
Sujana S. Chandrasekhar, MD, FACS, FAAOHNS, Consulting Editor
The year 2020 has seen disruptions in nearly every aspect of our lives, due to the global pandemic of COVID-19, caused by the virus severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). As such, we present the following 4 articles in this special series on COVID-19, guest edited by Dr Zara Patel, to detail what we have learned in this ever-changing landscape, and where we might go from here.
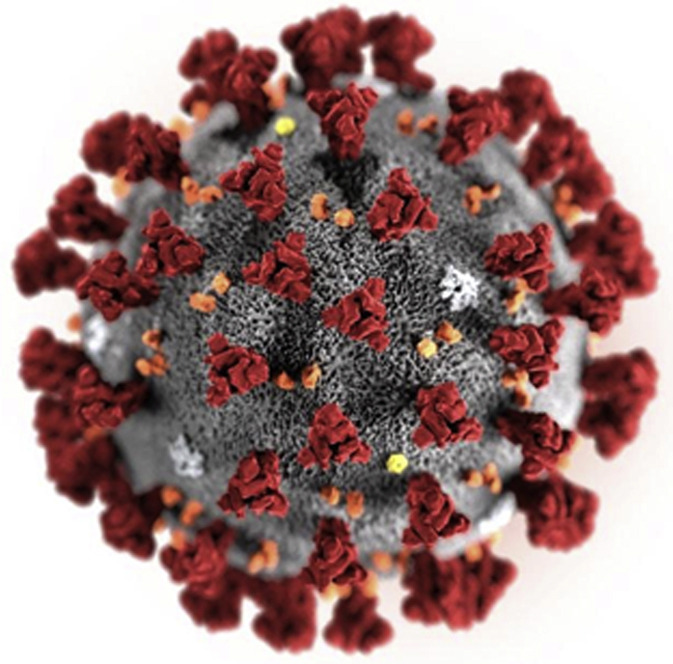
Coronaviruses are named for the crownlike spikes on their surface. They overwhelmingly infect animals, but at least 7 strains infect humans, including this new virus causing COVID-19. Four cause common colds. Two others rank among the deadliest of human infections: severe acute respiratory syndrome, or SARS, and Middle East respiratory syndrome, or MERS.
The original SARS outbreak first appeared in South China in 2002 but was able to be contained.1 SARS (or SARS-CoV) was spread by respiratory droplets and person-to-person contact, and there were no cases of presymptomatic individuals transmitting disease. Between November 2002 and July 2003, a total of 8098 people worldwide became ill with probable SARS-CoV; of these, 774 died. In the United States, 8 people who had traveled to SARS-CoV transmission areas got the disease, but none died. There were no cases after July 2003, and the global outbreak was declared over. In April 2004, the Chinese Ministry of Health reported new cases, but there is no evidence of wider transmission in the community.
The current disease named COVID-19 is caused by SARS-CoV-2 virus, a related but much more contagious coronavirus, which can be spread by presymptomatic/asymptomatic individuals. The first case was identified in China at the end of 2019, which is why this disease is called COronaVIrusDisease-2019. SARS-CoV-2 is very similar to known SARS-related coronaviruses in bats, especially horseshoe bats. It is believed that a bat virus mutated, infected an intermediate host, such as a civet or pangolin, and then mutated again, in a process called spillover, to be able to infect humans. The human form spreads via coughing, sneezing, and other contact. On March 11, 2020, COVID-19 was declared a pandemic by the World Health Organization.
Despite various degrees of lockdowns and closures worldwide, as of September 2020, there have been over 31.2 million confirmed cases of COVID-19 and 962,000 confirmed COVID-19 deaths, with cases reported in every country.2 In the United States, there have been 6.9 million cases and 200,000 deaths. These numbers are given with the understanding that the variability in testing can skew figures and positivity rates, and the death rates do not include deaths due to failure to access health care for other reasons (for example, myocardial infarction or cerebrovascular accident) due to COVID-19 closures and fears. Over 900 health care workers in the United States have died of COVID-19.3 Initial reports suggested that Otolaryngologists and Ophthalmologists were at higher risk of contracting this disease from their patients due to close exposure4; even with personal protective equipment, front-line health care workers have a 3 to 4 times increased risk of testing positive for COVID-19.5
The main symptoms encountered in COVID-19 are fever or chills, cough, shortness of breath or difficulty breathing, fatigue, muscle or body aches, headache, new loss of taste or smell, sore throat, congestion or runny nose, nausea or vomiting, and diarrhea. Emergency warning signs of this disease include dyspnea, chest pain or pressure, confusion, severe lethargy or stupor, and cyanosis.6 We are finding “happy hypoxemia” in COVID-19, that is, very low blood oxygenation but no sense of dyspnea. This can lead to delays in seeking care, and its cause remains to be elucidated.7 Many individuals have subsequently acquired pulse oximeters for use at home. While most cases of COVID-19 are self-limited and recovery is generally seen over a few days to 2 weeks, there are people with long-term issues of fatigue, cough, dyspnea, headache, joint pain, cardiopulmonary issues, blood-clotting abnormalities, cognitive and emotional issues; these people are thought to have “Long Covid,” and much more remains to be learned about them.
By following the 3 W’s: Wear a mask, Wash your hands, Watch your distance (maintain 6 feet from others not living in your home), some countries, states, and communities have brought their SARS-CoV-2 positivity rates down well below 1%, making reopenings possible. Unfortunately, even those successes can be undermined when people stop following that advice. In addition, as we are opening, we are using symptom and temperature screenings in physicians’ offices, hospitals, schools, and so forth. COVID-19 occurring at this time has provided an opportunity to reach out via Social Media and provide teaching. I even started a YouTube channel, Dr Sujana (https://www.youtube.com/c/DrSujana) that has educational videos about COVID-19, and a livestream show called “She’s On Call” (https://www.youtube.com/c/DrSujana), where we discuss COVID-19 and other health issues. Please feel free to share them with your patients.
As for educating each other, Dr Zara Patel, the Guest Editor of Special Articles: Otolaryngology in COVID-19 in this issue of Otolaryngologic Clinics of North America, has been at the forefront of identifying and explaining otolaryngologic manifestations of this disease and how ENT surgeons can protect ourselves and our staff members while caring for our patients. I am grateful to her for compiling the next 4 articles to encompass what we know at this point regarding this novel coronavirus disease. The authors of these articles have risen to the challenge of writing about a disease process that is evolving rapidly in real time. We hope that you find this special section useful as we all navigate our way in this global pandemic.
References
- 1.https://www.cdc.gov/sars/about/faq.html Available at: Accessed September 8, 2020.
- 2.https://www.who.int/emergencies/diseases/novel-coronavirus-2019 Available at: Accessed September 8, 2020.
- 3.https://khn.org/news/exclusive-over-900-health-workers-have-died-of-covid-19-and-the-toll-is-rising/ Available at: Accessed September 8, 2020.
- 4.Husain I.A. 2020. https://blogs.scientificamerican.com/observations/why-covid-19-is-a-special-danger-to-otolaryngologists/. April 24 Available at: Accessed September 8, 2020.
- 5.Nguyen L.H., Drew D.A., Graham M.S. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health. 2020;5(9):e475–e483. doi: 10.1016/S2468-2667(20)30164-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html Available at: Accessed September 8, 2020.
- 7.González-Duarte A., Norcliffe-Kaufmann L. Is 'happy hypoxia' in COVID-19 a disorder of autonomic interoception? A hypothesis. Clin Auton Res. 2020;30(4):331–333. doi: 10.1007/s10286-020-00715-z. [DOI] [PMC free article] [PubMed] [Google Scholar]


