History
Spine injuries have been described since 3000 BC in Egypt when it was illustrated in Edwin Smith’s surgical papyrus [37], and many classifications for subaxial spine injuries have been developed and used in the intervening decades since Bohler [6] did so in 1929 [2-6, 9, 15, 17, 18, 25, 30, 38, 45, 47-49] (Table 1). Although most of these classifications have contributed to the understanding of spinal stability and mechanisms of injury, each classification also has at least one shortcoming that caused it to fall into disuse. The most-common shortcomings have included: lack of exclusivity to the cervical spine, use of injury mechanism, lack of consideration of neurological status, and lack of validity.
Table 1.
Previous classification systems involving either the subaxial cervical spine, or morphologic characteristics of thoracolumbar injuries that are also used to describe similar morphologic injury characteristics of the subaxial cervical spine
| Author | Notable contributions | Disadvantages |
| Bohler [6] | Vertebra versus neural arch injuries | Primarily thoracolumbar |
| Watson-Jones [45] | Wedge, comminuted, fracture dislocation identified. Importance of posterior longitudinal ligament | |
| Nicoll et al. [30] | Different wedge fracture types | |
| Kelly and Whitesides [25] | Two-column concept (anterior and posterior column) | |
| Holdsworth [17] | First classification based on injury mechanism; importance of posterior ligamentous complex | |
| Denis [9] | Three-column theory (middle column) | |
| Whitley and Forsyth [49] | Promoted mechanism-based classification for subaxial cervical trauma | Retrospective interpretation of an injury mechanism based on observed morphology |
| White and Punjabi [47, 48] | Defined spinal stability in the cervical spine based on biomechanical study | Iatrogenic injuries to cadaveric specimens, not real patient injuries. |
| Jacobs [18] | Promoted mechanism-based classification | Not comprehensive |
| Babcock [5] | ||
| Allen et al. [3] | Mechanism based classification, comprehensive categories | Challenging for beginners; retrospective interpretation of an injury mechanism based on observed morphology |
| Harris [15] | Similar to Allen-Ferguson, but included rotational vectors and categories based on causative force vectors | Lack of gradation for compression injuries; challenging for beginners |
| Aebi and Nazarian [2] | Upper and lower cervical spine in same system; bony or ligamentous involvement or both | Lack of clinical relevance |
| Argenson et al. [4] | Rotational injuries; high interobserver reliability | Oversimplification of some flexion-distraction and extension-distraction types |
We believe that classifications used for the thoracolumbar spine are ill-suited to the subaxial spine because of the important anatomic and biomechanical differences between those anatomic locations. The different anatomic and biomechanical characteristics between the subaxial cervical spine and the thoracolumbar spine are reasons they should not be classified together. The use of injury mechanism instead of morphology is a shortcoming, as the direct reading of images requires a person to first identify a morphologic feature on imaging, then interpret this morphology into a mechanism of injury. This extra step in interpretation was thought to be overly complicated, leading to less intraobserver reliability [38, 41]. The lack of consideration with respect to the neurological status of the patient allows for a treatment decision to be made without considering the patient evaluation, which is generally an important aspect that guides intervention. Ultimately, however, the most-common shortcoming was lack of validity of the classification system, making most not generalizable or reproducible enough for practical use.
For these reasons, Vaccaro et al. [41] developed the Subaxial Injury Classification and Severity Scale (SLICS) for subaxial cervical spine injuries. This system sought to create a simpler classification system that could be used to help guide patient treatment and facilitate communication among treating physicians. SLICS includes three separate categories: the morphology, the neurologic status of the patient, and integrity of the discoligamentous complex (DLC). Each of these categories is summed for a total score that is meant to guide surgical versus nonsurgical management of the injury.
Purpose
Subaxial cervical spine injuries account for more than two-thirds of all cervical spine trauma, and these patients are considerably more likely to have neurologic symptoms compared with patients who have atlantoaxial injuries [1, 14]. Subaxial cervical spine injuries, like all injuries to the cervical spine, require emergent evaluation and communication among physicians to correctly treat the patient. Vaccaro et al. [41] sought to create this classification system to help facilitate physician communication through simpler injury morphologic characteristics, and to help predict surgical versus nonsurgical management with the summation of three different categories. Although prognostic and research utility are other common reasons to use a classification system, Vaccaro et al. [41] did not specifically address those reasons during the creation of SLICS. Identification and communication between physicians about these injuries is critical in treating patients promptly and appropriately.
Unfortunately, as will be discussed further, the SLICS system is not well validated. This lack of validation renders the primary goals of guiding treatment and facilitating physician communication for subaxial cervical spine injuries inadequate, or even potentially harmful, in the clinical setting. Where research is concerned, using an inadequately validated classification system is problematic, as it undermines the robustness of research based on it.
Description
The SLICS scale has an incorporated scoring system that helps to guide the transition from nonsurgical to surgical management based on three categories: morphologic features, integrity of the DLC, and neurologic status of the patient [41] (Table 2). This is similar to another classification system created by Vaccaro for thoracolumbar injuries, called the Thoracolumbar Injury Classification and Injury Severity Score System (TLICS) [19, 43], except that the DLC integrity in SLICS is replaced with the posterior ligamentous complex (PLC) in the TLICS system, along with some subtle differences in the individual scoring categories. The scores in SLICS are determined by an interpretation of radiographs, CT images, and MRI. Each category has a point value based on increasing severity, from 0 (least severe) to 4 (most severe). If the summative score of the three categories is less than or equal to 3, then nonsurgical treatment is recommended in SLICS [41]. If the score is 5 or greater, surgical management is recommended by the creators of SLICS. A score of 4 is indeterminate in terms of recommending for or against surgical management by the creators of SLICS. The purpose of this overall score is to maximize the likelihood of neurologic recovery if a deficit exists and/or to prevent neurologic decline if instability is present [41].
Table 2.
Subaxial Injury Classification and Severity Scale (SLICS) for subaxial cervical spine injuries
| Injury | Score |
| Morphologic features | |
| No morphologic abnormality | 0 |
| Compression | 1 |
| Burst | 2 |
| Distraction | 3 |
| Rotational and/or translational | 4 |
| Integrity of the discoligamentous complex | |
| Intact | 0 |
| Indeterminate | 1 |
| Disrupted | 2 |
| Patient’s neurologic status | |
| Intact | 0 |
| Nerve root injury | 1 |
| Complete | 2 |
| Incomplete | 3 |
| Persistent cord compression (in the setting of a neurologic deficit) | +1 |
| Total SLICS score | 0 - 10 |
Author recommendations based on total score: nonoperative treatment for a total score ≤ 3; operative treatment for a total score ≥ 5; for a total score of 4, a recommendation is indeterminate requiring discretion of the treating surgeon.
Morphologic Features
The injury morphology category is based on the injury pattern. It is scored as a 0 for no abnormality. A score of 1 is given for compression injuries and 2 for burst injuries (Fig. 1). A score of 3 is given for distraction injuries (Fig. 2). A score of 4 is given for rotational or translation injuries (Fig. 3) [41]. With distraction injuries, either the anterior or posterior columns may have remained intact. This contrasts with a rotation or translation injury, in which both the anterior and posterior structures are more likely to be compromised, according to MRI studies [41]. Therefore, rotation or translation injuries are associated with a greater degree of instability, and this is accounted for in this scoring system. An example injury that would be categorized as translational shows the disruption of both the anterior and posterior structures (Fig. 4).
Fig. 1 A-E.
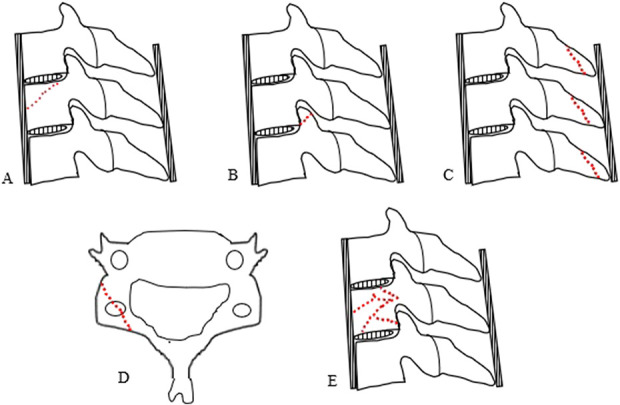
Illustrations of example injuries that would fall into the compression morphologic category of the Subaxial Injury Classification and Severity Scale. (A) Simple compression fracture, (B) simple nondisplaced superior articulating process fracture, (C) spinous process fractures, (D) lateral mass fracture. (E) An example burst fracture with or without retropulsion would be placed into the burst morphologic category. Dotted lines represent fracture lines.
Fig. 2 A-C.
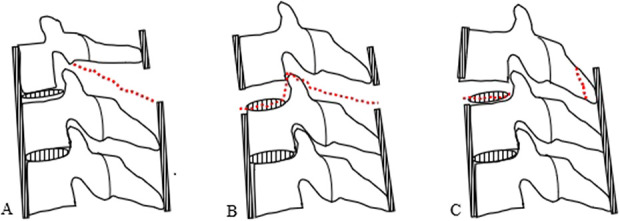
Illustrations of three different types of injuries that would fit into the distraction category of morphologic features. (A) Injury to the posterior elements causing distraction of the two adjacent spinous processes. (B) Injury to the discoligamentous complex, anterior, and posterior ligaments with distraction between the two vertebra. (C) Spinous process fracture with superior distraction of the anterior vertebral body. Dotted lines represent ligamentous disruption or fracture lines.
Fig. 3 A-D.
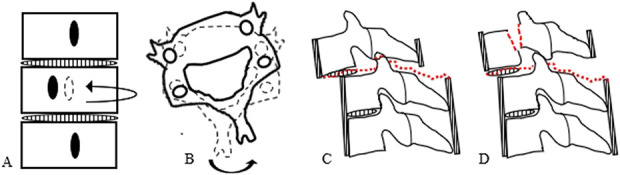
Illustrations of four different types of injury patterns that would fit into the rotational/translational category of morphologic features. (A) Coronal plane view of a vertebral body segment with rotational malalignment of the middle segment relative to the superior and inferior vertebrae based on the change in orientation of the spinous process. (B) Axial plane view of an inferior vertebra, solid line, with rotational deformity relative to the inferior vertebra, dashed line. (C) Translational injury showing facet dislocation, a superior articular process fracture, and disruption of both the anterior and posterior ligamentous. (D) Fracture of the pedicle with translation of the anterior fragment and disruption of both the anterior and posterior ligamentous structures. Dotted lines represent ligamentous disruption or fracture lines.
Fig. 4 A-B.
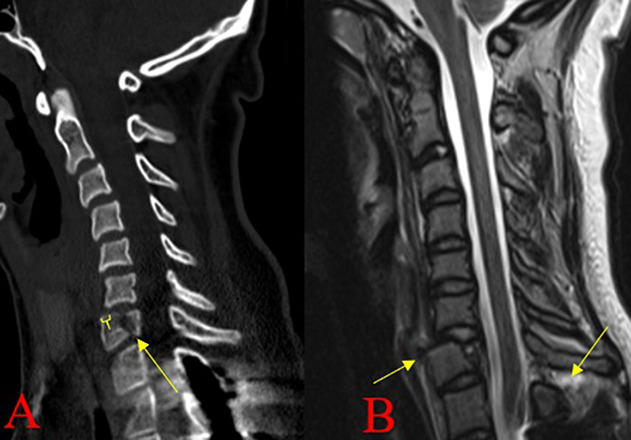
(A) Sagittal CT imaging example of a translational injury demonstrating by a C7 vertebral body fracture with retrolisthesis of the C6 vertebra relative to the C7 vertebra and (B) Sagittal MR images showing disruption of the anterior and posterior ligamentous structures.
Integrity of the Discoligamentous Complex (DLC)
The DLC includes the following anatomic structures: vertebral disc, anterior longitudinal ligament, posterior longitudinal ligament, ligamentum flavum, facet capsules, interspinalis muscle, and supraspinous ligaments. When there is no injury to any of these structures, a score of 0 is given, an indeterminate condition of these structures is assigned a score of 1, and injury to any of these structures is given a score of 2, which is associated with a greater degree of instability. Injury to the DLC is considered separately in the assessment of spinal stability because the healing capacity of these soft tissues is less predictable than that of bone healing, and if injury to the DLC is misjudged, it may lead to instability, deformity, and neurologic decline [41]. With the use of MR imaging, subtle signal changes on different sequences can help verify if the DLC is intact (Fig. 5). When there is a high suspicion for disruption of the DLC, but there is either poor or nonexistent imaging studies, this makes the determination of disrupted or intact DLC difficult giving this category an indeterminate score. In the setting of suspected DLC disruption based on CT images alone, additional MR imaging with obvious signal change and evidence of DLC disruption supports the presence of instability (Fig. 6).
Fig. 5 A-C.

(A) Sagittal CT imaging example of a compression fracture of C7, with sagittal (B) MR-STIR sequence and (C) MR-T2-weighted sequence showing no disruption of the discoligamentous complex.
Fig. 6 A-C.
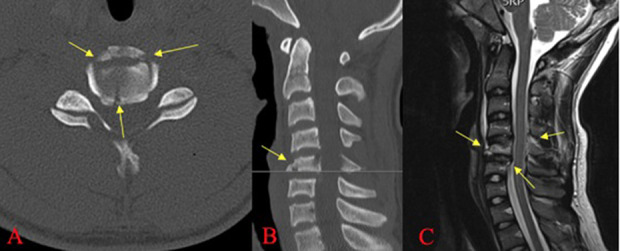
CT imaging example of a C5 burst fracture in the (A) axial and (B) sagittal plane with (C) sagittal MR imaging showing disruption of the discoligamentous complex.
Neurologic Status
A clinical evaluation of the patient and determination of his or her neurologic status is important, along with correlating the imaging studies to the observed clinical presentation [41, 47]. Neurologic status is scored as a 0 for a patient without neurologic impairment, 1 for a nerve root injury, 2 for a complete spinal cord injury, and 3 for an incomplete spinal cord injury; an additional point can be added to any of these scores if continuous cord compression is observed in the setting of a neurologic deficit.
With three categories, and up to five grades in each category, this classification system can be difficult to use in practice because of the wide variations in score tallying. The studies discussed below have sought to validate this classification system, but they have not found it to have a high level of interobserver reliability, meaning that the scoring system is not consistent enough between observers to effectively and accurately communicate a given subaxial spine injury. Because of this lack of reliability, it should not be used clinically and means that research based on the classification system may be misleading.
Validation
To justify widespread use of the SLICS, a high degree of interobserver and intraobserver reliability would be critical; unfortunately, this has not been demonstrated. Five studies have looked at the interobserver and/or intraobserver reliability of SLICS as a whole and its three categories separately [24, 28, 39, 41, 44] (Table 3). To our knowledge, only the developers [39, 41] of the system and a single institution study in South Korea [28] have written supportively in terms of its interobserver reliability, while others found inconsistent intra- and interobserver reliability across the three domains of the classification (morphology, DLC, and neurologic status) and the overall SLICS score [24, 44].
Table 3.
Interobserver and Intraobserver ICC and kappa values for different validation studies of SLICS
| Study | Interobserver or intraobserver data | Morphology | Integrity of DLC | Neurologic status | Total SLICS score | ||||
| ICC | Kappa | ICC | Kappa | ICC | Kappa | ICC | Kappa | ||
| Vaccaro et al. [41] | Interobserver | 0.57 | 0.51 | 0.49 | 0.33 | 0.87 | 0.62 | 0.71 | 0.20 |
| Intraobserver | 0.75 | 0.65 | 0.66 | 0.50 | 0.90 | 0.72 | 0.83 | 0.39 | |
| Stone et al. [39] | Interobserver | 0.86 | 0.90 | 0.98 | 0.79 | ||||
| Intraobserver | 0.94 | 0.94 | 0.99 | 0.98 | |||||
| Lee et al. [28] | Interobserver | 0.60 | 0.30 | 1.0 | 0.78 | ||||
| Intraobserver | 0.92 | 0.88 | 1.0 | 0.96 | |||||
| Van Middendorp et al. [44] | Interobserver | 0.29 | 0.46 | 0.70 | 0.78 | ||||
| Intraobserver | |||||||||
| Kanagaraju et al. [24] | Interobserver | 0.32 | 0.21 | 0.32 | 0.21 | 0.46 | 0.28 | 0.41 | 0.15 |
| Intraobserver | 0.33 | 0.41 | 0.59 | 0.39 | 0.78 | 0.65 | 0.16 | 0.23 | |
ICC = intraclass correlation coefficient; SLICS = Subaxial Injury Classification and Severity Scale; DLC = discoligamentous complex.
At the time the SLICS classification was created, Vaccaro et al. [41] demonstrated the following interobserver reliability ratings for the these SLICS categories: Moderate for injury morphology, fair for the DLC category, substantial for neurologic status, slight to fair for the overall score, and moderate for the SLICS management recommendation (intraclass correlation coefficient (ICC) = 0.58; κ = 0.44). Although the authors suggested there was a high construct validity because interrater agreement for treatment recommendations based on the SLICS algorithm was 93.3%, low ICC and kappa values suggest that a substantial portion of patient injuries were mischaracterized, which is also evident by the contradictory ICC and kappa values of the overall score category that suggests fair (ICC = 0.71) and slight (κ = 0.2) agreement, respectively. Ideally, each category (and not just the overall score) should have good reliability, and if this is not the case, it means that there may be elements of each injury pattern that are missed. As such, this system is not suitable for clinical care or research.
In an external validation study, Kanagaraju et al. [24] compared SLICS with the Allen-Ferguson classification. They found only slight-to-fair interobserver reliability and poor-to-fair intraobserver reliability for the overall SLICS score; the highest level of agreement for the individual categories was the neurological status, which was only rated as fair (ICC = 0.46; κ = 0.28). This study appears to be more comprehensive than the other four studies because of the number of patients involved, the number and types of observers, the results for both interobserver and intraobserver reliability, the reporting of both ICC and kappa values, the geographical variability, and the lack of original SLICS authors involved in the study (Table 4). Another external validation study by Van Middendorp et al. [44], which also did not have any contributing developer of SLICS in the study byline, also demonstrated only fair-to-moderate interobserver reliability within the morphology and DLC integrity categories. However, we note that it did show substantial agreement for the overall SLICS score comparable to Vaccaro’s results [41, 44]. Van Middendorp et al. [44] only reported ICC values for interobserver data, and they had no data regarding intraobserver reliability.
Table 4.
Summary of the different validation studies done for the SLICS classification and their notable study characteristics
| Study | Patient cases | Number and type of observers | Geographical diversity of where observers work | CT/MRI availability for each patient case | Case selection method | Original SLICS authors involved? |
| Vaccaro et al. [41] | 11 | 20 (five neurosurgeons, 15 orthopaedic spine surgeons) | Five countries | Not reported | Self-selected | Original article |
| Stone et al. [39] | 50 | Five fellowship-trained spine surgeons | Two countries | 100% for CT, 70% for MRI | Consecutive case series | Yes |
| Lee et al. [28] | 75 | Three (one spine surgeon, one resident, one radiologist) | South Korea only, single institution | 100% for both CT and MRI | Cases selected for clarity, only operative cases | No |
| Van Middendorp et al. [44] | 51 | 12 (five fellowship-trained spine surgeons, seven spine fellows) | Nine countries | 100% CT, 41% MRI | Consecutive case series | No |
| Kanagaraju et al. [24] | 34 | 13 spine surgeons from STSG ISCS | Four countries | Not reported | Consecutive case series | No |
SLICS = Subaxial Injury Classification and Severity Scale; STSG ISCS = Spine Trauma Group of the International Spinal Cord Society.
Stone et al. [39] and Lee et al. [28] also sought to validate the SLICS classification. Stone et al. [39] demonstrated excellent agreement in every category and overall SLICS score for both interobserver and intraobserver reliability, but that study included developers of the SLICS system. In addition, Stone et al. [39] had the smallest number of observers, and its geographical diversity was second only to Lee et al. [28]. Lee et al. [28] showed substantial-to-excellent agreement in every category of the interobserver and intraobserver reliability, except for the moderate agreement in the DLC integrity category for interobserver data. However, a shortcoming of Lee’s study, which might contribute to the high reliability they observed, was that the patients who were selected were only those who were treated nonoperatively [28].
Several other studies have also been done to look at the correlation of the SLICS score with surgical versus nonsurgical treatment of patients, with varying results [7, 8, 11, 16, 20-23, 33-35, 44, 46]. Although some of these are high-quality studies, they fail to address the lack of reliability inherent within the SLICS system that the above-mentioned studies have reported.
The biggest limitation of the SLICS system is the lack of supportive data from a higher quality, more generalizable external validation study. For these reasons, along with the low intra- and interobserver reliability observed in the higher-quality validation studies of the SLICS system [24, 44], we recommend that this classification system not be used for communication among physicians or to guide treatment.
Limitations
As with any classification system, and especially given the evolving history of previous classification systems for traumatic subaxial cervical spine injuries, there are limitations to SLICS. The most obvious limitation is the poor interobserver reliability of morphologic characteristics. Vaccaro et al. [41] theorized that this would increase with time and increased familiarity with the classification system, but ultimately the opposite has been true in the validation studies that followed [24, 44]. The morphologic characteristic category was created because other classifications focusing on the mechanism were complex, indirect evaluations of the injury and had numerous categories to apply when classifying a patient’s injuries. The morphology section of this classification was intended to lead to a simpler, more-direct interpretation based on imaging [41], and so it might be easier to remember. Unfortunately, it appears that this difference did not improve the performance of the new classification. Its poor reliability may be explained by the fact that the injury’s morphology was oversimplified, leading to mischaracterizations of injury patterns, which also led to the poor reliability of the overall score that integrated this morphology category.
Another limitation regarding the validation of the SLICS classification is the imaging. A study to determine the utility of CT alone versus CT and MRI in calculating the SLICS score showed higher interobserver reliability with the CT and MRI analysis [29]. Some validation studies did not state whether full CT and MR images were available for all patients [24, 28, 39, 41, 44], which could have influenced the findings in important ways.
When specific injuries patterns are encountered using the SLICS algorithm that result in a treatment recommendation for nonoperative care or when the injury falls into the indeterminate category, this presents yet another limitation to the classification system (Table 5). Although the list provided in the table shows some common scenarios where SLICS is limited, it is not comprehensive and does not address injuries to other surrounding structures in the cervical spine, such as the vertebral artery. Some evidence supports the decision to pursue operative treatment in the specific examples given, along with the commonly supported surgical indications including decompression of the spinal cord, stabilization to keep injuries from progressing, and deformity correction [10, 12, 13, 26, 27, 31, 32, 36, 40]. When looking at these specific injury patterns and supportive evidence for operative treatment, it is easy to see how the use of SLICS could lead to poor treatment choices when treating physicians try to communicate using an imperfectly validated classification. The limitations of this classification system ultimately led Vaccaro to create the AO Spine Sub-axial Cervical Spine Classification system, which remains under investigation [42].
Table 5.
A list of specific injuries that would carry a nonoperative or indeterminate recommendation from the SLICS algorithm, which would otherwise be treated surgically based on commonly accepted surgical indications in the available evidence [10, 12, 13, 26, 27, 31, 32, 36, 40]
| Example injury | Total SLIC Score |
| Burst fracture (2), with a nerve root injury (1), with or without continuous cord compression (+1) | 3-4 |
| Complete (2) or incomplete (3) spinal cord injury with indeterminate DLC injury (1) | 3-4 |
| Compression fracture (1) with a complete (2) or incomplete (3) spinal cord injury | 3-4 |
| DLC injury (2) with severe kyphosis | 2 |
| DLC injury (2) with nerve root (1) or complete spinal cord injury (2) | 3-4 |
| Floating lateral mass (compression = 1, DLC injury = 2), with or without a nerve root injury | 3-4 |
| Other facet fractures without observed distraction/translation/rotation components, and with varying degrees of neurological deficit | 1-4 |
SLICS = Subaxial Injury Classification and Severity Scale; DLC = discoligamentous complex.
Conclusions
The SLICS scale is the first subaxial cervical spine injury classification that includes the morphologic characteristics of the injury and a neurologic evaluation of the patient. It incorporates an evaluation of stability, the patient, and the injury’s morphology. Although a few studies showed good interobserver reliability with this classification [26, 28, 39], those studies are of lower quality than some more-recent studies that have questioned the intra- and interobserver reliability of this system [39, 44]. Because of this, we cannot recommend its use in clinical practice or research until high-quality studies demonstrate it to be reproducible across a range of users’ experience levels and clinical settings.
Footnotes
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Both author certify that neither he, nor any member of his immediate family, has funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Both authors certify that his institution waived approval for the reporting of this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Aebi M. Surgical treatment of upper, middle and lower cervical injuries and non-unions by anterior procedures. Eur Spine J. 2010;19 Suppl:S33-S39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aebi M, Nazarian S. [Classification of injuries of the cervical spine] [in German]. Orthopade. 1987;16:27-36. [PubMed] [Google Scholar]
- 3.Allen BL, Jr, Ferguson RL, Lehmann TR, O'Brien RP. A mechanistic classification of closed, indirect fractures and dislocations of the lower cervical spine. Spine (Phila Pa 1976) 1982;7:1-27. [DOI] [PubMed] [Google Scholar]
- 4.Argenson C, de Peretti F, Ghabris A, Eude P, Lovet J, Hovorka I. Classification of lower cervical spine injuries. Eur J Orthop Surg Traumatol. 1997;7;215-229. [Google Scholar]
- 5.Babcock JL. Cervical spine injuries. Diagnosis and classification. Arch Surg. 1976;111:646-651. [DOI] [PubMed] [Google Scholar]
- 6.Bohler L. The Treatment of Fractures. A Translation of “Technik der Knochenbruchbehandlung im Frieden und im Kriege” by M. E. Steinberg. Vienna, Austria: Wilhelm Maudrich; 1929. [Google Scholar]
- 7.Bono CM, Schoenfeld A, Gupta G, Harrop JS, Anderson P, Patel AA, Dimar J, Aarabi B, Dailey A, Vaccaro AR, Gahr R, Shaffrey C, Anderson DG, Rampersaud R. Reliability and reproducibility of subaxial cervical injury description system: a standardized nomenclature schema. Spine (Phila Pa 1976). 2011;36:E1140–E1144. [DOI] [PubMed] [Google Scholar]
- 8.Cruz HY, Joaquim AF, Tedeschi H, Patel AA. Evaluation of the SLICS use in the treatment of subaxial cervical spine injuries. Arq Neuropsiquiatr. 2015;73:445-449. [DOI] [PubMed] [Google Scholar]
- 9.Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976) . 1983;8:817-831. [DOI] [PubMed] [Google Scholar]
- 10.Dvorak MF, Fisher CG, Aarabi B, et al. Clinical outcomes of 90 isolated unilateral facet fractures, subluxations, and dislocations treated surgically and nonoperatively. Spine (Phila Pa 1976). 2007;32:3007-3013. [DOI] [PubMed] [Google Scholar]
- 11.Dvorak MF, Fisher CG, Fehlings MG, Rampersaud YR, Oner FC, Aarabi B, Vaccaro AR. The surgical approach to subaxial cervical spine injuries: an evidence-based algorithm based on the SLIC classification system. Spine (Phila Pa 1976). 2007;32:2620-2629. [DOI] [PubMed] [Google Scholar]
- 12.Fehlings M, Rabin D, Sears W, Cadotte D, Aarabi B. Current practice in the timing of surgical intervention in spinal cord injury. Spine. 2010;35:166–173. [DOI] [PubMed] [Google Scholar]
- 13.Fehlings MG, Vaccaro A, Wilson JR, et al. Early versus delayed decompression for traumatic cervical spinal cord injury: results of the Surgical Timing in Acute Spinal Cord Injury Study (STASCIS). PLoS One. 2012;7:e32037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Feuchtbaum E, Buchowski J, Zebala L. Subaxial cervical spine trauma. Curr Rev Musculoskelet Med. 2016;9:496-504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Harris JH, Jr, Edeiken-Monroe B, Kopaniky DR. A practical classification of acute cervical spine injuries. Orthop Clin North Am. 1986;17:15-30. [PubMed] [Google Scholar]
- 16.Hitti FL, McShane BJ, Yang AI, Rinehart C, Albayar A, Branche M, Malhotra NR, Janjua MB, Ali ZA, Schuster JM, Ozturk AK. Predictors of failure of nonoperative management following subaxial spine trauma and creation of modified subaxial injury classification system. World Neurosurg. 2019;122:e1359-e1364. [DOI] [PubMed] [Google Scholar]
- 17.Holdsworth F. Fractures, dislocations, and fracture-dislocations of the spine. J Bone Joint Surg Am. 1970;52:1534-1551. [PubMed] [Google Scholar]
- 18.Jacobs B. Cervical fractures and dislocations (C3-7). Clin Orthop Relat Res. 1975;18-32. [DOI] [PubMed] [Google Scholar]
- 19.Jiménez-Almonte JH, King JD, Luo TD, Cassidy RC, Aneja A. Classifications in Brief: Thoracolumbar Injury Classification and Injury Severity Score System. Clin Orthop Relat Res. 2018;476:1352-1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Joaquim AF, Ghizoni E, Tedeschi H, da Cruz HY, Patel AA. Clinical results of patients with subaxial cervical spine trauma treated according to the SLIC score. J Spinal Cord Med. 2014;37:420-424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Joaquim AF, Lawrence B, Daubs M, Brodke D, Patel AA. Evaluation of the subaxial injury classification system. J Craniovertebr Junction Spine. 2011;2:67-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Joaquim AF, Patel AA. Subaxial cervical spine trauma: evaluation and surgical decision-making. Global Spine J. 2014;4:63-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Joaquim AF, Patel AA, Vaccaro AR. Cervical injuries scored according to the Subaxial Injury Classification system: An analysis of the literature. J Craniovertebr Junction Spine. 2014;5:65-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kanagaraju V, Yelamarthy PKK, Chhabra HS, Shetty AP, Nanda A, Sangondimath GM, Das KD, Bansal ML, Mohaptra B, Patel N, Abel R, Tuli S, Barros T, Tandon V. Reliability of Allen Ferguson classification versus subaxial injury classification and severity scale for subaxial cervical spine injuries: a psychometrics study. Spinal Cord. 2019;57:26-32. [DOI] [PubMed] [Google Scholar]
- 25.Kelly RP, Whitesides TE., Jr Treatment of lumbodorsal fracture dislocations. Ann Surg. 1968;167:705-717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Koivikko MP, Myllynen P, Karjalainen M, Vornanen M, Santavirta S. Conservative and operative treatment in cervical burst fractures. Arch Orthop Trauma Surg. 2000;120:448-451. [DOI] [PubMed] [Google Scholar]
- 27.Lee SH, Sung JK. Unilateral lateral mass-facet fractures with rotational instability: new classification and a review of 39 cases treated conservatively and with single segment anterior fusion. J Trauma. 2009;66:758-767. [DOI] [PubMed] [Google Scholar]
- 28.Lee WJ, Yoon SH, Kim YJ, Kim JY, Park HC, Park CO. Interobserver and Intraobserver Reliability of Sub-Axial Injury Classification and Severity Scale between Radiologist, Resident and Spine Surgeon. J Korean Neurosurg Soc. 2012;52:200-203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mascarenhas D, Dreizin D, Bodanapally UK, Stein DM. Parsing the utility of CT and MRI in the subaxial cervical spine injury classification (SLIC) system: is CT SLIC enough? AJR Am J Roentgenol. 2016;206:1292-1297. [DOI] [PubMed] [Google Scholar]
- 30.Nicoll EA. Fractures of the dorso-lumbar spine. J Bone Joint Surg Br. 1949;31:376-394. [PubMed] [Google Scholar]
- 31.O'Dowd JK. Basic principles of management for cervical spine trauma. Eur Spine J. 2010;19(Suppl 1):S18-S22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Papadopoulos SM, Selden NR, Quint DJ, Patel N, Gillespie B, Grube S. Immediate spinal cord decompression for cervical spinal cord injury: feasibility and outcome. J Trauma. 2002;52:323-332. [DOI] [PubMed] [Google Scholar]
- 33.Patel AA, Dailey A, Brodke DS, Daubs M, Anderson PA, Hurlburt RJ, Vaccaro AR, Spine Trauma Study Group. Subaxial cervical spine trauma classification: the Subaxial Injury Classification system and case examples. Neurosurg Focus. 2008;25:E8. [DOI] [PubMed] [Google Scholar]
- 34.Patel AA, Hurlbert RJ, Bono CM, Bessey JT, Yang N, Vaccaro AR. Classification and surgical decision making in acute subaxial cervical spine trauma. Spine (Phila Pa 1976). 2010;35(21 Suppl):S228–S234. [DOI] [PubMed] [Google Scholar]
- 35.Samuel S, Lin JL, Smith MM, Hartin NL, Vasili C, Ruff SJ, Cree AK, Ball JR, Sergides IG, Gray R. Subaxial injury classification scoring system treatment recommendations: external agreement study based on retrospective review of 185 patients. Spine (Phila Pa 1976). 2015;40:137-142. [DOI] [PubMed] [Google Scholar]
- 36.Shanmuganathan K, Mirvis SE, Levine AM. Rotational injury of cervical facets: CT analysis of fracture patterns with implications for management and neurologic outcome. AJR Am J Roentgenol. 1994;163:1165-1169. [DOI] [PubMed] [Google Scholar]
- 37.Silver JR. History of the treatment of spinal injuries. Postgrad Med J. 2005;81:108-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Song KJ, Lee SK, Ham DH, Kim YJ, Choi BW. Limitation of previous Allen classification and subaxial cervical spine injury classification (SLIC) system in distractive-extension injury of cervical spine: proposal of modified classification system. Eur Spine J. 2016;25:74-79. [DOI] [PubMed] [Google Scholar]
- 39.Stone AT, Bransford RJ, Lee MJ, Vilela MD, Bellabarba C, Anderson PA, Agel J. Reliability of classification systems for subaxial cervical injuries. Evid Based Spine Care J. 2010;1:19-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Toh E, Nomura T, Watanabe M, Mochida J. Surgical treatment for injuries of the middle and lower cervical spine. Int Orthop. 2006;30:54-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Vaccaro AR, Hulbert RJ, Patel AA, Fisher C, Dvorak M, Lehman RA, Jr, Anderson P, Harrop J, Oner FC, Arnold P, Fehlings M, Hedlund R, Madrazo I, Rechtine G, Aarabi B, Shainline M, Spine Trauma Study Group. The subaxial cervical spine injury classification system: a novel approach to recognize the importance of morphology, neurology, and integrity of the disco-ligamentous complex. Spine (Phila Pa 1976). 2007;32:2365-2374. [DOI] [PubMed] [Google Scholar]
- 42.Vaccaro AR, Koerner JD, Radcliff KE, Oner FC, Reinhold M, Schnake KJ, Kandziora F, Fehlings MG, Dvorak MF, Aarabi B, Rajasekaran S, Schroeder GD, Kepler CK, Vialle LR. AOSpine subaxial cervical spine injury classification system. Eur Spine J. 2016;25:2173-2184. [DOI] [PubMed] [Google Scholar]
- 43.Vaccaro AR, Lehman RA, Jr, Hurlbert RJ, Anderson PA, Harris M, Hedlund R, Harrop J, Dvorak M, Wood K, Fehlings MG, Fisher C, Zeiller SC, Anderson DG, Bono CM, Stock GH, Brown AK, Kuklo T, Oner FC. A new classification of thoracolumbar injuries: the importance of injury morphology, the integrity of the posterior ligamentous complex, and neurologic status. Spine (Phila Pa 1976) . 2005;30:2325-2333. [DOI] [PubMed] [Google Scholar]
- 44.van Middendorp JJ, Audigé L, Bartels RH, Bolger C, Deverall H, Dhoke P, Diekerhof CH, Govaert GAM, Guimera V, Koller H, Morris SAC, Setiobudi T, Hosman AJF. The Subaxial Cervical Spine Injury Classification System: an external agreement validation study. Spine J. 2013;13:1055-1063. [DOI] [PubMed] [Google Scholar]
- 45.Watson-Jones R. The results of postural reduction of fractures of the spine. J Bone Joint Surg Am. 1938;20:567-586. [Google Scholar]
- 46.Whang PG, Patel AA, Vaccaro AR. The development and evaluation of the subaxial injury classification scoring system for cervical spine trauma. Clin Orthop Relat Res. 2011;469:723-731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.White AA, 3rd, Johnson RM, Panjabi MM, Southwick WO. Biomechanical analysis of clinical stability in the cervical spine. Clin Orthop Relat Res. 1975;109:85-96. [DOI] [PubMed] [Google Scholar]
- 48.White AA, 3rd, Panjabi MM. Update on the evaluation of instability of the lower cervical spine. Instr Course Lect. 1987;36:513-520. [PubMed] [Google Scholar]
- 49.Whitley JE, Forsyth HF. The classification of cervical spine injuries. Am J Roentgenol Radium Ther Nucl Med. 1960;83:633-644. [PubMed] [Google Scholar]


