Abstract
Background
In response to the coronavirus disease 2019 (COVID-19) pandemic, the Centers for Medicare and Medicaid Services pledged payment for telehealth visits for the duration of this public health emergency in an effort to decrease COVID-19 transmission and allow for deployment of residents and attending physicians to support critical-care services. Although the COVID-19 pandemic has vastly expanded telehealth use, no studies to our knowledge have analyzed the implementation and success of telehealth for orthopaedic trauma. This population is unique in that patients who have experienced orthopaedic trauma range in age from early childhood to late adulthood, they vary across the socioeconomic spectrum, may need to undergo emergent or urgent surgery, often have impaired mobility, and, historically, do not always follow-up consistently with healthcare providers.
Questions/purposes
(1) To what extent did telehealth usage increase for an outpatient orthopaedic trauma clinic at a Level 1 trauma center from the month before the COVID-19 stay-at-home order compared with the month immediately following the order? (2) What is the proportion of no-show visits before and after the implementation of telehealth?
Methods
After nonurgent clinic visits were postponed, telehealth visits were offered to all patients due to the COVID-19 stay-at-home order. Patients with internet access who had the ability to download the MyChart application on their mobile device and agreed to a telehealth visit were seen virtually between March 16, 2020 and April 10, 2020 (COVID-19) by three attending orthopaedic trauma surgeons at a large, urban, Level 1 trauma center. Clinic schedules and patient charts were reviewed to determine clinical volumes and no-show proportions. The COVID-19 period was compared with the 4 weeks before March 16, 2020 (pre-COVID-19), when all visits were conducted in-person. The overall clinic volume decreased from 340 to 233 (31%) between the two periods. The median (range) age of telehealth patients was 46 years (20 to 89). Eighty-four percent (72 of 86) of telehealth visits were postoperative and established nonoperative patient visits, and 16% (14 of 86) were new-patient visits. To avoid in-person suture or staple removal, patients seen for their 2-week postoperative visit had either absorbable closures, staples, or nonabsorbable sutures removed by a home health registered nurse or skilled nursing facility registered nurse. If radiographs were indicated, they were obtained at outside facilities or our institution before patients returned home for their telehealth visit.
Results
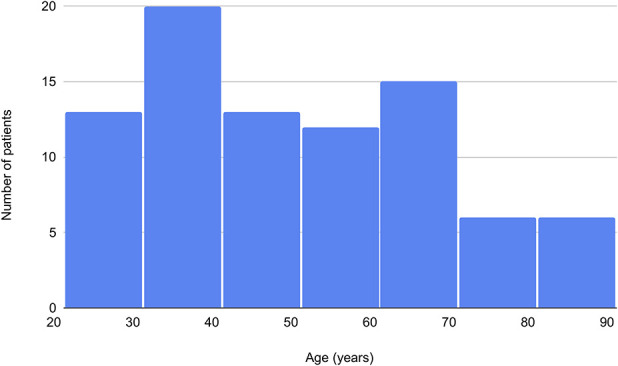
There was an increase in the percentage of office visits conducted via telehealth between the pre-COVID-19 and COVID-19 periods (0% [0 of 340] versus 37% [86 of 233]; p < 0.001), and by the third week of implementation, telehealth comprised approximately half of all clinic visits (57%; [30 of 53]). There was no difference in the no-show proportion between the two periods (13% [53 of 393] for the pre-COVID-19 period and 14% [37 of 270] for the COVID-19 period; p = 0.91).
Conclusions
Clinicians should consider implementing telehealth strategies to provide high-quality care for patients and protect the workforce during a pandemic. In a previously telehealth-naïve clinic, we show successful implementation of telehealth for a diverse orthopaedic trauma population that historically has issues with mobility and follow-up. Our strategies include postponing long-term follow-up visits, having sutures or staples removed by a home health or skilled nursing facility registered nurse, having patients obtain pertinent imaging before the visit, and ensuring that patients have access to mobile devices and internet connectivity. Future studies should evaluate the incidence of missed infections or stiffness as a result of telehealth, analyze the subset of patients who may be more vulnerable to no-shows or technological failures, and conduct patient surveys to determine the factors that contribute to patient preferences for or against the use of telehealth.
Level of Evidence
Level III, therapeutic study.
Introduction
In response to the coronavirus disease 2019 (COVID-19) pandemic, the Centers for Disease Control recommended exploring alternatives to face-to-face visits [4], and the Centers for Medicare and Medicaid Services pledged payment for telehealth visits in broader circumstances throughout the COVID-19 public health emergency [5]. These measures aimed to decrease COVID-19 transmissions and potentially allow for deployment of residents and attending physicians to support critical care services. With the California stay-at-home order on March 19, 2020, providers across all specialties at our institution responded with various strategies, including implementing telehealth clinic visits and delaying nonurgent in-person patient encounters, leading to decreased hospital traffic, personal protective equipment consumption, and face-to-face interactions.
Although prompted by a pandemic, substituting telehealth visits for in-person orthopaedic surgery encounters is not a novel idea. Studies within orthopaedics have found favorable cost benefits of telehealth specifically for new oncology patients, and that telehealth substitutes adequately for clinic encounters even when ROM examination is necessary [1, 6]. A survey of institutions participating in the Electronic Residency Application Service revealed a 63% proportion of telehealth use with an additional 23% of facilities in the process of establishing telehealth capabilities [11]. Some orthopaedic trauma surgeons have also made changes to their typical protocols to eliminate the need for early postoperative follow-up, including using absorbable suture for closing wounds or discharging patients home with suture removal kits [12].
A good clinical strategy during the COVID-19 pandemic and for future crises decreases face-to-face interaction between the patient and provider as well as community exposure, and minimizes necessary clinic personnel without compromising patient outcomes. The COVID-19 pandemic has vastly expanded telehealth use in a variety of specialties, including colorectal cancer, urology, and vascular surgery [2, 3, 8]. In addition, several online-based platforms have made remote appointments and consultations more feasible worldwide [7, 13]. However, to our knowledge no prior studies have analyzed the implementation of telehealth in orthopaedic trauma care, which is unique in that this population encompasses all ages and socioeconomic statuses, its associated diagnoses do not provide the convenience of delay as in elective surgery, the patients often have impaired mobility, and in many prior studies patient follow-up has been inconsistent. Therefore, in this study we evaluated the implementation and highlight the benefits and drawbacks of changing clinic structure at a Level 1 orthopaedic trauma center during the COVID-19 pandemic that can be used for future crises.
We therefore asked: (1) To what extent did telehealth usage increase for an outpatient orthopaedic trauma clinic at a Level 1 trauma center from the month before the COVID-19 stay-at-home order compared with the month immediately following the order? (2) What is the proportion of no-show visits before and after the implementation of telehealth?
Patients and Methods
Study Design and Setting
This was a retrospective study comparing clinic volume for the period before the stay-at-home order (February 17, 2020 to March 15, 2020; pre-COVID-19 period) to the month immediately following it (March 16, 2020 to April 10, 2020; COVID-19 period) at UC San Diego Health, a large, urban, Level 1 trauma center in San Diego, CA, USA. At the strong recommendation of our hospital system and the Orthopaedic Trauma Association, our orthopaedic trauma department discontinued nonessential surgery and clinic visits starting on March 16, 2020. The determination of nonessential was subject to the attending surgeon’s discretion, but generally included established patients greater than 4 weeks from injury or surgery with no specific concern for wound or fracture healing complications.
Participants
Nonurgent clinic visits, which were defined as long-term follow-up visits without concern for wound healing, nonunion, or where advancement of weightbearing status was not pending radiographs were postponed until the next necessary follow-up. Telehealth visits were offered for all postoperative, established, and new patients during the COVID-19 period to reduce in-person patient encounters. One week before scheduled postoperative and established patient appointments and 1 day to 2 days before new patient clinic visits, clinic medical assistants called patients to discuss converting to a telehealth visit. Patients were required to have a mobile device capable of downloading the telehealth MyChart application and internet access for participating in the virtual visit. The medical assistants instructed patients to obtain imaging before their visit when indicated. Non-English speaking patients were also offered telehealth visits, with a translator present via video streaming or telephone and physical exam performed on video. Patients without technological capabilities or who declined a virtual visit maintained their original appointments. Patients with traumatic wounds from an open injury were also offered a telehealth visit but were recommended to come in person for wound healing surveillance purposes.
All patients who participated in an office visit, whether virtual or in person, were included in the study. Patients who were no shows were recorded as such. Our control period was the pre-COVID-19 period, 4 weeks before March 16, 2020, during which all visits were conducted in person. Following this time, clinic volumes for postoperative, established, and new patients decreased. The change in clinic volumes for three attending orthopaedic trauma surgeons (PJG, AKS, WTK) was collected using our institution’s electronic health record and compared with clinic volumes during the 4 weeks before March 16, 2020 (pre-COVID-19 period). The overall clinic volume decreased 31% (from 340 to 233) when comparing pre-COVID-19 to COVID-19 (Table 1).
Table 1.
A comparison of clinic structure before and after the implementation of telehealth
| Clinic characteristics | Pre-COVID-19: February 17, 2020 to March 13, 2020 (n = 340) |
COVID-19: March 16, 2020 to April 10, 2020 (n = 233) |
p value |
| Telehealth visits | 0% (0) | 37% (86) | < 0.001a |
| In-person visits | 100% (340) | 63% (147) | |
| No-show proportion | 13% | 13% | 0.91 |
=statistically significant.
Description of Experiment, Treatment, or Surgery
To avoid in-person suture or staple removal, patients seen for their 2-week postoperative visit had either absorbable monocryl closures or staples or nonabsorbable sutures removed by a home health registered nurse or skilled nursing facility resident nurse. If radiographs were indicated, they were obtained at outside facilities or at our institution before the patients scheduled telehealth visit.
On the day of the telehealth visit, the patient would log onto their medical MyChart application on their mobile device, and the provider would receive a notification that the patient was ready for their 20-minute virtual visit. The provider would then log on and conduct the video visit. After the history was obtained, patients were instructed to show their incision on the video and perform their maximum ROM. Patients with poorly healing incisions were instructed to come for an in-person appointment, and those with poor ROM were considered for earlier physical therapy. Sensation and vascular exam were not a routine part of the telehealth appointment. Once the visit was completed, the medical assistant would schedule the next appointment with the patient via the MyChart application.
Aftercare
Postoperative care in the COVID-19 cohort did not deviate from normal care. In both scenarios, patients were seen at 2 and 6 weeks postoperatively. For most patients, sutures were removed at 2 weeks and imaging was obtained at 6 weeks. Postoperative ROM, weightbearing, and physical therapy protocols remained unchanged.
Variables, Outcome Measures, Data Sources, and Bias
Clinic visits were recorded as either in-person, video telehealth, or telephone encounters. Patients who did not cancel more than 24 hours in advance of the visit were designated as no shows, which is consistent with our clinic policy.
Our primary study outcome was to quantify the increased use of telehealth visits for outpatient orthopaedic trauma clinics during stay-at-home orders. We compared in-person versus telehealth clinic visits of our three orthopaedic trauma attendings (PJG, AKS, WTK) during the first 4 weeks of stay-at-home to the 4 weeks immediately preceding the stay-at-home order.
Our secondary study outcome was to quantify the proportion of no-show clinic visits during telehealth implementation compared with in-person visits before stay-at-home orders. We again compared the patient no-shows from the first 4 weeks of stay-at-home orders to the preceding 4 weeks.
Demographics, Description of Study Population
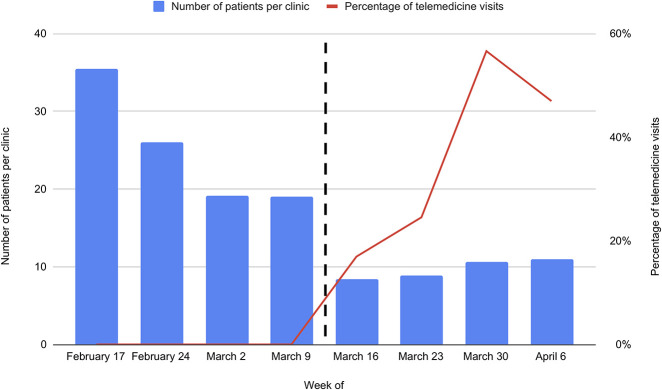
The median (range) age of telehealth patients was 46 years (20 to 89) (Fig. 1). Forty-eight percent (41 of 86) of patients were men.
Fig. 1.
This graph shows the age distribution of patients seen via telehealth. Patients of all ages were amenable to telehealth, and in our study, their ages ranged from 20 years to 89 years.
Accounting for all Patients
We included all clinic patients during the 8-week period. This totaled 573 patient encounters: 487 in-person visits and 86 telehealth appointments. No clinic visits were excluded. Because this study evaluated the implementation of a novel system, patient clinical outcomes were not analyzed.
Statistical Analysis, Study Size
We used IBM SPSS Statistics for Macintosh, Version 26.0 (IBM Corp, Armonk, NY, USA), for all statistical analyses, with alpha set at 0.05 to declare statistical significance. We used a chi-square test to analyze the no-show proportions pre-COVID-19 and COVID-19. Fisher’s exact test was used to compare the percentage of telehealth visits between the two time periods, given the low incidence of this type of visit in the pre-COVID-19 period.
Results
Change in Telehealth Usage
The proportion of visits conducted under telehealth increased during the first month of the COVID-19 stay-at-home order (0% [0 of 340] versus 37% [86 of 233]; p < 0.001). By the third week of implementation, approximately half of all clinic visits were conducted using telehealth (57% [30 of 53]). Eighty-four percent (72 of 86) of telehealth visits were postoperative and established nonoperative patient visits, and 16% (14 of 86) were new-patient visits (Fig. 2).
Fig. 2.
This graph shows changes in clinic volume and structure during the COVID-19 pandemic. There was an overall decrease in the number of patients per clinic, as well as an increase in the percentage of visits that were conducted virtually via telehealth.
Did the Proportion of No-show Visits Increase with Telehealth?
There was no difference in the no-show proportion between the two periods (13% [53 of 393] for the pre-COVID-19 period and 14% [37 of 270] for the COVID-19 period; p = 0.91). One telehealth visit (1% [1 of 86]) had to be cancelled during the study period because of problems with connectivity.
Discussion
As of this writing, the United States has reported more patients with COVID-19 than any other country, and the numbers continue to rise [9]. Given the severity of the global pandemic, it is of utmost importance to minimize in-person patient interactions with hospital systems and promote social distancing. In this study, we offered a viable alternative for a Level 1 trauma center’s orthopaedic trauma clinic that can be used by clinics throughout the United States to deliver high-quality care for a trauma population that encompasses all ages and socioeconomic statuses, a population that often must undergo time-sensitive surgery, typically has impaired mobility, and historically does not consistently follow-up with healthcare providers. After postponing nonurgent clinic visits to reduce volume, many remaining office visits can be conducted via telehealth, with sutures or staples removed by a home health or skilled nursing facility registered nurse and imaging obtained before the visit. In our experience, postoperative and new patients of all ages were amenable to telehealth without changes in no-show proportions. Furthermore, decreasing the clinic volume allows for the deployment of essential healthcare workers to other settings to care for patients with COVID-19. By improving outpatient care, we can not only decrease patient exposure to COVID-19 but also contribute to the workforce during this time of need.
Limitations
This study had several limitations. First, this study lacked data on long-term outcomes to evaluate whether conversion to telehealth led to additional adverse outcomes, such as early surgical-site infections that could have been better evaluated during an in-person visit. In some instances, video quality for a telehealth visit is not adequate to see the surgical site and detect an early surgical-site infection. To address this concern, we offer two solutions. First, in contrast to Stinner et al. [12], who suggested giving patients suture or staple removal kits along with links to instructional videos, we worked with home health agencies to have a registered nurse conduct an in-home visit, examine the surgical site, and, if ready, remove the sutures or staples. Admittedly, the number needed to treat with a home health registered nurse to prevent one surgical-site infection may be high. However, by going this route, we hoped to reduce the increased patient morbidity associated with a surgical-site infection. Second, we suggest that patients send photographs of their surgical wound to their provider before the clinic appointment. This would allow providers to review surgical sites for the upcoming clinic visit and convert the telehealth visit to an in-person appointment if any of the photographs show anything that is concerning. Although we understand that not having a surgeon evaluate the patient in person may lead to missed infections, further studies are needed to determine how often telehealth-related complications might occur.
A second limitation is the inability to perform a full physical exam via telehealth. During the video visit, we performed wound checks and ROM exams but were unable to perform detailed neurological or vascular exams. Infection and stiffness are two crucial findings of the physical exam for orthopaedic trauma and are able to be detected well via telehealth, as they do not require the use of special maneuvers that other specialties employ, such as a sports surgeon’s use of the Lachman test, or a spine surgeon’s use of Hoffman’s sign. Despite these shortcomings of the physical exam via telehealth, we believe the benefits of minimizing in-person encounters during a pandemic outweigh the risks of an unstudied complication profile. As other institutions implement telehealth, we encourage keeping these limitations in mind.
Third, to our knowledge, there is a lack of data for orthopaedic trauma telehealth; consequently, there are currently no accepted “best practices.” As the evidence improves from institution-reported telehealth experiences stemming from the COVID-19 pandemic, we will be better equipped to establish standards of care. In this study, we present our methods of introducing telehealth within a previously telehealth-naïve institution and have proven its feasibility. We believe best practices should include the following: all patients should be called days before their appointment, be offered the option of telehealth, be instructed to obtain imaging where applicable, and be dvised about the the risks and benefits of telehealth via informed consent.
Change in Telehealth Usage
Our study found that approximately half of orthopaedic trauma clinic visits can be conducted via telehealth, 2 weeks after introducing these structural changes. The reduced volume and rise in telehealth visits not only reduced the sheer number of encounters between patients and the high-risk clinical environment, but it also had downstream effects of reducing asymptomatic spread and augmenting the COVID-19 workforce by repurposing orthopaedic residents. Our findings were similar to that of Loeb et al. [10], who found that providers estimated that roughly one-third of patients would be suitable for telehealth visits, and they anticipated seeing one-fourth of their normal clinic volume, or one-half of the reduced clinic volume, remotely. Almost two-thirds of Electronic Residency Application Service-participating orthopaedic institutions are providing telehealth services, of which 83% implemented these services because of the COVID-19 pandemic [11]. Thus, despite the absence of data to our knowledge, we imagine other institutions will be able to reproduce similar proportions of virtual visits, even in the more tenuous trauma population. Many unanswered questions remain regarding telehealth in the orthopaedic population, and we hope that future studies will explore these. First, as mentioned, the inability to perform a full physical exam increases the risk of missed diagnoses, and a long-term follow-up study would help determine the incidence of missed complications as a result of telehealth. In addition, an analysis of which patients were more susceptible to complications, no shows, or technological failures can give insight into the more vulnerable populations that may benefit from an in-person visit.
Did the Proportion of No-show Visits Increase with Telehealth?
We found no difference in no-show proportions before and after the introduction of telehealth. The cumulative time saved by conducting visits virtually provides patients with more time with their families and less time away from work. Anecdotally, we were pleasantly surprised to see that patients living with housing insecurity were able to conduct telehealth visits, which may help them, as they sometimes have difficulty garnering resources to travel to in-person visits. These patients were subject to the same minimum requirements of a mobile device and internet connectivity, which many were able to gain from public WiFi networks. In addition, we successfully conducted virtual visits with patients whose ages ranged from 20 to 89 years, with a relatively even distribution across all ages (Fig. 1), sugesting the wide applicability of telehealth for patients who have experienced orthopaedic trauma. Patients may currently be more amenable to telehealth clinic visits given the pandemic climate to promote social distancing and reduce the number of times they interact with the clinic setting. However, they may not have the same enthusiasm once stay-at-home orders are relaxed and social distancing requirements are eased. Thus, future studies may conduct patient surveys to determine what personal, medical, or socioeconomic factors contribute to a patient’s preference for or against telehealth.
Conclusions
In an orthopaedic trauma population, we found that approximately half of clinic visits can be conducted virtually within 2 weeks of introducing telehealth to a previously telehealth-naïve system. We also found no difference in no-show proportions before and after the introduction of telehealth. Clinicians might consider implementing similar telehealth strategies to reduce in-person patient-provider interactions if a resurgence of COVID-19 cases were to arise, even in this high-risk population. These strategies include postponing long-term follow-up visits, having sutures or staples removed by a home health or skilled nursing facility registered nurse, having patients obtain pertinent imaging before the visit, and ensuring that patients have access to mobile devices and internet connectivity. Future studies should evaluate the incidence of missed infections or stiffness as a result of telehealth, analyze the subset of patients who may be more vulnerable to no shows or technological failures, and conduct patient surveys to determine the factors that contribute to patient preferences for or against the use of telehealth.
Footnotes
Each author certifies that he or she has no commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Aponte-Tinao L, Farfalli G, Albergo J, Plazzotta F, Sommer J, Luna D, de Quirós F. Face to Face Appointment vs. Telehealth in First Time Appointment Orthopedic Oncology Patients: A Cost Analysis. Stud Health Technol Inform. 2019;264:512-515. [DOI] [PubMed] [Google Scholar]
- 2.Barsom EZ, Jansen M, Tanis PJ, van de Ven AW, van Oud-Alblas MB, Buskens CJ, Bemelman WA, Schijven MP. Video consultation during follow up care: effect on quality of care and patient-and provider attitude in patients with colorectal cancer. Surg Endosc. [Published online ahead of print March 20, 2020]. DOI: 10.1007/s00464-020-07499-3. [DOI] [PMC free article] [PubMed]
- 3.Borchert A, Baumgarten L, Dalela D, Jamil M, Budzyn J, Kovacevic N, Yaguchi G, Palma-Zamora I, Perkins S, Bazzi M, Wong P. Managing Urology Consultations During COVID-19 Pandemic: Application of a Structured Care Pathway. Urology. 2020. [Published online ahead of print April 21, 2020]. DOI: 10.1016/j.urology.2020.04.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Interim Guidance for Healthcare Facilities: Preparing for Community Transmission of COVID-19 in the United States. Available at: https://www.cdc.gov/coronavirus/2019-ncov/healthcare-facilities/guidance-hcf.html. Accessed April 9, 2020.
- 5.Centers for Medicare & Medicaid Services. Medicare telehealth health care provider fact sheet: Medicare coverage and payment of virtual services. Available at: https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet. Accessed April 9, 2020.
- 6.Fenelon C, Murphy E, Galbraith J, O’Sullivan M. Telesurveillance: Exploring the Use of Mobile Phone Imaging in the Follow-Up of Orthopedic Patients with Hand Trauma. Telemed J E Health. 2019;25:1244-1249. [DOI] [PubMed] [Google Scholar]
- 7.Guoxiu W. Online medical platforms attract more users during COVID-19 in China. CGTN. 19 March 2020. Available at: https://news.cgtn.com/news/2020-03-19/Online-medical-platforms-attract-more-users-during-COVID-19-in-China-OZzlI4bhAs/index.html. Accessed May 28, 2020. [Google Scholar]
- 8.Hemingway JF, Singh N, Starnes BW. Emerging Practice Patterns in Vascular Surgery During the COVID-19 Pandemic. J Vasc Surg. [Published online ahead of print April 30, 2020]. DOI: 10.1016/j.jvs.2020.04.492. [DOI] [PMC free article] [PubMed]
- 9.Hopkins University & Medicine Johns. Coronavirus Resource Center. Available at: https://coronavirus.jhu.edu/map.html. Accessed April 9, 2020.
- 10.Loeb A, Rao S, Ficke J, Morris C, Riley L, III, Levin A. Departmental Experience and Lessons Learned with Accelerated Introduction of Telemedicine During the COVID-19 Crisis. J Am Acad Orthop Surg. 2020;28:e469-e476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Parisien R, Shin M, Constant M, Saltzman B, Li X, Levine W, Trofa D. Telehealth Utilization in Response to the Novel Coronavirus (COVID-19) Pandemic in Orthopaedic Surgery. J Am Acad Orthop Surg. 2020;28:e487-e492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stinner D, Lebrun C, Hsu J, Jahangir A, Mir H. The Orthopaedic Trauma Service and COVID-19 – Practice Considerations to Optimize Outcomes and Limit Exposure. J Orthop Trauma . [Published online ahead of print April 23, 2020]. DOI: 10.1097/BOT.0000000000001782. [DOI] [PMC free article] [PubMed]
- 13.WeDoctor WeDoctor. Global Consultation and Prevention Center. 2020. Available at: https://promo.guahao.com/en/global/pneumonia/?_cp=yhcbz0315&cs=share&from=timeline&isappinstalled=0. Accessed May 28, 2020.