Abstract
Ulcerative colitis, a chronic and recurrent inflammatory disease, is localized to the colonic mucosa but can affect other organs and lead to various complications. Gastroduodenitis associated with ulcerative colitis has been reported. However, little is known about esophageal ulcers. We herein report two rare cases of esophageal ulcers associated with ulcerative colitis. Furthermore, the clinical and histological characteristics of 18 previously reported cases are summarized. This case series and literature review will encourage the accurate diagnosis and treatment of esophageal ulcers associated with ulcerative colitis.
Keywords: ulcerative colitis, esophageal ulcer, manifestation
Introduction
Ulcerative colitis (UC) is primarily a disease of the colon; however, extracolonic manifestations have been described. Extracolonic manifestations particularly involve the blood, joints, skin, biliary tracts, liver, kidneys, lungs, and upper digestive tract (1). Gastroduodenitis associated with UC (GDUC) has been noted in 7.6% of severe cases of UC (2, 3), making it a common extracolonic manifestation of UC. In contrast, there have been relatively few reports of esophageal ulcer occurring as an extracolonic manifestation of UC (4).
We herein report two cases of UC complicated with esophageal ulcers. Furthermore, we review 18 previously reported cases of esophageal ulcers associated with UC. We summarize these cases to help characterize esophageal ulcer occurring as a complication of UC.
Case Reports
Case 1
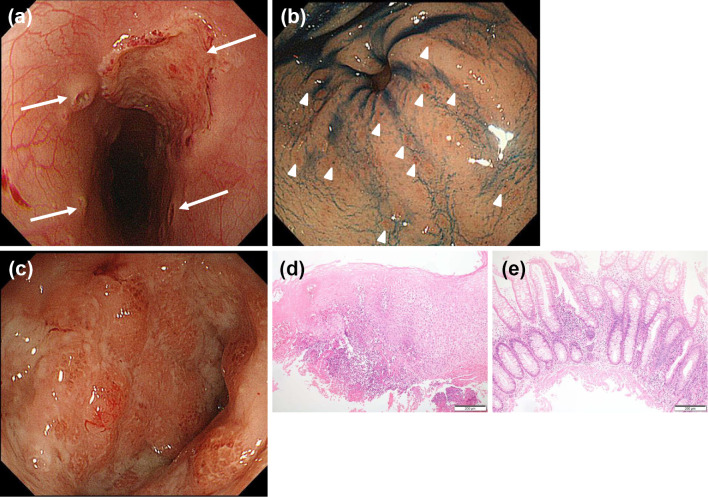
A 16-year-old girl presented with chest pain and diarrhea with blood and mucus. No oral, genital ulcers or skin lesions were evident. Esophagogastroduodenoscopy (EGD), showed an ulcer with aphthae in the esophagus (Fig. 1a) and diffuse aphthae in the stomach (Fig. 1b). A histological examination of the esophageal ulcers showed severe inflammatory cell infiltration (Fig. 1d), and the gastric erosions revealed focally enhanced gastritis. Colonoscopy revealed superficial ulcers and mucosal friability (Fig. 1c) from the rectum to the cecum. The terminal ileum was normal. In the histological examination, inflammatory cell infiltration with cryptitis was detected in the sigmoid colon and rectum (Fig. 1e); therefore, pancolitis-type UC was diagnosed comprehensively.
Figure 1.
Esophagogastroduodenoscopy (EGD), colonoscopy, and their pathological findings. (a) EGD showing an ulcer with aphthae (arrows) in the mid intrathoracic esophagus. (b) EGD showing widespread aphthae (arrowheads) at the antrum. (c) Colonoscopy showing erythema and mucosal friability in the sigmoid colon. (d) Biopsy specimen from the esophageal ulcers showing severe inflammatory cell infiltration [Hematoxylin and Eosin (H&E) staining, ×100]. (e) Biopsy specimen from the colon showing inflammatory cell infiltration with cryptitis in the rectum (H&E staining, ×100).
She was not taking any medicine, including non-steroidal anti-inflammatory drugs, and Helicobacter pylori infection was not confirmed. A serological examination of viral infections (varicella zoster virus, herpes simplex virus, cytomegalovirus, and Epstein-Barr virus-DNA) was also negative. Therefore, esophageal ulcers and gastroduodenitis associated with UC (GDUC) were diagnosed.
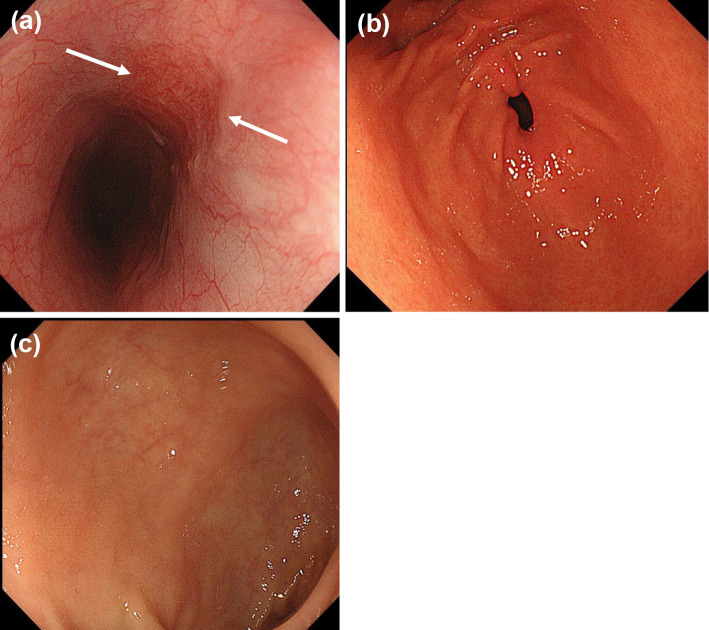
Treatment with intravenous prednisolone (60 mg/day) was started, and her chest pain and diarrhea were resolved in a few days. EGD on the seventh day showed healing of the esophageal ulcers (Fig. 2a) and gastroduodenal aphthae (Fig. 2b). Colonoscopy showed improvement in the inflammation of the colon (Fig. 2c). She has experienced no relapse for two years.
Figure 2.
Esophagogastroduodenoscopy (EGD) and colonoscopic findings. (a) EGD showing marked healing of the esophageal ulcers (arrows). (b) EGD showing healing of the gastroduodenal aphthae. (c) Colonoscopy showing improvement of mucosal edema and vascular appearance of the sigmoid colon.
Case 2
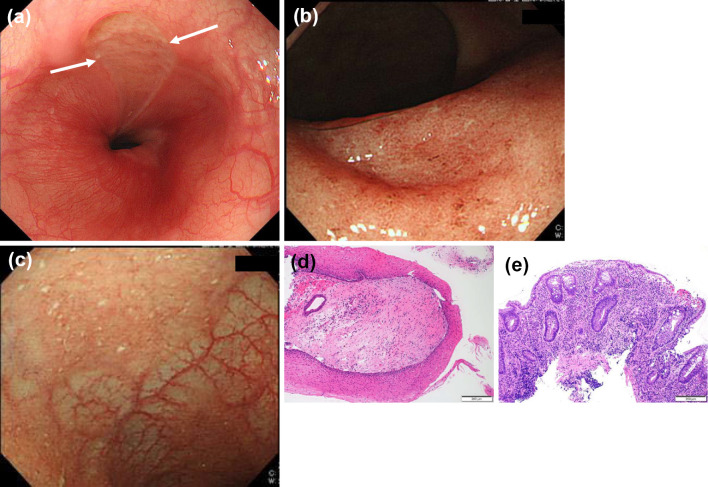
A 19-year-old woman was admitted to our hospital due to bloody stool and chest pain on swallowing. She was not taking any medication. Laboratory tests showed hypoalbuminemia, mild anemia and inflammatory responses: total protein (6.9 g/dL), albumin (2.8 g/dL), hemoglobin (10.1 g/dL), white blood cell (4,140/mm3), mild neutrophilic leukocytosis (61.6%), thrombocytosis (platelets 28.9×104/μL), and increased C-reactive protein levels (6.88 mg/dL). Stool cultures were normal. Serological assays for viruses, including herpes simplex, cytomegalovirus, varicella, and Epstein-Bar did not demonstrate primary infection. Because of her mouth and chest pain symptoms, EGD was performed, showing a longitudinal ulcer in the lower esophagus (Fig. 3a) and oral ulcers. Histologic findings showed infiltration of inflammatory cells in the epithelia (Fig. 3d). Colonoscopy showed superficial ulcers and mucosal friability (Fig. 3b) in the entire colon, from the rectum to the cecum. We also detected mucosal friability in the terminal ileum (Fig. 3c). The histologic findings here showed inflammatory cell infiltration with basal plasmacytosis in the transverse colon and inflammatory cell infiltration with cryptitis in the rectum (Fig. 3e). She was diagnosed with esophageal ulcer complicated with pancolitis-type UC comprehensively.
Figure 3.
Esophagogastroduodenoscopy (EGD), colonoscopy, and their pathological findings. (a) EGD showing a longitudinal ulcer in the lower esophagus. (b) Colonoscopy showing mucosal friability in the rectum. (c) Colonoscopy showing mucosal friability in the terminal ileum. (d) Biopsy specimen from the esophageal ulcers showing infiltration of inflammatory cells in the epithelia [Hematoxylin and Eosin (H&E) staining, ×100]. (e) Biopsy specimen from the rectum showing inflammatory cell infiltration with basal plasmacytosis and cryptitis (H&E staining, ×100).
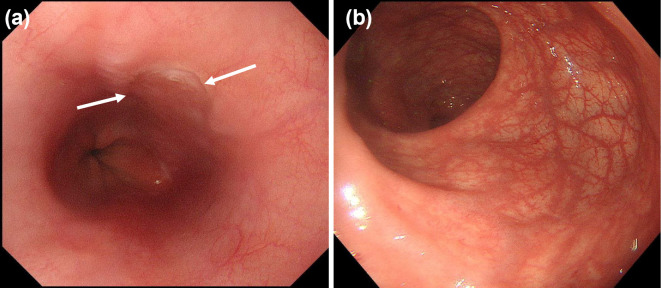
Induction therapy was started with intravenous prednisolone (50 mg/day). Thereafter, her bloody stool and pain on swallowing improved within one week. EGD after four weeks showed healing of the oral and esophageal ulcers (Fig. 4a). Colonoscopy after four weeks also showed complete remission (Fig. 4b). She has shown no relapse of esophageal lesions for one year.
Figure 4.
Esophagogastroduodenoscopy (EGD) and colonoscopic findings. (a) EGD showing healing of the esophageal ulcers. (b) Colonoscopy showing remission of the rectum.
Discussion
In 1961, Margoles et al. (5) first reported a case of pancolitis-type UC with esophagitis. There have been 18 reported cases of esophageal ulcers associated with UC, and we encountered 2 new cases ourselves. The previously reported cases of esophageal ulcers associated with UC (case 3 to 20) and our new cases (case 1 and 2) are summarized in Tables 1-3.
Table 1.
Clinical Data of UC Patients with Esophageal Ulcer.
| Case (No) |
Ref No. |
Age (yrs) |
Sex | Duration of UC |
UC phase | Type | UC treatment |
|---|---|---|---|---|---|---|---|
| 1 | Ours | 16 | F | 0 | Active | Total | PSL |
| 2 | Ours | 19 | F | 0 | Active | Total | PSL |
| 3 | 6 | 15 | M | 2 years | Remission | Left side | PSL, SASP |
| 4 | 7 | 23 | M | 5 years | Remission | Total | PSL, SASP |
| 5 | 8 | 21 | F | 0 | Active | N/A | PLS, SASP |
| 6 | 19 | M | 0 | Active | N/A | N/A | |
| 7 | 10 | 47 | F | 0 | Active | Right side | 5ASA |
| 8 | 4 | 18 | F | 7 years | Relapse Active | Total | SASP |
| 9 | 11 | 18 | M | 1 year | Active | Left side | PSL, 5ASA |
| 10 | 12 | 19 | M | 0 | Active | Total | none |
| 11 | 13 | 51 | M | 0 | Active | Total | PSL, 5ASA |
| 12 | 14 | 33 | M | 0 | Active | Total | PSL, LCAP |
| 13 | 15 | 52 | F | 3 years | Relapse Active | Left side | SASP |
| 14 | 5 | 28 | M | 17 years | Post operation | Total | Total colectomy and ileostomy |
| 15 | 8 | 26 | M | 2 months | Post operation | Total | Sbtotal colectomy and ileostomy |
| 16 | 14 | F | 5 years | Post operation | Total | Sbtotal colectomy and ileostomy | |
| 17 | 24 | M | 9 years | Post operation | Total | Total proctocolectomy | |
| 18 | 9 | 21 | M | 3 years | Post operation | Total | Total colectomy and ileostomy |
| 19 | 16 | 47 | M | 21 years | Post operation | N/A | Sbtotal colectomy and ileostomy |
| 20 | 53 | M | N/A | Post operation | Total | Sbtotal colectomy |
UC: ulcerative colitis, N/A: data not available, PSL: prednisolone, SASP: salazosulfapyridine, 5-ASA: 5-aminosalicylic acid, F: female, M: male
Table 2.
Clinical Data of UC Patients with Esophageal Ulcer.
| Case (No) | Esophagial ulcer (EU) | Location | EU symptoms |
|---|---|---|---|
| 1 | An esophageal ulcer with aphthae | Middle esophagus | Chest pain |
| 2 | Longitudinal oesophageal ulcer | Lower esophagus | Chest pain on swallowing |
| 3 | Severe esophagitis | Lower esophagus | Parasternal chest pain and dysphagia |
| 4 | Shallow ulceration with gross diffuse irregularity and polyp formation | Middle and lower esophagus | Dysphagia |
| 5 | Active ulcerative esophagitis | N/A | N/A |
| 6 | Marked ulcerative esophagitis | N/A | Substenal pain and dysphagia |
| 7 | Multiple irregular esophageal ulcers | Whole esophagus | Anterior chest pain and dysphagia |
| 8 | Longitudinal oesophageal ulcer with haemorrhage | Middle and lower esophagus | Sore throat and pain on swallowing |
| 9 | Punched-out esophageal ulcer | Middle esophagus | Sore throat and anterior chest pain |
| 10 | Punched-out esophageal ulcer | Middle esophagus | General fatigue |
| 11 | Punched-out esophageal ulcer | Middle and lower esophagus | Anterior chest pain on swallowing |
| 12 | Punched-out esophageal ulcer | Middle and lower esophagus | Anterior chest pain and dysphagia |
| 13 | Punched-out esophageal ulcer | Middle esophagus | Anterior chest pain on swallowing |
| 14 | Web formation | Middle esophagus | No |
| 15 | Esophagial ulcerations with perforaton into the anterior mediastinum | N/A | Dysphagia, fever, hypotension |
| 16 | Necrotizing fibrinopurulent ulceration | N/A | N/A |
| 17 | Ulcerative and membranous esophagitis | N/A | Nausea, vomiting and hematemesis |
| 18 | Multiple friable ulcerations | Whole esophagus | Severe odynophagia and dyspahgia |
| 19 | Necrosis | Lower esophagus | Epigastric pain |
| 20 | Necrosis | Middle and lower esophagus | Hematemesis |
UC: ulcerative colitis, N/A: data not available
Table 3.
Clinical Data of UC Patients with Esophageal Ulcer.
| Case (No) | EU biopsy | EU treatment | Outcome of EU | Other complication |
|---|---|---|---|---|
| 1 | Severe inflammatory cell infiltration | PSL | Improvement | No |
| 2 | Infiltration of inflammatory cells in the epithelia and no specific information | PSL | Improvement | Oral ulcer |
| 3 | Superficial inflammation | PSL | Improvement | Maculopapular eruption |
| 4 | Chronically inflamed and edematous, with a dense infltrate of plasma cells, lymphocytes, and histocytes | PSL | Improvement | Buccal ulceration and arthritis |
| 5 | N/A | - | - | No |
| 6 | N/A | - | - | Necrotic ulceration in the inguinal, genital regions and lower extremities |
| 7 | Nonspecific findings other than inflammatorycell infiltration | 5ASA, H2blocker | Improvement | No |
| 8 | Nonspecific findings other than inflammatorycell infiltration | PSL | Improvement | No |
| 9 | Nonspecific findings (Appearance of regenerative epithelium) | PSL | Improvement | Oral ulcer and pancreatitis |
| 10 | Nonspecific findings | PSL, SASP | Improvement | No |
| 11 | Thickening of epithelial stratum spinosum without nuclear inclusion body | PPI | Improvement | No |
| 12 | Nonspecific findings (Appearance of regenerative epithelium) | PPI | Improvement | No |
| 13 | Nonspecific findings other than inflammatorycell infiltration | PSL | Improvement | No |
| 14 | N/A | PSL | N/A | Mouth and pyoderma gangrenosum |
| 15 | N/A | - | - | Oral ulcerations, pustular dermatitis, arthritis |
| 16 | N/A | - | - | N/A |
| 17 | N/A | - | - | Ulcar of his buttock, paronychia of hands |
| 18 | Dense infiltrate of polymorphonuclear cells, a few eosinophils and mononuclear cells | PSL, tetracycline | N/A | Arthritis, episcleritis, oral ulcerations and erythema nodosum |
| 19 | Inflammatory cell and infiltration | PPI | Stricture | No |
| 20 | Not examination | PPI | Stricture | No |
UC: ulcerative colitis, EU: esophageal ulcer, N/A: data not available, PSL: prednisolone, SASP: salazosulfapyridine, 5-ASA: 5-aminosalicylic acid, PPI: proton pump inhibitor
We reviewed these 20 cases and summarized their findings in Table 1 (4-16). The average age of the patients was 28.2 years (range 14-53), and the ratio of men to women was 14:6. The duration of UC was from 0 to 21 years. There were 13 cases of pancolitis, 3 cases of left-side colitis, 1 case of right-side colitis, and 3 cases with unknown details. Seven of the 18 cases had esophageal ulcers at the onset of UC, and 2 cases had ulcers at the time of UC relapse. Two cases were in UC remission, and 7 cases occurred after total colectomy. According to the review results, esophageal ulcer complications were relatively common in the young compared with the elderly. Furthermore, esophageal ulcer was often complicated in patients at the onset of colitis, or at the time of relapse. It has been reported more aggressive UC entities, such as active pancolitis, may be related to the development of gastroduodenitis associated with UC (GDUC) (2). Furthermore, cases of esophageal ulcers after surgery indicate UC may not be resolved in other organs, even after total colectomy (3).
Of the 20 cases, there were 4 cases of multiple esophageal ulcers. There were two cases of entire esophageal ulcer, five of mid-esophageal ulcer, two of lower to middle esophageal ulcer, and five with unknown details. Endoscopic findings of esophageal ulcer complicated with UC were different from GDUC. While GDUC was defined as friable and granular mucosa (2, 3), esophageal ulcer complicated with UC is a punched-out ulcer and mostly occurs in the middle to the lower esophagus.
Regarding the pathology, in all cases described, only non-specific inflammatory cell infiltration was observed, with no UC-specific findings reported. Although the relationship between the esophageal ulcers and UC was not confirmed histologically, no other causes of esophageal ulcers were identified, and treatment for UC was also effective for the esophageal lesions. Regarding treatment, 10 cases were treated with prednisolone, and 2 cases received 5-aminosalicylate. GDUC is treated with medications similar to those used for UC (3, 17) and is more responsive to treatment, showing less frequent relapse than colitis. Our two newly reported cases followed a similar course.
Of the 18 reported cases, 45% had other complications, namely oral lesions in 7 cases, skin lesions in 6 cases, arthritis in 3 cases, and pancreatitis in 1 case. The case reported by Knudsen and Sparberg (6) had a generalized maculopapular eruption as a complication associated with pancolitis-type UC. The patient reported by Rosendorff (7) had buccal ulceration and arthritis. Most cases of UC with esophageal ulcer have had other extracolonic manifestations. Various extracolonic manifestations of UC, such as ocular lesions, skin disease, and peripheral arthritis, have been reported (1); however, their causes are currently unknown.
In conclusion, esophageal ulcer associated with UC is extremely rare. In most cases, it may occur as an extracolonic manifestation. The pathological findings of esophageal lesion are non-specific for UC. Therefore, a comprehensive diagnosis excluding disorders related to infection and medication is required. UC-associated esophageal ulcers are typically associated with the disease onset or relapse of UC. particularly in younger patients, and the treatment response is fortunately considered good. However, the etiology of esophageal ulcer associated with UC remains unknown. Since UC has various pathologies, the accumulation of more cases will be necessary to confirm these findings in the future. The two cases reported in the present study also had atypical aspects and require strict follow-up.
We believe that this case series and literature review will facilitate the accurate and prompt diagnosis of esophageal ulcer associated with UC.
Informed consent was obtained from the patients for the publication of their information and imaging.
The authors state that they have no Conflict of Interest (COI).
Financial Support
This work was supported by Takeda Japan Medical Office Funded Research Grant 2018.
References
- 1. Greenstein AJ, Janowits HD, Sachar DB. The extra-intestinal complications of Crohn's disease and ulcerative colitis: a study of 700 patients. Medicine (Baltimore) 55: 401-412, 1976. [DOI] [PubMed] [Google Scholar]
- 2. Hori K, Ikeuchi H, Nakano H, et al. . Gastroduodenitis associated with ulcerative colitis. J Gastroenterol 43: 193-201, 2008. [DOI] [PubMed] [Google Scholar]
- 3. Hisabe T, Matsui T, Miyaoka M, et al. . Diagnosis and clinical course of ulcerative gastroduodenal lesion associated with ulcerative colitis: possible relationship with pouchitis. Dig Endosc 22: 268-274, 2010. [DOI] [PubMed] [Google Scholar]
- 4. Askawa A, Kojima Y, Fujii E, et al. . Case of ulcerative colitis associated with oesophageal ulcer. J Int Med Res 28: 191-196, 2000. [DOI] [PubMed] [Google Scholar]
- 5. Margoles JS, Wenger J. Stomal ulceration associated with pyoderma gangrenosum and chronic ulcerative colitis. Report of two cases. Gastroenterology 41: 594-598, 1961. [PubMed] [Google Scholar]
- 6. Knudsen KB, Sparberg M. Ulcerative oesophagitis and ulcerative colitis. JAMA 201: 140, 1967. [DOI] [PubMed] [Google Scholar]
- 7. Rosendorff C, Grieve NW. Ulcerative oesophagitis in association with ulcerative colitis. Gut 8: 344-347, 1967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Christopher NL, Watson DW, Farber ER. Relationship of chronic ulcerative oesophagitis to ulcerative colitis. Ann Intern Med 70: 971-976, 1969. [DOI] [PubMed] [Google Scholar]
- 9. Haward MZ, Gilbert R, Simmy B. Apthous ulcers of the esophagus in a patient with ulcerative colitis. Gastrointest Endosc 30: 298-299, 1984. [DOI] [PubMed] [Google Scholar]
- 10. Konishi H, Mitsuhashi Y, Fujino N, et al. . A case of right-sided ulcerative colitis associated with unusual esophageal ulcer. Chiba Medical Association Magazine 50: 143-144, 1998. (in Japanese). [Google Scholar]
- 11. Ikeda Y, Yonezawa K, Suzuki K, et al. . A case of ulcerative colitis associated with a hemorrhagic esophageal ulcer. J Kushiro City Gen Hosp 12: 129-133, 2000. (in Japanese). [Google Scholar]
- 12. Higashi Y, Nakamura T, Sunayama K, et al. . A case of ulcerative colitis combined with esophageal ulcer. Nihon Rinsho Geka Gakkai Zasshi (J Japan Surg Assoc) 65: 143-146, 2004. (in Japanese, Abstract in English). [Google Scholar]
- 13. Sato N, Kurakata H, Hirano N, et al. . A case of ulcerative colitis combined with esophageal ulcer. Progress of Digestive Endoscopy 65: 90-91, 2004. (in Japanese). [Google Scholar]
- 14. Ose T, Ishihara S, Oshima N, et al. . A case of ulcerative colitis complicated with giant esophageal ulcer. Clinics in Gastroenterology 11: 93-96, 2005. [Google Scholar]
- 15. Izawa N, Sugaya T, Kanamori A, et al. . A case of ulcerative colitis with esophageal ulcer. Progress of Digestive Endoscopy 87: 94-95, 2015. (in Japanese, Abstract in English). [Google Scholar]
- 16. Kuroki H, Sugita A, Koganei K, et al. . Two cases of esophageal ulcer after surgical treatment for ulcerative colitis. Clin J Gastroenterol. Forthcoming. [DOI] [PubMed] [Google Scholar]
- 17. Chiba M, Ono I, Wakamatsu H, Wada I, Suzuki K. Diffuse gastroduodenitis associated with ulcerative colitis: treatment by infliximab. Dig Endosc 25: 622-625, 2013. [DOI] [PubMed] [Google Scholar]