Abstract
Can social contextual factors explain international differences in the spread of COVID-19? It is widely assumed that social cohesion, public confidence in government sources of health information and general concern for the welfare of others support health advisories during a pandemic and save lives. We tested this assumption through a time-series analysis of cross-national differences in COVID-19 mortality during an early phase of the pandemic. Country data on income inequality and four dimensions of social capital (trust, group affiliations, civic responsibility and confidence in public institutions) were linked to data on COVID-19 deaths in 84 countries. Associations with deaths were examined using Poisson regression with population-averaged estimators. During a 30-day period after recording their tenth death, mortality was positively related to income inequality, trust and group affiliations and negatively related to social capital from civic engagement and confidence in state institutions. These associations held in bivariate and mutually controlled regression models with controls for population size, age and wealth. The results indicate that societies that are more economically unequal and lack capacity in some dimensions of social capital experienced more COVID-19 deaths. Social trust and belonging to groups were associated with more deaths, possibly due to behavioural contagion and incongruence with physical distancing policy. Some countries require a more robust public health response to contain the spread and impact of COVID-19 due to economic and social divisions within them.
Keywords: COVID-19, Social capital, Income inequality, Pandemic
Highlights
-
•
Income inequality was associated with 30-day mortality rates in 84 countries.
-
•
Some dimensions of social capital are associated with fewer COVID-19 deaths.
-
•
Social trust is associated with more deaths, possibly due to behavioural contagion.
1. Introduction
As the novel coronavirus disease 2019 (COVID-19) pandemic continues to spread globally, efforts to contain the virus and avoid a scenario where critically ill patients overwhelm healthcare systems have become a public health priority. Despite these efforts, more than 800 000 lives have been lost to the virus at the time of writing (World Health Organization, 2020). Country differences have emerged in rates of new cases and deaths despite having a similar policy response that involves, among other things, physical distancing. Some of this variation may relate to social contextual factors that influence compliance with health advisories (e.g., physical distancing, washing hands frequently, wearing a facemask) and tolerance of prolonged disruptions to travel, work and social and cultural activities (Gilles et al., 2011; van der Weerd et al., 2011) in addition to underlying social inequities in vulnerability and health care access (Takian et al., 2020). We investigated why some countries have experienced lower COVID-19 mortality than others by examining income inequality and social bonds and linkages that facilitate collective action.
Income inequality defines social stratifications in health and mortality (Bor, Cohen and Galea, 2015; Pickett and Wilkinson, 2015). Its negative consequences for population health are well documented and have been attributed to biased public policies that benefit the rich, such as low taxes and low public spending and psychosocial pathways of class anxiety and distrust (Bor et al., 2017; de Mello and Tiongson, 2006). Relative income differences within societies also shape social patterns in infectious disease. Socioeconomic disparities in H1N1 mortality were attributed to differential exposure to the virus, differential susceptibility to disease and differential access to health care once disease has developed (Rutter et al., 2012). New research (e.g., Ahmed et al., 2020; Takian et al., 2020) has observed a similar pattern in COVID-19, with more transmission and worse health outcomes in poorer populations due to overcrowded housing and work conditions. Some research in the US recently found moderate correlations between state-level income inequality and COVID-19 cases and deaths (Mollalo et al., 2020; Oronce et al., 2020) and other communicable disease (e.g., sexually transmitted disease, tuberculosis; Holtgrave and Crosby, 2003, 2004), however cross-national evidence of a contextual association with COVID-19 is scarce.
We also turned to the literature on social capital and health to make sense of emerging international differences in COVID-19 mortality. Social capital is a broad theoretical construct that describes shared social resources that stem from being a part of “institutionalised relationships of mutual acquaintance and recognition” (Bourdieu and Wacquant, 1992, p. 119). Its definitions and conceptual frameworks describe some combination of distinct yet related contextual factors including trust, social networks and norms of reciprocity (e.g., Besser, 2009; Putnam, 2000). These core dimensions run along strong, close-knit social ties such as those between family members and close friends as well as along weak social ties between members of different groups (Poortinga, 2012). They also support other social resources that include, among other things, group affiliations, public confidence in state authority and governance and collective action in response to common threats (Koh and Cadigan, 2018; Poortinga, 2012). To our knowledge, however, the benefits of social capital for surviving a pandemic have yet to be examined.
Our supposition that social capital may play a role in COVID-19 deaths stems, in part, from our observation that during the 2003 SARS crisis in Hong Kong, public anxiety about the virus was associated with lack of confidence in government and health institutions (Cheung and Tse, 2008). Likewise, during the H1N1 pandemic, studies from different countries found that protective behaviours and intentions to vaccinate related to confidence in health authorities (Chuang et al., 2015; Freimuth et al., 2014; Gilles et al., 2011; van der Weerd et al., 2011). The notion that public distrust of health authorities could affect the course of COVID-19 resonates strongly with governments, but this is just one outcome of social capital. The benefits, if any, of living in more affiliated, trusting or community-engaged societies are unclear.
We contend that two issues have complicated efforts to apply the aforementioned knowledge to understand country-level differences in COVID-19 deaths. First, individual attitudes and health behaviours do not necessarily correspond to similar links at a societal level. Income inequality and social capital are ecologic constructs that have not been closely examined in the context of a global pandemic. Second, not all dimensions of social capital are necessarily protective. Some research into the “dark side” of social capital found that strong ingroup bonds correlate with poor mental health and risky behaviours (e.g., depression, alcohol misuse, all-cause mortality; Villalonga-Olives and Kawachi, 2017) and rejection of outgroup social norms (Zmerli, 2010). Still, given that most studies show positive links to health, we tested the idea that dimensions of social capital may support engagement in health protective measures and therefore expected to find less COVID-19 mortality in countries that experienced lower income inequality and greater social capital.
2. Methods
2.1. Data sources
Our hypotheses and methods were preregistered with AsPredicted, 2020. We used time-series analysis on countries that had documented 10 or more COVID-19 deaths as of September 3, 2020, and previously participated in the World Values Survey (WVS; Inglehart et al., 2014). The WVS provided the data to assess social capital. Specifically, we used the most recent WVS data available on social capital: cycle 7 (2017–2020) for 44 countries, cycle 6 (2010–2014) for 27 countries and cycle 5 (2005–2009) for the remaining 7 countries. The WVS follows an international protocol and recruits stratified samples of at least 1000 adults per country.
Data on income inequality were provided by the Standardized World Income Inequality Database (SWIID; Solt, 2020). The European Centre for Disease Prevention and Control (ECDC) provided international data on COVID-19 deaths (ECDC, 2020). The ECDC relies on national sources for this information and continually updates its tracking data for surveillance and research purposes. We did not use data on confirmed cases due to their sensitivity to testing for which limited information had been gathered.
For the control variables, we used World Bank Databank data on country wealth (gross national income per person expressed in constant 2017 international dollars and converted by purchasing power parity rates; World Bank, 2020a) and percentage of the country population over the age of 65 (World Bank, 2020b). The United Nations Population Division (2020) supplied data on country populations in 2019.
2.2. Measures
The SWIID contains harmonised estimates of post-taxation, post-transfer income inequality (Gini index) in 2018 based on data from United Nations University's World Income Inequality Database and Luxembourg Income Study (Solt, 2020). The Gini index has a theoretical range of 0 (perfect equality with everyone having equal income) to 1 (perfect inequality with one person having all the income).
We measured four dimensions and outcomes of social capital using a previously developed 17-item scale (supplementary Table S1; Elgar et al., 2011). The WVS Social Capital Scale has four factor-analytically derived indices that measured trust (6 items), group affiliations (4 items), civic engagement (4 items) and confidence in state institutions (3 items). Although the scale excludes some aspects of social capital (e.g., norms of reciprocity) because these topics were not covered in the WVS, we chose this scale because it has been argued to be one of the best measures of social capital in terms of its content and construct validity in diverse cultural contexts (see Agampodi et al., 2015). Nonetheless, we conducted both exploratory and confirmatory factor analyses on the data obtained from Cycles 5 to 7 of the WVS. These analyses replicated the factor structure identified by Elgar and colleagues (2011; see supplementary Table S2).
2.3. Analysis
Country scores on each of the four social capital indices were calculated by summing the survey responses and then fitting the data to weighted regressions of each total. These models included fixed effects of gender (male or female), age (years), household income (country-specific decile group) and country (dummy coded). Predicted total scores for each country were then scaled to a range of 0–1 to facilitate comparisons of their associations with mortality. These country-level data were then linked to 30-day panels of COVID-19 deaths, spanning the period January 22 to September 3, 2020 and containing 2490 country/day observations (average 29.6 per country). We then merged data on income inequality, country wealth, population, percentage of the population over the age of 65 and a dummy variable to control unmeasured differences between WVS cycles.
Associations with deaths over time were tested using Poisson regression (xtpoisson in Stata 16.1 [StataCorp LLC, College Station, TX]) with population-averaged estimators. This approach was chosen due to time-invariant predictors and strong likelihood of autocorrelated residuals over time (Hubbard et al., 2010). The exposure variable was specified as time (in days) that elapsed since 10 deaths were recorded. Associations were reported as incidence rate ratios (IRR; Beck and Katz, 1995). At a reviewer's request, we deviated from our registered hypothesis by adding population age as a control variable, which was tested separately. For descriptive purposes we reported countries’ doubling time in days (T d) as function of daily growth rates (G) in deaths, T d =log(2)/log(1 + G). Replication data and syntax were made publicly available via the Open Science Framework (Stefaniak et al., 2020). Original microdata from the WVS can be downloaded from http://www.worldvaluessurvey.org.
3. Results
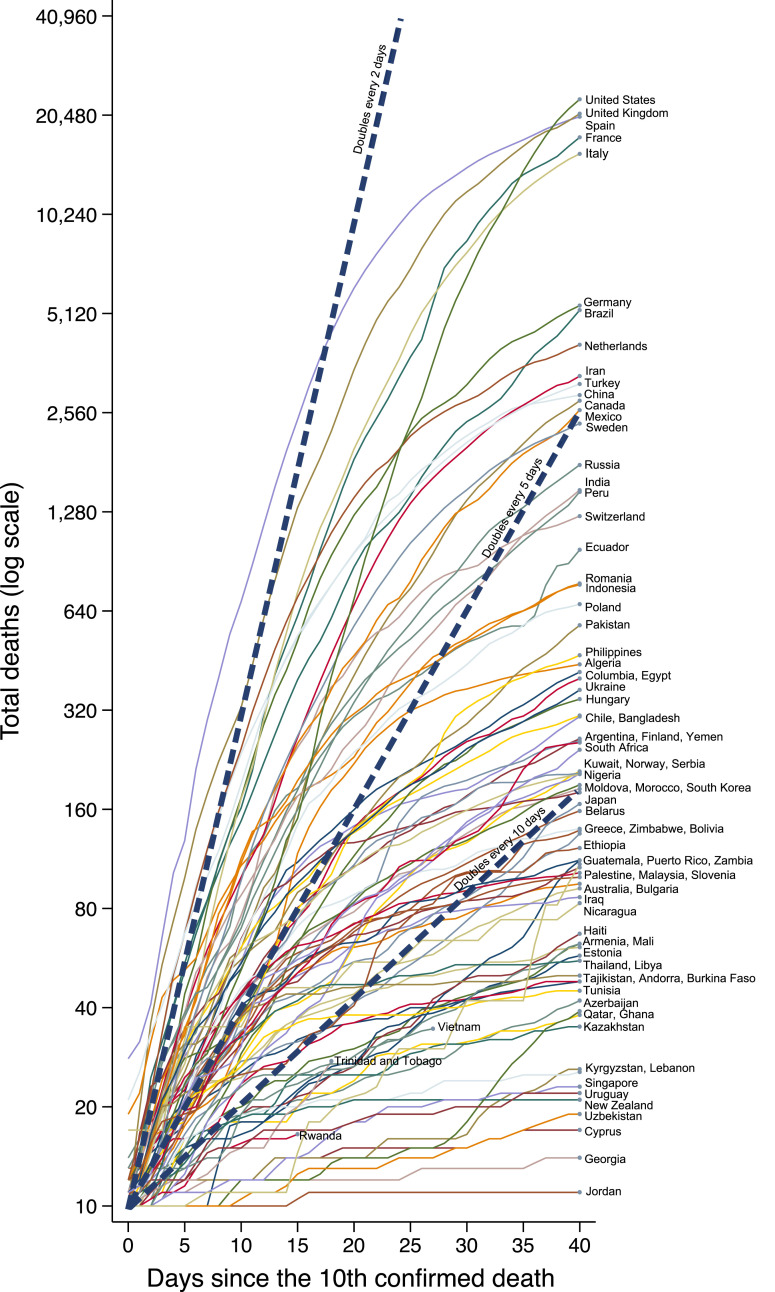
Doubling times in deaths ranged from 2.99 days in Nicaragua to 23.33 days in Morocco (mean = 10.73, SD = 4.34). Fig. 1 shows cumulative mortality in the 84 countries that met the inclusion criteria for the study. Income inequality (Gini index) ranged from 0.23 (Belarus) to 0.60 (South Africa; mean = 0.37, SD = 0.07). Supplementary Table S3 shows doubling time, deaths, income inequality and social capital scores by country. Country rankings in social capital are shown in supplementary Figure S1. As shown in Table 1 , income inequality was correlated with three dimensions of social capital: social trust (r = −0.38, p < 0.01), group affiliations (r = 0.38, p < 0.01), and civic engagement (r = −0.33, p < 0.05). Correlations between social capital dimensions and doubling times were mostly modest or non-significant.
Fig. 1.
Cumulative COVID-19 deaths in 84 countries during a 40-day period after recording 10 deaths (as of September 3, 2020).
Table 1.
Descriptive statistics on key variables and intercorrelations in 84 countries involved in the World Values Survey during a 30-day period after recording the tenth COVID-19 death (as of September 3, 2020).
| Variable | Mean (SD) | Range | Correlations |
|||||
|---|---|---|---|---|---|---|---|---|
| 1. | 2. | 3. | 4. | 5. | 6. | |||
| 1. Income inequality | 0.37 (0.07) | 0.23, 0.60 | – | |||||
| 2. Social trust | 0.38 (0.22) | 0.00, 1.00 | −0.38** | – | ||||
| 3. Group affiliations | 0.39 (0.28) | 0.00, 1.00 | 0.38** | 0.20 | – | |||
| 4. Civic engagement | 0.74 (0.19) | 0.00, 1.00 | −0.33** | 0.20 | −0.09 | – | ||
| 5. Confidence in state institutions | 0.45 (0.21) | 0.00, 1.00 | −0.18 | 0.25* | 0.01 | 0.21 | – | |
| 6. Doubling time in deaths | 10.72 (4.34) | 2.99, 23.33 | −0.01 | −0.23* | −0.16 | −0.01 | −0.03 | – |
*p < 0.05. **p < 0.01. SD = standard deviation.
Using bivariate regressions (Table 2 , Model 1), we found that COVID-19 death rates were positively related to population size, country wealth and percentage of the population age 65+. These unadjusted regressions also showed positive associations with income inequality and all four dimensions social capital. Because each social capital index was scaled to have a 1-point range, IRRs should be interpreted as ratios in deaths at the maximum observed level of social capital to deaths at the lowest. It should also be noted that a 1-point difference in the Gini index of income inequality spans its theoretical range (0–1), not the observed range (0.23–0.60).
Table 2.
Poisson regression of mortality rates in 84 countries involved in the World Values Survey during a 30-day period after recording the tenth COVID-19 death (as of September 3, 2020).
| Bivariate associations (Model 1) |
Mutually adjusted (Model 2) |
Mutually adjusted (Model 3) |
||||
|---|---|---|---|---|---|---|
| IRR (SE) | 95% CI | IRR (SE) | 95% CI | IRR (SE) | 95% CI | |
| Population (millions) | 4.01 (0.04) | 3.94, 4.08 | 12.29 (0.18) | 11.95, 12.64 | 16.20 (0.25) | 15.72, 16.70 |
| Country wealth | 1.03 (0.00) | 1.03, 1.03 | 1.05 (0.00) | 1.05, 1.05 | 1.04 (0.00) | 1.04, 1.04 |
| Income inequality | 5.97 (0.08) | 5.68, 5.90 | 1.65 (0.08) | 1.50, 1.81 | 1.67 (0.07) | (1.53, 1.82) |
| Social capital | ||||||
| Social trust | 7.92 (0.05) | 7.83, 8.01 | 3.38 (0.08) | 3.22, 3.54 | 1.73 (0.04) | 1.65, 1.81 |
| Group affiliations | 3.90 (0.03) | 3.85, 3.95 | 0.56 (0.01) | 0.54, 0.58 | 1.09 (0.02) | 1.05, 1.14 |
| Civic engagement | 2.84 (0.01) | 2.82, 2.87 | 4.91 (0.11) | 4.70, 5.13 | 0.73 (0.02) | 0.69, 0.78 |
| Confidence in state institutions | 3.49 (0.02) | 3.44, 3.53 | 0.01 (0.00) | 0.00, 0.01 | 0.01 (0.00) | 0.01, 0.01 |
| WVS cycle (ref. 5) | ||||||
| Cycle 6 | 1.82 (0.01) | 1.80, 1.85 | 0.41 (0.00) | 0.40, 0.42 | 0.53 (0.01) | 0.52, 0.54 |
| Cycle 7 | 1.32 (0.01) | 1.31, 1.34 | 0.45 (0.01) | 0.43, 0.46 | 0.46 (0.01) | 0.45, 0.47 |
| Population over 65 years (%) |
1.08 (0.00) |
1.07, 1.08 |
1.09 (0.00) |
1.09, 1.09 |
||
| Goodness-of-fit: | (Empty model) | (Model 2) | (Model 3) | |||
| Deviance | 273 419.47 | 161 804.54 | 154 027.04 | |||
| Dispersion | 109.807 | 64.98 | 61.85 | |||
| Pearson χ2 | 703 286.66 | 294 888.22 | 304 138.67 | |||
| Dispersion Pearson χ2 | 282.444 | 118.43 | 122.14 | |||
| Wald χ2 | -- | 249 658.63 | 258 961.92 | |||
Note: IRR = Incidence rate ratio. CI = confidence interval. WVS = World Values Survey. Sample includes 2490 daily observations (average: 29.6 days per country). Country wealth (gross national income per capita) is measured constant 2017 international dollars (thousands). Lower deviance and dispersion indicate better model fit.
With mutual controls applied (Model 2), the positive association between income inequality and deaths remained significant (IRR = 1.65, 95% CI = 1.50 to 1.81) as did the positive associations with trust (IRR = 3.38, 95% CI = 3.22 to 3.54) and civic engagement (IRR = 4.91, 95% CI = 4.70 to 5.13). However, two social capital dimensions now showed negative associations with deaths—group affiliations (IRR = 0.56, 95% CI = 0.54 to 0.58) and confidence in state institutions (IRR = 0.01, 95% CI = 0.00 to 0.01). With an additional control for population age (Model 3), group affiliations became positively associated with deaths and civic engagement became negatively associated. The fully adjusted model (Model 3) had better overall fit to the data and showed that 30-day mortality positively related to income inequality (IRR = 1.73, 95% CI = 1.65 to 1.81). In terms, of social capital, deaths were negatively related to civic engagement (IRR = 0.73, 95% CI = 0.69 to 0.78), and confidence in state institutions (IRR = 0.01, 95% CI = 0.01 to 0.01), but positively related to group affiliations (IRR = 0.73, 95% CI = 0.69 to 0.78) and social trust (IRR = 1.73, 95% CI = 1.65 to 1.81). The association with income inequality corresponds to a 25% increase in mortality between the least and most unequal countries in our sample.
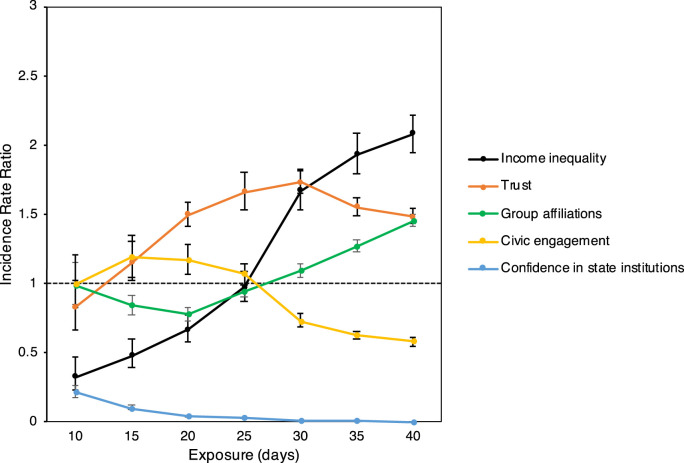
We further investigated whether the observed effects were sensitive to exposure time. Using the fully adjusted model (Table 2, Model 3) and by varying the exposure variable from 10 to 40 days, we found that income inequality, trust and group affiliations were consistently related to more deaths after 25 days of exposure (IRRs > 1) and the other social capital dimensions related to fewer deaths (IRRs < 1; Fig. 2 ).
Fig. 2.
Marginal effects of exposure (days since countries reported their 10th COVID-19 death) on associations of mortality with income inequality and four dimensions of social capital in 84 countries involved in the World Values Survey. Incident rate ratios (IRR) below 1 represent negative associations; above 1 represent positive associations. Error bars represent 95% confidence intervals.
4. Discussion
Identifying social contextual factors that align with the health impacts of the COVID-19 pandemic supports public health policy and confounds a common intuition about the protective role of social trust. Our analyses revealed that country-level wealth and income inequality were positively and consistently related to mortality after other social factors were controlled. Two dimensions of social capital related to less mortality, ceteris paribus: civic engagement and confidence in state institutions. Two other dimensions of social capital, social trust and group affiliations, related to more deaths during the early phase of the pandemic. Below we discuss three key findings of the study.
To our knowledge, this is the first study to show that cross-national differences in COVID-19 mortality relate to income inequality. This finding aligns with studies that found associations between inequality and various measures of population health (Pickett and Wilkinson, 2015; Ram, 2006) and recent evidence from the United States (Mollalo et al., 2020; Oronce et al., 2020). The association held up to multiple controls, including country wealth and social capital, and therefore is not well explained by differences in trust, as suggested elsewhere (Pickett and Wilkinson, 2015). Rather, relative income differences within societies are likely to be a proxy of health inequities between socioeconomic groups that, in the context of a pandemic, are compounded by structural inequalities in work and living conditions. In many countries, regardless of their wealth, lower wage earners are over-represented among the “essential workers” in retail, public transit and health care settings whom cannot easily practice physical distancing (Dorn et al., 2020). More pre-existing health conditions, greater exposure to the virus, and poorer access to health services among the poor explain why more economically unequal countries (not necessarily the poorest) experienced significantly more COVID-19 deaths during the Spring of 2020 (Rutter et al., 2012; Takin et al., 2020). The positive association with country wealth supports the conclusion that countries’ efforts to limit mortality early in the pandemic were challenged by relative income poverty, not absolute poverty. A caveat here is that wealthier countries may also have more accurate data or shorter lags in supplying death counts to health officials.
Second, COVID-19 mortality was also associated with a lack of confidence in state institutions. This result is consistent with social research during the SARS and H1N1 pandemics (Cheung and Tse, 2008; Chuang et al., 2015; Freimuth et al., 2014) and can be interpreted through theories of social capital that differentiate social relationships that run horizontally within or between groups (bonding and bridging) and linking social capital that lies in the confidence and trust running vertically between citizens and governing institutions (e.g., Putnam, 2000; Szreter and Woolcock, 2004). A lack of linking social capital is reflected in low voting participation, distrust in government and government's distrust in health experts (Ehsan et al., 2019; Poortinga, 2012). It is unclear which specific pathways underlie the observed link to COVID-19 mortality and further investigation is warranted given the importance of public confidence in state institutions to physical distancing policy.
Social capital derived from civic engagement also related to less mortality, which is consistent with evidence about its positive links to health (Elgar et al., 2011; Poortinga, 2012). Being actively engaged in the community is particularly beneficial when communities face a common threat or are asked to compromise some personal freedom for the common good (e.g., wearing a mask in public). Governments and other organisations can capitalise on this engagement during a pandemic by supporting safe ways for people to socialise and remain involved in their communities and cultural activities.
Third, an unexpected finding was the positive associations between mortality and two other sources of social capital, group affiliations and trust. We expected to find negative associations here given prior evidence of their positive links to health (e.g., Ehsan et al., 2019). Identifying with positively valued groups provides a sense of meaning and purpose, satisfies a need to belong, strengthens self-esteem and self-efficacy, and supports health and well-being (Vignoles et al., 2005). We attribute this finding to how ingroup bonds reinforce risky health behaviours through the phenomenon of behavioural contagion (see review by Villalonga-Olives and Kawachi, 2017). High trusting and affiliated societies may be more susceptible to misinformation about the severity of COVID-19, bogus treatments, or dismissive attitudes towards physical distancing (Zmerli, 2010). Trust interferes with efforts to contain transmission through physical distancing. Dezecache et al. (2020), Drury (2018), and others have argued that social affiliation and contact are natural responses to threat and these inclinations were adaptive in our evolutionary past. Taylor's (2012) “tend and befriend” psychological theory of stress describes the innate human desire to affiliate when threatened. We “tend to offspring to ensure their survival and affiliate with others for protection and comfort” (Taylor, 2012, p. 32). Despite their evolutionary significance, these social cravings pose a barrier to public safety in the context of COVID-19. The lesson here is that social capital, in all its forms, is generally agnostic about whether it has positive or negative influences on health. Its various dimensions and outcomes are neither fungible nor consistently beneficial to good health.
The strengths of the study include a large and diverse sample in which surveys of social capital were carried out prior to the pandemic. The sample represented 86% of the global population. Furthermore, social capital was measured using a multidimensional scale that was fielded using a standardised survey protocol. There are also limitations that should be noted. We investigated the initial phase of the pandemic by excluding countries that met the inclusion criteria after the time of writing. Some of the data on social capital were from an older cycle of the WVS (2005–09). Also, data on social capital were aggregated with adjustments for some compositional differences in the WVS samples, but we caution against an ‘atomistic fallacy’ that ecologic differences between societies correspond to similar differences between individuals.
5. Conclusions
The social determinants of health shape collective responses to dynamically evolving threats such as the current COVID-19 pandemic. Civic engagement, confidence in institutional authorities and low income inequality may facilitate public health advice and, in turn, save lives. Our results also foreshadow obstacles some countries may face to convince citizens to get vaccinated once a vaccine is developed, and prioritising vaccine development over containment. Specifically, vaccination rates may differ between countries as a function of income inequality and social capital.
In summary, our analysis found that COVID-19 mortality relates to income inequality and specific dimensions of social capital after other cross-national differences in wealth, population size, and population age were controlled. Further research is urgently needed on the material and psychosocial pathways that underlie these associations, such as the generosity of public expenditures and policies that mitigate the impacts of COVID-19, public access to testing and health care, and inequality in pre-existing health conditions between the rich and poor. From this preliminary analysis early in the pandemic, we conclude between-country differences in mortality track with economic and social divisions within them.
Credit author statement
Frank J. Elgar: Conceptualisation, Methodology, Formal analysis, Investigation, Data curation, Writing - original draft, Writing - review & editing, Project administration. Anna Stefaniak: Methodology, Validation, Writing - original draft, Writing - review & editing, Resources. Michael J. A. Wohl: Conceptualisation, Methodology, Investigation, Writing - original draft, Writing - review & editing, Project administration.
Acknowledgments
The authors acknowledge funding support from the Canada Research Chairs awarded to the first author.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.socscimed.2020.113365.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Agampodi T.C., Agampodi S.B., Glozier N., Siribaddana S. Measurement of social capital in relation to health in low and middle income countries (LMIC): a systematic review. Soc. Sci. Med. 2015;128:95–104. doi: 10.1016/j.socscimed.2015.01.005. [DOI] [PubMed] [Google Scholar]
- Ahmed F., Ahmed N., Pissarides C., Stiglitz J. Why inequality could spread COVID-19. Lancet Public Health. 2020;5 doi: 10.1016/S2468-2667(20)30085-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- AsPredicted . AsPredicted; 2020. Social capital, income inequality and COVID-19 mortality, Protocol #38817.https://aspredicted.org/bm3yk.pdf [Google Scholar]
- Beck N., Katz J.N. What to do (and not to do) with time-series cross-section data. Am. Polit. Sci. Rev. 1995;89:634–647. doi: 10.2307/2082979. [DOI] [Google Scholar]
- Besser T.L. Changes in small town social capital and civic engagement. J. Rural Stud. 2009;25:185–193. doi: 10.1016/j.jrurstud.2008.10.005. [DOI] [Google Scholar]
- Bor J., Cohen G.H., Galea S. Population health in an era of rising income inequality: USA, 1980-2015. Lancet. 2017;389:1475–1490. doi: 10.1016/S0140-6736(17)30571-8. [DOI] [PubMed] [Google Scholar]
- Bourdieu P., Wacquant L.P.D. University of Chicago Press; Chicago: 1992. An Invitation to Reflexive Sociology. [Google Scholar]
- Cheung C.K., Tse J.W. Institutional trust as a determinant of anxiety during the SARS crisis in Hong Kong. Soc. Work. Publ. Health. 2008;23:41–54. doi: 10.1080/19371910802053224. [DOI] [PubMed] [Google Scholar]
- Chuang Y.C., Huang Y.L., Tseng K.C., Yen C.H., Yang L.H. Social capital and health-protective behavior intentions in an influenza pandemic. PloS One. 2015;10 doi: 10.1371/journal.pone.0122970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Mello L., Tiongson E.R. Income inequality and redistributive government spending. Publ. Finance Rev. 2006;34:282–305. doi: 10.1177/1091142105284894. [DOI] [Google Scholar]
- Dezecache G., Frith C.D., Deroy O. Pandemics and the great evolutionary mismatch. Curr. Biol. 2020;30:R417–R419. doi: 10.1016/j.cub.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dorn A.V., Cooney R.E., Sabin M.L. COVID-19 exacerbating inequalities in the US. Lancet. 2020;395:1243–1244. doi: 10.1016/S0140-6736(20)30893-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drury J. The role of social identity processes in mass emergency behaviour: an integrative review. Eur. Rev. Soc. Psychol. 2018;29:38–81. doi: 10.1080/10463283.2018.1471948. [DOI] [Google Scholar]
- Ehsan A., Klaas H.S., Bastianen A., Spini D. Social capital and health: a systematic review of systematic reviews. SSM Popul Health. 2019;8:100425. doi: 10.1016/j.ssmph.2019.100425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elgar F.J., Davis C.G., Wohl M.J., Trites S.J., Zelenski J.M., Martin M.S. Social capital, health and life satisfaction in 50 countries. Health Place. 2011;17:1044–1053. doi: 10.1016/j.healthplace.2011.06.010. [DOI] [PubMed] [Google Scholar]
- European Centres for Disease Prevention and Control Download today's data on the geographic distribution of COVID-19 cases worldwide. 2020. https://www.ecdc.europa.eu/en/publications-data/download-todays-data-geographic-distribution-covid-19-cases-worldwide Accessed.
- Freimuth V.S., Musa D., Hilyard K., Quinn S.C., Kim K. Trust during the early stages of the 2009 H1N1 pandemic. J. Health Commun. 2014;19:321–339. doi: 10.1080/10810730.2013.811323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilles I., Bangerter A., Clémence A., Green E.G.T., Krings F., Staerklé C., Wagner-Egger P. Trust in medical organizations predicts pandemic (H1N1) 2009 vaccination behavior and perceived efficacy of protection measures in the Swiss public. Eur. J. Epidemiol. 2011;26:203–210. doi: 10.1007/s10654-011-9577-2. [DOI] [PubMed] [Google Scholar]
- Holtgrave D.R., Crosby R.A. Social capital, poverty, and income inequality as predictors of gonorrhoea, syphilis, chlamydia and AIDS case rates in the United States. Sex. Transm. Infect. 2003;79:62–64. doi: 10.1136/sti.79.1.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holtgrave D.R., Crosby R.A. Social determinants of tuberculosis case rates in the United States. Am. J. Prev. Med. 2004;26:159–162. doi: 10.1016/j.amepre.2003.10.014. [DOI] [PubMed] [Google Scholar]
- Hubbard A.E., Ahern J., Fleischer N.L., Van der Laan M., Lippman S.A., Jewell N., Bruckner T., Satariano W.A. To GEE or not to GEE: comparing population average and mixed models for estimating the associations between neighborhood risk factors and health. Epidemiology. 2010;21:467–474. doi: 10.1097/EDE.0b013e3181caeb90. [DOI] [PubMed] [Google Scholar]
- Inglehart R.C., Haerpfer A., Moreno C. JD Systems Institute; 2014. World Values Survey: Round Six - Country-Pooled Datafile 2010-2014.http://www.worldvaluessurvey.org/WVSDocumentationWV6.jsp Accessed. [Google Scholar]
- Koh H.K., Cadigan R.O. Disaster preparedness and social capital. In: Kawachi I., Subramanian S., Kim D., editors. Social Capital and Health. Springer; New York: 2018. [Google Scholar]
- Mollalo A., Vahedi B., Rivera K.M. GIS-based spatial modeling of COVID-19 incidence rate in the continental United States. Sci. Total Environ. 2020;728:138884. doi: 10.1016/j.scitotenv.2020.138884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oronce C.I.A., Scannell C.A., Kawachi I., Tsugawa Y. Association between state-level income inequality and COVID-19 cases and mortality in the USA. J. Gen. Intern. Med. 2020;35:2791–2793. doi: 10.1007/s11606-020-05971-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickett K.E., Wilkinson R.G. Income inequality and health: a causal review. Soc. Sci. Med. 2015;128:316–326. doi: 10.1016/j.socscimed.2014.12.031. [DOI] [PubMed] [Google Scholar]
- Poortinga W. Community resilience and health: the role of bonding, bridging, and linking aspects of social capital. Health Place. 2012;18:286–295. doi: 10.1016/j.healthplace.2011.09.017. [DOI] [PubMed] [Google Scholar]
- Putnam R.D. Simon and Schuster; New York: 2000. Bowling Alone: the Collapse and Revival of American Community. [Google Scholar]
- Ram R. Further examination of the cross-country association between income inequality and population health. Soc. Sci. Med. 2006;62:779–791. doi: 10.1016/j.socscimed.2005.06.034. [DOI] [PubMed] [Google Scholar]
- Rutter P.D., Mytton O.T., Mak M., Donaldson L.J. Socio-economic disparities in mortality due to pandemic influenza in England. Int. J. Publ. Health. 2012;57:745–750. doi: 10.1007/s00038-012-0337-1. [DOI] [PubMed] [Google Scholar]
- Solt F. Measuring income inequality across countries and over time: the standardized World income inequality Database. Soc. Sci. Q. 2020;101:1183–1199. doi: 10.1111/ssqu.12795. [DOI] [Google Scholar]
- Stefaniak A., Wohl M.J.A., Elgar F.J. Income inequality, social capital and COVID-19 mortality: replication materials. Open Science Framework. 2020 http://osf.io/8kwn3 Accessed. [Google Scholar]
- Szreter S., Woolcock M. Health by association? Social capital, social theory, and the political economy of public health. Int. J. Epidemiol. 2004;33:650–667. doi: 10.1093/ije/dyh013. [DOI] [PubMed] [Google Scholar]
- Takian A., Kiani M.M., Khanjankhani K. COVID-19 and the need to prioritize health equity and social determinants of health. Int. J. Publ. Health. 2020 doi: 10.1007/s00038-020-01398-z. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S.E. Tend and befriend theory. In: Van Lange P.A.M., Kruglanski A.W., Higgins E.T., editors. Handbook of Theories of Social Psychology. Sage; Thousand Oaks, CA, USA: 2012. pp. 32–49. [DOI] [Google Scholar]
- United Nations Population Division . United Nations Population Division; 2020. World Population Prospects 2019.https://population.un.org/wpp/ Accessed. [Google Scholar]
- van der Weerd W., Timmermans D.R., Beaujean D.J., Oudhoff J., van Steenbergen J.E. Monitoring the level of government trust, risk perception and intention of the general public to adopt protective measures during the influenza A (H1N1) pandemic in The Netherlands. BMC Publ. Health. 2011;11:575. doi: 10.1186/1471-2458-11-575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vignoles V.L., Regalia C., Manzi C., Golledge J., Scabini E. Beyond self-esteem: influence of multiple motives on identity construction. J. Pers. Soc. Psychol. 2005;90:308–333. doi: 10.1037/0022-3514.90.2.308. 2006. [DOI] [PubMed] [Google Scholar]
- Villalonga-Olives E., Kawachi I. The dark side of social capital: a systematic review of the negative health effects of social capital. Soc. Sci. Med. 2017;194:105–127. doi: 10.1016/j.socscimed.2017.10.020. [DOI] [PubMed] [Google Scholar]
- World Bank . World Bank; 2020. GNI Per Capita, Atlas Method (Current US$)http://data.worldbank.org/indicator/NY.GNP.PCAP.PP.KD Accessed. [Google Scholar]
- World Bank . World Bank; 2020. Population Ages 65 and above (% of Total Population)https://data.worldbank.org/indicator/sp.pop.65up.to.zs Accessed. [Google Scholar]
- World Health Organization . World Health Organization; 2020. Coronavirus Disease 2019 (COVID-19) Weekly Epidemiological Update.https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200831-weekly-epi-update-3.pdf?sfvrsn=d7032a2a_4 Accessed. [Google Scholar]
- Zmerli S. Social capital and norms of citizenship: an ambiguous relationship? Am. Behav. Sci. 2010;53:657–676. doi: 10.1177/0002764209350829. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.