey. BMJ Open. 2017;7(12):e017408 10.1136/bmjopen-2017-017408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Urada LA, Simmons J. Social and structural constraints on disclosure and informed consent for HIV survey research involving female sex workers and their bar managers in the Philippines. J Empir Res Hum Res Ethics. 2014;9(1):29–40. 10.1525/jer.2014.9.1.29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Yang H, Li X, Stanton B, Chen X, Liu H, Fang X, et al. HIV-related risk factors associated with commercial sex among female migrants in China. Health Care Women Int. 2005;26(2):134–48. 10.1080/07399330590905585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Devoglio LL, Corrente JE, Borgato MH, Godoy I. Smoking among female sex workers: prevalence and associated variables. J Bras Pneumol. 2017;43(1):6–13. 10.1590/S1806-37562016000000162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.González-Forteza C, Rodríguez EM, de Iturbe PF, Vega L, Tapia AJ. Social correlates of depression and suicide risk in sexual workers from Hidalgo, Mexico. Salud Mental. 2014;37(4):349–54. [Google Scholar]
- 66.Rael CT, Davis A. Depression and key associated factors in female sex workers and women living with HIV/AIDS in the Dominican Republic. Int J STD AIDS. 2017;28(5):433–40. 10.1177/0956462416651374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Baral S, Beyrer C, Muessig K, Poteat T, Wirtz AL, Decker MR, et al. Burden of HIV among female sex workers in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12(7): 538–49. 10.1016/S1473-3099(12)70066-X [DOI] [PubMed] [Google Scholar]
- 68.Abelson A, Lyons C, Decker M, Ketende S, Mfochive Njindam I, Fouda G, et al. Lifetime experiences of gender-based violence, depression and condom use among female sex workers in Cameroon. Int J Soc Psychiatry. 2019;65(6):445–57. 10.1177/0020764019858646 [DOI] [PubMed] [Google Scholar]
- 69.Ortblad KF, Musoke DK, Chanda MM, Ngabirano T, Velloza J, Haberer JE, et al. Knowledge of HIV Status Is Associated With a Decrease in the Severity of Depressive Symptoms Among Female Sex Workers in Uganda and Zambia. J Acquir Immune Defic Syndr. 2020;83(1):37–46. 10.1097/QAI.0000000000002224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ranjbar F, Sadeghi-Bazargani H, Pishgahi A, Nobari O, Farahbakhsh M, Farhang S, et al. Mental health status among female sex workers in Tabriz, Iran. Arch Womens Ment Health. 2019;22(3):391–7. Epub 2018/08/22. 10.1007/s00737-018-0907-1 . [DOI] [PubMed] [Google Scholar]
- 71.Brody C, Chhoun P, Tuot S, Pal K, Chhim K, Yi S. HIV risk and psychological distress among female entertainment workers in Cambodia: a cross-sectional study. BMC Public Health. 2016;16:133 10.1186/s12889-016-2814-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Rhead R, Elmes J, Otobo E, Nhongo K, Takaruza A, White PJ, et al. Do female sex workers have lower uptake of HIV treatment services than non-sex workers? A cross-sectional study from east Zimbabwe. BMJ Open. 2018;8(2):e018751 10.1136/bmjopen-2017-018751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Bitty-Anderson AM, Gbeasor-Komlanvi FA, Johnson P, Sewu EK, Dagnra CA, Salou M, et al. Prevalence and correlates of alcohol and tobacco use among key populations in Togo in 2017: a cross-sectional study. BMJ Open. 2019;9(11):e028934 10.1136/bmjopen-2019-028934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Akinnawo EO. Mental health implications of the commercial sex industry in Nigeria. Health Transition Review. 1995;5:173–7. [Google Scholar]
- 75.Berger BO, Grosso A, Adams D, Ketende S, Sithole B, Mabuza XS, et al. The Prevalence and Correlates of Physical and Sexual Violence Affecting Female Sex Workers in Swaziland. J Int Violence. 2018;33(17):2745–66. [DOI] [PubMed] [Google Scholar]
- 76.Grosso AL, Ketende SC, Stahlman S, Ky-Zerbo O, Ouedraogo HG, Kouanda S, et al. Development and reliability of metrics to characterize types and sources of stigma among men who have sex with men and female sex workers in Togo and Burkina Faso. BMC Infect Dis. 2019;19(1):208 10.1186/s12879-019-3693-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kim HY, Grosso A, Ky-Zerbo O, Lougue M, Stahlman S, Samadoulougou C, et al. Stigma as a barrier to health care utilization among female sex workers and men who have sex with men in Burkina Faso. Ann Epidemiol. 2018;28(1):13–9. 10.1016/j.annepidem.2017.11.009 [DOI] [PubMed] [Google Scholar]
- 78.Fang X, Li X, Yang H, Hong Y, Zhao R, Dong B, et al. Profile of female sex workers in a Chinese county: does it differ by where they came from and where they work? World Health Popul. 2007;9(1):46–64. 10.12927/whp.2007.18695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Hong Y, Li X, Fang X, Zhao R. Correlates of suicidal ideation and attempt among female sex workers in China. Health Care Women Int. 2007;28(5):490–505. 10.1080/07399330701226529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Shahmanesh M, Wayal S, Cowan F, Mabey D, Copas A, Patel V. Suicidal behavior among female sex workers in Goa, India: the silent epidemic. Am J Public Health. 2009;99(7):1239–46. 10.2105/AJPH.2008.149930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Su S, Li X, Zhang L, Lin D, Zhang C, Zhou Y. Age group differences in HIV risk and mental health problems among female sex workers in Southwest China. AIDS Care. 2014;26(8):1019–26. 10.1080/09540121.2013.878780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Sherwood JA, Grosso A, Decker MR, Peitzmeier S, Papworth E, Diouf D, et al. Sexual violence against female sex workers in The Gambia: a cross-sectional examination of the associations between victimization and reproductive, sexual and mental health. BMC Public Health. 2015;15:270 10.1186/s12889-015-1583-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Zhang L, Li X, Wang B, Shen Z, Zhou Y, Xu J, et al. Violence, stigma and mental health among female sex workers in China: A structural equation modeling. Women Health. 2017;57(6):685–704. 10.1080/03630242.2016.1186781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zaller N, Huang W, He H, Dong Y, Song D, Zhang H, et al. Risky alcohol use among migrant women in entertainment venues in China. Alcohol Alcohol. 2014;49(3):321–6. 10.1093/alcalc/agt184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Yang Q, Operario D, Zaller N, Huang W, Dong Y, Zhang H. Depression and its correlations with health-risk behaviors and social capital among female migrants working in entertainment venues in China. PLoS ONE. 2018;13(2):e0191632 10.1371/journal.pone.0191632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Zhang C, Li X, Chen Y, Hong Y, Shan Q, Liu W, et al. Alcohol and other drug use, partner violence, and mental health problems among female sex workers in southwest China. Health care Women Int. 2014;35(1):60–73. 10.1080/07399332.2012.757317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Hosseinpoor AR, Bergen N, Mendis S, Harper S, Verdes E, Kunst A, et al. Socioeconomic inequality in the prevalence of noncommunicable diseases in low- and middle-income countries: results from the World Health Survey. BMC Public Health. 2012;12:474 10.1186/1471-2458-12-474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Borges G, Nock MK, Haro Abad JM, Hwang I, Sampson NA, Alonso J, et al. Twelve-month prevalence of and risk factors for suicide attempts in the World Health Organization World Mental Health Surveys. J Clin Psychiatry. 2010;71(12):1617–28. 10.4088/JCP.08m04967blu [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Devries KM, Mak JY, Bacchus LJ, Child JC, Falder G, Petzold M, et al. Intimate partner violence and incident depressive symptoms and suicide attempts: a systematic review of longitudinal studies. PLoS Med. 2013;10(5):e1001439 10.1371/journal.pmed.1001439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Patel V, Weobong B, Weiss HA, Anand A, Bhat B, Katti B, et al. The Healthy Activity Program (HAP), a lay counsellor-delivered brief psychological treatment for severe depression, in primary care in India: a randomised controlled trial. Lancet. 2017;389(10065):176–85. 10.1016/S0140-6736(16)31589-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Chibanda D, Weiss HA, Verhey R, Simms V, Munjoma R, Rusakaniko S, et al. Effect of a Primary Care-Based Psychological Intervention on Symptoms of Common Mental Disorders in Zimbabwe: A Randomized Clinical Trial. JAMA. 2016;316(24):2618–26. 10.1001/jama.2016.19102 [DOI] [PubMed] [Google Scholar]
- 92.Abramsky T, Devries K, Kiss L, Nakuti J, Kyegombe N, Starmann E, et al. Findings from the SASA! Study: a cluster randomized controlled trial to assess the impact of a community mobilization intervention to prevent violence against women and reduce HIV risk in Kampala, Uganda. BMC Med. 2014;12:122 10.1186/s12916-014-0122-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Kapiga S, Harvey S, Mshana G, Hansen CH, Mtolela GJ, Madaha F, et al. A social empowerment intervention to prevent intimate partner violence against women in a microfinance scheme in Tanzania: findings from the MAISHA cluster randomised controlled trial. Lancet Glob Health. 2019;7(10):e1423–e34. 10.1016/S2214-109X(19)30316-X [DOI] [PubMed] [Google Scholar]
- 94.Beattie TS, Bhattacharjee P, Isac S, Mohan HL, Simic-Lawson M, Ramesh BM, et al. Declines in violence and police arrest among female sex workers in Karnataka state, south India, following a comprehensive HIV prevention programme. J Int AIDS Soc. 2015;18:20079 10.7448/IAS.18.1.20079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Nadkarni A, Weobong B, Weiss HA, McCambridge J, Bhat B, Katti B, et al. Counselling for Alcohol Problems (CAP), a lay counsellor-delivered brief psychological treatment for harmful drinking in men, in primary care in India: a randomised controlled trial. Lancet. 2017;389(10065):186–95. 10.1016/S0140-6736(16)31590-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
(DOCX)
CEBM, Centre for Evidence-Based Management.
(DOCX)
(DOCX)
(TIF)
(TIF)
(TIF)
HIV, human immunodeficiency virus.
(TIF)
Data Availability Statement
The data underlying the quantitative synthesis are provided in Tables 1 and 2 within the manuscript.