Abstract
Amyloid Protein Precursor gene duplication is a rare cause of early-onset Alzheimer's disease that can be associated with Cerebral Amyloid Angiopathy. This condition predisposes cerebrovascular events, specifically, intracerebral hemorrhagic stroke. This report describes a case of first-time intracerebral hemorrhage in a patient with APP gene duplication during SARS-CoV-2 infection, a typically pro-thrombotic and pro-inflammatory condition, as a possible trigger for this condition.
Keywords: COVID-19, Stroke, Early-onset Alzheimer's disease
Abbreviations: APP, Amyloid Protein Precursor; MRI, Magnetic Resonance Imaging; CT, computed tomography; NR, normal range; Aβ, Amyloid-β; CAA, Cerebral Amyloid Angiopathy.
Highlights
-
•
Stroke could be triggered by COVID-19 infection in high-risk patients.
-
•
Altered level of consciousness could be the first manifestation of COVID-19.
-
•
CT thorax scan must be considered during neuroimaging studies in stroke patients.
1. Case presentation
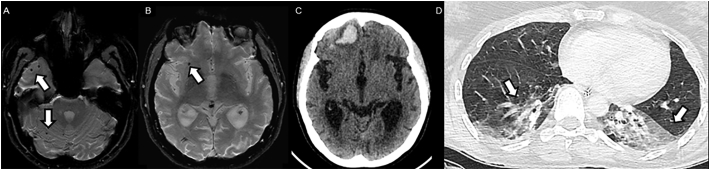
A 38-year-old white woman was admitted to the emergency deparment due to acute impairment of consciousness. She has a past history of early-onset Alzheimer's disease related to a sporadic heterozygous Amyloid Protein Precursor (APP) gene duplication. Before admission, her clinical background was characterized by global aphasia, gait apraxia, myoclonic jerks and sporadic episodes of generalized seizures. There was no previous history of cardiovascular risk factors. Her Brain Magnetic Resonance Imaging presented typical bilateral hippocampus atrophy and scattered microbleeds in the cerebral lobes and cerebellum, sparing the brainstem (Fig. 1A and B). Due to COVID-19 pandemic she was in social isolation with her mother and one caregiver, who was their only link to the outside.
Fig. 1.
: Brain and lung CT imaging suggestive of COVID-19.
(A,B) Axial gradient echo (GRE) T2-weighted magnetic resonance imaging (MRI), showing scattered microbleeds (thin arrows) in the cerebral lobes and cerebellum, sparing the brainstem. (C) Non-contrast brain computed tomography (CT) demonstrates an acute hemorrhage in the right frontal lobe. (D) Transverse thin-section chest computed tomography (CT) scan in a patient with SARS-CoV-2 (COVID-19) infection shows bilateral ground-glass opacities (large arrows).
On the day of her admission, her caregiver reported an acute change in the level of consciousness unrelated to seizures. On clinical examination, she presented stupor (Glasgow Coma Scale was 10) and had no signs of localization; her brainstem reflexes were normal. Brain computed tomography scan was performed and showed acute hemorrhage in the right frontal lobe (Fig. 1C).
On day 1, non-productive cough was noted, but not associated with fever. The infectious panel presented uncommon leukocytosis and lymphopenia, C-Reactive Protein level was 100 mg/L (normal range, < 6 mg/L) and D-dimer 3769 ng/mL (NR, < 400 ng/mL). Platelet levels were normal. Thorax CT scan (Fig. 1D) was performed due to clinical context, which shown bilateral ground-glass opacities and crazy paving appearance highly suggestive of COVID-19 infection in the current clinical context of pandemic and patient was isolated. On day 3, Real Time-Polymerase Chain Reaction to SARS-CoV-2 of oropharyngeal and nasal specimens swabs were positive to SARS-CoV-2.
2. Discussion
COVID-19 has been related to thrombotic conditions, including ischemic stroke [1], cerebral venous thrombosis [2], pulmonary embolism [3], disseminated intravascular coagulation [4]. It is hypothesized that SARS-CoV-2 promotes a pro-thrombotic state [5] which predisposes the occurrence of thrombotic diseases, but the mechanism is still unclear to this date.
There are previous reports of intracerebral hemorrhage during SARS-CoV-2 infection [6], but always there were cardiovascular risk factors or low platelets levels. Herein, we describe a case of a patient who presented to the emergency department with altered level of consciousness and revealed a concomitant COVID-19 infection and intracerebral hemorrhage.
Most of the previous patients in the course of acute cerebrovascular disease had manifestations of ischemic stroke during COVID-19, but this patient presented an intracerebral hemorrhage during the infection, even without known cardiovascular risk factors and normal platelet levels. Even in COVID-19 patients, early post-mortem brain MRI findings [7] suggestive of subcortical micro- and macro-bleeds are possible landmarks of intracranial vasculopathy induced by direct viral action on endothelial cells triggered by high expression of Angiotensin II receptors. We hypothesize that SARS-CoV-2 infection and exacerbated inflammatory process due to abnormal elevation of cytokines (e.g. cytokines storm) contributed to CAA associated vasculopathy [8], aggravated the amyloid-β (Aβ) deposition, accelerating CAA associated vasculopathy, promoting disruption, occlusion and permeability changes and predisposed intracerebral hemorrhage. It is an important note that inflammation is a possible trigger to this process in CAA patients and this subset of patients with COVID-19 has increased viral load, loss of lung function, lung injury and fatal outcomes [9]. Common trigger factors of hemorrhage in CAA patients are hypertension; thrombolytics, anticoagulation, antiplatelet and anti-amyloid therapies, all absent in the present case [8]. Beyond specific genetic factors (APP and Presenilin genes mutations), exposure to severe infections, like sepsis, also recognized by highly abnormal inflammatory responses, were previously associated and recognized as a trigger to stroke [10]. It is clear that CAA is already a condition with high risk of lobar hemorrhage, but appears that combination of abnormal inflammatory response of COVID-19 has developed a central role in increasing this risk.
3. Conclusion
In light of these findings, we suggest that combination of the inflammatory state provoked by COVID-19 infection could work as a trigger to exacerbation of CAA, increasing deposition of Aβ, and its associated vasculopathies, thereby contributing to occurrence of hemorrhagic stroke. Due to current pandemic setting, it may be precedent to perform concomitant CT thorax sacn, in addition to neuroimaging, studies and follow protected code stroke protocols, when a patient presents with decreased level of consciousness and especially in situations of impaired respiratory assessment. Following this procedure may serve to respect the safety of healthcare workers in unexpected situations.
Acknowledgment
We acknowledge Suzanne Adair, pH.D. and Frank Adair, pHarm.D., pH.D. for providing language help and proof reading. This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brasil (CAPES) - Finance Code 001
Contributor Information
Pedro Fraiman, Email: fraiman@ufrn.edu.br.
Clecio Godeiro-Junior, Email: cleciojunior@yahoo.com.br.
References
- 1.Dafer R.M., Osteraas N.D., Biller J. Acute stroke care in the coronavirus disease 2019 pandemic. J. Stroke Cerebrovasc. Dis. 2020;29(1) doi: 10.1016/j.jstrokecerebrovasdis.2020.104881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hughes C., Nichols T., Pike M., Subbe C., Elghenzai S. Cerebral venous sinus thrombosis as a presentation of COVID-19. Eur. J. Case Rep. Intern. Med. 2020;7(5) doi: 10.12890/2020_001691. 001691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wichmann D., Sperhake J.P., Lütgehetmann M., Steurer S., Edler C., Heinemann A., Heinrich F., Mushumba H., Kniep I., Schröder A.S., Burdelski C., de Heer G., Nierhaus A., Frings D., Pfefferle S., Becker H., Bredereke-Wiedling H., de Weerth A., Paschen H.R., Sheikhzadeh-Eggers S., Stang A., Schmiedel S., Bokemeyer C., Addo M.M., Aepfelbacher M., Püschel K., Kluge S. Autopsy findings and venous thromboembolism in patients with COVID-19. Ann. Intern. Med. 2020;173(4):268–277. doi: 10.7326/M20-2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Terpos E., Ntanasis-Stathopoulos I., Elalamy I., Kastritis E., Sergentanis T.N., Politou M., Psaltopoulou T., Gerotziafas G., Dimopoulos M.A. Hematological findings and complications of COVID-19. Am. J. Hematol. 2020;95(7):834–847. doi: 10.1002/ajh.25829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cavallieri F., Marti A., Fasano A., Salda A.D., Ghirarduzzi A., Moratti C., Bonacini L., Ghadirpour R., Pascarella R., Valzania F., Zedde M. Prothrombotic state induced by COVID-19 infection as trigger for stroke in young patients: a dangerous association. eNeurologicalSci. 2020;100247 doi: 10.1016/j.ensci.2020.100247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morassi M., Bagatto D., Cobelli M., D'Agostini S., Gigli G.L., Bnà C., Vogrig A. Stroke in patients with SARS-CoV-2 infection: case series. J. Neurol. 2020;268(8):2185–2192. doi: 10.1007/s00415-020-09885-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Coolen T., Lolli V., Sadeghi N., Rovai A., Trotta N., Taccone F.S., Creteur J., Henrard S., Goffard J.-C., Dewitte O., Naeije G., Goldman S., De Tiege X. Early postmortem brain MRI findings in COVID-19 non-survivors. medRxiv. 2020 doi: 10.1212/WNL.0000000000010116. [DOI] [PubMed] [Google Scholar]
- 8.Yamada M. Cerebral amyloid angiopathy: emerging concepts. J. Stroke. 2015;17(1):17–30. doi: 10.5853/jos.2015.17.1.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vaninov N. In the eye of the COVID-19 cytokine storm. Nat. Rev. Immunol. 2020;20(5):277. doi: 10.1038/s41577-020-0305-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sebastian S., Stein L.K., Dhamoon M.S. Infection as a stroke trigger. Stroke. 2019;50(8):2216–2218. doi: 10.1161/STROKEAHA.119.025872. [DOI] [PubMed] [Google Scholar]