Abstract
The main purpose of our review study was to estimate depression prevalence among Saudi Arabian medical students according to the published articles and try to reveal the main associated factors. A systematic search was performed through PubMed/Medline and Google Scholar databases. A review of 18 studies published between January 2010 and March 2019 was composed of the following selection of necessary articles approved by PICO (population, intervention, control, and outcomes) criteria. The prevalence of depression among medical students of Saudi Arabia ranged from 30.9% to 77.6% with a mean prevalence of 51.5%. Depression severity was evaluated by various questionnaires, so we summarized the extracted data and revealed that medical students tend to have moderate to severe depression to a greater extent than mild depressive symptoms (33.27% vs 29.9%). The findings of this review suggest a high incidence of depression among medical students and the influence of associate sociodemographic factors. Females are considered to be at a higher risk of depression. First-year medical students are the most susceptible to develop depressive symptoms. Smoking is strongly associated with depression severity. Marital status, eating habits, usage of stimulants, and sleep disturbances are within significant findings of our review study.
Keywords: Depression, medical students, prevalence, Saudi Arabia
Introduction
Mental health is considered as an indispensable component of health according to the World Health Organization and UN Office of the High Commissioner for Human Rights.[1] Depression is a common psychiatric disorder leading to both social and physical disability and loss of productivity.[2] In the latest estimation by WHO, the prevalence of depression worldwide is 322 million.[3] In the last few years, the percentage of living people with depression has increased by 18.4% between 2005–2015.[4] It is anticipated that depression would be the second driving reason for disability by the year 2020[5] In 2015, the total cases in Saudi Arabia has been estimated to be nearly 1.4 million (4.8% of the population).[3] Depression is a life-threatening disorder. A more accurate term “depressive disorders” has a variety of clinical manifestations. Depressive disorders include disruptive mood dysregulation disorder, major depressive disorder, persistent depressive disorder, premenstrual dysphoric disorder, and depressive disorder due to another medical condition.[6] Depression has been connected to several causes including social environments such as traumatic events and daily stressors. Genetic factors have also been considered as a likely cause.[7,8,9,10,11] According to the Diagnostic and Statistical Manual of Mental Disorders 5th edition, depressive disorders are characterized by the presence of sadness, emptiness, or irritable mood, accompanied by somatic and cognitive changes that significantly affect the individual's everyday performance.[6] Depression is frequently undiagnosed and untreated.[12] Many reasons hamper help-seeking behavior, one of which is the lack of mental health literacy.[13] Another reason is the stigma or negative attitude towards people with mental disorders.[13,14]
The diagnostic criteria for major depressive disorder in the DSM-5 include the presence of five or more of the following symptoms for 2 weeks with the mandatory presence of both depressed mood and anhedonia. Among other symptoms may count sleep disturbances, significant weight changes, psychomotor agitation or retardation, fatigue, feelings of worthlessness or excessive guilt, decreased concentration, and recurrent thoughts of death and suicide. However, substance use, another medical condition and single manic or hypomanic episode experienced in the past exclude the presence of major depressive disorder. Depending on the number and severity of symptoms, a depressive episode can be categorized as mild, moderate, or severe.[6]
Unique questionnaires were developed to evaluate the severity of depression. The most widely used depressive symptoms evaluation survey is the Patient Health Questionnaire which is composed of 9 questions with 4 options scored from 0 to 3 points with a total score of 27. In this questionnaire scores are classified as follows: none 0–4, mild 5–9, moderate 10–14, moderately severe 15–19, and severe depression 20 and more.[15] Beck depression inventory is a 21-question multiple-choice screening tool covering sadness, pessimism, sense of failure, dissatisfaction, guilt, the expectation of punishment, weight loss, somatic preoccupation, and loss of libido. Total score can range from 0 to 63, thus the classification of depression scores involves normal 0–9, mild 10–15, moderate to severe 16–29, and severe 30 and more.[16] Depression, Anxiety and Stress Scale consists of 21 components and categorizes in the following manner: normal 0–4, mild 5–6, moderate 7–10, severe 11–13, and extremely severe 14 and more.[17] Mental Health Inventory consists of 38 items applying to anxiety, depression, and other components of emotional well-being.[18] Hospital Anxiety and Depression Scale includes 14 questions – each 7 concerning both depression and anxiety with evaluation scale from 0 to 3. A total number of points indicate normal state if 0–7, borderline state if 8–10, and a full presence of depressive disorder if 11–21.[19]
Psychological and mental health problems among university students are considered an escalating public health problem worldwide.[20] Medical students have a greater risk of developing depression. As reported, stress levels are higher in medical students compared to the general population.[21,22,23,24]
MBBS degree in Saudi Arabia is a program for undergraduates that runs for 7 years including 1 year of practical internship.[25]
Throughout the medical years as the materials needed for professional knowledge are dense and expanding year by year, responsibilities arise for the students each year, increasing in difficulty and complexity, stress accumulates due to not being able to complete certain objectives causing concern, anxiety, and depression for the students.[26]
Moreover, depression is a common issue among medical students of Saudi Arabia, we want to review the published literature on the topic at hand and list the associated factors.
Materials and Methods
Our systematic review follows PRISMA guidelines.[27]
Search strategy
We ran a systematic search to identify relevant studies evaluating the prevalence of depression among medical students in Saudi Arabia. The explored databases were PubMed/Medline and Google Scholar. Our search included articles with publication dates from 1/January/2010 till 31/March/2019, only in the English language.
The initial search was performed with the following keywords: depression, medical students, Saudi Arabia. A detailed search strategy [Figure 1]. Reference lists were explored to find more articles relevant to our study.
Figure 1.
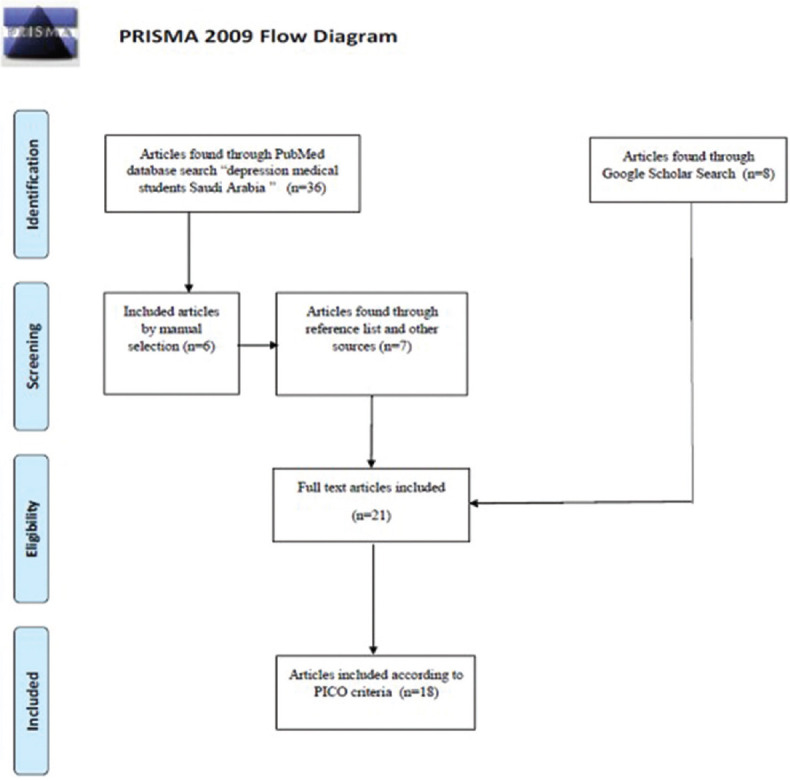
Article search strategy showing inclusion and exclusion of the material used in this literature review
Study selection
As a result of an initial search 36 articles were found. First step was checking titles and abstracts. According to our principles included articles’ titles had to answer our research question. What applies to abstracts, they had to fulfil the PICO criteria which refer to the Population, Intervention, Comparison and Outcomes.[28] The screening of titles and abstracts led to a manual selection of those meeting our criteria. We excluded studies if they included 1) children, adolescents, school students, 2) only non-medical students, 3) implied any other disorder without depression being included in the study (e.g. anxiety, stress, psychological distress, irritable bowel syndrome, and burnout).
We included the following studies, comparison among students of all 5 years and those not being enrolled yet (premedical year students),[29] comparative studies between medical and non-medical students,[30,31] an article applying migraine, tension headache, and depression.[32]
We gathered 21 articles associated with our topic, obtained from the primary search, and thorough investigation of reference lists of the articles fulfilling our criteria. After getting access to full-text articles we excluded three of them containing “depression” in the title but not being correct in terms, as those articles evaluated stress prevalence among medical students but did not implement depression screening.
Data extraction
Data were extracted to and the following features were integrated into the database: number of participants, methods of depression diagnosis, and the prevalence of depression categorized by severity.
Data analysis
Data were analyzed by SPSS-23 software for quantitative assessment.
Results
Characteristics of study participants
Most of the studies included students from all the years, whereas others were focused on certain groups: students from the stage of the basic science, 4th year only or interns only.
Two studies incorporated the only male, two included only females and the remaining articles referred to both genders.
Diagnosis of depression and anxiety
Diagnostic means of depression varied. Five studies used BDI, three preferred PHQ-9 while two performed DASS-21. The Aga Khan University Anxiety and Depression Scale, MHI-38, HADS, PHQ-2, Brief Symptom Inventory-18, and one developed by the researcher himself.[33] The abovementioned questionnaires were used to evaluate the severity of depression but also had additional sections for associated sociodemographic factors, academic level, GPA, smoking, etc.
Depression prevalence and severity evaluation
We approached the articles to assess the prevalence of depressive symptoms and how the severity is distributed among medical students of Saudi Arabia.
Jarwan's study included 136 students from the first three academic years (female-53.7%) at Umm Al-Qura University. The prevalence of depressive symptoms, in general, was 30.9%.[34] Another study by Alakhtar et al. among medical students from the same institution showed a prevalence of depression at 60.5%.[35]
In Al-Faris et al., 797 medical students of King Saud University were screened for depressive symptoms using BDI (74%-male). Numerous students (48.2%) had either mild (20.7%), moderate (16.6%), or severe depressive symptoms (10.9%). Female to male prevalence ratio was 58% vs 45%, respectively.[36]
AbdulAziz et al. evaluated prevalence and levels of neurotic depression among female students at Taibah University and tried to verify the relationship of depressive symptoms to chocolate eating habits. The study included 295-females who were tested by BDI. The distribution was as follows: mild depression 60.3%, moderate-severe 39.7%.[37]
Alshehri et al. studied 50-male medical students from the third academic year in Imam Mohammed Ibn Saud Islamic University. Results of self-administered PHQ-9: minimal depressive symptoms 24%, mild 18%, moderate 8%, moderately severe 2%, and severe 0%.[38]
Alsalameh et al. involved 1171 medical students from 5 regions in KSA, the PHQ-9 questionnaire was used. Females compared to males: minimal depressive symptoms – 24.7% vs 21.2%, moderate depression – 21.1% vs 13.9%, and severe depression – 18.6% vs 16.4%.[39]
Nooli et al. performed a study among 49-male medical interns at King Khalid University via PHQ-9. The prevalence of depression was 77.6%.[40]
Al-Samghan et al. study were performed among 532 students (female-183) of King Khalid University. DASS questionnaire was used and depression was recognized in 52.1%: mild 15.5%, moderate 19.7%, severe 8.4%, and extremely severe 8.4%.[41]
Inam conducted a study among medical students of Qassim University. The study included 288-male and 105-female students from the premedical year and the first three medical years. Students completed the AKUADS survey. The prevalence of anxiety and depression in females and males was 60.6% and 44.4%, respectively (P < 0.05).[20] Prince Sattam Bin Abdulaziz University medical students of all years were screened by Agrawal et al. with DASS-21 showing 39.5% prevalence among the 185 participants.[42]
Reported associated factors influence on depression severity
Within all the found articles, the most comprehensive study focused on factors associated with depression done by Sultan et al. Researchers aimed to show the prevalence of depression and associated factors among all medical students at Taibah University. Depression was screened by the PQ-2 questionnaire. Prevalence of depression was 28.3% (male-31.6% vs female-24.05%). The prevalence of depression was more frequently reported by second and third-year students (33.6% vs 33.1%) wherein single-students depression rate (29.65%) was compared to married-students (10.5%). One meal per day led to a significant prevalence of depression (51.7%). Consuming stimulant drugs indicated higher rates of depression (48.1%). Consuming energy drinks also correlated, the prevalence of depression with this factor: often 32.7%, most of the time 40%, and all the time 100%.
Prevalence of depressive symptoms associated with having neck or back pain (60%), hypertension (55%), bronchial asthma (47.5%), and anemia (42.7%). Depressive symptoms were present in those who spent more than 2 h in bed before sleeping (75%), used sleep medication (66.7%), slept less than 5 h a day (31.4%), and less than 3 h the night before examinations (43.7%).[43]
AbdulAziz et al. in their study reported a significant difference for depressed female participants consuming chocolate. Chocolate was assumed to have a positive effect on depression based on the amount consumed.[37]
Asiri et al. in their 2017 study included male students from all the years except the first year in Najran University to identify depression, anxiety, and stress among the students. Prevalence, in general, was 59.3%.[44]
A study by Ibrahim et al. among 450 medical students of King Abdulaziz University from 2010–2011. Hospital Anxiety and Depression Scale (HADS) questionnaire was used and showed a mean score of 6.59 ± 3.62 for depression. The study focused on comorbidity between depression and anxiety and led to a positive correlation (P < 0.001).[45]
Alharbi et al. used the PHQ-9 questionnaire in their study. The study included 2562 medical students from 20 medical universities (female-61.4%). Depression was seen in 83.4% of participants due to them scoring exceeding 4. 87.6% female and 66.6% male students had various levels of depression.[31]
A study by Desouky et al. was performed at Taif University engaging 1340 female students from 2016–2017. The study focused on the association between depression and migraine, tension-type headache. Beck Depression Inventory (BDI), ID-Migraine™ questionnaire and criteria of Hospital Anxiety and Depression Scale International Headache Society (IHS) were applied. Prevalence was significantly higher among students suffering from migraines. Medical students showed higher rates of headaches.[32]
Prevalence compared to other university students
Two studies were found to compare prevalence between medical vs non-medical students of Saudi Arabia.
Alzahrani's study included fourth-year students at Taif University. Around 81 medical students and 100 medical sciences students were included in this study. Prevalence was evaluated by a new inventory developed by the researcher himself. Overall prevalence was 34%, medical students and medical sciences students had a prevalence of 41% vs 28%, respectively.[33]
A study by Alkot et al. aimed to compare medical and non-medical students’ depression rates at Umm Al-Qura University. The study included both male and female students which are distributed from the College of Medicine, 103-male vs 77-female; College of Islamic Studies, 107-male vs 70-female; and College of Engineering and Islamic Architecture which only had 95-male students. Depression rates among all students: mild mood disturbance 29.7%, borderline 29.7%, evident depression among males 31.2% including – borderline clinical depression 11.8%, moderate 13.2%, severe 4.9%, extremely severe 1.3% while among females 26.4% including - borderline clinical depression 11.5%, moderate 12.8%, severe 1.4%, extremely severe 0.7%. There was a high rate of depression among the College of Medicine and College of Engineering and Islamic Architecture 34.5% and 34.8%, respectively, while the college of Islamic studies is 22.7%.[30]
Discussion
Summary of evidence
Our review included the minimal quantity of participants which was 49, and the maximum was 2562. We counted 8839 participants. The mean prevalence of depression based on data from literature was 51.46% (SD = 16.38%) with a minimum prevalence of 30.9% and a maximum of 77.6%.
To evaluate the severity of depression among medical students, we concluded to unify the data in the following way: minimal depressive symptoms and mild depression were summarized as “mild,” whereas moderate, moderate severity, and severe severity were summarized as “moderate-to-severe.” Thus, we got two categories which helped us to estimate the severity of depression more precisely. For mild depression we got mean value 29.9% (SD = 14.83%) and for moderate-to-severe depression 33.27% (SD = 16.95%).
It was difficult to estimate depression distribution among males and females as not every study evaluated prevalence in these groups. Yet some studies show that females are more prone to be having depression as opposed to males.[30,31,34,43]
Two studies described each state of severity with the male-to-female ratio. Results showed the following distribution: mild-20.5% vs 15.9%, moderate-11% vs 7.9%, and severe-2.7% vs 3.2%,[34] while in another study we had the following: mild-24.7% vs 21.2%, moderate-21.1% vs 13.9%, and severe-18.6% vs 16.4%.[39]
The correlation between the academic year and depression severity, a significant difference was found for the first year compared to others. It was reported in several articles that first-year students are at the highest risk of developing depressive symptoms.[34,36] Stress level is significantly lower in 4th-year students.[42] There was a study using the DASS-21 questionnaire that high rates were seen in the third year.[44]
Many studies were focused on Grade Point Average (GPA). Nuqali et al. conducted a study among 219 students (males-54.3%) from all years at Umm Al-Qura University. The study used a self-administered MHI-38 questionnaire providing participants with both English and validated Arabic versions. Researchers avoided administering the questionnaire at stressful periods to avoid false-positive responses. The mean MHI-38 depression score was 15.11 indicating moderate depression state. Male participants had higher MHI-38 scores of depression, yet no significant difference was found between genders in terms of GPA. The distress level was equal among medical students in all academic years. The less depressed the students were, the higher their GPA. Among the associated factors students mentioned academic-related stressors, however, family and relationship issues were the least reported ones.[46] Two studies showed that low academic performance students are more likely to develop depression.[34,45] Alakhtar et al. showed that GPA indicated a higher rate of depression among students with high and low GPA while having an intermediate GPA had lower rates.[35]
No significant difference was found for smoking and depression, it was mentioned that the difference between smokers and ex-smokers was 7%, whereas ex-smokers compared to the non-smoking participants showed a difference of 2%.[31] Smokers had a higher level of stress in comparison to non-smokers,[42] Moreover, smoking cigarettes, moassil, and shisha was associated with a significant risk of having depressive symptoms.[34] A significant correlation was found in smokers associated with depression severity: mild 38.4%, moderate 15.3%, and severe 7.6%.[40]
Living alone was indicated as a predisposing factor.[31] Single students had higher depression rates compared to married students (29.65% vs 10.5%).[31,37] There is also a report of married females having higher depression rates than single students (28.6% vs13.7%, P < 0.05). Non-Saudi nationality was also reported to be a predictor for depression.[45]
A study on self-reported usage of stimulant drugs and energetic drinks by Sultan et al. indicated higher rates of depression. Depression was found to be associated with comorbidities such as neck or back pain, hypertension, bronchial asthma, and anemia. Sleep disturbances were included not consistent with sleep hygiene, sleep deprivation, sleep medication usage were important influencing factors.[43]
Limitations
There is a huge need for epidemiological and scientific researches to be performed for a better understanding of depressive disorders prevalence.
As some studies did not see any difference in distress and depression, others conceived depression as a universal term without being introduced into the classification and differentiation of clinical forms of depressive disorders.[6]
Not all the studies were performed by a qualified mental health specialist. Most of the studies were held by students, moreover, the questionnaires were self-administered which means there was no interaction between participant and professional, therefore necessary clarifications were not made when needed. This kind of approach increases the potential for false-positive results.
Another limitation was study design, in some cases which did not collect a sample large enough, so the epidemiological material may not be consistent with the results.
Practical recommendations
To raise awareness for depression among medical students, it is recommended to deliver lectures. Medical students should be seen by psychiatrists in the college or screened by family physicians, mentorship should be implemented to assist them through it. The main issue is many medical students with depression remain underdiagnosed.[47]
Conclusions
Depression is a widely spread condition among medical students and as seen in our systemic review it is relatively high, which requires special attention to its epidemiological status verification, assessment of already proven influencing factors, and targeted research aimed towards supporting future healthcare professionals to provide a better healthcare service and to have a stable psychological state.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We would like to thank and show our gratitude to Dr. Hamad Abdulrahman Algaeed for sharing their pearls of wisdom with us and for the endless support during the course of writing this article.
References
- 1.UN Office of the High Commissioner for Human Rights (OHCHR), Fact Sheet No. 31, The Right to Health, June 2008, No. 31. Available from: https://www.refworld.org/docid/48625a742.html .
- 2.World Health Organization. Depression Fact sheet 369. 2012. Available form: https://wwwwhoint/mental_health/management/depression/who_paper_depression_wfmh_2012pdf .
- 3.Depression and Other Common Mental Disorders: Global Health Estimates. Geneva: World Health Organization; 2017. Licence: CC BY-NC-SA 3. Available form: https://apps.who.int/iris/bitstream/handle/10665/254610/WHO-MSD-MER-2017.2-eng.pdf . [Google Scholar]
- 4.GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1545–602. doi: 10.1016/S0140-6736(16)31678-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. The World Health Report: 2001: Mental Health: New Understanding. New Hope World Health Organization; 2001. Available form: https://appswhoint/iris/handle/10665/42390 . [Google Scholar]
- 6.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: Author; Available form: https://doiorg/101176/appibooks 9780890425596 . [Google Scholar]
- 7.Lauber C, Falcato L, Nordt C, Rössler W. Lay beliefs about causes of depression. Acta Psychiatr Scand. 2003;108(Suppl 418):96–9. doi: 10.1034/j.1600-0447.108.s418.19.x. [DOI] [PubMed] [Google Scholar]
- 8.Kanter JW, Busch AM, Weeks CE, Landes SJ. The nature of clinical depression: Symptoms, syndromes, and behavior analysis. Behav Anal. 2008;31:1–21. doi: 10.1007/BF03392158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ng CW, How CH, Ng YP. Major depression in primary care: Making the diagnosis. Singapore Med J. 2016;57:591–7. doi: 10.11622/smedj.2016174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chand SP, Arif H. StatPearls [Internet] Treasure Island (FL): StatPearls Publishing; 2020. Depression [Updated 2019 Aug 3] Available from: https://wwwncbinlmnihgov/books/NBK430847/ [Google Scholar]
- 11.Hasler G. Pathophysiology of depression: Do we have any solid evidence of interest to clinicians? World Psychiatry. 2010;9:155–61. doi: 10.1002/j.2051-5545.2010.tb00298.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Williams SZ, Chung GS, Muennig PA. Undiagnosed depression: A community diagnosis. SSM-Population Health. 2017;3:633–8. doi: 10.1016/j.ssmph.2017.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang C, Cramer KM, Cheng H, Do KA. Associations between depression literacy and help-seeking behavior for mental health services among high school students. School Ment Health. 2019;11:707–18. [Google Scholar]
- 14.Amarasuriya SD, Jorm AF, Reavley NJ, Mackinnon AJ. Stigmatising attitudes of undergraduates towards their peers with depression: A cross-sectional study in Sri Lanka. BMC Psychiatry. 2015;15:129. doi: 10.1186/s12888-015-0523-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kroenke K, Spitzer R. The PHQ-9: A new depression diagnostic and severity measure. Psychiatr Ann. 2002;32:509–15. [Google Scholar]
- 16.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arc Gen Psychiatry. 1961;4:561–71. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 17.Lovibond SH, Lovibond PF. Manual for the Depression Anxiety Stress Scales. 2nd ed. Sydney: Psychology Foundation; 1995. [Google Scholar]
- 18.Veit CT, Ware JE. The structure of psychological distress and well-being in general populations. J Consult Clin Psychol. 1983;51:730–42. doi: 10.1037//0022-006x.51.5.730. [DOI] [PubMed] [Google Scholar]
- 19.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 20.Eisenberg D, Hunt J, Speer N. Mental health in American colleges and universities: Variation across student. J Nerv Ment Dis. 2013;201:60–7. doi: 10.1097/NMD.0b013e31827ab077. [DOI] [PubMed] [Google Scholar]
- 21.WHO. Investing in Mental Health. Geneva: World Health Organization (WHO); 2003. Available from: https://wwwwhoint/mental_health/media/investing_mnhpdf . [Google Scholar]
- 22.Quek TT, Tam WW, Tran BX, Zhang M, Zhang Z, Ho CS, et al. The global prevalence of anxiety among medical students: A meta-analysis. Int J Environ Res Public Health. 2019;16:2735. doi: 10.3390/ijerph16152735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moir F, Yielder J, Sanson J, Chen Y. Depression in medical students: Current insights. Adv Med Educ Pract. 2018;9:323–33. doi: 10.2147/AMEP.S137384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dyrbye LN, Thomas MR, Shanafelt TD. Systematic review of depression, anxiety, and other indicators of psychological distress among US and Canadian medical students. Acad Med. 2006;81:354–73. doi: 10.1097/00001888-200604000-00009. [DOI] [PubMed] [Google Scholar]
- 25.Telmesani A, Zaini R, Ghazi H. Medical education in Saudi Arabia: A review of recent developments and future challenges. East Mediterr Health J. 2011;17:703–7. [PubMed] [Google Scholar]
- 26.Hill MR, Goicochea S, Merlo LJ. In their own words: Stressors facing medical students in the millennial generation. Med Educ Online. 2018;23:1530558. doi: 10.1080/10872981.2018.1530558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Moher D, Liberati A, Tetzlaff J, Altman DG The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ. 2009;339:2535. [PMC free article] [PubMed] [Google Scholar]
- 28.Huang X, Lin J, Demner-Fushman D. Evaluation of PICO as a knowledge representation for clinical questions. AMIA Annu Symp Proc. 2006;2006:359–63. [PMC free article] [PubMed] [Google Scholar]
- 29.Inam SB. Anxiety and depression among students of a medical college in Saudi Arabia. Int J Health Sci. 2007;1:295–300. [PMC free article] [PubMed] [Google Scholar]
- 30.Alkot M, Alnewirah A, Bagasi A, Alshehri A, Bawazeer N. Depression among medical versus non-medical students in Umm Al-Qura University, Makkah Al-Mukaramah, Saudi Arabia. Am J Psychiatry Neurosci. 2017;5:1–5. [Google Scholar]
- 31.Alharbi H, Almalki A, Alabdan F, Haddad B. Depression among medical students in Saudi medical colleges: A cross-sectional study. Adv Med Educ Pract. 2018;9:887–91. doi: 10.2147/AMEP.S182960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Desouky D, Zaid H, Taha A. Migraine, tension-type headache, and depression among Saudi female students in Taif University. J Egypt Public Health Assoc. 2019;94:7. doi: 10.1186/s42506-019-0008-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Alzahrani A. Depression and suicide among medical students: A comparison study between medical and medical sciences students in Taif University. Taif-KSA Int J Med Sci Public Health. 2017. p. 6. Available from: https://wwwejmanagercom/mnstemps/67/67-1473238873pdft=1562158091 .
- 34.Jarwan BK. Depression among medical students of Faculty of Medicine, Umm Al-Qura University in Makkah, Saudi Arabia. Int J Med Sci Public Health. 2015;4(2):184–191. doi:10.5455/ijmsph.2015.0911201436. [Google Scholar]
- 35.Alakhtar AM, Al-Homaidan HT. Depression among medical students at qassim university rate, severity, and contributing factors; using BDI II. Int J Dev Res. 2014;4:1768–72. [Google Scholar]
- 36.Al-Faris EA, Irfan F, Van Der Vleuten CPM, Naeem N, Alsalem A, Alamiri N, et al. The prevalence and correlates of depressive symptoms from an Arabian setting: A wake up call. Med Teach. 2012;34:S32–6. doi: 10.3109/0142159X.2012.656755. [DOI] [PubMed] [Google Scholar]
- 37.Abdul Aziz A, Al-Muwallad N, Al-Muwallad A, Mansour O, Mansour A. Neurotic depression and chocolate among female medical students at College of Medicine, Taibah University Almadinah Almunawwarah, Kingdom of Saudi Arabia. J Taibah Univ Med Sci. 2011;6:139–47. [Google Scholar]
- 38.Alshehri A, Alaskar F, Albahili F. Stress, depression and anxiety among medical students of Imam Mohammed Ibn Saud Islamic University, KSA. Egypt J Hosp Med. 2018;70:869–71. [Google Scholar]
- 39.Alsalameh N, Alkhalifah A, Alkhaldi N, Alkulaib A. Depression among medical students in Saudi Arabia. Egypt J Hosp Med. 2017;68:974–81. [Google Scholar]
- 40.Nooli A, Asiri A, Asiri A, Alqarni M, Alhilali F, Alayafi M, et al. Prevalence of depression among medical interns in King Khalid University. Int J Med Res Prof. 2017;3:131–3. [Google Scholar]
- 41.Al-Samghan AS, Al-Musa HM, Alqahtani NA, Alqahtani AM, Alqahtani KA, Alfatah HS, et al. Depression, Anxiety and Stress Disorders Among Medical Students in King Khalid University, Saudia Arabia. PJSR. 2016;9:1–5. [Google Scholar]
- 42.Agrawal S, Aleid M, Alotaibi R, Alwusaybie M, Almousa O, Aldalbahi HM, et al. Prevalence of depression, anxiety and stress among the undergraduate medical students of Prince Sattam Bin Abdulaziz University, Alkharj, Saudi Arabia. Int J Adv Res. 2017;5:1456–63. [Google Scholar]
- 43.Sultan SA, Alhosaini AA, Sheerah SA, Alrohaily AA, Saeed HM, Al-Raddadi NM, et al. Prevalence of depression among medical students at Taibah University, Madinah, Saudi Arabia. Int J Acad Sci Res. 2016;4:93–102. Available from: https://pdfssemanticscholarorg/1553/49b90e7bdccd20b65ef9715d1754af6c7052pdf . [Google Scholar]
- 44.Asiri S, Asiri A, Ulahannan S, Alshiek M. Prevalence of depression, anxiety and stress among male medical students at Najran University, Saudi Arabia. Int J Med Health Res. 2018;4:94–9. [Google Scholar]
- 45.Ibrahim N, Al-Kharboush D, El-Khatib L, Al-Habib A, Asali D. Prevalence and predictors of anxiety and depression among female medical students in King Abdulaziz University, Jeddah, Saudi Arabia. Iran J Public Health. 2013;42:726–36. [PMC free article] [PubMed] [Google Scholar]
- 46.Nuqali A, Al Nazzawi H, Felmban S, Assiri H, Felemban N. (2018) Assessing the Correlation between Medical Students’ Psychological Distress and Their Academic Performance in Makkah. Saudi Arabia Creative Education. 9:1332–1341. doi: 104236/ce201899099. [Google Scholar]
- 47.Tjia J, Givens JL, Shea JA. Factors associated with undertreatment of medical student depression. J Am Coll Health. 2005;53:219–24. doi: 10.3200/JACH.53.5.219-224. [DOI] [PubMed] [Google Scholar]


