Abstract
BACKGROUND: Common techniques, including photography and subjective assessments, have been used to measure the efficacy of skin rejuvenation treatments. However, the efficacy of skin treatments can be difficult to assess, particularly when the effects are gradual or subtle. OBJECTIVE: This study investigated the effectiveness of a skincare regimen for skin rejuvenation that employs comprehensive solar protection, ranging from ultraviolet through to near-infrared radiation, and nightly repair of photodamage, and clarified the difference in the results relative to other lifting medical procedures. METHODS: Twenty Japanese patients were enrolled in this study. The participants used topical skincare products (The Essential Six; RATIONALE, Victoria, Australia) for six months. Patients did not use any other skincare formulations and did not undergo any form of aesthetic procedures during the study. A superimposed three-dimensional volumetric assessment and quantification of three-dimensional skin surface displacement with vectors were performed at baseline and after six months of treatment with the topical skincare products. RESULTS: Improvements in skin texture and clarity as recorded via digital photography and volumetric reduction was observed relative to pretreatment in all patients. All patients self-reported skin rejuvenation, tightening, and lifting. Most vectors suggested three-dimensional skin surface displacement at the forehead, lateral sides of the cheek, and around the chin. CONCLUSION: Skin tightening and lifting effects are not synonymous. The results of this study suggest the solar-specfic skincare formulations evaluated here constitute a safe and effective means of skin rejuvenation and tightening.
Keywords: Rejuvenation, skin surface displacement, solar protection, solar repair, sunscreen, volumetric reduction
Incident solar energy is composed of less than 10 percent ultraviolet (UV) radiation, approximately 40 percent visible light (VL), and more than 50 percent near-infrared (NIR) radiation.1 Despite widespread sunscreen use by the global population, skin diseases, skin cancer, and photoaging continue to pose a health threat worldwide.1,2 More than 90 percent of the solar energy reaching the surface of the Earth consists of VL and NIR; intensive or ongoing exposure of VL and NIR, when combined with UV, also contributes to skin cancer and photoaging.1,2
Regarding NIR, the author has previously reported that solar NIR acts as an aging factor, where biological NIR protection is impaired and intensive or long-term exposure to solar NIR induces deleterious effects similar to those of UV.3–6 The sequela of solar NIR exposure include photoaging, long-lasting vasodilation, muscle thinning, skin ptosis, sagging, and potentially, photocarcinogenesis.7–10
The author has previously reported that commercially widespread sunscreens (SPF50+, PA+++ or PA++++) cannot block VL and NIR sufficiently and that skin rejuvenation could be finally achieved by extensive solar protection ranging from UV through to NIR and nightly repair of photodamage.1 Surprisingly, the global sunscreen industries have not yet created effective products blocking from UV through to NIR.
Regardless of age and skin type, rejuvenation is one of the most frequent requests in the aesthetic field. Although rejuvenating effects of various medical or cosmetic procedures have been reported extensively by previous studies, quantification of three-dimensional (3D) skin surface displacement with vectors has not been considered.
In this study, the author evaluated the efficacy of comprehensive solar protection, ranging from UV through to NIR, and nightly repair of photodamage using 3D volumetric assessment and the quantification of 3D skin surface displacement with vectors.
METHODS
Participants. Twenty Japanese patients (17 females and three males) aged 22 to 71 years (mean age: 40.8±14.3 years) with Fitzpatrick Skin Types III to V were enrolled in the study. All of the patients had visited Clinica Tanaka Plastic, Reconstructive Surgery and Anti-aging Center seeking improved skin health and rejuvenation. None of the participants reported any skin diseases or had undergone cosmetic treatments affecting the treatment zone within two years of this study. Patients were instructed not to use any other skincare products or undergo any aesthetic procedures during the course of this investigation and to continue with their normal diet throughout the study. The approval of an ethics committee was not required, since this study involved a retrospective review of previously treated patients.
Patients who lost weight during the study period were excluded from the study, as changes in this variable could affect the results. All patients signed an informed consent form approving their inclusion following an explanation of the study design and execution and agreed to the publication of results and images.
Topical skincare approach. The Essential Six (RATIONALE, Victoria, Australia) was used in this study. The Essential Six represents a comprehensive topical approach to environmental protection and repair of the skin, encompassing the solar spectrum (approximately 290–3,200nm) and the effects of various biochemical reactions and desiccation. The Essential Six consists of three solar protective formulations (Immunologist Serum, Antioxidant Serum, and Photodynamic Day Cream) to be applied in the morning and three solar repair formulations (Proceramide Cleanser, Catalyst Serum, and DNA Night Cream) to be applied at night. Patients applied the products to their facial skin for six months as directed by a physician without any other skincare products or medical treatment. Further information on the formulations can be found in Table 1.
Objective assessments. 3D imaging was performed as an objective assessment, acquired with a VECTRA Handy Camera and VECTRA software (Canfield Scientific Inc., Fairfield, New Jersey). This system can capture changes in skin topographic data as well as two-dimensional (2D) color representations. The camera sequence of image capture was calibrated to less than 3ms to accurately record facial topography, even if the subject could not maintain perfect stillness. Differences in facial tissue volume between pre- and posttreatment were demonstrated via 3D schematics, with relative degrees of skin tightening being represented by yellow to red zones (red, -5 mm change). Areas of no change in the face were illuminated as green zones.
The VECTRA software also measured local changes in 3D skin surface position with vectors.
These assessments were performed up to six months after treatment, with patients directed to maintain the same neutral facial expression for accuracy during all image capture sessions.
RESULTS
Marked improvements in skin texture and clarity were observed in 2D color digital photographs relative to the pretreatment for all patients (Figures 1A and 1B– 5A and 5B).
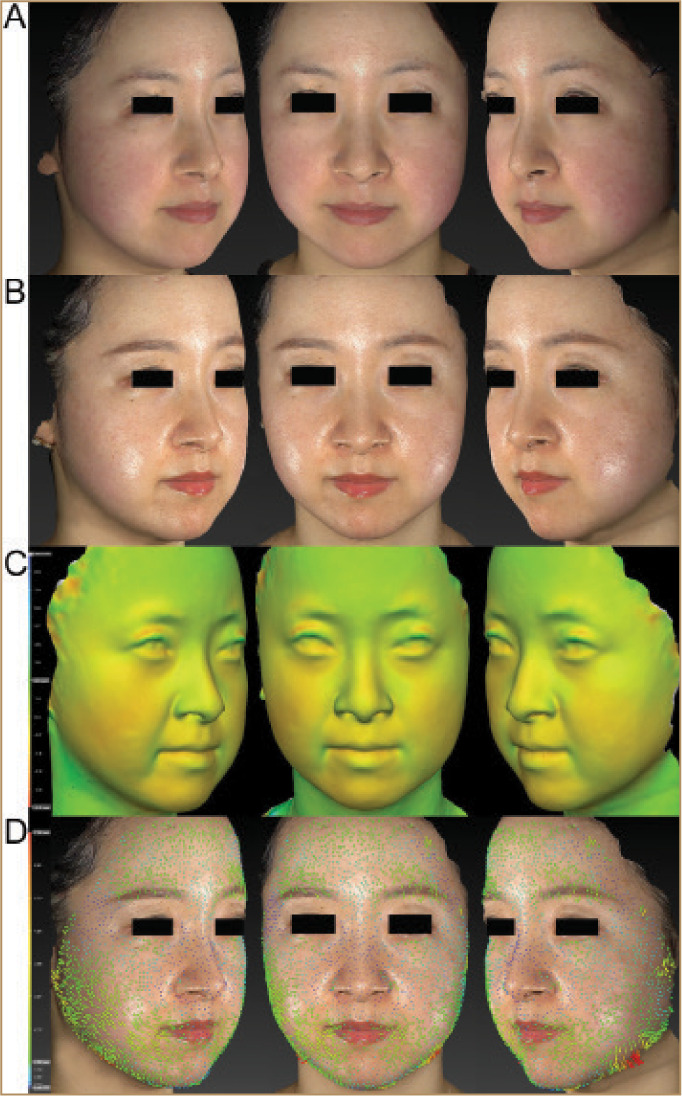
FIGURE 1.
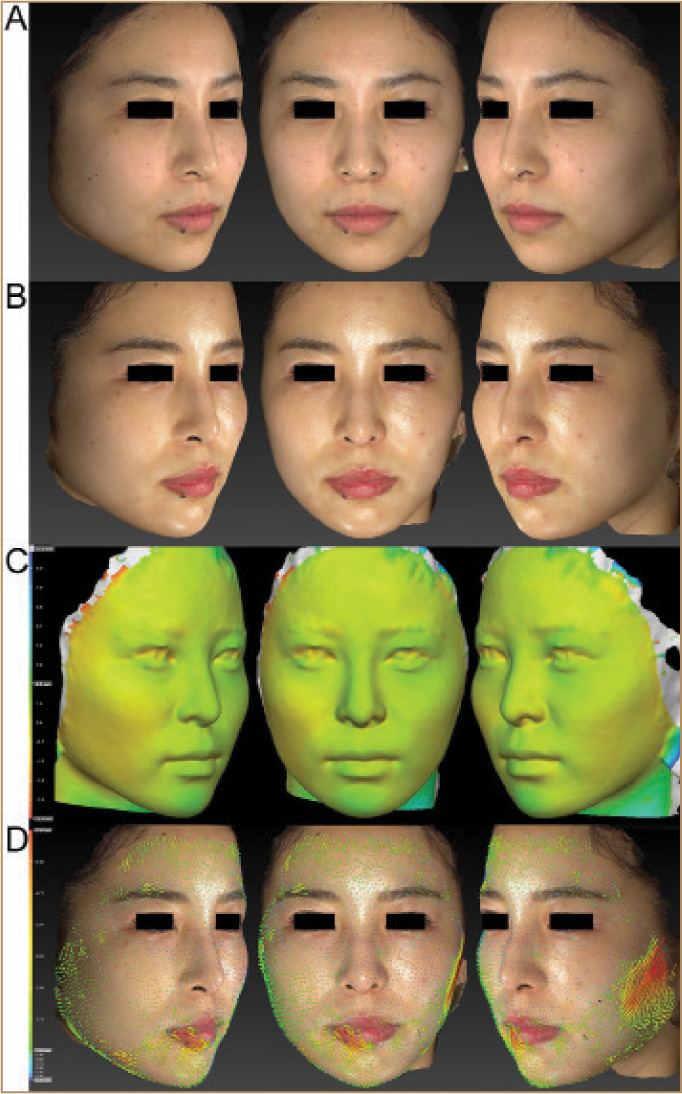
A 22-year-old Japanese female; images from top to bottom show: A) pretreatment, B) six months posttreatment, C) superimposed 3D volumetric assessment comparing pre- and six months posttreatment, and D) quantification of 3D skin surface displacement with vectors comparing pre- and six months posttreatment. Marked improvements of skin texture and clarity were observed in 2D color digital photographs relative to pretreatment (A, B). Reductions in 3D volumetric assessment outcomes were observed when compared with pretreatment (C). The varying degrees of tightening achieved are shown in colors yellow to red (-5.0 mm). Green areas indicate areas what remained unchanged. Each point of the skin surface at the forehead, periorbital areas, and medial sides of the cheek was 3D displaced in a centripetal direction (D). The varying degrees of the 3D movement of the skin are shown in colors blue (0.3mm) to red (6.2mm). Green vectors indicate areas that were 3D displaced from 1.0mm to 2.5mm.
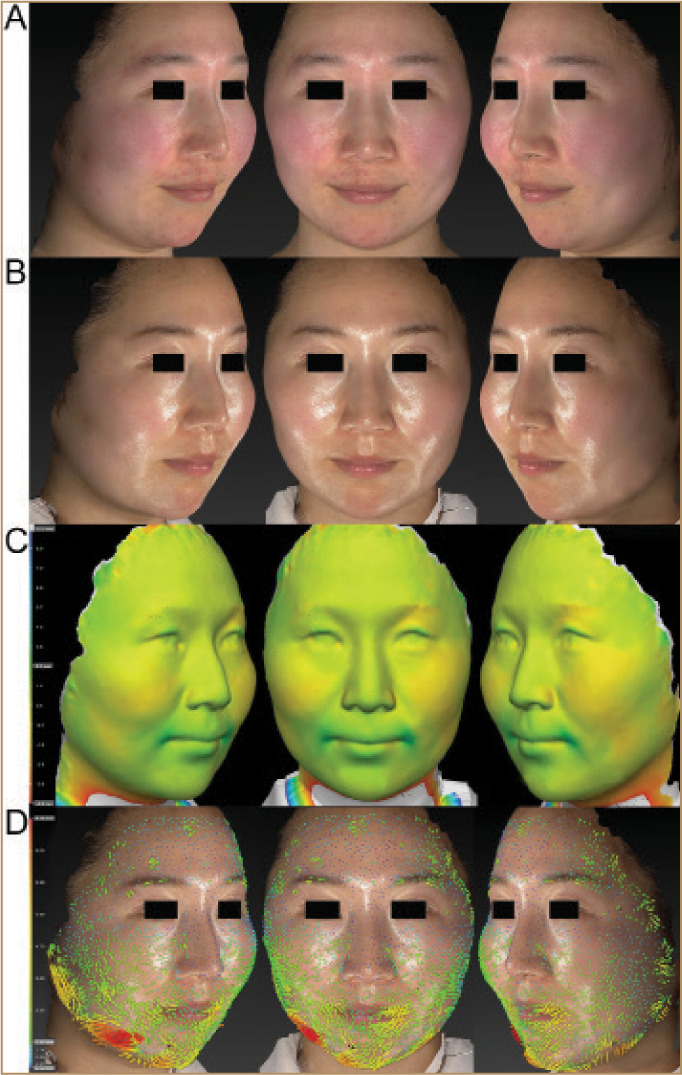
FIGURE 5.
A 42-year-old Japanese female; marked improvements in skin texture, redness, and clarity were observed in 2D color digital photographs relative to pretreatment (A, B). Tightening effects on the lower half of the face and perioral area were observed during 3D volumetric assessment (C). Each point of the skin surface in the forehead, cheeks, and perioral area was 3D displaced in a centripetal direction (D). The varying degrees of 3D movement of the skin are shown in colors blue (0.4 mm) to red (4.3 mm). Green vectors indicate areas that three-dimensionally displaced from 1.0 to 2.0mm.
A reduction in 3D volumetric assessment outcomes was observed compared to pretreatment in all patients (Figures 1C, 2C, 3C, 4C, 5C). Skin-firming effects shown in orange were induced in the lower two-thirds of the face, including in the perioral area and lower cheek.
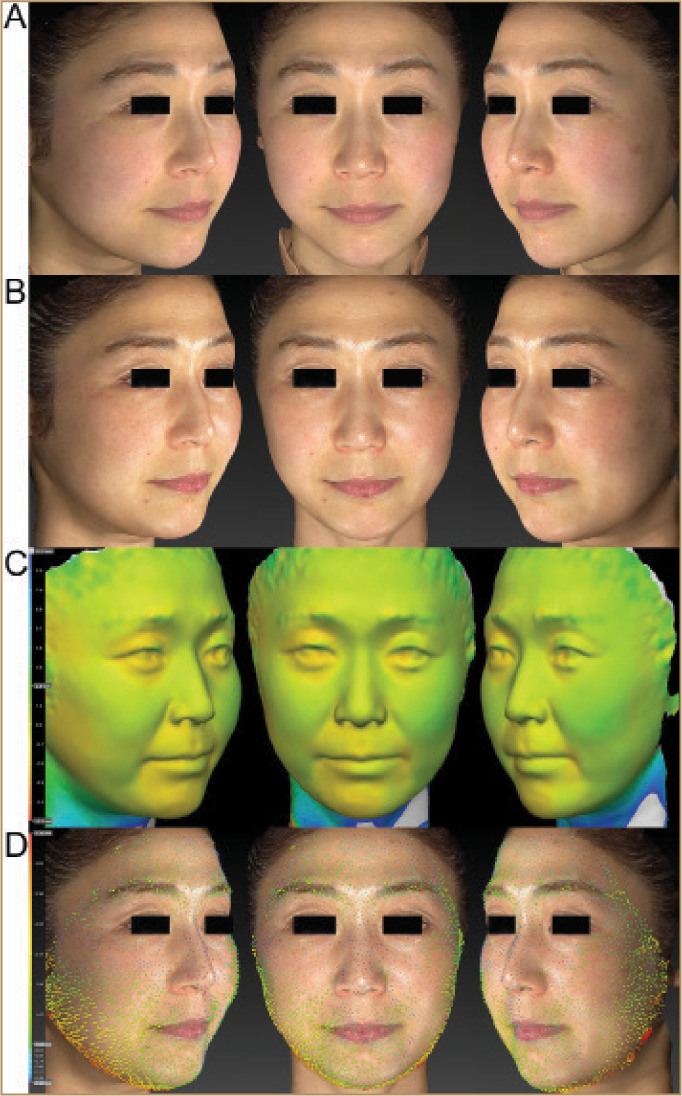
FIGURE 2.
A 25-year-old Japanese female; marked improvements in skin texture and clarity were observed in 2D color digital photographs relative to pretreatment (A, B). Tightening effects on the lower half of the face and perioral area were observed during 3D volumetric assessment (C). Each point of the skin surface at the forehead, periorbital areas, and medial sides of the cheek was 3D displaced in a centripetal direction (D). The vectors in the perioral area indicate downward. The varying degrees of 3D movement of the skin are shown in colors blue (0.7mm) to red (9.3mm). Green vectors indicate areas that were 3D displaced from 1.7 to 3.9mm.
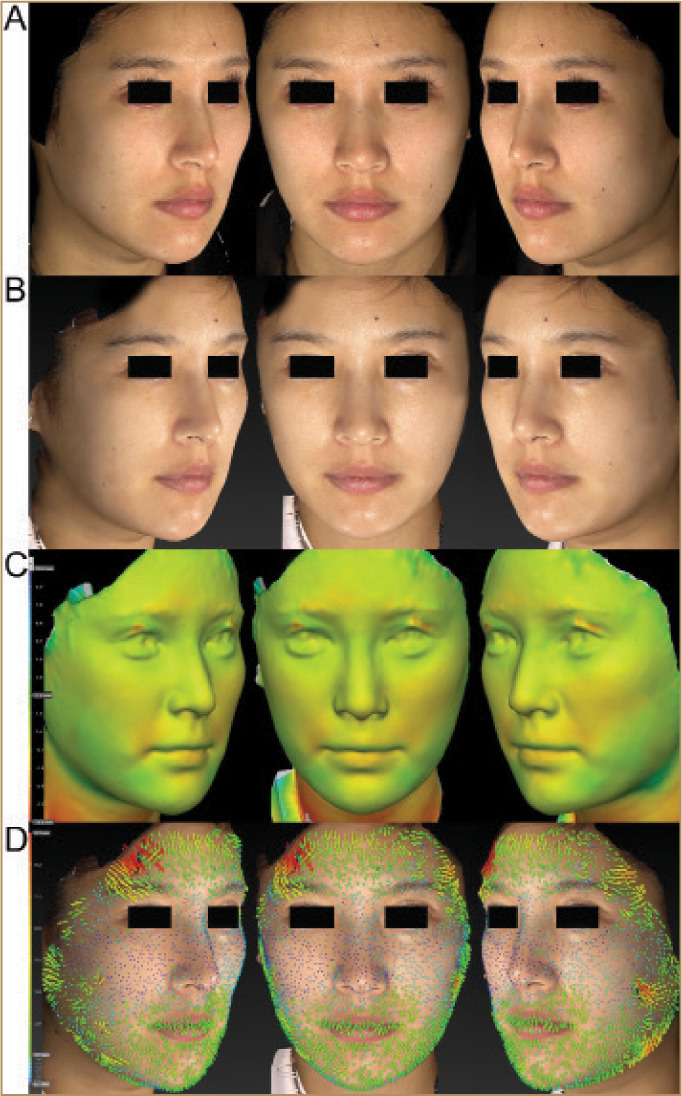
FIGURE 3.
A 27-year-old Japanese female; marked improvements in skin texture, redness, and clarity were observed on 2D color digital photographs relative to pretreatment (A, B). Tightening effects on the lower half of the face were observed during 3D volumetric assessment (C). Each point of the skin surface in the perinasal area and the cheeks was 3D displaced in a centripetal direction (D). The vectors in perioral area indicate downward. The varying degrees of the 3D movement of the skin are shown in colors blue (0.5mm) to red (9.1mm). Green vectors indicate areas that were 3D displaced from 1.4 to 3.6mm.
FIGURE 4.
A 37-year-old Japanese male; marked improvements in skin texture, redness, and clarity were observed on 2D color digital photographs relative to pretreatment (A, B). Tightening effects on the lower two-thirds of the face as well as the lower cheeks and peri-oral area were observed during 3D volumetric assessment (C). Each point of the skin surface on the forehead, periorbital areas, and cheeks was 3D displaced in a centripetal direction (D). The vectors in the perioral area indicate downward. The varying degrees of 3D movement of the skin are shown in colors blue (0.6mm) to red (7.5mm). Green vectors indicate areas that were 3D displaced from 1.3 to 3.1mm.
Most vectors showing 3D displacement of each point of the skin surface indicated centripetal movement, although patients and the author predicted that vectors would have indicated upwards (Figures 1D, 2D, 3D, 4D, 5D). Each point of the skin surface at the forehead, lateral sides of the cheek, and around the chin was 3D displaced in a centripetal direction. Displacement of the central area of the face encompassing the orbital, periorbital, nasal, perinasal, medial sides of the cheek was subtle but detectable. These results were sustained for six months. No treatment-related adverse events were observed. All patients reported that their skin looked and felt rejuvenated, tightened, and lifted.
DISCUSSION
Improvements in skin texture, clarity, and laxity are among the most frequent requests from patients seeking medical procedures, including face-lifting and laser or light therapies. Aggressive procedures, such as face-lifts, laser resurfacing, and ablative procedures have not been widely accepted among Japanese patients due to their potential risks and downtime.1 Laser or light treatments can provide the requested improvements when patients are treated continuously at clinics. However, these treatments are often accompanied by inflammation and downtime.
This skincare regimen examined in the present study provided improvements in skin texture, clarity, and laxity as measured through 2D and 3D assessments and satisfied most of the patients, even though the treatment was performed by the patients themselves at home. As the biological effects of solar energy (UV, VL and NIR) are significant,11–15 this skincare approach appeared to be effective in preventing and repairing photoaging.1 The results shown through objective investigation in this and prior studies were impressive and most of the patients were extremely satisfied with the results.1
Reductions in 3D volumetric assessment outcomes were observed when compared to pretreatment in all patients. Skin-firming effects were noted mainly in the lower two-thirds of the face, including the perioral area and lower cheek, which appeared to be preferable and satisfied the patients. The volumetric reduction and skin-tightening effects appeared to be similar to those seen with other medical procedures, such as NIR and radiofrequency approaches. However, the present skincare regimen provided skin-tightening effects without thermal stimulation of collagen production, edematous reactions, or thermal damage to the dermis.1
Procedures such as face-lifts, thread-lifts, and fillers can lift the skin and subcutaneous tissue, but cannot provide skin rejuvenation. The results induced by the comprehensive solar protection ranging from UV through to NIR and nightly repair of photodamage appeared to be different from those induced by face-lift, thread-lift, and filler procedures. Although the author predicted a vertical displacement in vectors, 3D movement of skin was observed to be centripetal at each point of the forehead, lateral sides of the cheek, and around the chin. This stands in contrast with both the marked upward vector displacement seen in surgical face lifts and thread lifting and the obvious centrifugal changes produced by injectable fillers. Data also revealed subtle centripetal displacement of the central areas of the face, including orbital, periorbital, nasal, perinasal, and medial sides of the cheek. Interestingly, all patients reported a satisfaction with a generalized sense of lifting. These results appear to be affected by the skin thickness and bone structures. Further studies are needed to investigate the mechanisms of this 3D centripetal displacement.
The skincare regimen evaluated here is pain-free and convenient, with results that appear to parallel invasive medical treatments. Although significant improvements in skin conditions were observed following treatment with the evaluated skincare regimen for six months, further investigations are needed to discern whether additional treatment or topical actives might be even more effective in skin rejuvenation and prevention of photoaging. Limitations. The absence of a control group and a comparison study may limit the significance of these findings. Additionally, it is acknowledged that this a preliminary study encompassing a relatively small number of patients. Further evaluations are needed involving larger numbers of patients to evaluate variations in treatment parameters. Moreover, lifestyle choices, including diet, alcohol, salt intake, and exercise and sleep patterns might influence the outcomes reported in this study.
CONCLUSION
The present skincare approach, consisting of daily solar protection from UV to NIR and nightly solar repair, represents a safe and highly efficacious treatment for solar damage and skin aging without inflammation and tissue damage and is recommended as a regimen for skin rejuvenation and the prevention of photoaging. Marked improvement in skin texture and clarity, volumetric reduction, skin-firming effects, and 3D centripetal skin surface displacement were observed through 2D and 3D assessments.
The advantages and clinical benefits of this approach suggest it could be easily adopted and may garner widespread use by patients regardless of age, sex, or skin type.
ACKNOWLEDGMENTS
I thank Richard Parker and Joshua Gosling from RATIONALE for formulation information relating to the skincare regimen used in the study and their helpful comments.
REFERENCES
- Tanaka Y. Long-term objective assessments of skin rejuvenation using solar protection and solar repair shown through digital facial surface analysis and three-dimensional volumetric assessment. Clin Cosmet Investig Dermatol. 2019;12:553–561. doi: 10.2147/CCID.S218176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanaka Y. Presented at the Nonsurgical Symposium. Gold Coast; Australia: 2018. Photoprotection update. June 15. [Google Scholar]
- Tanaka Y. The impact of near-infrared radiation in dermatology. World J Dermatol. 2012;1:30–37. [Google Scholar]
- Tanaka Y, Gale L. Beneficial applications and deleterious effects of near-infrared from biological and medical perspectives. Optics and Photonics Journal. 2013;3:31–39. 4A. [Google Scholar]
- Tanaka Y, Gale L. Protection from near-infrared to prevent skin damage. Optics and Photonics Journal. 2015;5(4):113–118. [Google Scholar]
- Tanaka Y, Nakayama J. Up-regulated epidermal growth factor receptor expression following near-infrared irradiation simulating solar radiation in a 3Dimensional reconstructed human corneal epithelial tissue culture model. Clin Interv Aging. 2016;11:1027–1033. doi: 10.2147/CIA.S111530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanaka Y, Matsuo K, Yuzuriha S. Long-lasting muscle thinning induced by infrared irradiation specialized with wavelengths and contact cooling: a preliminary report. ePlasty. 2010;10e40:327–335. [PMC free article] [PubMed] [Google Scholar]
- Tanaka Y, Matsuo K, Yuzuriha S. Long-lasting relaxation of corrugator supercilii muscle contraction induced by infrared irradiation. ePlasty. 2010;11:42–49. e6. [PMC free article] [PubMed] [Google Scholar]
- Tanaka Y, Matsuo K, Yuzuriha S. Near-infrared irradiation non-thermally affects subcutaneous adipocytes and bone. ePlasty. 2010;11:97–105. e12. [PMC free article] [PubMed] [Google Scholar]
- Tanaka Y, Matsuo K, Yuzuriha S. Near-infrared irradiation non-thermally induces long-lasting vasodilation by causing apoptosis of vascular smooth muscle cells. ePlasty. 2011;11:203–211. e22. [PMC free article] [PubMed] [Google Scholar]
- Schieke SM, Schroeder P, Krutmann J. Cutaneous effects of infrared radiation: from clinical observations to molecular response mechanisms. Photodermatol Photoimmunol Photomed. 2003;19(5):228–234. doi: 10.1034/j.1600-0781.2003.00054.x. [DOI] [PubMed] [Google Scholar]
- Tanaka Y, Tsunemi Y, Kawashima M et al. Objective assessment of skin tightening using water-filtered near-infrared (1000-1800 nm) device with a contact cooling and freezer stored gel in Asians. Clin Cosmet Investig Dermatol. 2013;6:167–176. doi: 10.2147/CCID.S47299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanaka Y, Motomura H, Jinno M. Biological defenses against ultra-violet, visible light, and near-infrared exposure. Optics and Photonics Journal. 2016;6(1):8–14. [Google Scholar]
- Calderhead G, Tanaka Y. London, England: IntechOpen; 2017. Photobiological basics and clinical indications of phototherapy for skin rejuvenation. In: Photomedicine: Advances in Clinical Practice. pp. 215–252. [Google Scholar]
- Tanaka Y. Nakayama J. Up-regulated expression of La ribonucleoprotein domain family member 6 and collagen type I gene following water-filtered broad-spectrum near-infrared irradiation in a 3Dimensional human epidermal tissue culture model as revealed by microarray analysis. Australas J Dermatol. 2018;59(2):e87–e92. doi: 10.1111/ajd.12604. [DOI] [PubMed] [Google Scholar]


